Abstract
Acromioclavicular (AC) joint instability is a fairly common and particularly limiting injury that may result in persistent pain and reduced quality of life. In most cases, conservative management is successful. However, in the case of a severe AC joint dislocation, surgical intervention may be warranted. Previous surgical techniques for treatment of AC joint instability include screw fixation between the coracoid and clavicle, coracoacromial ligament transfer from its acromial insertion to the clavicle, and reconstruction of the coracoacromial and/or coracoclavicular ligaments. The purpose of this Technical Note is to describe our preferred technique for the treatment of a high-grade AC dislocation through coracoacromial ligament transfer to the lateral clavicle and nonabsorbable suture fixation between the coracoid process and clavicle.
Acromioclavicular (AC) joint dislocations are relatively common and particularly disabling injuries of the shoulder, often affecting male athletes who participate in a contact sport. In fact, the estimated overall incidence of AC joint injuries is 9.2 per 1,000 person-years in young athletes.1 Although almost 90% of these injuries are low grade (Rockwood grade I or II), high-grade injuries may result in chronic pain, persistent muscular weakness, aesthetical deformity of the clavicle, and an overall reduced quality of life.2 The mechanism of injury is usually described as a direct force to the acromion if the patient falls with the arm in adducted position. However, in the case of an indirect force, the patient may fall onto the elbow, which results in a force vector that pushes the proximal humerus against the AC joint and leads to an AC dislocation.2
To accurately and consistently diagnose an AC dislocation, a thorough physical examination and a set of imaging examinations must be completed. In the acute setting, the patient may often complain of pain directly over the AC joint. Moreover, a visible deformity of the joint may be present especially in cases of Rockwood's grades III and V. After the physical examination, a series of radiographs must be completed including a shoulder trauma series3, 4 as well as the Zanca view, which is reported to be the most accurate view for examination of the AC joint.5 Furthermore, the anteroposterior view may be used to identify any vertical displacement of the clavicle, whereas the axillary view would be particularly useful in the case of a posterior dislocation. In the setting of a more complex case, computed tomography may be required for better assessment of fractures as well as the articular surfaces, whereas magnetic resonance imaging may be used to eliminate possible concomitant pathologies including associated ligamentous and cartilaginous injuries.4, 6 The purpose of this Technical Note is to describe our preferred technique for the treatment of a high-grade AC dislocation through coracoacromial ligament (CAL) transfer to the lateral clavicle and nonabsorbable suture fixation between the coracoid process and clavicle.
Surgical Technique
Preoperative Setup and Examination Under Anesthesia
The patient is positioned supine on the operating table and regional anesthesia is then applied by way of an interscalene block. In our experience, the initial use of regional anesthesia reduces immediate postoperative pain and allows the patient to effectively abide with the proposed rehabilitation protocol. After induction of general anesthesia, the patient is transferred to a beach chair position to optimize shoulder mobility during the procedure. Using a foam pad, the knees are kept in slight flexion and all bony prominences are well padded. The head is then checked to confirm that it is secured in position. After this, safety straps are used to fasten the patient to the operating table. Once the preoperative setup is complete, a physical examination of the shoulder is performed. The physical examination spans the following tests: range of motion of both shoulders, palpation of the AC joint, and ease of reducibility of the clavicle through application of superoinferior pressure onto the lateral pole of the clavicle. After examination under anesthesia, the nonoperative arm is maintained in adduction with a neutral position. Afterward, the left arm is sterilely prepped and draped in standard fashion while the arm is kept adducted and next to the body. All relevant bony prominences on the shoulder are identified via palpation, and then a surgical pen is used to outline the acromion, clavicle, and coracoid process to avoid unnecessary surgical exposure of any surrounding structures.
Exposure
Once the patient is in the correct position, the initial incision is completed based on Langer's lines to provide a more cosmetic scar. The incision is first marked, beginning at the coracoid process and extending to the most proximal aspect of the clavicle to ensure a good overall exposure of the AC and coracoclavicular joint space. A scalpel is then used to perform the longitudinal incision (Fig 1). After this, the subcutaneous tissue is bluntly dissected. The deltotrapezoidal fascia is exposed and opened in line with the skin incision through the use of Metzenbaum scissors. The superior and anterior aspects of the clavicle are then exposed with a coagulator, Cobb elevator, or Penfield dissector (Fig 2). It is important to maintain the integrity of all surrounding soft tissues that will be approximated later on in the procedure. Maintenance of these soft tissues ensures adequate soft tissue coverage of the sutures as well as proximal deep structures. In addition, the coagulator is used to demarcate the AC joint while releasing the lateral border of the clavicle from all previous scar tissues formed in the AC joint in a chronic setting. Then, attention is turned to the CAL. For this portion of the technique, thorough knowledge of the anatomy of the AC joint including the CAL and other surrounding structures is necessary. Metzenbaum scissors are used to carefully identify and isolate the CAL with care to avoid damage to all nearby structures.
Fig 1.
The patient is positioned in a beach chair position with the left arm prepped in a standard fashion. The coracoid process, acromion, and clavicle are palpated and marked using a surgical pen. Based on Langer's lines, a line is drawn from the coracoid process to the clavicle (A). A scalpel is then used for the surgical approach (B), starting at the coracoid process and extending to the superior border of the clavicle.
Fig 2.
The surgical approach for exposure of the acromioclavicular joint in the left shoulder is completed. Once the skin is incised, blunt dissection of the subcutaneous tissue is performed using Metzenbaum scissors (A). The deltotrapezoidal fascia is incised in line with the skin incision. Then, the superior and anterior aspect of the clavicle is exposed with release of all surrounding soft tissue (B). After this, exposure of the coracoacromial ligament (CAL) is completed (C).
Release of the CAL From the Acromial Insertion
Once the CAL is sufficiently exposed, sharp dissection is performed on the acromial insertion of the CAL using a scalpel (Fig 3). For dissection of this portion of the technique, we recommend the use of a scalpel, instead of Metzenbaum scissors or a coagulator. Once the CAL is released from the lateral portion, a No. 5 Ethibond suture (Ethicon, Somerville, NJ) is used to prepare this end of CAL using the Kessler suture technique.
Fig 3.
The coracoacromial ligament is released from its acromial insertion in the left shoulder through the use of a scalpel. The lateral border of the ligament is then prepared using a No. 5 Ethibond suture (Ethicon, Somerville, NJ) by way of the Kessler suture technique (A, B). (CAL, coracoacromial ligament; CHL, coracohumeral ligament.)
Tunnel Preparation and Excision of the Lateral End
A surgical ruler is used on the superior aspect of the clavicle to mark the position of 3 cm from the most lateral aspect of the clavicle with either a coagulator or surgical pen. A 2.5-mm drill is then used to make a tunnel at this position in a superior-to-inferior direction. Once the first tunnel is complete, the surgical ruler is used again to measure the position 1 cm lateral to the first tunnel. The position is marked with either a coagulator or surgical pen, and then a 2.5-mm drill is again used to make this second tunnel in a superior-to-inferior direction (Fig 4). To ensure stability of the clavicle during this portion of the procedure, we recommend securement of the clavicle with a Weber or similar clamp. After this, a total distance of 1 cm of the lateral aspect of the clavicle is measured using a surgical ruler. Then, this portion of clavicle is excised using a rongeur, thereby exposing the intramedullary canal. Once the lateral aspect of the clavicle is excised, a 2.5-mm drill is used to form 2 tunnels at the lateral aspect of the clavicle. The first tunnel begins at the anterior aspect of the intramedullary canal and is constructed toward the posterior aspect of the clavicle. Then, the second tunnel begins at the posterior aspect of the canal and is constructed toward the anterior aspect of the clavicle (Fig 5). Care is taken to avoid fractures of the lateral aspect of the clavicle while forming the tunnels. For this reason, we suggest that the end of both tunnels be at least 0.5 cm medial from the lateral edge of the clavicle.
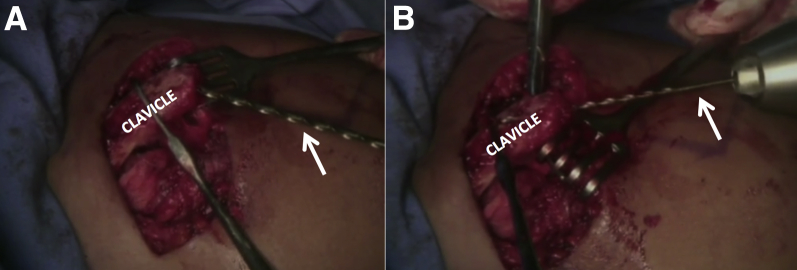
Fig 4.
After the coracoacromial ligament is released from its acromial insertion in the left shoulder, a surgical ruler is used to measure a 3 cm distance from the lateral end of the clavicle on the superior surface of the clavicle (A). The clavicle is secured and a 2.5-mm drill (white arrow) is used to create 2 tunnels in a superior-to-inferior direction (B). The first tunnel is located 3 cm from the acromioclavicular joint and the other is found 1 cm lateral from the first tunnel. Afterward, 1 cm of the most lateral end of the clavicle is resected using a rongeur (green arrow, C). (Yellow arrow, most lateral aspect of the clavicle.)
Fig 5.
Once the lateral end of the left clavicle is resected, a 2.5-mm drill (white arrows, A and B) is used to create 2 intramedullary tunnels. The first tunnel starts at the anterior aspect of the intramedullary canal and is constructed toward the posterior aspect of the clavicle. The second tunnel begins at the posterior aspect of the canal and is constructed toward the anterior aspect of the clavicle.
Suture Passage Underneath the Coracoid Process
Using Metzenbaum scissors, we define the margins of the coracoid process with care to avoid any potential damage to the ligamentous and muscle attachments of the coracoid. Once the outline of the coracoid process and its attachments are properly visualized, a coracoid suture passer (Hospitalia Cirurgica, Florianopolis, Brazil) is used to deliver the passing suture from medial to lateral, directly under the coracoid process. Once the passing suture has reached the lateral side of the coracoid process, 4 No. 5 Ethibond sutures (Ethicon) are passed under the coracoid process. Once the sutures have been passed under the coracoid, there are 4 suture limbs on the lateral side and 4 on the medial side, which totals 8 suture limbs spanning both sides of the coracoid. Two of the 4 suture limbs on the lateral side of the coracoid are then passed through the most medial tunnel of the lateral end of the clavicle. Then, 2 of the 4 suture limbs on the medial side of the coracoid are passed through the most lateral tunnel of the lateral end of the clavicle to make a figure “X” by passing one pair of suture limbs over the other pair (Fig 6).
Fig 6.
In the left shoulder, 4 No. 5 Ethibond sutures (Ethicon, Somerville, NJ) are passed underneath the coracoid process (yellow arrow, A) from lateral to medial. To facilitate the passage of all the sutures at once, a coracoid suture passer (Hospitalia Cirurgica, Florianopolis, Brazil) is used from medial to lateral with a total of 4 suture limbs on each side of the coracoid process. Two suture limbs on the lateral side are then passed through the most medial tunnel in the clavicle and 2 suture limbs on the medial side are passed through the most lateral tunnel one pair over the other (B).
Suture Fixation on the Superior Surface of the Clavicle
While simultaneously applying a superior-to-inferior force to reduce the clavicle, both suture limbs inside the most medial tunnel are tied together. Then, both suture limbs inside the most lateral tunnel are tied together. Once both suture limbs for each tunnel have been tied, they are tied together on the superior surface of the clavicle. Although the clavicle remains slightly anterior after the suture limbs are tied, our clinical experience suggests that this has no adverse effects postoperatively and, therefore, has no clinical relevance. The excess suture is then removed. The other 2 suture limbs on the lateral side of the coracoid process are then passed over the lateral aspect of the clavicle, 1 cm from the lateral edge of the clavicle and 1 cm lateral from the most lateral clavicular tunnel. Once the 2 suture limbs on the lateral side of the coracoid process have been passed over, they are tied to the remaining 2 suture limbs on the medial side of the coracoid process. The 4 suture limbs are tied and secured on the superior surface of the clavicle. The excess suture is then removed.
Coracromial Ligament Transfer to the Lateral Clavicle
Attention is then turned to the CAL once all suture limbs running underneath the coracoid process have been secured. The 2 suture limbs arising from the CAL end, previously prepared through the Kessler suture technique, are then passed through the previously prepared tunnels located 0.5 cm from the lateral end of the clavicle. Each suture limb is passed inside the intramedullary tunnel previously made (Fig 7). The lateral suture limb passed through the most medial tunnel and the medial suture limb passed through the most lateral tunnel. The CAL is then gently introduced inside the intramedullary canal and both suture limbs are tied and secured on the superior surface of the clavicle. The integrity and strength of the repair is then verified by taking the shoulder through normal range of motion. This confirms excellent stability of the AC joint after the repair as seen in Video 1. Finally, copious irrigation with a saline solution is performed; then the deltotrapezoidal fascia is closed using a No. 2 Vicryl suture (Ethicon). After this, the subcutaneous tissue layer is approximated using a No. 2 Vicryl suture (Ethicon). The skin layer is then closed using an intradermal suture with Monocryl 3-0 (Ethicon). Postoperative radiographs are obtained to verify the success of the technique (Fig 8).
Fig 7.
Once the clavicle of the left shoulder is reduced and kept in position using the nonabsorbable sutures, the sutures previously passed through the lateral end of the coracoacromial ligament (CAL, yellow arrow, (A)) are inserted through the intramedullary tunnels and tied and secured on the superior aspect of the clavicle. This fixation introduces the CAL into the intramedullary canal (B).
Fig 8.
Postoperative imaging showing the preoperative (A) and postoperative (B) views of the affected left shoulder and contralateral shoulder. Note the complete dislocation of the acromioclavicular joint on the left side (yellow arrow, A) compared with the noninjured, contralateral side (white arrows) as well as the reduction of the joint after our surgical technique (yellow arrow, B).
Rehabilitation Protocol
After surgery, the patient is immediately placed in a sling for 6 weeks. The goal during the rehabilitation protocol is to optimize the AC joint stability, while providing a safe environment for healing of the CAL in the clavicular intramedullary canal. At the patient's discretion, we suggest active hand, wrist, and elbow exercises with no resistance as soon as possible. At week 2, the use of the sling is discontinued during physiotherapy sessions, in which exercises of passive movement in the scapular plane is initiated. However, no abduction of the shoulder is allowed at this time. The range of motion is gradually increased from passive to active-assisted/active in nature based on the individual progress and discretion of the patient. At week 6, the sling is entirely discontinued and abduction exercises are initiated. Weightlifting is not permitted during the initial 4 months after surgery. Then, after these 4 months, the patient can begin progressive weight-training exercises. Although the return to sport is patient dependent, we recommend a return to noncontact sports no sooner than 6 months and a return to contact sports no sooner than 9 months. Advantages and disadvantages as well as pearls and pitfalls associated with the technique are summarized in Tables 1 and 2, respectively.
Table 1.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Low cost and reproducible | Open procedure with more exposure and damage to the surrounding soft tissues as well as greater risk of infection |
| No need for hardware fixation that avoids potential hardware complication | Nonanatomical reconstruction of the joint |
| Satisfactory reduction of the joint is achievable regardless of severity of acromioclavicular joint instability | |
| No arthroscopic proficiency is required | |
| No donor site morbidity |
Table 2.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Use Langer's lines for a cosmetically better appearance after surgery | A fracture of the clavicle is possible during drilling of the intramedullary holes located 0.5 cm from the lateral edge of the clavicle |
| Perform a subperiosteal soft tissue release on the clavicle to allow for an effective reapproximation and cover of the sutures | Damage to the ligament and tendon attachments of the coracoid process may occur during suture passage |
| A coracoid suture passer assists with suture passage underneath the coracoid from medial to lateral | Neurovascular damage is possible without caution |
| Pass the suture limbs, one over the other, through the clavicular tunnels |
Discussion
This Technical Note describes in detail our preferred method for the treatment of high-grade and chronic AC joint instability. Our technique has several advantages, which include low cost, no need for hardware fixation, satisfactory reduction of the AC joint, no need of arthroscopy proficiency, and no donor site morbidity. Several conservative and surgical techniques have been previously described for the treatment of all AC joint injury grades (Rockwood's grades I-VI). However, there is a lack of consensus regarding the best treatment option for Rockwood's grades III, given that surgery may be needed in these cases.7, 8 Although the literature suggests and supports conservative treatment for grades I and II, optimal treatment, whether conservative or surgical, of grade III injuries remains controversial.9 Spencer9 performed a systematic review and, despite a low-evidence level, concluded that conservative treatment for grade III injuries resulted in less time away from physical activity and less risk of potential complications; similar findings and conclusions regarding grade III injuries were reported by Ceccarelli et al.10 Nevertheless, controversy persists regarding this specific injury given that conservative management has resulted in chronic and recalcitrant symptoms.11, 12, 13
Treatment options for severe AC joint instability include screw fixation between the coracoid and clavicle as well as transfer of the CAL onto the coracoid, both in isolation and in association with supplementary fixation methods.14, 15, 16 Several authors have described positive outcomes after screw fixation. Esenyel et al.17 reported that the modified Bosworth procedure was associated with low AC joint degeneration and low complication rates including a rate of 86.7% of excellent results in patients after treatment. In addition, Lin et al.18 reported positive outcomes after coracoclavicular screw fixation in association with CAL reconstruction as 30 patients reported an 88.9% satisfaction rate after 23.6 months after surgery.
Outcomes after isolated CAL transfer to treat severe AC joint instability have been associated with success and high patient satisfaction.19, 20 The first description of this procedure was reported by Weaver and Dunn,19 in which the fixation of the shortened acromial end of the CAL into the medullary canal of the clavicle in conjunction with a combined oblique arthroplasty resection of the AC joint was illustrated. Shoji et al.21 also reported positive outcomes after CAL transfer for the treatment of grade III AC joint instability with 14 of 15 patients reporting full range of shoulder motion with no pain after surgery. However, a biomechanical study performed by Wilson et al.22 described that CAL transfer when completed in association with the fixation of the clavicle to the coracoid process provides a more reliable fixation that less likely results in revision. Sood et al.23 performed a systematic review on differences in outcomes between isolated CAL transfer and CAL transfer associated with a concomitant fixation procedure and found satisfactory results with similar recurrence rates. Despite similar outcomes, the group with an associated fixation procedure aside from CAL transfer experienced more complications especially when involving metal hardware. Ultimately, no definitive conclusion is possible regarding a potential difference between isolated CAL transfer and CAL transfer with supplementary fixation given the lack of high evidence studies.24
Anatomical reconstruction of the AC joint that involves CAL reconstruction through the use of a graft has been shown to result in positive outcomes.25 Regarding the comparison in outcomes between AC joint reconstruction through the use of a semitendinosus autograft and the modified Weaver-Dunn procedure, Hegazy et al.26 found better outcomes in AC joint reconstruction based on 20 patients with a mean follow-up time of 27.8 months. According to clinical and radiologic postoperative measurements, Tauber et al.27 found significantly better outcomes (based on mean American Shoulder and Elbow Surgeons and Constant scores) in coracoclavicular ligament reconstruction than the modified Weaver-Dunn for the treatment of grade III to V AC joint instability. Regarding arthroscopic surgery for the treatment of severe AC joint instability, Woodmass et al.28 reviewed complications after the arthroscopic fixation of the joint and reported shoulder pain, infection, coracoclavicular calcification, and loss of reduction as the most common postoperative complications. In conclusion, we present our preferred surgical technique for the treatment of an AC joint dislocation through the use of CAL transfer to the lateral clavicle and nonabsorbable suture fixation. Although we suggest the use of our technique, long-term, large cohort studies are needed to evaluate the real benefits of our procedure as well as to compare outcomes of the described technique with outcomes after AC joint reconstruction.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: The authors have received research grants from Health South East and Arthrex. However, these research grants did not involve and, ultimately, did not influence the production of this work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is positioned in a beach chair position with the left shoulder prepped in a sterile fashion. After this, relevant bony prominences are marked with a surgical pen. The incision to be made is then outlined following Langer's lines. A scalpel is used to perform a longitudinal incision, starting at the coracoid process and extending proximally to the clavicle. Afterward, the subcutaneous tissue is bluntly dissected. The deltotrapezoidal fascia is exposed and opened in line with the skin incision through the use of Metzenbaum scissors. The superior and anterior aspects of the clavicle are then exposed. Once the clavicle is entirely exposed, the lateral border of the clavicle is released from all scar tissues. With the use of a scalpel, the coracoacromial ligament (CAL) is released from its acromial insertion. A No. 5 Ethibond (Ethicon, Somerville, NJ) is then used to prepare the end of the CAL through the Kessler suture technique. Then, at 3 cm from the most lateral aspect of the clavicle, a 2.5-mm drill is used to make the first tunnel in a superior-to-inferior direction. The second tunnel is then made 1 cm lateral to the initial tunnel. After this, 1 cm of the most lateral aspect of the clavicle is excised using a rongeur, thereby exposing the intramedullary canal. Two tunnels, in which the end of the CAL will be placed, are then made 0.5 cm from the lateral end. The first tunnel begins at the anterior aspect of the intramedullary canal and is constructed toward the posterior aspect of the clavicle. Then, the second tunnel begins at the posterior aspect of the canal and is constructed toward the anterior aspect of the clavicle. After this, a coracoid suture passer (Hospitalia Cirurgica, Florianopolis, Brazil) is used to guide passing suture underneath the coracoid process with a total of 4 No. 5 Ethibond (Ethicon) suture limbs on each side, medial and lateral, of the coracoid. Two lateral suture limbs are then passed through the most medial tunnel in the clavicle and 2 medial suture limbs are passed through the most lateral tunnel, one pair over the other. The clavicle is then reduced and the sutures are tied and secured at the superior surface of the clavicle. The other lateral suture limbs are then passed over the lateral aspect of the clavicle and tied to the remaining 2 medial suture limbs. After this, the CAL is introduced into the intramedullary canal with each of the 2 suture limbs, previously prepared through the Kessler suture technique, individually passed through the 2 previously prepared tunnels 0.5 cm away from the lateral end of the clavicle. Finally, the deltotrapezoidal fascia, subcutaneous tissue, and skin layer are closed in a standard fashion and the procedure is complete.
References
- 1.Pallis M., Cameron K.L., Svoboda S.J., Owens B.D. Epidemiology of acromioclavicular joint injury in young athletes. Am J Sports Med. 2012;40:2072–2077. doi: 10.1177/0363546512450162. [DOI] [PubMed] [Google Scholar]
- 2.Beim G.M. Acromioclavicular joint injuries. J Athl Train. 2000;35:261–267. [PMC free article] [PubMed] [Google Scholar]
- 3.Garretson R.B., III, Williams G.R., Jr. Clinical evaluation of injuries to the acromioclavicular and sternoclavicular joints. Clin Sports Med. 2003;22:239–254. doi: 10.1016/s0278-5919(03)00008-5. [DOI] [PubMed] [Google Scholar]
- 4.Ernberg L.A., Potter H.G. Radiographic evaluation of the acromioclavicular and sternoclavicular joints. Clin Sports Med. 2003;22:255–275. doi: 10.1016/s0278-5919(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 5.Saccomanno M.F., DE Ieso C., Milano G. Acromioclavicular joint instability: Anatomy, biomechanics and evaluation. Joints. 2014;2:87–92. doi: 10.11138/jts/2014.2.2.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schaefer F.K., Schaefer P.J., Brossmann J., Hilgert R.E., Heller M., Jahnke T. Experimental and clinical evaluation of acromioclavicular joint structures with new scan orientations in MRI. Eur Radiol. 2006;16:1488–1493. doi: 10.1007/s00330-005-0093-1. [DOI] [PubMed] [Google Scholar]
- 7.Lee S., Bedi A. Shoulder acromioclavicular joint reconstruction options and outcomes. Curr Rev Musculoskelet Med. 2016;9:368–377. doi: 10.1007/s12178-016-9361-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Virk M.S., Apostolakos J., Cote M.P., Baker B., Beitzel K., Mazzocca A.D. Operative and nonoperative treatment of acromioclavicular dislocation: A critical analysis review. JBJS Rev. 2015;3 doi: 10.2106/JBJS.RVW.N.00092. [DOI] [PubMed] [Google Scholar]
- 9.Spencer E.E., Jr. Treatment of grade III acromioclavicular joint injuries: A systematic review. Clin Orthop Relat Res. 2007;455:38–44. doi: 10.1097/BLO.0b013e318030df83. [DOI] [PubMed] [Google Scholar]
- 10.Ceccarelli E., Bondi R., Alviti F., Garofalo R., Miulli F., Padua R. Treatment of acute grade III acromioclavicular dislocation: A lack of evidence. J Orthop Traumatol. 2008;9:105–108. doi: 10.1007/s10195-008-0013-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gumina S., Carbone S., Postacchini F. Scapular dyskinesis and SICK scapula syndrome in patients with chronic type III acromioclavicular dislocation. Arthroscopy. 2009;25:40–45. doi: 10.1016/j.arthro.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 12.Schlegel T.F., Burks R.T., Marcus R.L., Dunn H.K. A prospective evaluation of untreated acute grade III acromioclavicular separations. Am J Sports Med. 2001;29:699–703. doi: 10.1177/03635465010290060401. [DOI] [PubMed] [Google Scholar]
- 13.Wojtys E.M., Nelson G. Conservative treatment of grade III acromioclavicular dislocations. Clin Orthop Relat Res. 1991;268:112–119. [PubMed] [Google Scholar]
- 14.Godry H., Citak M., Konigshausen M., Schildhauer T.A., Seybold D. Treatment of chronic acromioclavicular joint dislocation in a paraplegic patient with the Weaver-Dunn procedure and a hook-plate. Orthop Rev (Pavia) 2016;8:6371. doi: 10.4081/or.2016.6371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adam F.F., Farouk O. Surgical treatment of chronic complete acromioclavicular dislocation. Int Orthop. 2004;28:119–122. doi: 10.1007/s00264-003-0520-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tienen T.G., Oyen J.F., Eggen P.J. A modified technique of reconstruction for complete acromioclavicular dislocation: A prospective study. Am J Sports Med. 2003;31:655–659. doi: 10.1177/03635465030310050401. [DOI] [PubMed] [Google Scholar]
- 17.Esenyel C.Z., Ozturk K., Bulbul M., Ayanoglu S., Ceylan H.H. Coracoclavicular ligament repair and screw fixation in acromioclavicular dislocations. Acta Orthop Traumatol Turc. 2010;44:194–198. doi: 10.3944/AOTT.2010.2329. [DOI] [PubMed] [Google Scholar]
- 18.Lin W.C., Wu C.C., Su C.Y., Fan K.F., Tseng I.C., Chiu Y.L. Surgical treatment of acute complete acromioclavicular dislocation: Comparison of coracoclavicular screw fixation supplemented with tension band wiring or ligament transfer. Chang Gung Med J. 2006;29:182–189. [PubMed] [Google Scholar]
- 19.Weaver J.K., Dunn H.K. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am. 1972;54:1187–1194. [PubMed] [Google Scholar]
- 20.Warren-Smith C.D., Ward M.W. Operation for acromioclavicular dislocation. A review of 29 cases treated by one method. J Bone Joint Surg Br. 1987;69:715–718. doi: 10.1302/0301-620X.69B5.3316237. [DOI] [PubMed] [Google Scholar]
- 21.Shoji H., Roth C., Chuinard R. Bone block transfer of coracoacromial ligament in acromioclavicular injury. Clin Orthop Relat Res. 1986;208:272–277. [PubMed] [Google Scholar]
- 22.Wilson D.R., Moses J.M., Zilberfarb J.L., Hayes W.C. Mechanics of coracoacromial ligament transfer augmentation for acromioclavicular joint injuries. J Biomech. 2005;38:615–619. doi: 10.1016/j.jbiomech.2004.04.015. [DOI] [PubMed] [Google Scholar]
- 23.Sood A., Wallwork N., Bain G.I. Clinical results of coracoacromial ligament transfer in acromioclavicular dislocations: A review of published literature. Int J Shoulder Surg. 2008;2:13–21. doi: 10.4103/0973-6042.39582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rhee Y.G., Park J.G., Cho N.S., Song W.J. Clinical and radiologic outcomes of acute acromioclavicular joint dislocation: Comparison of Kirschner's wire transfixation and locking hook plate fixation. Clin Shoulder Elbow. 2014;17:159–165. [Google Scholar]
- 25.Saccomanno M.F., Fodale M., Capasso L., Cazzato G., Milano G. Reconstruction of the coracoclavicular and acromioclavicular ligaments with semitendinosus tendon graft: A pilot study. Joints. 2014;2:6–14. [PMC free article] [PubMed] [Google Scholar]
- 26.Hegazy G., Safwat H., Seddik M., Al-Shal E.A., Al-Sebai I., Negm M. Modified Weaver-Dunn procedure versus the use of semitendinosus autogenous tendon graft for acromioclavicular joint reconstruction. Open Orthop J. 2016;10:166–178. doi: 10.2174/1874325001610010166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tauber M., Gordon K., Koller H., Fox M., Resch H. Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: A prospective comparative study. Am J Sports Med. 2009;37:181–190. doi: 10.1177/0363546508323255. [DOI] [PubMed] [Google Scholar]
- 28.Woodmass J.M., Esposito J.G., Ono Y. Complications following arthroscopic fixation of acromioclavicular separations: A systematic review of the literature. Open Access J Sports Med. 2015;6:97–107. doi: 10.2147/OAJSM.S73211. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is positioned in a beach chair position with the left shoulder prepped in a sterile fashion. After this, relevant bony prominences are marked with a surgical pen. The incision to be made is then outlined following Langer's lines. A scalpel is used to perform a longitudinal incision, starting at the coracoid process and extending proximally to the clavicle. Afterward, the subcutaneous tissue is bluntly dissected. The deltotrapezoidal fascia is exposed and opened in line with the skin incision through the use of Metzenbaum scissors. The superior and anterior aspects of the clavicle are then exposed. Once the clavicle is entirely exposed, the lateral border of the clavicle is released from all scar tissues. With the use of a scalpel, the coracoacromial ligament (CAL) is released from its acromial insertion. A No. 5 Ethibond (Ethicon, Somerville, NJ) is then used to prepare the end of the CAL through the Kessler suture technique. Then, at 3 cm from the most lateral aspect of the clavicle, a 2.5-mm drill is used to make the first tunnel in a superior-to-inferior direction. The second tunnel is then made 1 cm lateral to the initial tunnel. After this, 1 cm of the most lateral aspect of the clavicle is excised using a rongeur, thereby exposing the intramedullary canal. Two tunnels, in which the end of the CAL will be placed, are then made 0.5 cm from the lateral end. The first tunnel begins at the anterior aspect of the intramedullary canal and is constructed toward the posterior aspect of the clavicle. Then, the second tunnel begins at the posterior aspect of the canal and is constructed toward the anterior aspect of the clavicle. After this, a coracoid suture passer (Hospitalia Cirurgica, Florianopolis, Brazil) is used to guide passing suture underneath the coracoid process with a total of 4 No. 5 Ethibond (Ethicon) suture limbs on each side, medial and lateral, of the coracoid. Two lateral suture limbs are then passed through the most medial tunnel in the clavicle and 2 medial suture limbs are passed through the most lateral tunnel, one pair over the other. The clavicle is then reduced and the sutures are tied and secured at the superior surface of the clavicle. The other lateral suture limbs are then passed over the lateral aspect of the clavicle and tied to the remaining 2 medial suture limbs. After this, the CAL is introduced into the intramedullary canal with each of the 2 suture limbs, previously prepared through the Kessler suture technique, individually passed through the 2 previously prepared tunnels 0.5 cm away from the lateral end of the clavicle. Finally, the deltotrapezoidal fascia, subcutaneous tissue, and skin layer are closed in a standard fashion and the procedure is complete.