Abstract
The present study aimed to retrospectively compare the relative rates of mastery of exemplars for individuals with ASD (N = 313) who received home-based and center-based services. A between-group analysis found that participants mastered significantly more exemplars per hour when receiving center-based services than home-based services. Likewise, a paired-sample analysis found that participants who received both home and center-based services had mastered 100 % more per hour while at the center than at home. These analyses indicated that participants demonstrated higher rates of learning during treatment that was provided in a center setting than in the participant’s home.
Keywords: Autism spectrum disorder, Applied behavior analysis, Center-based services, Treatment
There is substantial empirical support for treatments based on applied behavior analysis (ABA) for autism spectrum disorder (ASD; Virués-Ortega, 2010), and researchers have begun to focus on the optimization of specific aspects of behavioral intervention. Individual child outcomes have been shown to vary, which may be due to disparities in intervention variables as well as individual differences. Researchers have employed different tools to measure progress of learning and determine treatment effectiveness or outcomes. These measures include changes in scores on standardized assessments as well as skill mastery (Fava & Strauss, 2014). Treatment variables that have been investigated include child’s age, language skills, intellectual functioning, adaptive functioning, and severity of ASD, as well as treatment intensity and practitioner or teacher training (Fava & Strauss, 2014). However, one variable that has not been studied extensively is whether the setting in which the intervention occurs significantly impacts the child’s rate of learning.
ABA can be delivered in settings such as community centers, homes, and schools, and many children receive ABA therapy across multiple locations. Roberts et al. (2011) found that children receiving services at a center (i.e., child play groups with a concurrent parent support and training program) made more gains than those who received service in their home (i.e., program delivered in the home with the parents), but the procedures and intensity of treatment (i.e., hours per week) differed across the two conditions. Currently, very little research has compared children’s outcomes when practitioners consistently deliver the treatment in both locations.
There are several factors related to a setting that may influence the effectiveness of treatment, including distractors, amount and quality of supervision, and opportunities for socialization and generalization. Certain settings may allow for a more controlled environment while others may contain more distractions. Supervisors may be more available and provide additional direct supervision in center-based settings than in home settings. Lastly, the presence of other individuals with ASD and unfamiliar practitioners may allow for more opportunities for socialization as well as generalization of skills. These represent some aspects of treatment that may differ as a function of location and may ultimately influence a child’s progress.
Due to the variability in both ASD symptom presentation as well as treatment implementation, it is necessary for researchers and practitioners to identify components of treatment that are most likely to optimize results. Given that few researchers have investigated whether location serves as an aspect of treatment that influences learning, the purpose of this study was to conduct a program evaluation to investigate whether children with ASD who had received ABA services learned more skills during home-based services (HBS) or center-based services (CBS). This was done through a retrospective analysis of clinical records comparing the relative rates of mastery of exemplars in each location. Given the potential benefits of treatment delivered in a center setting, we hypothesized that participants would have shown a greater rate of learning per hour during CBS than HBS.
Method
Participants
Pre-existing clinical records were selected from a pool of 804 children who had received behavioral intervention services from a large community-based behavioral health center during a 3-month period (September 1st to November 30th, 2015). Records were selected if they met the following criteria: a diagnosis of ASD (American Psychiatric Association [APA], 2013), autistic disorder (APA, 2000), pervasive developmental disorder, not otherwise specified (PDD-NOS; [APA, 2000]), or Asperger’s disorder (APA, 2000), age between 3 and 12 years old. Of the 358 participants assessed for eligibility, seven were excluded because they did not have an ASD diagnosis and 38 were excluded because they were not within the age range. These criteria resulted in a sample size of 313 individual records. Of these 313 participants, 72 had received CBS (average weekly treatment hours = 16.97, SD = 7.88; average age = 6.68 years, SD = 2.17) and 241 had received HBS (average weekly treatment hours = 13.46, SD = 7.16; average age = 7.22 years, SD = 2.28). See Fig. 1 for the distribution of treatment hours. The age, diagnosis, and gender profiles of the individuals whose clinical records were used in the study were as follows: 276 males (age range 3–12 years, mean age: 7.11 years, 229 autistic disorder, 30 ASD, 15 PDD-NOS, 2 Asperger’s disorder) and 37 females (age range 3–12 years, mean age: 7.0 years, 31 autistic disorder, 3 ASD, 3 PDD-NOS, 0 Asperger’s disorder).
Fig. 1.
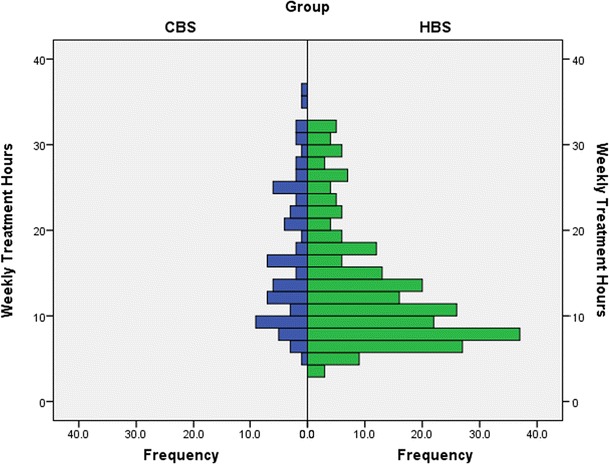
Distribution of weekly treatment hours for CBS and HBS groups
A secondary analysis was conducted to assess for differences in rate of learning within the same individual across both CBS and HBS sessions. For this analysis, only those participants who had received both CBS and HBS sessions were analyzed. This resulted in a sample size of 44 participants: 38 males (age range 3–12 years, mean age: 6.08 years, 31 autistic disorder, 6 ASD, 0 PDD-NOS, 1 Asperger’s disorder) and 6 females (age range 3–9 years, mean age: 6.5 years, 3 autistic disorder, 2 ASD, 1 PDD-NOS, 0 Asperger’s disorder). The average number of weekly treatment hours for these participants was 16.74 (range 6.06–34.58 h, SD = 7.82). Participants in this study resided and received services in the states of AZ, CA, CO, IL, LA, NY, TX, and VA.
Data Collection
Through the course of normal service delivery, practitioners used the Skills™ system to identify treatment targets, plan interventions, and track treatment response. The Skills™ assessment evaluates skills across all areas of development and has been shown to have good internal consistency as well as inter-rater and test-retest reliability (Dixon, Tarbox, Najdowski, Wilke, & Granpeesheh, 2011). Persicke et al. (2014) assessed the validity of the Skills™ Assessment by comparing direct observation and parent response to the Skills™ items and found that Pearson product-moment correlation coefficients ranged from moderate to high (r = .65–.95). These data were integrated with operational information (such as treatment hours) collected by the participating treatment centers.
Treatment
Participants had received one-on-one individualized behavioral intervention by trained behavioral practitioners. Each child’s program had been customized to address the areas of functioning in which the child showed deficits, such as language, social skills, independent living skills, play, academics, motor skills, and executive functioning. All treatment programs were based on the Center for Autism and Related Disorders (CARD) model of treatment (Granpeesheh, Tarbox, Najdowski, & Kornack, 2014), which included the following components: (1) one-on-one treatment was delivered by trained behavioral practitioners, (2) both discrete trial training and natural environment training strategies were used, (3) language intervention used a verbal behavior approach, (4) both errorless and least-to-most prompting strategies were used, (5) research-based behavioral principles and procedures were used (e.g., reinforcement, extinction, stimulus control, generalization training, chaining, and shaping), (6) a function-based approach was employed for the assessment and treatment of challenging behaviors, (7) parents were included in all treatment decisions and received regular training; and 8) direct supervision was given on a regular basis.
Training for behavioral practitioners was multifaceted and included a combination of an eLearning program (www.ibehavioraltraining.com), classroom-style training, field-experience training, and evaluation. Practitioners received supervision from a Board Certified Behavior Analyst (BCBA) monthly or weekly and attended monthly professional development trainings that reviewed treatment procedures. Each participant had a monthly supervised clinic to ensure consistency and generalization across practitioners. Once mastered, programs were put on maintenance to continue to target them in more naturalistic settings to enhance generalization.
Each participant had a team of several practitioners who delivered sessions either in the participant’s home or at the center. There were no explicit differences in treatment across locations (e.g., supervision, targeted skills). Participants were not randomly assigned to center-based or home-based treatment, as the session location was determined by parent preference as well as participant and practitioner availability.
Data Analysis
The independent variable for this study was the location of treatment services (i.e., home or center). The dependent variable for all analyses within this study was rate of mastery of learning objectives, which was calculated as the mean number of learning objectives mastered per hour. Mastery of a learning objective was defined by the treatment supervisor on an individual basis but had to include greater than 70 % accuracy of responding to the learning objective for at least two treatment sessions across two different days. A mastery criterion of 80 % accuracy is often used, but supervisors may deviate from this criterion if they believe it is clinically appropriate. Only mastered objectives from one-on-one discrete trial training sessions were included in this study.
The number of treatment hours and mastered learning objectives ranges over several orders of magnitude, which can result in a large amount of variance. The logarithmic transform was applied to reduce skew caused by this variance, as well as improve the interpretability of the data. Because this variance is due to the data itself, and not outliers, the logarithmic transform was used as it preserves the numerical relationship of variables.
Two separate analyses were run to examine potential differences in rate of mastery across condition. First, an analysis of covariance using group as the fixed factor, age and weekly treatment hours as covariates, was used to compare rate of mastery of all home-based sessions with all center-based sessions over the course of 3 months. The second was a within-subject analysis that was performed only for participants that received both HBS and CBS. This analysis compared within-subject rates of mastery in each location. The purpose of the within-subject analysis was to evaluate whether the results were consistent when the analysis controlled for individual differences (e.g., skill level, ASD symptoms, parent situation and involvement, etc.).
Results
For the first analysis, the covariate, participant age, was not significantly related to the rate of mastery F(1, 309) = 2.696, p = 0.102. The covariate, average weekly treatment hours, was significantly related to the rate of mastery, F(1, 309) = 30.068, p < 0.001. There was also a significant group effect after controlling for the effect of the average weekly treatment hours F(1, 309) = 21.700, p < 0.001. On average, participants mastered more learning objectives per hour of treatment in the CBS group (M = 0.103, SE = 0.016) than in the HBS group (M = 0.053, SE = 0.004). See Fig. 2.
Fig. 2.
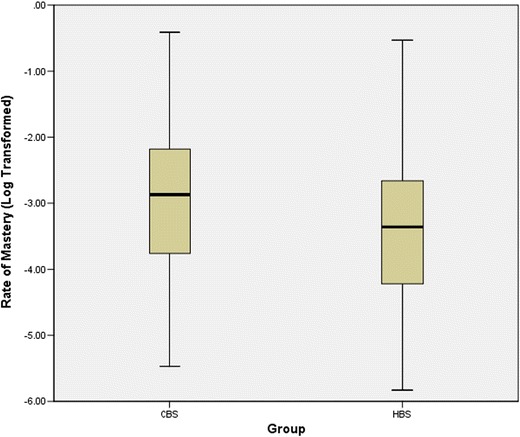
Rate of mastery comparison between service locations: between groups
A secondary analysis was conducted to evaluate differences in the rate of mastery within the same individual across both CBS and HBS sessions. As a group, participants mastered significantly more learning objectives per hour during CBS sessions (M = 0.14, SE = 0.023) than during their HBS sessions (M = 0.07, SE = 0.010). This difference was significant, t(43) = 3.489, p = 0.001 and showed a medium to large effect size (r = 0.47). See Fig. 3.
Fig. 3.
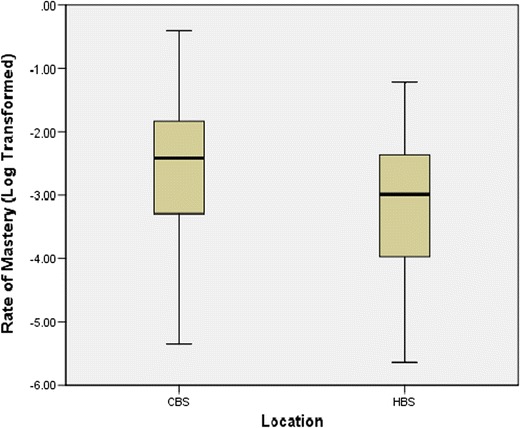
Rate of mastery comparison between service locations: paired samples
Discussion
The analyses for this study were conducted retrospectively using pre-existing clinical records of participants enrolled in ABA services. The results of the current study indicate that as a group, participants had mastered significantly more exemplars when receiving center-based services than home-based services. Also, the average treatment hours received per week, while only differing by 3.5 h between groups, showed a significant impact on the rate of mastery. That is to say that even a slight increase in average treatment hours per week increased the number of mastered learning objectives per hour.
In order to better account for individual differences, we also compared learning within the same participant for those who received both HBS and CBS. The results of this analysis showed that on average, individuals achieved 100 % more learning per hour during CBS relative to HBS. These complimentary analyses suggest that the observed improvements may be due to factors related to service location rather than individual differences (e.g., level of functioning, skills at intake, parental situations, intervention goals, etc.). These results are consistent with those of Roberts et al. (2011), and the current study expanded this research by focusing on one-on-one treatment delivered by trained behavioral practitioners. The findings of this study provide preliminary evidence that a setting may influence rates of learning during treatment.
One argument for favoring home-based sessions over center-based sessions is the idea that parents or caregivers are more likely to participate in treatment sessions if the sessions are located in their home. However, the idea that simple proximity to treatment will improve parent participation is similar to the failed strategy that Stokes and Baer (1977) noted as “train and hope.” In contrast, center-based sessions may provide more structure and a more intentional environment for parents and caregivers to be trained within. Center-based services may allow for more control over the environment and therefore result in a decrease in potential distractors, which may facilitate increased rates of learning.
Another important aspect of CBS is that participants may have the opportunity to interact and generalize social skills with unfamiliar practitioners as well as with peers with ASD who also receive services at the center. Additionally, setting may influence the quality and quantity of supervision. Given the potential association between supervision and participant outcomes (Eikeseth, Hayward, Gale, Gitlesen, & Eldevik, 2009), additional supervision could be considered an advantage of CBS.
Decisions about treatment implementation may often be made based on convenience or availability rather than on how the setting may impact clinical outcomes. Location availability is often limited, as many ABA service providers only offer services either in the home or at a center. This indicates that there may not always be an option regarding location of services. Further, parents or caregivers also may choose the location based on convenience. While these represent practical considerations regarding the delivery of ABA services, these treatment decisions should be based on best-practice guidelines and not simply on convenience. As such, when a child and family are considered to be equally eligible for home-based or center-based services, the results of this study support the recommendation of Roberts et al. (2011) that center-based services may provide better outcomes.
A potential limitation of this study is that these findings represent the CARD model of ABA service delivery (Granpeesheh et al., 2014). While this promotes consistency in ABA delivery across the two conditions of this study, these results may not generalize to other models of ABA service delivery. For example, training methods may differ across different models and agencies. Future researchers would do well to evaluate the effect of service location on ABA outcomes across other models. Additionally, this study used pre-existing clinical records and as such, the treatment location was not randomly assigned. While factors related to individual differences were controlled for by the within-subject analysis, there are additional factors (e.g., time of day of treatment, whether new programs were targeted, generalization opportunities, skills targeted, and amount of supervision) that may have impacted rates of learning.
While the current study provides preliminary evidence for differences in progress between treatment settings, future research should focus on identifying and isolating the variables that may account for these differences. There are many factors related to setting that may impact participants’ progress (e.g., distractors, opportunities for generalization and socialization, level of supervision, access to resources, and proximity to other practitioners). Additional research to evaluate the effects of these variables is warranted.
The general lack of research evaluating the impact of service location is a significant gap in the literature on intervention for ASD. The present study found that participants made significantly more progress in center-based locations compared to home-based location across groups as well as within participants. In light of these results and the absence of other studies, practitioners are encouraged to consider the appropriateness of center-based services when delivering treatment for ASD.
Compliance with Ethical Standards
Informed Consent
The data collected for the present study were from a research database of de-identified archived clinical records. As such, the Institution Review Board (IRB00004971) concluded that 45 CFR part 46 of the U.S. Department of Health and Human Services regulation does not apply.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
This study did not receive external funding.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-5. Arlington, Va: American Psychiatric Association; 2013. [Google Scholar]
- Dixon DR, Tarbox J, Najdowski AC, Wilke AE, Granpeesheh D. A comprehensive evaluation of language for early behavioral intervention programs: the reliability of the SKILLS language index. Research in Autism Spectrum Disorders. 2011;5(1):506–511. doi: 10.1016/j.rasd.2010.06.016. [DOI] [Google Scholar]
- Eikeseth S, Hayward D, Gale C, Gitlesen J-P, Eldevik S. Intensity of supervision and outcome for preschool aged children receiving early and intensive behavioral interventions: a preliminary study. Research in Autism Spectrum Disorders. 2009;3(1):67–73. doi: 10.1016/j.rasd.2008.04.003. [DOI] [Google Scholar]
- Fava L, Strauss K. Response to early intensive behavioral intervention for autism—an umbrella approach to issues critical to treatment individualization. International Journal of Developmental Neuroscience. 2014;39:49–58. doi: 10.1016/j.ijdevneu.2014.05.004. [DOI] [PubMed] [Google Scholar]
- Granpeesheh D, Tarbox J, Najdowski AC, Kornack J. Evidence-based treatment for children with autism: the CARD model. Waltham, MA: Elsevier; 2014. [Google Scholar]
- Persicke A, Bishop MR, Coffman CM, Najdowski AC, Tarbox J, Chi K, et al. Evaluation of the concurrent validity of a skills assessment for autism treatment. Research in Autism Spectrum Disorders. 2014;8(3):281–285. doi: 10.1016/j.rasd.2013.12.011. [DOI] [Google Scholar]
- Roberts J, Williams K, Carter M, Evans D, Parmenter T, Silove N, et al. A randomised controlled trial of two early intervention programs for young children with autism: centre-based with parent program and home-based. Research in Autism Spectrum Disorders. 2011;5(4):1553–1566. doi: 10.1016/j.rasd.2011.03.001. [DOI] [Google Scholar]
- Stokes TF, Baer DM. An implicit technology of generalization. Journal of Applied Behavior Analysis. 1977;10(2):349–367. doi: 10.1901/jaba.1977.10-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virués-Ortega J. Applied behavior analytic intervention for autism in early childhood: meta-analysis, meta-regression and dose–response meta-analysis of multiple outcomes. Clinical Psychology Review. 2010;30(4):387–399. doi: 10.1016/j.cpr.2010.01.008. [DOI] [PubMed] [Google Scholar]


