Abstract
Bucket-handle tears of the meniscus comprise nearly 10% of all meniscus tears and commonly affect the young male population. Displacement of the free segment can lead to significant pain and disability, necessitating reduction and surgical treatment. General contraindications include malalignment, severe arthritis, significant comorbidities, or chronic asymptomatic tears, but otherwise repair should almost always be performed. Options for surgical treatment include partial meniscectomy and arthroscopic repair using an all-inside, outside-in, or inside-out technique. The purpose of this Technical Note is to detail our arthroscopic inside-out repair technique augmented with bone marrow aspirate concentrate.
Bucket-handle meniscal tears present a unique challenge to surgeons due to their complexity and frequency, accounting for up to 10% of all meniscal tears.1 Early diagnosis and repair of bucket-handle tears is crucial. Failure to treat or treatment with meniscectomy can result in earlier progression of osteoarthritis because of loss of tibiofemoral contact area and increased contact pressure across the joint.2 Although medial tears are 3 times more common,3 further difficulties can arise with lateral tears, which may spontaneously reduce, making symptoms intermittent and identification on magnetic resonance imaging less reliable.4, 5, 6 Nonetheless, magnetic resonance imaging has good sensitivity and specificity in the detection of these tears, and their displaced fragments.7 Consistent imaging signs with good sensitivity include a double posterior cruciate ligament sign, a double anterior horn meniscus sign, and/or a fragment in the intercondylar notch.8
Surgical repair can restore near intact biomechanics,9 with several techniques described for the repair of bucket-handle tears including all-inside, inside-out, and outside-in techniques.10 The purpose of this Technical Note is to describe the procedure for inside-out repair of a post-traumatic meniscus bucket-handle tear.
Operative Indications
Patients with significant malalignment in the ipsilateral compartment should have consideration for concomitant alignment correction surgery.11 Furthermore, patients with significant comorbidities, severe arthritis (grade 3 or 4 chondromalacia), or asymptomatic chronic bucket-handle tears should not undergo repair.12, 13 Outside of these contraindications, anatomical repair of the bucket-handle tear should almost always be performed.
Patient Positioning and Anesthesia
The patient is placed in the supine position on the operating table. After induction of general anesthesia, a bilateral knee examination is performed to evaluate for any concurrent ligamentous instability and to assess for knee range of motion (ROM). However, during the physical examination, caution must be exercised to prevent further tearing of the meniscus and allow for adequate reduction and subsequent repair. A well-padded high-thigh tourniquet is subsequently placed on the operative leg, which is then placed into a leg holder (Mizuho OSI, Union City, CA), whereas the contralateral knee is placed into an abduction stirrup (Birkova Product LLC, Gothenburg, NE). The leg holder should be placed proximal enough to allow exposure for an inside-out meniscal repair. The foot of the operating table is then lowered, allowing the surgeon to freely manipulate the knee as needed.
Surgical Technique
A detailed description of the technique is shown in Video 1. Pearls and pitfalls of this technique and a step-by-step approach are described in Tables 1 and 2, respectively.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Correct portal placement is vital for improved visualization | Misplacement of the portals can make the repair challenging |
| Slight changes in the position of the knee might facilitate reduction of the bucket-handle tear | Do not force the reduction if there is not sufficient space for the bucket handle to be reduced underneath the femoral condyle; consider trephination of the medial collateral ligament with a spinal needle to create enough space to reduce the meniscal tear |
| A blunt instrument is used to help reduce the bucket-handle tear | Do not use sharp instruments to reduce the meniscus because it might create a radial tear |
| Multiple inside-out vertical mattress sutures should be placed to secure the meniscus | Avoid tying the sutures around the popliteal retractor |
| Extensive probing should be performed to ensure the strength of the construct after repair |
Table 2.
Sequential Steps Inside-Out Meniscal Repair
| Medial Repair | Notes |
|---|---|
| Diagnostic arthroscopy | Standard anterolateral and anteromedial portals |
| Granulation tissue debridement of tear | 4.5-mm shaver |
| Posteromedial vertical incision | 4 cm length, 2/3 distal, 1/3 proximal to the joint line |
| Dissection through the oblique sartorius fascia | Proximal to distal using Metzenbaum scissors |
| Retraction of sartorius, gracilis, semitendinosus | Protect the saphenous nerve |
| Placement of a popliteal retractor | Interval between the medial gastrocnemius and joint capsule |
| Suture cannula directed through the anterolateral portal | Valgus force, knee at 10° to 20° of flexion |
| Needle retrieval | Flex to 70° to 90° |
| Second needle placed adjacent to the first | Keep slight tension to avoid suture puncture/laceration |
| Continue suture placement posterior to anterior | Placement 3 to 5 mm apart |
| Cut needles and tag sutures with hemostat or tie immediately | Avoid overtensioning to prevent puckering |
| Thoroughly irrigate wound | – |
| Close in a standard layered fashion | – |
| Lateral Repair | Notes |
|---|---|
| Lateral vertical skin incision | 2.5 to 4 cm, posterior to the FCL |
| Deep transverse oblique incision from posterior ITB to Gerdy's | Stay anterior to the biceps tendon to avoid the peroneal nerve |
| Superficial ITB incision 5 mm anterior to the posterior margin | Avoid injury to the FCL and deep lateral capsule |
| Placement of a retractor | Interval between the lateral gastrocnemius and joint capsule |
| Suture cannula directed through the anteromedial portal | Varus force, knee at 10° to 20° of flexion |
FCL, fibular collateral ligament; ITB, iliotibial band.
Inside-Out Meniscus Repair
The patient is placed in a supine position with the knee distal to the break in the table, which allows for easier access to the posteromedial or posterolateral knee when the foot of the table is flexed (Fig 1). An initial diagnostic arthroscopy is performed with traditional anterolateral and anteromedial portals. After the anterolateral arthroscopic portal is made, the anteromedial portal is made with the aid of a spinal needle to optimize its position. Creating additional portals or switching the viewing and working portals may be necessary to access posterior tears. It is often beneficial to debride a portion of the retropatellar fat pad to improve instrument access and passage.
Fig 1.
Intraoperative photograph showing the knee position in the operating suite. The patient is placed in a supine position with a well-padded high-thigh tourniquet placed on the operative leg (left), which is then placed into a leg holder, whereas the contralateral knee is placed into an abduction stirrup. The foot of the bed is lowered to allow the operative leg to hang freely within the surgical field.
Meniscus tear preparation is the next step, and this should not be overlooked to achieve a successful repair. Granulation tissue debridement on both sides of the tear is performed with a 4.5-mm shaver. Taking the time to debride the granulation tissue and meniscal edges is crucial for maximizing the healing response at the tear site. In the setting of a displaced bucket-handle tear (Fig 2), access to and preparation of the posterior meniscal edge can often be easier with the meniscal fragment displaced anteriorly. Once the repair bed is prepared, the meniscus is reduced into its appropriate anatomic position with the use of a probe, camera trochar, or other suitable instrument (Fig 3).
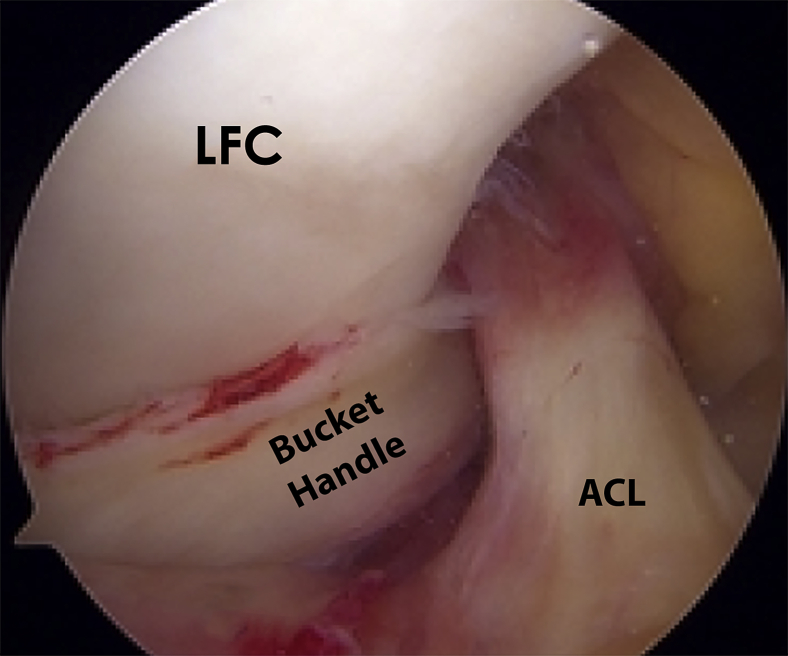
Fig 2.
The arthroscopic image shows a right knee with a bucket-handle tear of the lateral meniscus as viewed from the anterolateral portal and the knee at 90° of flexion. Subsequent debridement of the remnant meniscus edge is performed to maximize the healing response. In this picture, the displaced fragment of the lateral meniscus can be seen within the intercondylar femoral notch, adjacent to the ACL. (ACL, anterior cruciate ligament; LFC, lateral femoral condyle.)
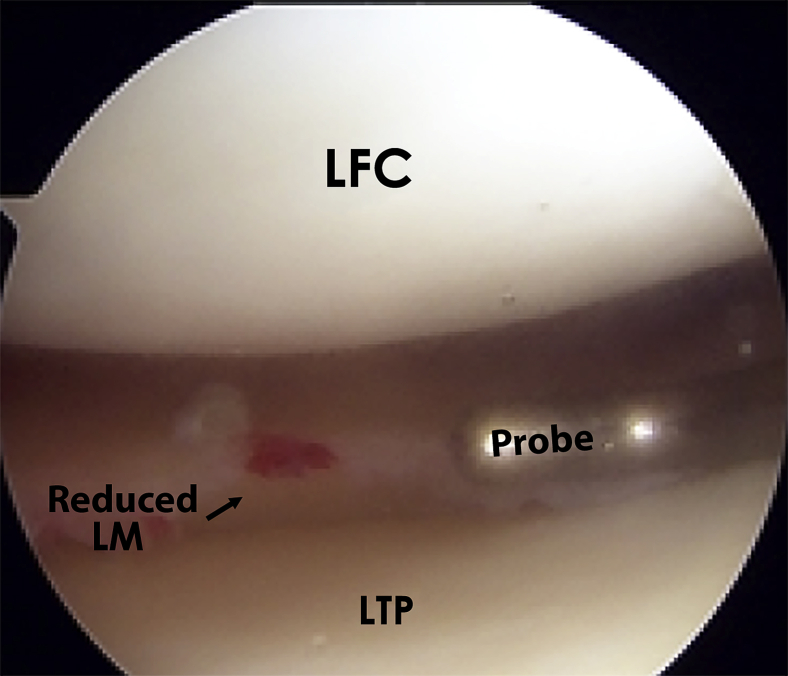
Fig 3.
Arthroscopic images of a right knee viewed through the anterolateral portal with the probe inserted through the anteromedial portal. Once the meniscus tear preparation and debridement is complete, the next step is to reduce the meniscus into its appropriate anatomic position. Here, reduction is achieved with the use of a probe. (LFC, lateral femoral condyle; LM, lateral meniscus; LTP, lateral tibial plateau.)
Medial Approach
After tear preparation, a posteromedial incision is made. Incision placement may be facilitated by transillumination of the medial compartment and/or by palpation with a probe placed along the medial joint line. Transillumination also helps visualize the saphenous vein. An approximately 4-cm incision is made posterior to the superficial medial collateral ligament. Because the suture needles often angle downward as they exit the joint capsule, it is helpful to have two-thirds of the incision distal to the joint line with one-third proximal.
The approach is made with the knee in flexion. The oblique sartorius fascia should be identified as one dissects deep to the subcutaneous tissue. By the use of Metzenbaum scissors, the anterior fascia should be dissected distal to proximal. The sartorius, gracilis, and semitendinosus tendons should be retracted to protect the saphenous nerve, which lies posteromedial to the tendons. On deeper dissection, one should identify the interval between the medial head of the gastrocnemius and the joint capsule, remaining proximal to the semimembranosus tendon. The muscle of the gastrocnemius can be bluntly dissected off the capsule using a pair of Metzenbaum scissors, followed by using a blunt key elevator. The surgeon's finger may be useful to aid in the separation of the muscle from the capsule. Working distal to proximal facilitates the dissection of the gastrocnemius off of the posterior capsule. A popliteal retractor is placed within this plane, which will serve to retract and protect the neurovascular structures located lateral to the medial head of the gastrocnemius. We prefer to use a large spoon in this capacity. The retractor should be held so that the needles piercing the posterior capsule are deflected medially toward the assistant. Keeping the knee in 20° to 60° of flexion relaxes the hamstrings and medial gastrocnemius, which improves visualization of the needles as they exit the posterior capsule.
Lateral Approach
With the knee in 90° of flexion, a 2.5-cm to 4-cm vertical skin incision is made posterior to the fibular collateral ligament. After locating the joint line with the use of an arthroscopic probe, a transverse oblique incision is performed following the posterior border of the iliotibial band (ITB) down to Gerdy's tubercle and centered over the lateral joint line. It is important to stay anterior to the biceps tendon because the peroneal nerve is located posteromedial to the biceps femoris tendon. The superficial layer of the ITB is then incised along its posterior aspect. Care must be taken when making this incision to avoid injury to the fibular collateral ligament and deep lateral capsule. The incision through the ITB is positioned approximately 5 mm anterior to the posterior margin of the superficial layer of the ITB. Blunt dissection must be performed (from the ITB window accessed in the previous step) toward the fibular head and proximal to the long and short heads of the biceps tendon.
The next interval lies between the lateral head of the gastrocnemius (superiorly) and the posterolateral joint capsule (anteriorly). The lateral gastrocnemius muscle can be bluntly dissected off the capsule and verified in the same manner as the medial repair. A retractor within this plane will serve to retract and protect the neurovascular structures located medial to the lateral head of the gastrocnemius, as well as the peroneal nerve, which will lie on the posterior side of the biceps tendon. The retractor should be held so that the needles piercing the posterior capsule are deflected laterally toward the assistant.
Meniscal Repair
A commercially available device (SharpShooter, Ivy Sports Medicine, Montvale, NJ) is used to place sutures (No. 2 Ethibond) into the meniscus. For medial meniscus tears, entry from the anterolateral portal decreases the risk of damaging the reflected neurovascular structures and optimizes the direction of the needle as it exits the capsule. The reverse is true for lateral meniscus tears. If the initial anterior portals are not optimal to access the posterior horn of the meniscus, one should create an additional portal at a more accessible position with the aid of a spinal needle. With the surgeon applying a valgus force to the joint for medial tears and a varus force for lateral meniscal tears, the cannula is directed toward the tear under arthroscopic visualization. One should place the suture cannula in the desired location at the tear site and pass the tip of the needle just past the end of the cannula to visualize its exact entry point into the meniscus or capsule.
The surgeon places the knee in 10° to 20° of flexion and the needle is passed through the meniscus. Once the needle is through the posterior capsule, flexing the knee to 70° to 90° assists in needle retrieval. The cannula is then redirected to deliver the second needle and place the suture adjacent to the first. It is important to keep slight tension on the suture to avoid inadvertent puncture or laceration of the suture with the second needle. The second suture is placed similarly to the first to create a vertical, oblique, or horizontal pattern. One must pay particular attention when placing the needle through the more central meniscus segment and then continuing into the peripheral segment or capsule that anatomic reduction is maintained. If possible, a vertical suture pattern is preferred because it allows for greater capture of the strong circumferential fibers of the meniscus; however, oblique and horizontal patterns are often used as well for complex meniscal tears. An assistant should be prepared to retrieve the suture needle using a needle driver and optimal lighting to visualize the needle's delivery through the posterior capsule. As the needle tip is visualized, the assistant often has to bend the needle to deliver the 25.4-cm needle. Sutures are typically placed from posterior to anterior; however, if there is difficulty visualizing the first needle, an anterior suture may be placed because it is typically easier to locate and can help to guide the expected delivery location of subsequent posterior sutures.
In a similar fashion, multiple sutures are placed between 3 and 5 mm apart (Fig 4). For tears at the meniscocapsular junction, often the first needle is passed through the meniscus and the second just through the capsule adjacent to the tear. Both femoral- and tibial-sided sutures may be placed. Typically, femoral-sided sutures are placed first. Sometimes, this will create a “puckering” of the meniscus superiorly and resultant gapping of the tear on the tibial side. This should be reduced with tibial-sided sutures placed in a similar fashion. One of the benefits of the inside-out repair technique is that the needle diameters are smaller than those for all-inside devices, which allows for the passage of a greater number of sutures and fixation points without creating as much iatrogenic damage to the meniscus tissue.
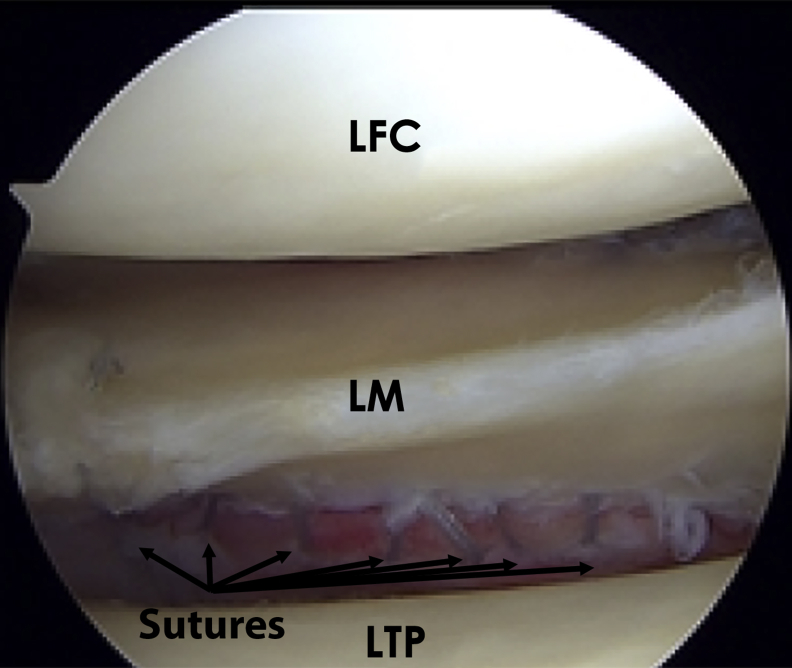
Fig 4.
The arthroscopic image shows a right knee with a bucket-handle tear of the lateral meniscus as viewed from the anterolateral portal. For lateral meniscus tears, entry of the repair device is through the anteromedial portal. If possible, a vertical suture (No. 2 Ethibond) pattern is preferred because it allows for greater capture of the strong circumferential fibers of the meniscus. Multiple sutures are placed between 3 and 5 mm apart (arrows). (LFC, lateral femoral condyle; LM, lateral meniscus; LTP, lateral tibial plateau.)
As the assistant delivers the needles and sutures, the needle is cut off, and the sutures are tagged with a hemostat. The hemostats can be kept in order by placing them in an Alice clamp. Either sutures can be tied immediately or several sutures can be clamped and tied as a group. It is important not to overtighten the sutures. At the end of the procedure, the wound is thoroughly irrigated and closed in a standard layered fashion.
Bone Marrow Aspirate Concentrate
The left posterior iliac crest is identified and sterilely prepped and draped. Six milliliters of 1% lidocaine local anesthetic is injected into the skin and down to the periosteum over the desired bone marrow aspirate concentrate (BMAC) harvest site. The bony landmarks are palpated and a bone marrow aspiration trochar and needle assembly are percutaneously inserted through the skin and subcutaneous tissue until it reaches the posterior iliac crest. The trochar is then inserted centered between the outer and inner walls of the iliac crest. Then a power instrument is used to advance the trochar through the dense cortical bone into the medullary cavity of the posterior iliac crest. Before aspiration, 1 mL of Anticoagulant Citrate Dextrose Solution, Solution A, is preloaded into the syringe and injected into the trochar. Approximately 50 to 60 mL of bone marrow is aspirated. The BMAC aspiration sample is then processed after it is harvested. The bone marrow aspirate is placed in a centrifuge and spun at a rate of 3,200 revolutions per minute for 15 minutes. Typically, a 6 mL sample of BMAC is obtained after processing. The BMAC is subsequently injected intra-articularly (Fig 5).
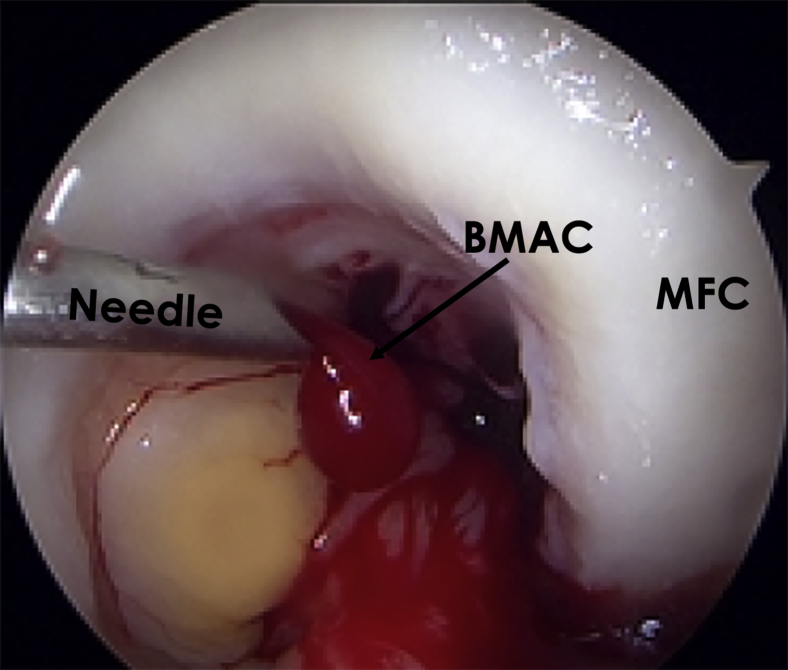
Fig 5.
The arthroscopic image shows a right knee as viewed from the anteromedial portal while injecting through the anterolateral portal. Once the meniscus is repaired, a 6 cc sample of BMAC is injected within the joint to maximize healing potential and increase the number of growth factors and progenitor cells in the intra-articular environment. (BMAC, bone marrow aspirate concentrate; MFC, medial femoral condyle.)
Postoperative Rehabilitation
After surgery, the patient is non-weight-bearing for 6 weeks with crutches and a knee immobilizer. Passive ROM exercises are initiated on postoperative day 1 with motion restricted to 90° of flexion for the first 2 weeks, and then progressed as tolerated. During the first 6 weeks, the patient's primary exercises are patellar mobilizations, passive knee ROM, and quadriceps activation exercises. Patients are permitted to begin weaning off crutches at 6 weeks. Once they are full weight bearing, patients begin closed chain strengthening exercises with training periodization focused on first developing muscular endurance, followed by strength and power. Deep squatting and sitting cross-legged should be avoided until at least 4 months postoperatively. Patients may begin running exercises at 3 months, with initiation of speed and agility drills at 4 months. In our practice, gradual return to play progression is initiated after 4 months after the successful completion of a functional sports test. Return to sports or activity is allowed when normal strength, stability, and knee ROM comparable with the contralateral side; this typically occurs at 4 to 5 months postoperatively.
Discussion
This Technical Note describes our surgical technique for the treatment of a reparable bucket-handle tear of the meniscus. Reduction and repair of a bucket-handle meniscus tear can be difficult, particularly if the meniscal segment has been degenerated between the time of injury and surgery. Furthermore, bucket-handle tears can lead to significant pain and dysfunction if the segment has displaced into the intercondylar notch, necessitating prompt reduction and treatment.
A bucket-handle tear is a longitudinal, full-thickness tear, which is reported to comprise almost 10% of all meniscus tears.1 This type of tear pattern is commonly seen in younger (<40 years old) male patients and is most often (72%) located in the peripheral portion of the menisci.1 In addition, medial meniscus bucket-handle tears frequently accompany anterior cruciate ligament injury, emphasizing the need for a thorough physical and arthroscopic examination.
The prognosis after meniscal injury is highly variable depending on the size and location of the tear. Furthermore, healing rates are reported to be up to 87% and 59% for the peripheral and central-thirds, respectively, in patients who underwent a meniscal repair in the setting of an anterior cruciate ligament reconstruction.14 An increased concern for the preservation of meniscal tissue, particularly regarding its role in knee stability, contact forces, and preventing degenerative changes,15, 16 has led to a trend of fewer reported meniscal procedures but an increase in meniscal repair cases over the last decade.17 In addition, new arthroscopic devices allow for meniscal repairs to be performed with less invasiveness and decreased surgical time.18
Several treatment options are available for meniscus preservation, including all-inside, outside-in, and inside-out techniques. The all-inside and outside-in techniques provide better access to the posterior and anterior horns of the menisci, respectively, whereas the inside-out technique is typically used to repair peripheral tears between 1 and 4 cm in length. A recent systematic review reported similar functional outcomes, failure rates, and complications between inside-out and all-inside repairs of isolated meniscus tears.19 In our opinion, the inside-out technique provides the most stable repair of bucket-handle tear patterns. Although repair is attempted whenever possible, a tear located in the avascular zone, a tear with associated degenerative changes, inability of anatomic reduction, or deformation of the torn segment may be indications for partial meniscectomy.20
Another possible adjunct to meniscal repair is the injection of biologic factors. Laboratory studies evaluating the effect of augmentation with fibrin clot, platelet-rich plasma, and growth factors after meniscal repair have been promising, although clinical outcomes are still lacking. Our technique combines the meniscal repair with application of BMAC. Despite containing a limited number of stem cells, BMAC serves as a source of growth factors that are thought to play an important role because of their anabolic and anti-inflammatory effects. A high concentration of growth factors, including platelet-derived growth factor, transforming growth factor-β, and bone morphogenetic proteins-2, -7, which are reported to have anabolic and anti-inflammatory effects, are contained within BMAC. BMAC has been shown to be a safe regenerative therapy with good results, but most studies report its efficacy in the treatment of osteoarthritis and focal chondral defects.21, 22 The efficacy of different biologics cannot be compared, because BMAC has been reported to have a significantly different cellular and cytokine composition than platelet-rich plasma, warranting further investigation and comparison of these biologics in meniscal injury and repair.23
In conclusion, we recommend our described technique for the treatment of reparable bucket-handle tears to better preserve the kinematics and prevent early degeneration of the tibiofemoral joint. Nevertheless, future long-term studies with large sample sizes are required to assess the efficacy of repair augmented with BMAC in the setting of isolated bucket-handle tears.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.F.L. receives support from Arthrex, Ossur, and Smith & Nephew; receives consultancy fees and royalties from Arthrex, Smith & Nephew, and Ossur; and has grants/grants pending from Health East and NIH R-13 grant for biologics and patents from Ossur and Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The video details our technique for medial and lateral inside-out repairs of bucket-handle meniscus tears. The first part of the video shows on a cadaveric specimen the posteromedial and posterolateral approaches required for inside-out suture retrieval. The arthroscopic footage that follows is of a male right knee viewed through an anteromedial portal. An inside-out repair of a medial bucket-handle tear is performed using 18 sutures and augmented with bone marrow aspirate concentrate.
References
- 1.Metcalf M.H., Barrett G.R. Prospective evaluation of 1485 meniscal tear patterns in patients with stable knees. Am J Sports Med. 2004;32:675–680. doi: 10.1177/0095399703258743. [DOI] [PubMed] [Google Scholar]
- 2.Krause W.R., Pope M.H., Johnson R.J., Wilder D.G. Mechanical changes in the knee after meniscectomy. J Bone Joint Surg Am. 1976;58:599–604. [PubMed] [Google Scholar]
- 3.Johnson M.J., Lucas G.L., Dusek J.K., Henning C.E. Isolated arthroscopic meniscal repair: A long-term outcome study (more than 10 years) Am J Sports Med. 1999;27:44–49. doi: 10.1177/03635465990270011501. [DOI] [PubMed] [Google Scholar]
- 4.Breitenseher M.J., Trattnig S., Dobrocky I. MR imaging of meniscal subluxation in the knee. Acta Radiol. 1997;38:876–879. doi: 10.1080/02841859709172428. [DOI] [PubMed] [Google Scholar]
- 5.Makdissi M., Eriksson K.O., Morris H.G., Young D.A. MRI-negative bucket-handle tears of the lateral meniscus in athletes: A case series. Knee Surg Sports Traumatol Arthrosc. 2006;14:1012–1016. doi: 10.1007/s00167-005-0011-8. [DOI] [PubMed] [Google Scholar]
- 6.Suganuma J., Mochizuki R., Inoue Y., Yamabe E., Ueda Y., Kanauchi T. Magnetic resonance imaging and arthroscopic findings of the popliteomeniscal fascicles with and without recurrent subluxation of the lateral meniscus. Arthroscopy. 2012;28:507–516. doi: 10.1016/j.arthro.2011.08.311. [DOI] [PubMed] [Google Scholar]
- 7.Dunoski B., Zbojniewicz A.M., Laor T. MRI of displaced meniscal fragments. Pediatr Radiol. 2012;42:104–112. doi: 10.1007/s00247-011-2231-z. [DOI] [PubMed] [Google Scholar]
- 8.Magee T.H., Hinson G.W. MRI of meniscal bucket-handle tears. Skeletal Radiol. 1998;27:495–499. doi: 10.1007/s002560050426. [DOI] [PubMed] [Google Scholar]
- 9.Baratz M.E., Fu F.H., Mengato R. Meniscal tears: The effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14:270–275. doi: 10.1177/036354658601400405. [DOI] [PubMed] [Google Scholar]
- 10.Grant J.A., Wilde J., Miller B.S., Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: A systematic review. Am J Sports Med. 2012;40:459–468. doi: 10.1177/0363546511411701. [DOI] [PubMed] [Google Scholar]
- 11.Chahla J., Moulton S.G., LaPrade C.M., Dean C.S., LaPrade R.F. Posterior meniscal root repair: The transtibial double tunnel pullout technique. Arthrosc Tech. 2016;5:e291–e296. doi: 10.1016/j.eats.2016.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhatia S., LaPrade C.M., Ellman M.B., LaPrade R.F. Meniscal root tears: Significance, diagnosis, and treatment. Am J Sports Med. 2014;42:3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 13.Moon H.K., Koh Y.G., Kim Y.C., Park Y.S., Jo S.B., Kwon S.K. Prognostic factors of arthroscopic pull-out repair for a posterior root tear of the medial meniscus. Am J Sports Med. 2012;40:1138–1143. doi: 10.1177/0363546511435622. [DOI] [PubMed] [Google Scholar]
- 14.Asahina S., Muneta T., Yamamoto H. Arthroscopic meniscal repair in conjunction with anterior cruciate ligament reconstruction: factors affecting the healing rate. Arthroscopy. 1996;12:541–545. doi: 10.1016/s0749-8063(96)90191-7. [DOI] [PubMed] [Google Scholar]
- 15.Fairbank T.J. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30:664–670. [PubMed] [Google Scholar]
- 16.Montgomery S.R., Zhang A., Ngo S.S., Wang J.C., Hame S.L. Cross-sectional analysis of trends in meniscectomy and meniscus repair. Orthopedics. 2013;36:e1007–e1013. doi: 10.3928/01477447-20130724-15. [DOI] [PubMed] [Google Scholar]
- 17.Parker B.R., Hurwitz S., Spang J., Creighton R., Kamath G. Surgical trends in the treatment of meniscal tears: Analysis of data from the american board of orthopaedic surgery certification examination database. Am J Sports Med. 2016;44:1717–1723. doi: 10.1177/0363546516638082. [DOI] [PubMed] [Google Scholar]
- 18.Sgaglione N.A. Meniscus repair update: Current concepts and new techniques. Orthopedics. 2005;28:280–286. doi: 10.3928/0147-7447-20050301-13. [DOI] [PubMed] [Google Scholar]
- 19.Fillingham Y.A., Riboh J.C., Erickson B.J., Bach B.R., Jr., Yanke A.B. Inside-out versus all-inside repair of isolated meniscal tears. Am J Sports Med. 2017;45:234–242. doi: 10.1177/0363546516632504. [DOI] [PubMed] [Google Scholar]
- 20.Weiss C.B., Lundberg M., Hamberg P., DeHaven K.E., Gillquist J. Non-operative treatment of meniscal tears. J Bone Joint Surg Am. 1989;71:811–822. [PubMed] [Google Scholar]
- 21.Shapiro S.A., Kazmerchak S.E., Heckman M.G., Zubair A.C., O'Connor M.I. A prospective, single-blind, placebo-controlled trial of bone marrow aspirate concentrate for knee osteoarthritis. Am J Sports Med. 2017;45:82–90. doi: 10.1177/0363546516662455. [DOI] [PubMed] [Google Scholar]
- 22.Chahla J., Dean C.S., Moatshe G., Pascual-Garrido C., Serra Cruz R., LaPrade R.F. Concentrated bone marrow aspirate for the treatment of chondral injuries and osteoarthritis of the knee: A systematic review of outcomes. Orthop J Sports Med. 2016;4 doi: 10.1177/2325967115625481. 2325967115625481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cassano JM, Kennedy JG, Ross KA, Fraser EJ, Goodale MB, Fortier LA. Bone marrow concentrate and platelet-rich plasma differ in cell distribution and interleukin 1 receptor antagonist protein concentration [published online February 1, 2016]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-3981-9. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The video details our technique for medial and lateral inside-out repairs of bucket-handle meniscus tears. The first part of the video shows on a cadaveric specimen the posteromedial and posterolateral approaches required for inside-out suture retrieval. The arthroscopic footage that follows is of a male right knee viewed through an anteromedial portal. An inside-out repair of a medial bucket-handle tear is performed using 18 sutures and augmented with bone marrow aspirate concentrate.