Abstract
Arthroscopic shoulder surgery can be performed in both the beach chair and lateral decubitus positions. The lateral decubitus position allows for excellent exposure to all aspects of the glenohumeral joint and is therefore frequently employed in procedures such as stabilization, in which extensive visualization of the inferior and posterior aspects of the joint is required. Improved visualization is imparted due to applied lateral and axial traction on the operative arm, which increases the glenohumeral joint space. To perform arthroscopy surgery in the lateral decubitus position successfully, meticulous care during patient positioning and setup must be taken. In this Technical Note, we describe the steps required to safely, efficiently, and reproducibly perform arthroscopic shoulder surgery in the lateral decubitus position.
Arthroscopic shoulder surgery can be performed in both the beach chair (BC) and lateral decubitus (LD) positions. The advantages and disadvantages of both positions for shoulder arthroscopy have been described in detail.1, 2 One of the most significant advantages of the LD position is increased visualization and working space within the glenohumeral joint with instrumentation. Specifically, improved access is allowed to the inferior and posterior labrum, inferior capsule, subacromial space, and articular side of the rotator cuff.2 This is accomplished with lateral and axial traction applied to the operative arm held within a traction device. By positioning the glenoid parallel to the floor,3 a reference point can be established that assists in identifying relevant surgical anatomy and orienting the operating surgeon. The LD position also allows the surgeon to operate with his/her arms at his/her side, rather than in an abducted position, as is often required while working in the BC position, which allows for increased comfort and decreased fatigue.
The effort and time needed to safely set patients up for surgery in both BC and LD often depends on the familiarity and experience of the surgeon, the operating room staff, the type of anesthesia, and the number of assistants available. Surgeons' preferences for patient positioning are often based on their training experience, and certainly, level of comfort plays a significant role in overall decision making. In the subsequent section, we describe our technique for LD patient positioning for shoulder arthroscopy. A summary of key steps is provided in Table 1, and a summary of the technique is provided in Video 1.
Table 1.
Key Steps to Lateral Decubitus Patient Positioning
| 1. Proper placement of beanbag device on operating table and set up of lateral traction device |
| 2. Coordinated team approach to rolling patient into lateral decubitus position, making sure to stabilize head during the roll |
| 3. Placement of pillows between legs and underneath bottom leg for adequate padding |
| 4. Insertion of axillary roll |
| 5. Inflation of beanbag device and securing patient with table strap and tape |
| 6. Turning operating table 60° to 90° |
| 7. Placement of operative arm in lateral traction device with maximum of 10 pounds of applied traction |
| 8. Standard sterile prepping and draping |
Technique
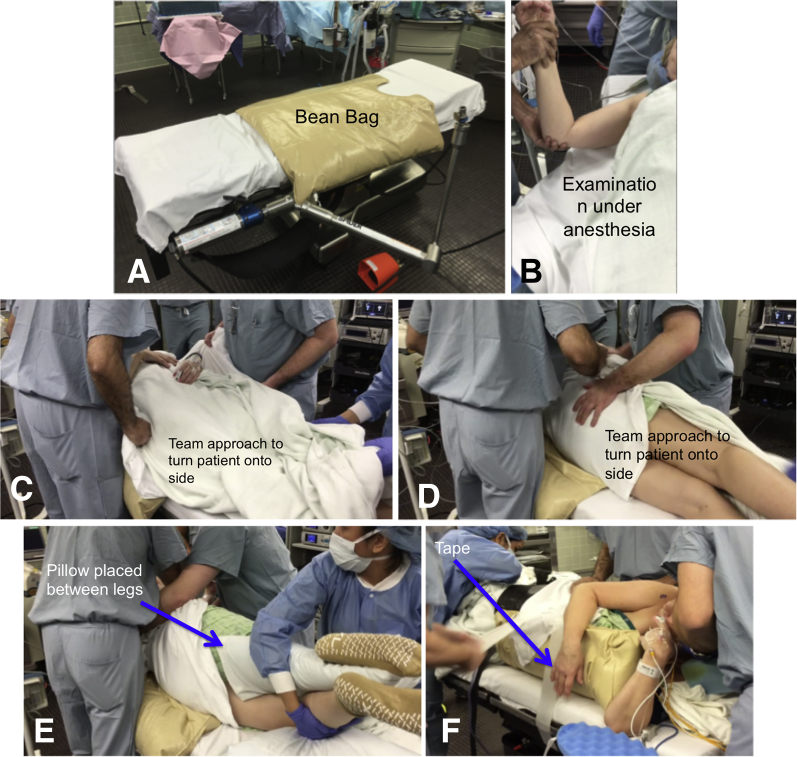
Following the induction of regional anesthesia, with or without general anesthesia, the patient is transferred to the operating room table using a team approach, coordinated by the anesthesiologist. The setup of the LD position begins with the patient lying supine on a beanbag (Olympic Vac-Pac System, Natus Medical, San Carlos, CA) on the operating table (Fig 1A). Care should be taken during patient transfer onto the operating table to ensure the patient is optimally positioned on the beanbag, as it is more difficult to adjust the position of the patient relative to the beanbag after transfer. Prior to patient positioning, an examination under anesthesia should be carried out on the operative arm (Fig 1B). The examiner should assess range of motion in all planes as well as stability in all directions. Tape placed over the eyes by the anesthesia team can protect the eyes from corneal abrasions. Sequential compression devices are placed on both lower extremities for venous thromboembolism prophylaxis.
Fig 1.
(A) Operating table with beanbag device (Olympic Vac-Pac System, Natus Medical, San Carlos, CA) and traction device (Spider 2 Limb Positioner, Smith and Nephew, Andover, MA) secured to table prior to the start of the procedure. (B) Examination under anesthesia on the right arm for evaluation of range of motion in all planes. (C, D) The surgical and anesthesia teams roll the patient to the lateral decubitus position with the operative shoulder up. (E) Both knees are bent, and padding (i.e., pillow or foam pad) is placed under the down knee as well as in between the knees to protect the fibular head and avoid pressure injuries to the common peroneal nerve. (F) A surgical table strap (Bryton Corporation, Indianapolis, IN) and multiple pieces of adhesive tape spanning the width of the operating table are used to secure the patient within the beanbag and to the table.
Patient Positioning
Following the examination under anesthesia, the surgical and anesthesia teams roll the patient into the LD position with the operative shoulder up (Fig 1 C and D). A team approach must be used during this and all portions of the setup to ensure that the patient is being moved and positioned safely. The head is stabilized at all times by the anesthesia team during positioning and is maintained in the neutral position during the procedure by resting on a foam pad (or pillow) and being secured with tape (Table 1). Care is taken to protect the eyes and ears. Next the sides of the beanbag are brought up and stabilized along both the front and back of the patient by the surgical team, making sure there is a barrier (such as a blanket or sheet) between the beanbag and the patient. Once satisfied with the position of the beanbag and the patient, suction is then applied to the beanbag to secure it into place. At this time, the surgical team should inspect the beanbag position to make sure it is in such a position to allow the surgeon to have access to the shoulder by aligning the upper border of the beanbag with the axilla of the nonoperative arm. Some surgeons prefer a “sloppy lateral” position in which the beanbag is set such that the patient's torso leans posteriorly approximately 20° to 30°. Both knees are bent, and padding in the form of a pillow or foam pad is placed under the down knee as well as in between the knees to protect the fibular head and avoid pressure injuries to the common peroneal nerve (Fig 1E, Table 2). Next an axillary roll is placed under the nonoperative axilla, with approximately 2 to 3 fingerbreadths between the roll and the axilla anterolaterally, to minimize compression to the brachial plexus and to allow for adequate blood flow to the nonoperative arm. There are a variety of options for the axillary roll itself, including a cylindrical gel pad, an inflated bladder of a blood pressure cuff, a bag of intravenous fluids wrapped in a towel, and so on. Once the patient is properly positioned, a safety strap is used to secure the patient within the beanbag and to the table (Fig 1F). In addition, we secure the patient with thick tape both at the level of the thighs and the torso in an effort to maintain the body in a steady position for the duration of the surgical procedure. The operating table is then rotated 60° to 90° to give the surgical team a dedicated workspace, while maintaining appropriate access to the patient for the anesthesia team.
Table 2.
Pearls and Pitfalls of the Lateral Decubitus Position
| Pearls | Pitfalls |
|---|---|
| Document detailed physical examination both in the office and under anesthesia, including range of motion in all planes. | Pad and carefully position all bony prominences and the contralateral arm when positioning patient in the lateral decubitus position. |
| Use a maximum of 10 pounds of applied traction to minimize risk of neurovascular injury. | Double check that the patient is positioned appropriately prior to sterile draping as poor positioning will increase difficulty of the case. |
| The authors prefer to position the patient in the “sloppy lateral” position if intraoperative conversion to an open approach is anticipated. | Carefully placed portals under direct visualization will help to avoid neurovascular injury. |
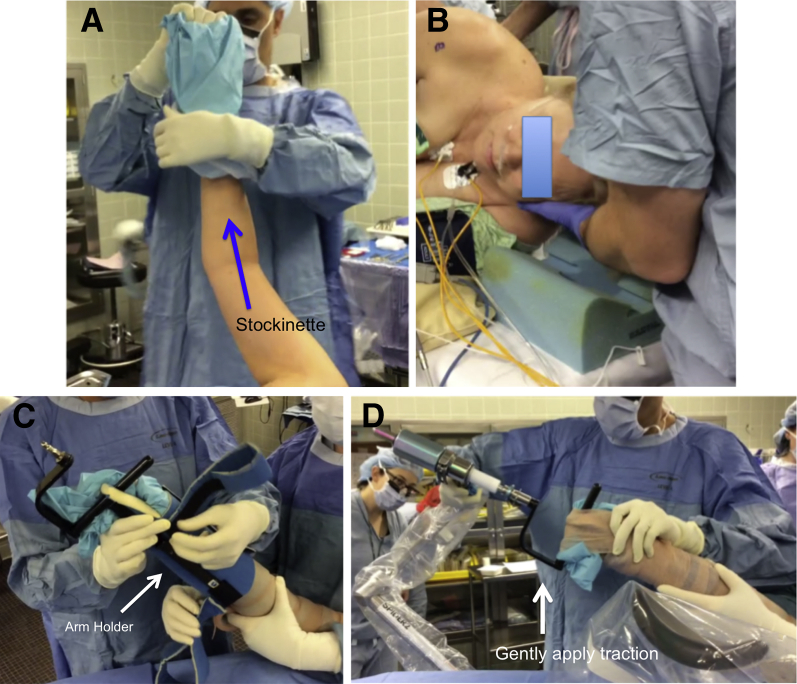
Traction Setup
After the operating table is secured into position, the operative arm is sterilely prepped and draped. The operative arm is then placed in a sterile stockinette (Fig 2A) and wrapped with a self-adherent wrap, such as Coban (3M Health Care, St. Paul, MN), making sure to keep the hand available for placement in a commercial arm-holding device. Commonly available arm-holding devices include the shoulder distraction system/STaR sleeve (Arthrex, Naples, FL) or the Spider (Smith and Nephew, Andover, MA), as shown in Video 1. The anesthesia staff should check the placement and security of the patient's head prior to securing the operative arm in the traction device (Fig 2B). The arm holder is secured around the operative arm, and additional self-adherent wrap is applied circumferentially for further security (Fig 2C). The arm is then placed into the traction device, and traction is applied (Fig 2 D-F). When applying traction, one must consider adequate visualization against the risk of neurovascular damage and reduced perfusion of the operative arm.4 A position that allows for approximately 15° of forward flexion and 45° of abduction, with no more than 10 pounds of axial traction, has been shown to maximize operative visibility while minimizing brachial plexus strain.5 Care must be taken to ensure that the patient's head and neck are maintained in a neutral position before the procedure starts (Fig 2B). While the specific steps to apply traction depend on the traction system being used, the principles remain the same, and care should be taken to ensure that the minimum traction necessary to visualize the joint is applied to minimize stress on critical neurovascular structures. In any traction system, the arm may be adjusted with regards to the amount of abduction and forward flexion depending on surgeon preference. Similarly, regardless of the traction system used, a sterile “bump” of rolled towels or sheets can be placed in the axillary space in order to improve abduction without increasing traction.
Fig 2.
(A) The operative arm (right side) is placed in a sterile stockinette (Smith and Nephew, Andover, MA) and then wrapped with Coban (3M, St. Paul, MN) making sure to keep the hand open for placement into the arm holder device (Spider 2 Limb Positioner, Smith and Nephew). (B) The head is stabilized at all times by the anesthesia team and can be maintained in the neutral position with a foam pad and towels if necessary. (C) The arm holder (Smith and Nephew) is secured around the operative arm with Velcro straps, and then Coban (3M) is applied circumferentially for further security. (D, E) The arm is then placed into the traction device (Spider 2 Limb Positioner) and traction is applied with a maximum of 10 pounds. (F) Operative arm (right arm) placed in lateral traction device (Spider 2 Limb Positioner) wrapped in Coban for securement of the operative arm after sterile preparation and subsequent draping. (G, H) Example of the Arthrex (Naples, FL) commercially available arm holder for securement of the operative arm after sterile preparation and draping.
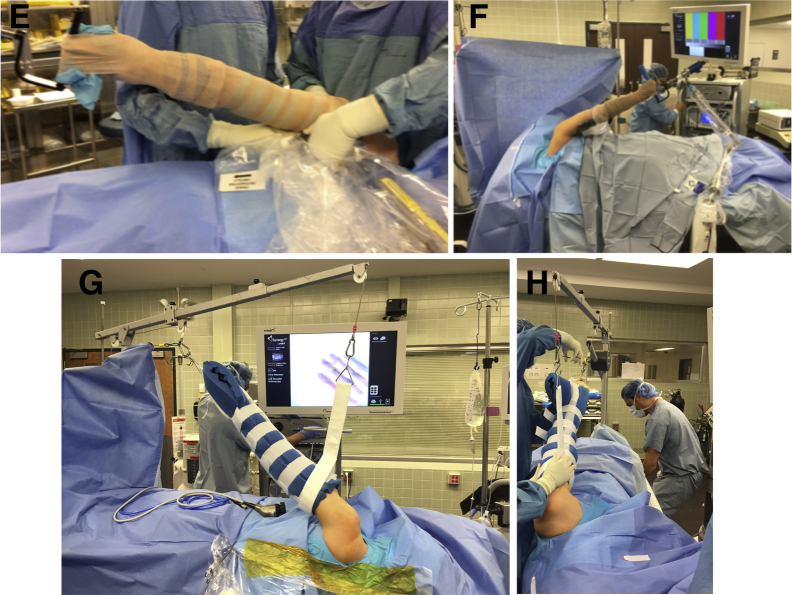
Portal Placement
After the patient is adequately positioned, anticipated portal sites are drawn out using bony landmarks, including the acromion, clavicle, acromioclavicular joint, and coracoid process (Fig 3). Before proceeding further, the surgical team ensures that the proper perioperative arthroscopy fluid is readily available. The authors typically use an arthroscopy pump system with the pressure initially set to 40 mmHG, with normal saline with 1:1,000 epinephrine (typically 1 mL for a 5-L bag of fluid). In the BC position, the standard posterior portal is typically placed 2 cm inferior and 1 cm medial to the posterolateral corner of the acromion. In the LD position, this portal is established slightly more laterally, typically in line with the posterolateral border of the acromion. After the posterior portal is established, we typically insert the arthroscope and establish the subsequent portals under direct visualization. For the standard anterior midglenoid portal, we typically employ palpation of the soft spot just lateral to the coracoid process to help determine the anticipated site for this portal, followed by spinal needle localization under direct visualization. When establishing an anteroinferior (trans-subscapularis, or 5 o'clock) portal, one should be cautious of the risks of damage to the musculocutaneous nerve and cephalic vein, which are more at risk than when establishing these portals in the BC position.6 Accessory portals, including the anterior-superior-lateral portal as well as the posterolateral accessory (7 o'clock) portal, can be placed depending on the nature of the procedure. For standard stabilization procedures in the LD position, we typically use a standard posterior portal (established just off the posterolateral edge of the acromion), a standard anterior portal, a percutaneous trans-subscapularis portal, and a 7 o'clock portal.
Fig 3.

Operative arm (right arm) placed in lateral traction device (Spider 2 Limb Positioner, Smith and Nephew, Andover, MA) with anticipated portal sites marked using bony landmarks, including the acromion, clavicle, acromioclavicular joint, and coracoid process. Here the posterior portal (P) and posterolateral portal (PL) are marked.
Discussion
In this Technical Note, we describe a safe, reliable, and reproducible technique for patient positioning in the LD position for shoulder arthroscopy. As noted above, one of major advantages of the LD position is increased visualization and access to the glenohumeral joint, lending itself to procedures such as instability and SLAP repairs (Table 3).5 In this position, excellent visualization of the posterior and posteroinferior aspects of the joint are allowed, often obviating the need to create portals that disrupt the rotator cuff.7 Setup uses the application of lateral and axial traction to the operative arm, thereby widening the joint space and allowing for easier use of instrumentation and suture passage.2
Table 3.
Advantages and Disadvantages of the Lateral Decubitus Position
| Advantages | Disadvantages |
|---|---|
| Improved visualization of the glenohumeral joint, obviating the need to create accessory portals that disrupt the rotator cuff | Risk of neurologic injury due to applied lateral and axial traction on the operative arm (peripheral nerves and brachial plexus) |
| Increased working space, specifically to the inferior and posterior labrum, inferior capsule, subacromial space, and articular side of the rotator cuff | Risk of vascular injury due to portal placement, especially the cephalic vein |
| Allows surgeon to operate with arms at side for increased comfort and decreased fatigue (as opposed to abducted position) | Increased difficulty with intraoperative conversion to an open approach |
| Bubbles created by electrocautery move laterally, providing a clearer view | Difficulty manipulating the operative arm when in applied traction |
| Lower incidence of cerebral desaturation events compared with the beach chair position. | Increased difficulty identifying internal and external anatomic landmarks |
When considering both the BC and LD positions, there are many advantages and disadvantages associated with each setup. One disadvantage of the BC position is that the patient head may act as a mechanical barrier for superior and posterior portals, which is not typically a problem in the LD position. The LD position allows full access circumferentially around the glenohumeral joint without impedance by the patient's head. In addition, fogging of the arthroscope lens and collection of bubbles within the subacromial space can obstruct the view during shoulder arthroscopy in the BC position,2 whereas in the LD position, bubbles generated by electrocautery move laterally, providing a clearer view. Deliberate hypotensive anesthesia is commonly used to reduce bleeding during arthroscopic shoulder surgery; however, this may lead to cerebrovascular morbidity, particularly in the BC position in which it may be more difficult to monitor the patient's true cerebral blood pressure due to the upright position of the patient.2 Murphy et al.8 reported a significantly higher incidence of cerebral desaturation events during arthroscopic shoulder surgery in the BC position compared with in the LD position.
Intraoperative conversion to an open approach has been thought to be more challenging in the LD position compared with the BC position and may require repositioning with new draping/prepping. In the authors' experience, the most common reason to convert from an arthroscopic procedure to an open procedure is to perform a mini-open proximal biceps tendon tenodesis. In these cases, the authors will initially position the patient in the “sloppy lateral” position as described earlier, and when the time comes to convert to the open procedure, traction is released and the patient is gently leaned backward in a safe position, obviating the need for a new drape/prep.
Importantly, there are potential complications associated with the LD position, including neurovascular injuries related to traction and portal placement. The traction applied in LD can lead to damage of peripheral nerves and the brachial plexus, with a reported incidence of up to 10% to 30%.1, 9 Fortunately, despite this relatively high incidence, the persistence of clinically significant neurapraxia is relatively rare.2 Andrews et al.10 reported neurapraxia of the musculocutaneous nerve in one patient and ulnar nerve in 2 patients, out of a series of 120 patients undergoing shoulder arthroscopy in the LD position. Similarly, Ogilvie-Harris et al.11 reported one case of musculocutaneous nerve palsy in 439 patients undergoing arthroscopic shoulder surgery in the LD position. Klein et al.12 examined the strain placed on the brachial plexus in the LD position and concluded that 45° of forward elevation with 0° or 90° of abduction yielded maximum visibility with minimal strain. Lo et al.13 performed a cadaveric study examining portal placement in shoulder arthroscopy in the LD position to evaluate the neurovascular structures at risk using an outside-in technique. The investigators found that the cephalic vein was at the greatest risk of injury during placement of an anterior or 5 o'clock portal, but other structures including the axillary nerve, musculocutaneous nerve, lateral cord of the brachial plexus, and axillary artery were greater than 20 mm away from portal sites. In another cadaveric study, Lo et al. characterized the distances of specific portions of the coracoid to at-risk neurovascular structures. The investigators found that the lateral cord of the brachial plexus was the closest structure to the anteromedial coracoid tip and that the axillary nerve was closest to the anteromedial aspect of the coracoid base.14 These 2 studies suggest that portal placement in the LD position and surgery in the proximity of the coracoid is relatively safe; however, knowledge of relevant surgical anatomy is critical in avoiding potentially serious complications.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.T.H. receives support from Norvartis and Nuvasive. M.T.P. receives support from AAOS, Arthrex, SLACK, the American Orthopaedic Society for Sports Medicine, American Shoulder and Elbow Surgeons, Arthroscopy, the Arthroscopy Association of North America, the International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine, Joint Restoration Foundation (Allosource), Knee, Orthopedics, San Diego Shoulder Institute, and Society of Military Orthopaedic Surgeons. A.A.R. receives support from the American Orthopaedic Society for Sports Medicine, Arthrex, DJO Surgical, Orthopedics, Orthopedics Today, Ossur, SAGE, Saunders/Mosby-Elsevier, SLACK, Smith and Nephew, Wolters Kluwer Health, Lippincott Williams and Wilkins, and American Shoulder and Elbow Surgeons. N.N.V. receives support from Arthrex, Arthroscopy, Arthrosurface, Cymedica, DJ Orthopaedics, Minivasive, Omeros, Orthospace, Smith and Nephew, ConMed Linvatec, Miomed, Mitek, Vindico Medical-Orthopedics Hyperguide, Arthroscopy Association Learning Center Committee, SLACK American Orthopaedic Society for Sports Medicine, American Shoulder and Elbow Surgeons, Journal of Knee Surgery, and Ossur.
Supplementary Data
Technique for lateral decubitus patient position setup of the right arm including examination under anesthesia, axillary roll insertion, lateral traction device setup (Spider 2 Limb Positioner, Smith and Nephew, Andover, MA), and marking of anticipated portal placement with narration of all critical steps.
References
- 1.Peruto C.M., Ciccotti M.G., Cohen S.B. Shoulder arthroscopy positioning: lateral decubitus versus beach chair. Arthroscopy. 2009;25:891–896. doi: 10.1016/j.arthro.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Li X., Eichinger J.K., Hartshorn T., Zhou H., Matzkin E.G., Warner J.P. A comparison of the lateral decubitus and beach-chair positions for shoulder surgery: advantages and complications. J Am Acad Orthop Surg. 2015;23:18–28. doi: 10.5435/JAAOS-23-01-18. [DOI] [PubMed] [Google Scholar]
- 3.Gross R.M., Fitzgibbons T.C. Shoulder arthroscopy: a modified approach. Arthroscopy. 1985;1:156–159. doi: 10.1016/s0749-8063(85)80002-5. [DOI] [PubMed] [Google Scholar]
- 4.Hennrikus W.L., Mapes R.C., Bratton M.W., Lapoint J.M. Lateral traction during shoulder arthroscopy: its effect on tissue perfusion measured by pulse oximetry. Am J Sports Med. 1995;23:444–446. doi: 10.1177/036354659502300412. [DOI] [PubMed] [Google Scholar]
- 5.Provencher M.T., McIntire E.S., Gaston T.M., Frank R.M., Solomon D.J. Avoiding complications in shoulder arthroscopy: pearls for lateral decubitus and beach chair positioning. Techn Shoulder Elbow Surg. 2010;11:1–3. [Google Scholar]
- 6.Gelber P.E., Reina F., Caceres E., Monllau J.C. A comparison of risk between the lateral decubitus and the beach-chair position when establishing an anteroinferior shoulder portal: a cadaveric study. Arthroscopy. 2007;23:522–528. doi: 10.1016/j.arthro.2006.12.034. [DOI] [PubMed] [Google Scholar]
- 7.Provencher M.T., Romeo A.A., Solomon D.J., Bach B.R., Jr., Cole B.J. Arthroscopic preparation of the posterior and posteroinferior glenoid labrum. Orthopedics. 2007;30:904–905. doi: 10.3928/01477447-20071101-03. [DOI] [PubMed] [Google Scholar]
- 8.Murphy G.S., Szokol J.W., Marymont J.H. Cerebral oxygen desaturation events assessed by near-infrared spectroscopy during shoulder arthroscopy in the beach chair and lateral decubitus positions. Anesth Analgesia. 2010;111:496–505. doi: 10.1213/ANE.0b013e3181e33bd9. [DOI] [PubMed] [Google Scholar]
- 9.Skyhar M.J., Altchek D.W., Warren R.F., Wickiewicz T.L., O'Brien S.J. Shoulder arthroscopy with the patient in the beach-chair position. Arthroscopy. 1988;4:256–259. doi: 10.1016/s0749-8063(88)80040-9. [DOI] [PubMed] [Google Scholar]
- 10.Andrews J.R., Carson W.G., Jr., Ortega K. Arthroscopy of the shoulder: technique and normal anatomy. Am J Sports Med. 1984;12:1–7. doi: 10.1177/036354658401200101. [DOI] [PubMed] [Google Scholar]
- 11.Ogilvie-Harris D.J., Wiley A.M. Arthroscopic surgery of the shoulder. A general appraisal. J Bone Joint Surg Br. 1986;68:201–207. doi: 10.1302/0301-620X.68B2.3958003. [DOI] [PubMed] [Google Scholar]
- 12.Klein A.H., France J.C., Mutschler T.A., Fu F.H. Measurement of brachial plexus strain in arthroscopy of the shoulder. Arthroscopy. 1987;3:45–52. doi: 10.1016/s0749-8063(87)80009-9. [DOI] [PubMed] [Google Scholar]
- 13.Lo I.K., Lind C.C., Burkhart S.S. Glenohumeral arthroscopy portals established using an outside-in technique: neurovascular anatomy at risk. Arthroscopy. 2004;20:596–602. doi: 10.1016/j.arthro.2004.04.057. [DOI] [PubMed] [Google Scholar]
- 14.Lo I.K., Burkhart S.S., Parten P.M. Surgery about the coracoid: neurovascular structures at risk. Arthroscopy. 2004;20:591–595. doi: 10.1016/j.arthro.2004.04.060. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique for lateral decubitus patient position setup of the right arm including examination under anesthesia, axillary roll insertion, lateral traction device setup (Spider 2 Limb Positioner, Smith and Nephew, Andover, MA), and marking of anticipated portal placement with narration of all critical steps.