Abstract
Anterior cruciate ligament reconstruction with bone–patellar tendon–bone autograft has long been considered the graft preference for young, active patients with anterior cruciate ligament injuries. The central-third of the native patellar tendon is a reliable graft and is the preferred option for competitive athletes given its excellent track record with high return-to-play rates and low failure rates. Disadvantages to using this graft include donor site morbidity and associated postoperative anterior knee pain, the risk of patellar fracture or patellar tendon tear, and the potential for graft-construct mismatch. In this Technical Note, we describe our preferred technique for bone–patellar tendon–bone autograft harvest and preparation for anterior cruciate ligament reconstruction.
Anterior cruciate ligament reconstruction (ACLR) remains one of the most commonly performed knee operations in the United States.1 Among ACLR autograft options, the literature is variable regarding the preferred graft choice for a given patient, as excellent functional outcomes with low recurrence rates have been reported after both bone–patellar tendon–bone (BPTB) autograft and hamstring autograft.2 The central one-third of the patellar tendon has become the preferred autograft for ACLR in high-level athletes with excellent long-term outcomes, low recurrence rates, and high rates of return to sport.3, 4 Graft selection for ACLR is largely based on the surgeon's experience and preference, although several patient-specific factors must be considered, including patient size, as hamstring tendons may be too small to allow for an adequate graft, particularly in petite female patients.
In this Technical Note, we describe our preferred technique for BPTB autograft harvest and graft preparation for ACLR. A summary of key steps is provided in Table 1, and a summary of the technique is provided in Video 1.
Table 1.
Key Steps for Bone–Patellar Tendon–Bone Autograft Harvest for ACLR
| Identify anatomic landmarks |
| Tibial tubercle |
| Patellar borders |
| Vertically oriented skin incision—approximately 5 cm |
| Visualization of both medial and lateral borders of the patellar tendon |
| Incise and preserve the paratenon for complete visualization of the patellar tendon |
| Measure and mark the central one-third of the patellar tendon |
| Longitudinally incise the tendon from proximal to distal after collagen orientation |
| Harvest tibial plug—10 mm × 25 mm |
| Harvest patella bone plug—10 mm × 20-25 mm |
| Separate autograft from the underlying patellar fat pad |
| Accurately size the bone plug according to the surgeon's preference |
| Write down bone plug measurements |
| Drill 2 holes in the tibia bone plug and 1 hole in the femoral bone plug—using the K wire |
| Passing a No. 5 suture through each hole |
| Mark the bone-tendon junction on both bone plugs for proper orientation during graft passaging and fixation |
| Bone grafting—focus on the patella first |
| Closure of the paratenon using a No. 1 absorbable suture |
| Closure of subcutaneous and skin layers in a standard fashion |
ACLR, anterior cruciate ligament reconstruction.
Technique
Patient Positioning
We perform ACLR under general anesthesia with the patient in the supine position. Before final positioning, the injured knee is examined under anesthesia to confirm the diagnosis. If there is any concern over the diagnosis of an ACL injury, a diagnostic arthroscopy can be performed before harvesting the patellar tendon graft.
After the examination under anesthesia, a padded tourniquet is placed high on the operative thigh, and the patient is positioned such that the operative leg is hanging off of the end of the operating table in a leg holder (Arthrex, Naples, FL), with the contralateral leg in a well-leg holder. The foot of the bed is lowered, allowing the surgeon room to harvest the graft while seated. The operative leg is prepped and draped in a standard fashion.
Graft Harvest
With the knee flexed to 90°, an approximately 8-cm longitudinal incision is made from the inferior pole of the patella to approximately 2 cm distal to the tibial tubercle, along the medial aspect of the patellar tendon (not directly in the midline). Placing this incision slightly medial will more easily allow access for tibial tunnel drilling without having to extend the incision. Dissection is carried through the subcutaneous tissue to the patellar tendon paratenon layer sharply with a knife. Small skin flaps can be created to allow for adequate visualization of the medial and lateral borders of the patellar tendon. The paratenon is then incised longitudinally along the mid-portion of the patellar tendon. Typically we will create a small “nick” in the paratenon with a No. 15 scalpel, and then use Metzenbaum scissors to incise the paratenon proximally and distally, exposing the underlying patellar tendon (Fig 1).
Fig 1.
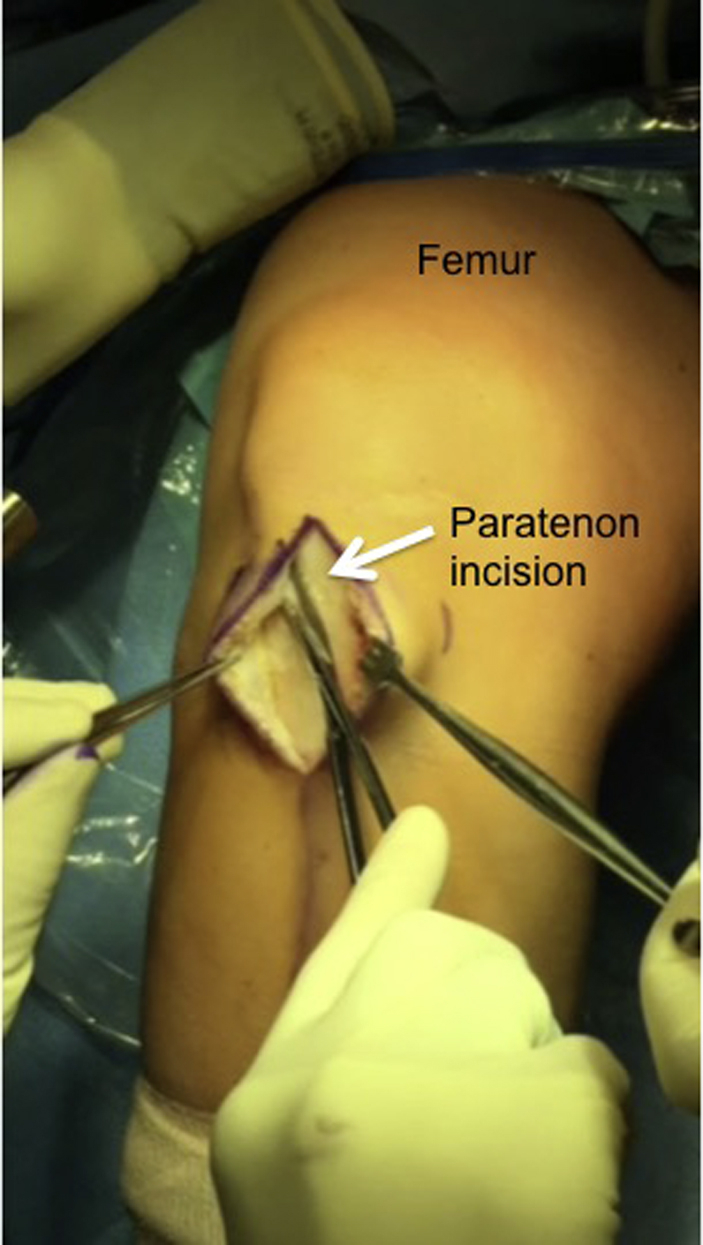
Intraoperative photograph showing identification and dissection of the paratenon layer during bone–patellar tendon–bone autograft harvest in a patient undergoing left knee anterior cruciate ligament reconstruction.
At this point, a ruler is used to measure the width of the patellar tendon, which is typically 30 mm (Fig 2). The ruler is then used to identify the middle one-third of the tendon, which is what will ultimately be harvested. The distal pole of the patella and tubercle is lightly marked with a sterile marking pen. A thin osteotome (Arthrex) or the No. 238 saw blade (Stryker, Kalamazoo, MI) can be used as a template for the planned harvest width. Care is taken to leave at least 10 mm of tendon medially. Next, starting either medially or laterally, a scalpel is used to incise the tendon longitudinally from proximal to distal, keeping the knife blade moving smoothly in line with the fibers of the tendon until the tibia is reached (Fig 3). This step is then repeated on the other side of the tendon graft. Care should be taken not to narrow or widen the second incision relative to the initial incision.
Fig 2.
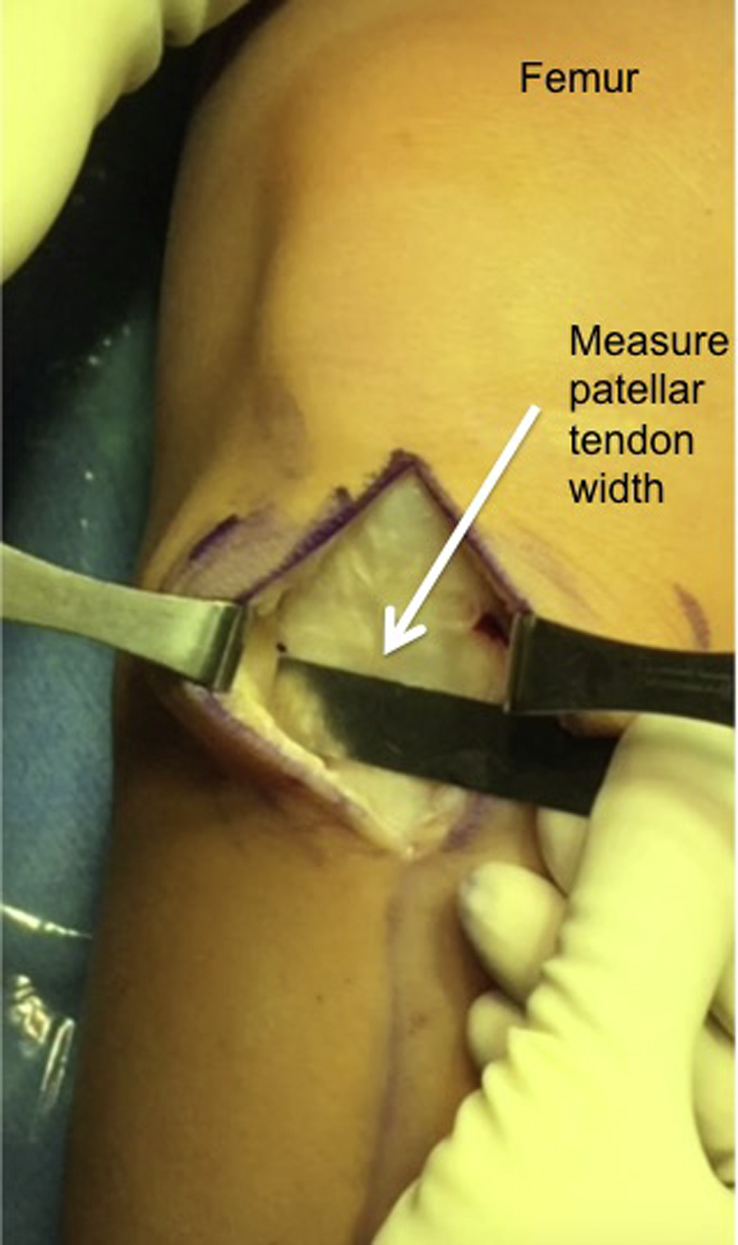
Intraoperative photograph of a patient undergoing left knee anterior cruciate ligament reconstruction showing measurement of the patellar tendon width before harvest.
Fig 3.
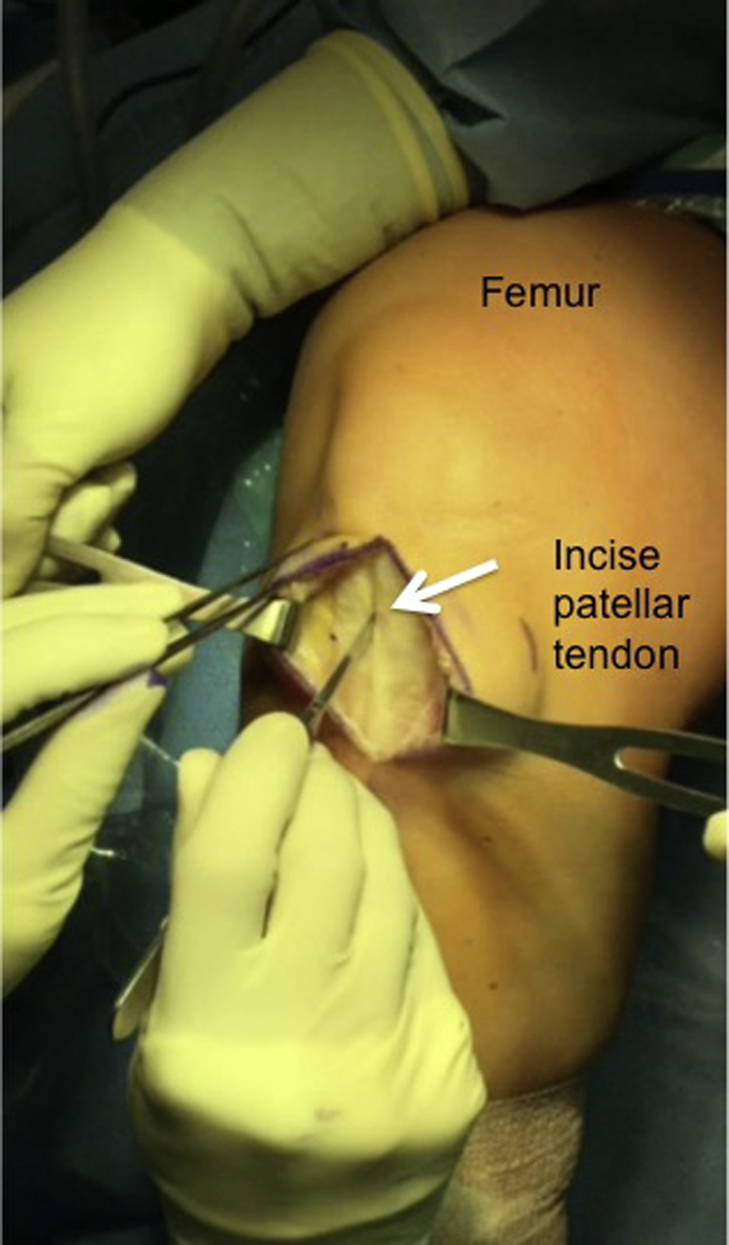
Intraoperative photograph of a patient undergoing left knee anterior cruciate ligament reconstruction showing the harvest of the central third of the patellar tendon with a scalpel.
Next, the tibial plug is harvested. We aim for a bone plug that is approximately 10 mm wide and 25 mm long. The oscillating saw (Stryker) is used to score the tibial cortex before penetrating the saw blade into the bone (Fig 4). Once the cortex has been scored, the saw blade is inserted to a depth of approximately 8 to 10 mm along each side of the plug. The saw blade should be aimed slightly medially when on the lateral side of the tibial plug, and slightly laterally when on the medial side of the tibial plug, to ultimately create an equilateral triangle-shaped tibial bone plug. The distal horizontal (cross) cut is made by aiming the saw 45° obliquely toward either of the longitudinal cuts, to avoid cutting beyond the longitudinal cuts, thus avoiding the creation of a potential stress riser in the tibial bone. A thin osteotome (Arthrex) is then used to gently lift the tibial plug out from the tibia. If adequate saw cuts have been made, the tibial plug should be able to be easily freed up. Do not force the tibial plug out by levering it with the osteotome—instead, recut with the saw if necessary.
Fig 4.
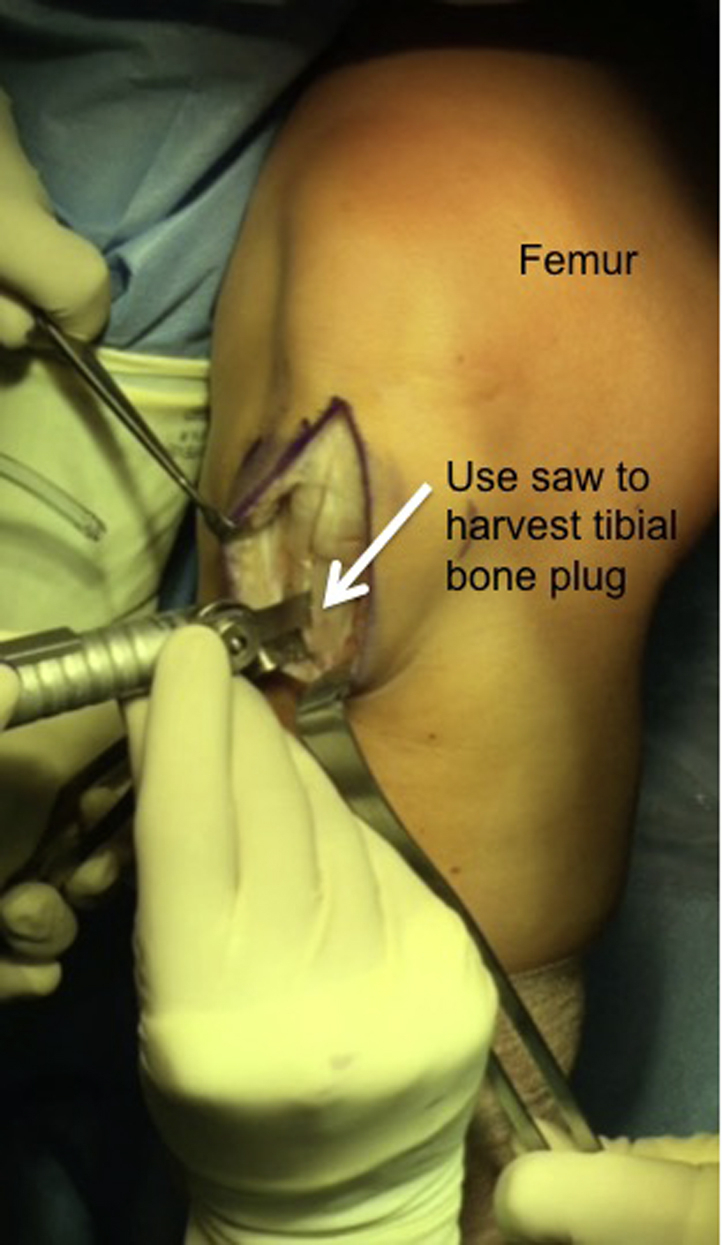
Intraoperative photograph of a patient undergoing left knee anterior cruciate ligament reconstruction showing harvesting of the tibial bone plug with an oscillating saw.
Next, attention is turned to the patellar plug. We aim for a bone plug that is approximately 10 mm wide and 20 to 25 mm long. The oscillating saw (Stryker) is used to score the patellar cortex before actually penetrating the saw blade into the bone (Fig 5). Once the cortex has been scored, the saw blade is inserted to a depth of approximately 6 to 7 mm along each side of the plug, taking care to avoid injury to the underlying articular cartilage. The saw blade should be aimed approximately 30° toward the midline when harvesting on either side of the plug to ultimately create a trapezoidal-shaped patellar bone plug. The proximal horizontal (cross) cut is made by aiming the saw 45° obliquely toward either of the longitudinal cuts, to avoid cutting beyond the longitudinal cuts, thus avoiding the creation of a potential stress riser in the patellar bone. Thin curved osteotomes (Arthrex) are used to gently free the plug out from the patella. If adequate saw cuts have been made, the patellar plug should be able to be easily freed up (Fig 6). We recommend avoiding the use of a mallet when using an osteotome on the patella to decrease fracture risk. Careful dissection with Metzenbaum scissors is used to remove any remaining soft tissue attachments, and the graft is carefully removed from the knee by the harvesting surgeon and brought to the back table.
Fig 5.
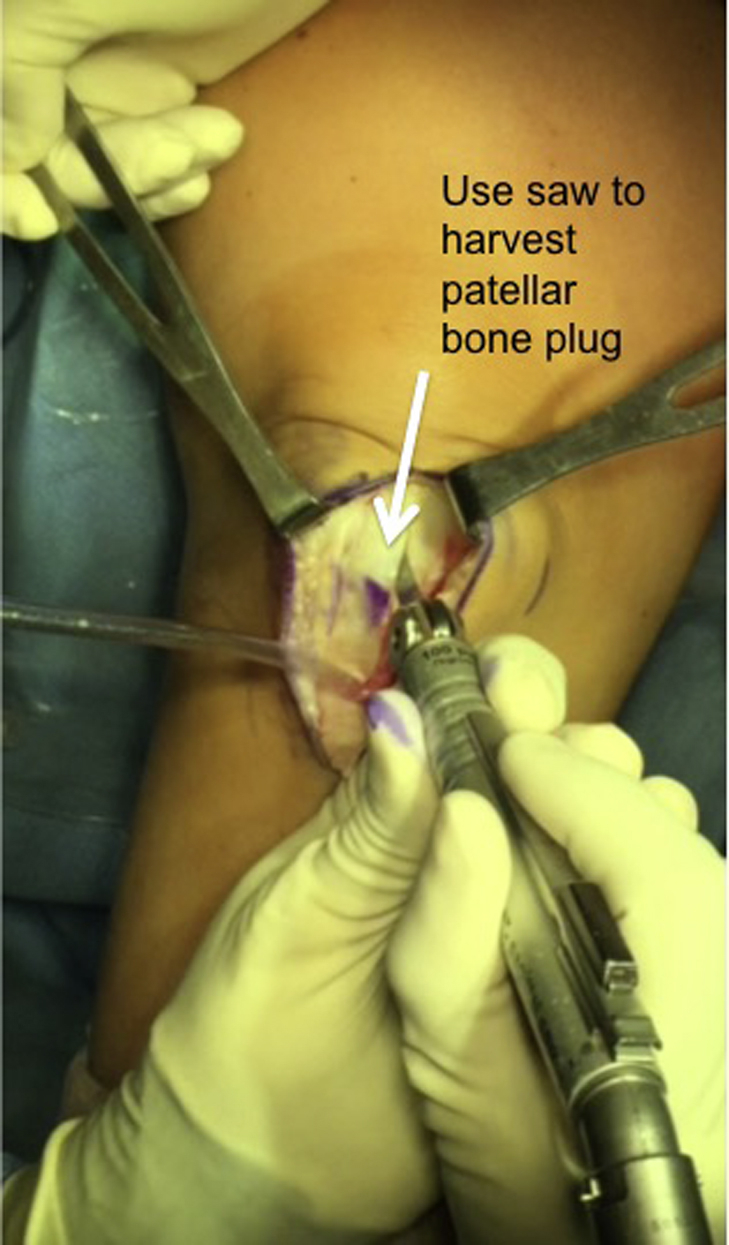
Intraoperative photograph of a patient undergoing left knee anterior cruciate ligament reconstruction showing harvesting of the patellar bone plug with an oscillating saw.
Fig 6.
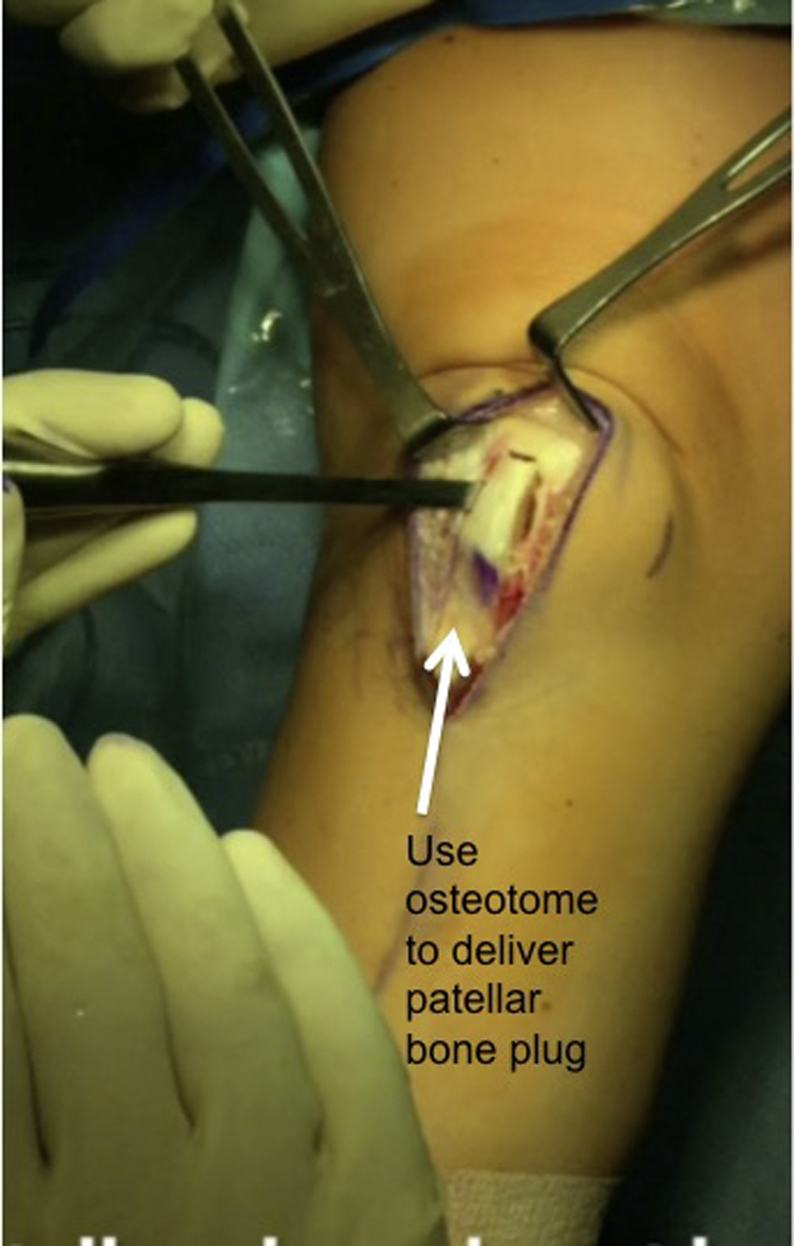
Intraoperative photograph of a patient undergoing left knee anterior cruciate ligament reconstruction showing the use of an osteotome to gently free up the patellar bone plug after an oscillating saw has been used to cut the plug free from the tibia. Care is taken to avoid forceful harvest of the patellar plug to avoid iatrogenic fracture.
Graft Preparation
The BPTB graft can be prepared in a variety of ways. For the most patients, we aim to prepare both bone plugs slightly smaller than 10 mm (an “easy 10”), particularly on the femoral plug, to ensure that the plugs pass easily through the bone tunnels. We typically fashion the femoral plug to be approximately 20 to 22 mm in length, while leaving the tibial plug longer (at least 25 mm), as this plug can be shaved down after final fixation if needed. The bone plugs are trimmed to the appropriate size using any combination of a saw, rongeur, and scissors. Excess bone should be saved to be grafted into the bone plug harvest sites at the end of the case. Sizing tubes are used to confirm that each plug is appropriately sized and will be able to be passed easily through the bone tunnels (Fig 7).
Fig 7.
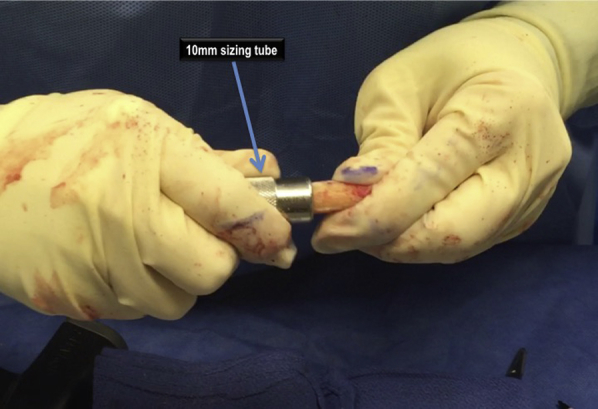
Intraoperative photograph showing bone–patellar tendon–bone autograft preparation in a patient undergoing left knee anterior cruciate ligament reconstruction, ensuring that the bone block can easily fit through the appropriately sized tunnel (in this case, a size 10 for both the tibial and femoral plugs).
A small 0.062-inch K-wire (Stryker) is used to drill 2 holes approximately 5 mm apart in the tibial bone plug in the cancellous part of the plug, parallel to the cortical surface, followed by shuttling a No. 5 high-strength nonabsorbable suture (Ethicon, Somerville, NJ) through each hole. In the femoral plug, only 1 hole is drilled (followed by suture shuttling) to allow the graft to be pulled through the tunnel during graft passing. Alternatively, if using the “push-in” technique, no drill holes or sutures need to be placed through the femoral plug (Fig 8). Finally, the bone-tendon junction of the femoral bone plug is marked with a sterile marking pen, as well as the far end of the tibial plug, which will assist with graft orientation during graft passage and fixation.
Fig 8.
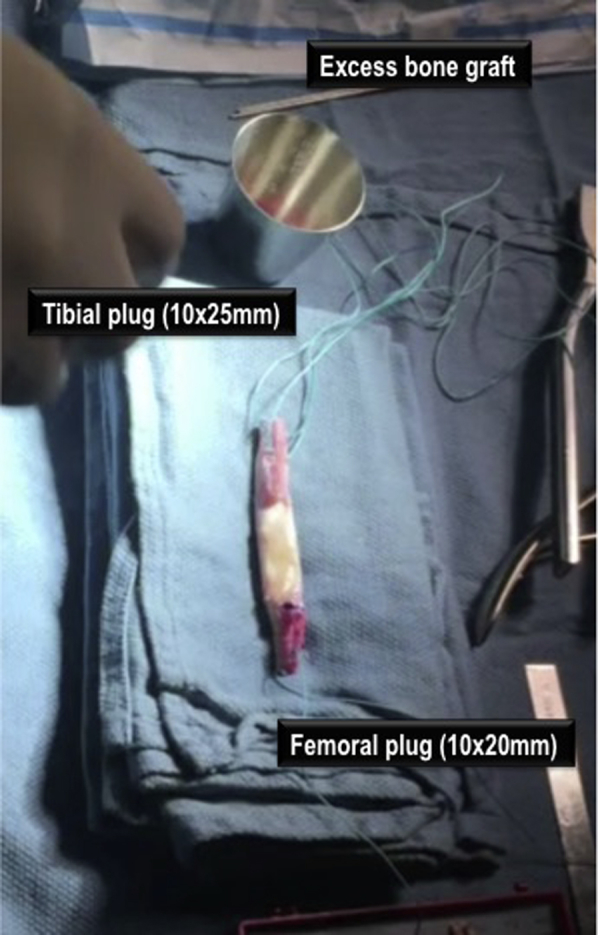
Intraoperative photograph showing final bone–patellar tendon–bone autograft preparation in a patient undergoing left knee anterior cruciate ligament reconstruction.
Closure
After ACLR, bone saved from the bone tunnel reamings and from the back-table graft preparation is used to graft the patellar and tibia bone plug harvest sites, emphasizing the patellar site. The patellar tendon defect is then loosely reapproximated with 2-3 No. 1 Vicryl interrupted sutures (Ethicon) with the knee in flexion, taking care not to overtighten the tendon. Next, the paratenon layer is closed with a running No. 1 absorbable suture (Ethicon) from proximal to distal. The subcutaneous tissue and skin layer are closed in a standard fashion.
Discussion
In this Technical Note, we describe a technique of BPTB autograft harvest and preparation for ACLR. BPTB autografts are considered the preferred graft choice for ACLR in high-level athletes, and offer the advantage of bone to bone integration of the graft versus the soft tissue to bone healing in the setting of ACLR with the hamstring autograft.5 Despite the potential advantages, it is important to recognize the potential complications associated with ACLR with the BPTB autograft, including patella fracture, patella maltracking, anterior knee pain (especially with kneeling), and extensor mechanism complications.3, 4 Anterior knee pain after BPTB harvest may be reduced by bone grafting the patellar and tibial bone plug harvest sites (Table 2).
Table 2.
Pearls and Pitfalls Associated With Bone–Patellar Tendon–Bone Autograft Harvest for ACLR
| Pearls | • Perform examination under anesthesia and confirm diagnosis of ACL tear before harvesting the patellar tendon |
| • Leave at least 10 mm of native patellar tendon medially | |
| • Score the cortex of the tibial and patellar bone plugs before cutting into the bone | |
| • For the horizontal (cross) cut for both the tibial and patellar plug, aim the saw 45° obliquely toward either of the longitudinal cuts, to avoid cutting beyond the longitudinal cuts, thus avoiding the creation of a potential stress riser in the tibial bone | |
| • Anterior knee pain after BPTB harvest may be reduced by bone grafting the patellar and tibial bone plug harvest sites | |
| Pitfalls | • Making skin incision directly in the midline will make it difficult to use that incision for tibial tunnel drilling—ensure that the incision is slightly medial to avoid this problem |
| • Take care not to narrow or widen the second incision relative to the initial incision when harvesting the middle third of the patellar tendon | |
| • Avoid harvesting plugs that are too large (donor site morbidity and more difficult graft preparation) or too small (inadequate graft) | |
| • Avoid mallet use on the patella (or minimize) to avoid iatrogenic patellar fracture |
ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone.
No clinical studies to date have been able to prove consistently superior outcomes after ACLR with one autograft choice over another (Table 3). Data from the MOON group, for example, suggest higher failure rates after ACLR with BPTB allografts versus BPTB autografts, but the authors note no differences when comparing BPTB autografts with hamstring autografts.6 A recent systematic review analyzing 22 studies comparing outcomes after BPTB autograft with quadruple-hamstring autograft found that the BPTB patients might have improved rotational stability compared with hamstring patients, but that hamstring patients have lower rates of postoperative complications.7 Notably, a recent study of 12,643 patients from the Norwegian Cruciate Ligament Registry showed an increased risk of revision ACLR after index reconstruction with hamstring autografts versus BPTB autografts.8 In a 2016 randomized controlled trial comparing the long-term outcomes after hamstring autograft versus BPTB autograft for ACLR, Webster et al.9 found no differences in the rate of graft rupture or contralateral ACL injury at the final follow-up. Importantly, more patients who underwent ACLR with BPTB autograft were participating in sport on a weekly basis compared with patients who received hamstring autograft.
Table 3.
Advantages and Disadvantages Associated With Bone–Patellar Tendon–Bone Autograft Versus Hamstring Autograft Versus Quadriceps Tendon Autograft for ACLR
| Advantages | Disadvantages | |
|---|---|---|
| Patellar tendon | • Gold standard • Better restoration of Lachman, pivot shift, and instrumented laxity testing compared with hamstring autografts • Earlier healing for bone to bone healing |
• Anterior knee pain • Risk of patella fracture • Risk of patellar tendon rupture • Subject to graft-tunnel mismatch (can be avoided with intraoperative adjustments, however) |
| Hamstring | • Less anterior knee pain • Strongest biomechanical graft at time = 0 • More cosmetic • Advantageous for transphyseal ACLR in the pediatric population |
• Potential for small graft diameters (especially in females) • Potential for increased graft laxity over time • Longer healing for soft-tissue to bone |
| Quadriceps | • Large cross-sectional area, can be helpful for revision ACLR in the setting of expanded bone tunnels • Excellent biomechanical strength compared with native ACL • Bone to bone healing on one end, with soft tissue on the other that may be advantageous for transphyseal ACLR in the pediatric population |
• Anterior knee pain • Risk of patella fracture • Risk of patellar tendon rupture • Lack of long-term clinical studies |
ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction.
Overall, given the similar overall outcomes and failure rates for most patients undergoing ACLR with BPTB autograft and hamstring autograft, determining the most appropriate graft for a given patient undergoing ACLR should be based on both patient and surgeon preferences.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Surgical technique for bone–patellar tendon–bone autograft harvest and preparation for use during left knee anterior cruciate ligament reconstruction (ACLR) in a patient.
References
- 1.Mall N.A., Chalmers P.N., Moric M. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42:2363–2370. doi: 10.1177/0363546514542796. [DOI] [PubMed] [Google Scholar]
- 2.Gabler C.M., Jacobs C.A., Howard J.S., Mattacola C.G., Johnson D.L. Comparison of graft failure rate between autografts placed via an anatomic anterior cruciate ligament reconstruction technique: A systematic review, meta-analysis, and meta-regression. Am J Sports Med. 2016;44:1069–1079. doi: 10.1177/0363546515584043. [DOI] [PubMed] [Google Scholar]
- 3.West R.V., Harner C.D. Graft selection in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2005;13:197–207. doi: 10.5435/00124635-200505000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Mohtadi N.G., Chan D.S., Dainty K.N., Whelan D.B. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011:CD005960. doi: 10.1002/14651858.CD005960.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Noyes F.R., Butler D.L., Grood E.S., Zernicke R.F., Hefzy M.S. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am. 1984;66:344–352. [PubMed] [Google Scholar]
- 6.Kaeding C.C., Pedroza A.D., Reinke E.K., Huston L.J., Consortium M., Spindler K.P. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: Prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583–1590. doi: 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xie X., Liu X., Chen Z., Yu Y., Peng S., Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015;22:100–110. doi: 10.1016/j.knee.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 8.Persson A., Fjeldsgaard K., Gjertsen J.E. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: A study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42:285–291. doi: 10.1177/0363546513511419. [DOI] [PubMed] [Google Scholar]
- 9.Webster K.E., Feller J.A., Hartnett N., Leigh W.B., Richmond A.K. Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: A 15-year follow-up of a randomized controlled trial. Am J Sports Med. 2016;44:83–90. doi: 10.1177/0363546515611886. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for bone–patellar tendon–bone autograft harvest and preparation for use during left knee anterior cruciate ligament reconstruction (ACLR) in a patient.


