Abstract
Meniscal ramp lesions have been reported to be present in 9% to 17% of patients undergoing anterior cruciate ligament reconstruction. Detection at the time of arthroscopy can be accomplished based upon clinical suspicion and careful evaluation without the use of an accessory posteromedial portal. Options for surgical treatment include arthroscopic repair using an all-inside or inside-out technique. The purpose of this Technical Note is to detail our arthroscopic inside-out repair technique for meniscal ramp lesions.
A “ramp lesion” is a specific medial meniscal tear that is less well-known, although it is reported to be present in 9% to 17% of acute anterior cruciate ligament (ACL) injuries.1, 2, 3 This injury pattern was first reported in 1988 by Strobel4 and described as a medial meniscal injury involving the peripheral attachment of the posterior horn. Although less common, lateral meniscal ramp lesions may also occur.
Currently, there are conflicting ideas regarding the precise anatomic location of ramp lesions; some investigators use the traditional definition of a meniscocapsular disruption,2 whereas others describe the meniscotibial ligament of the posterior horn as the site of injury.3 This also stems from difficulty diagnosing ramp lesions via both magnetic resonance imaging (MRI)1 and arthroscopy.3, 5 In order to further evaluate the ability of MRI to enable diagnosis of these injuries, a large study was performed by DePhillipo et al., and it was reported that a posteromedial tibial bone bruise was a secondary finding associated with ramp lesions.6
It is believed that repair of meniscal ramp lesions will lead to improved healing and joint stability, although further anatomical and biomechanical studies need to be undertaken to better describe these lesions and their biomechanical importance. The purpose of this article is to demonstrate a systematic evaluation for identification of ramp lesions and also describe an inside-out repair arthroscopy-assisted repair technique.
Surgical Technique
Prevalence, Clinical Evaluation, and Operative Indications
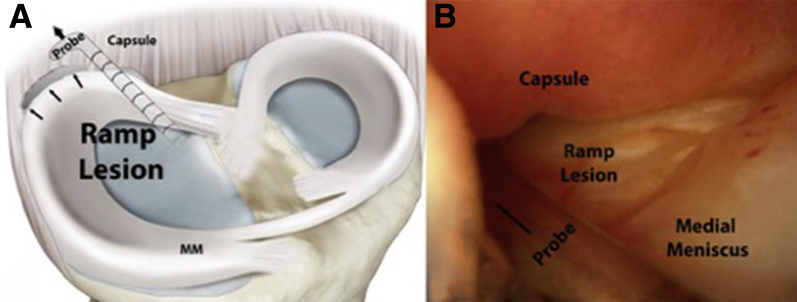
Meniscal ramp lesions occur concomitantly with 9% to 19% of all ACL tears.1, 2 Due to the limited diagnostic sensitivity for both physical exam and MRI (Fig 1) (due to the closure of the gap between the meniscus and the capsule during extension), careful arthroscopic evaluation of the meniscocapsular junction is vital. Patients with evidence of acute disruption of the meniscocapsular junction with associated increased meniscal translation are indicated for repair of the ramp lesion, especially in the setting of an ACL tear.
Fig 1.
A magnetic resonance image (MRI) depicting a ramp lesion (depicted with arrow) with an associated posteromedial bone bruise (also depicted with arrow). MRI does not have a very high sensitivity for depicting ramp lesions, however, it should always be part of a diagnostic work-up, and in some cases, such as image depicted, it can be quite helpful.
Patient Positioning and Anesthesia
The patient is placed in the supine position on the operating table. After the induction of general anesthesia, a bilateral knee examination is performed to assess knee range of motion and evaluate for concurrent ligamentous laxity. A well-padded thigh tourniquet is placed on the operative extremity, which is then secured in a leg holder (Mizuho OSI, Union City, CA) while the contralateral knee is padded and placed into an abduction stirrup (Birkova Product, Gothenburg, NE). The leg holder should be placed proximal enough to allow a medial or lateral approach for an inside-out meniscal repair. The foot of the operating table is then lowered, allowing the surgeon to freely manipulate the knee.
Arthroscopic Evaluation
This surgical technique is shown in detail in Video 1. Additionally, pearls and pitfalls of this technique and a step-by-step approach are described in Tables 1 and 2, respectively.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Good visualization of the posterior part of the meniscus to diagnose ramp lesions | Nerve injuries |
| High level of suspicion | Vascular injuries in the posterior knee |
| A posteromedial portal can help to visualize the posterior part of the medial meniscus. | Failure to identify the ramp lesions |
| Inside-out meniscal repair with vertical mattress sutures for a strong repair construct | Failure to protect the repair with appropriate rehabilitation protocol |
| Create a posteromedial approach (Chahla et al.)4 |
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| A high level of suspicion and a comprehensive review of the imaging is vital to detect these lesions: look for posteromedial tibial marrow edema and a slight separation of the posteromedial capsule from the meniscus. | Do not attribute bone marrow changes only to the anterior cruciate ligament (ACL) injury. Actively look for associated lesions. |
| A systematic approach to verify for the absence of this lesion can yield better ACL reconstruction outcomes with lower failure rates. | Failing to address a meniscal ramp lesion can result in changed knee biomechanics and increased failure rates. |
| Inside-out sutures allow for more versatility when repairing the meniscus. | Technically demanding, need for an additional approach. |
| Excellent results have been reported for these repairs due to the favorable zone of the tear and also because they are usually associated with ACL reconstructions, which further improves the biological profile of these lesions. | Although extended surgical time can be expected because of the repair, a careful look into the posteromedial capsule should be routinely performed with the creation of accessory portals if necessary. |
An initial diagnostic arthroscopy is performed with standard anterolateral and anteromedial portals directly adjacent to the patellar tendon. No additional portals are usually required to assess for the presence of meniscal ramp lesions. In patients undergoing a concurrent ACL reconstruction, we prefer to debride the ACL remnant and ream the femoral tunnel prior to evaluation of the menisci.
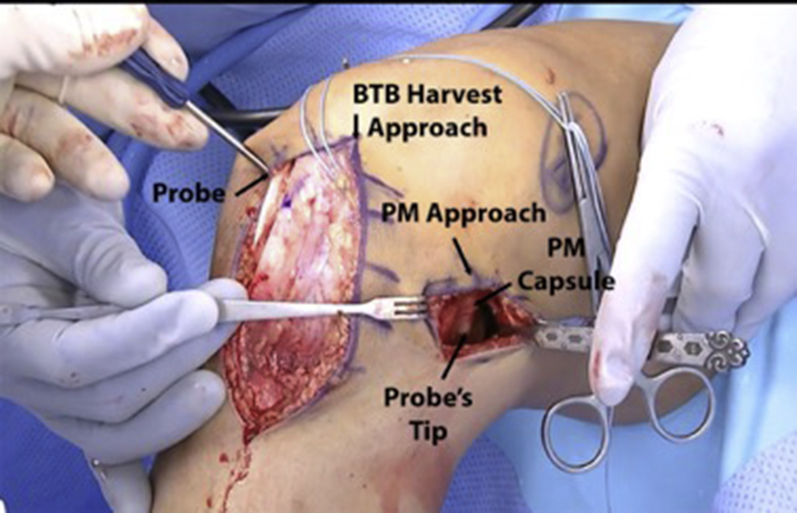
Viewing from the anterolateral portal, the arthroscope is advanced through the intercondylar notch with the knee in 30° of flexion for inspection of the posterior horn of the medial meniscus. A probe is directed over the superior aspect of the posterior horn of the medial meniscus to allow for inspection of the junction between the meniscus and capsule to identify whether a ramp lesion is present. The probe is used to displace the posteromedial capsule from the posteromedial meniscocapsular attachment. A ramp lesion is diagnosed if a tear or separation is present at this junction (Fig 2A).
Fig 2.
(A) Illustration depicting technique to assess for ramp lesion, using a probe to retract the posteromedial capsule away from the posteromedial meniscocapsular attachment on a left knee. A ramp lesion is diagnosed if a tear or separation is present at this junction. (B) Corresponding arthroscopic evaluation of meniscal ramp lesion without the use of an accessory posteromedial portal as viewed from the anteromedial portal and inserting the probe through the anterolateral portal.
Additionally, a probe can be inserted under the inferior aspect of the posterior horn of the medial meniscus and placed in the meniscocapsular junction to assess the integrity of the tibial attachment (Fig 2B). If a ramp lesion is present, the meniscus will sublux anteriorly. An accessory posteromedial portal can be used but is rarely required to completely visualize the posterior meniscocapsular attachment.
Medial Approach
After inspection and confirmation of the presence of a ramp lesion, a posteromedial approach is planned. The incision placement may be facilitated by transillumination of the medial compartment and by palpation of an intra-articular probe placed along the medial joint line. Transillumination of the skin with the arthroscope allows visualization of the saphenous vein. An incision approximately 4 cm in length is made posterior to the medial collateral ligament. Because the suture needles often angle downward as they exit the joint capsule, it is helpful to have two-thirds of the incision distal to the joint line with one-third proximal.
The approach is made with the knee in flexion. The oblique pes fascia should be identified during dissection deep to the subcutaneous tissue. The anterior sartorius fascia is identified and subsequently dissected from proximal to distal. The pes tendons should be retracted to protect the saphenous nerve, which lies posteromedial to the tendons. Upon deeper dissection, the interval between the medial head of the gastrocnemius and the posteromedial joint capsule is identified (Fig 3). The gastrocnemius is then dissected off the capsule using Metzenbaum scissors, followed by using a blunt Cobb elevator. Blunt digital dissection may also be useful to aid in the separation of the muscle from the capsule. Working from distal to proximal facilitates the dissection of the gastrocnemius off of the posterior capsule. A Cobb elevator is temporarily placed posteriorly within this interval followed by a bent spoon placed anterior to the Cobb to protect the neurovascular structures (Fig 4). The spoon retractor should be held so that the needles piercing the posterior capsule are deflected medially toward the assistant. Keeping the knee in 70° to 90° of flexion relaxes the hamstring and gastrocnemius, which improves visualization retrieval of the needles as they exit the posterior capsule.
Fig 3.
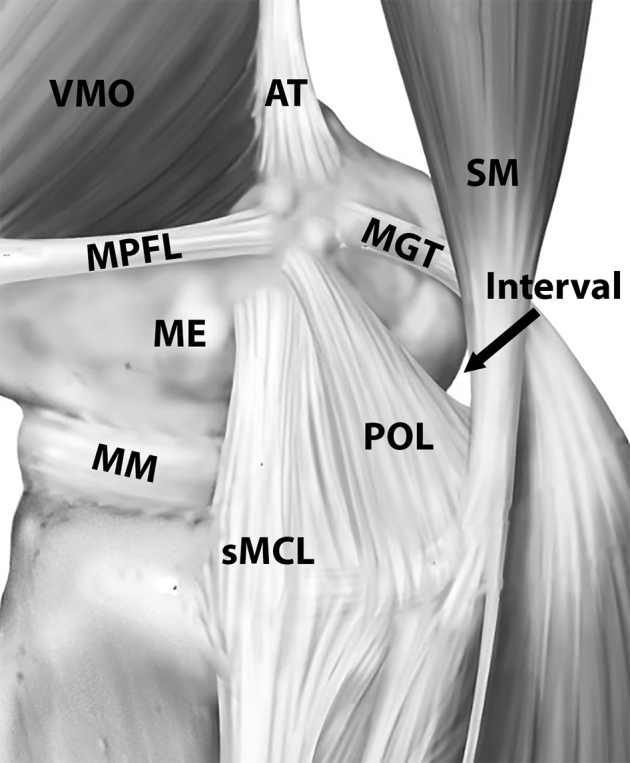
The interval is identified between the medial head of the gastrocnemius and the posteromedial capsule on a right knee. This schematic image also depicts the anatomic relationship of the superficial medial collateral ligament and the semimembranosus in relation to the interval.
Fig 4.
A bent spoon is used as a retractor inserted between the posteromedial (PM) joint capsule anteriorly and the medial head of the gastrocnemius muscle posteriorly in this right knee. The probe can be inserted through the anteromedial portal and used to visualize the trajectory of suture needle placement prior to beginning meniscal repair.
Meniscal Repair
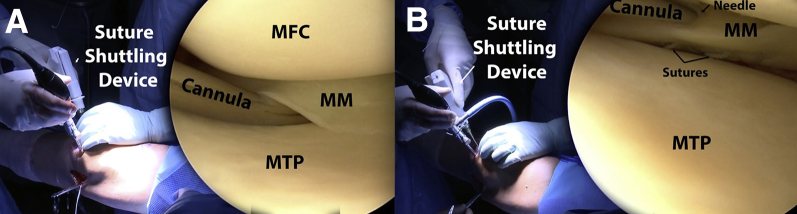
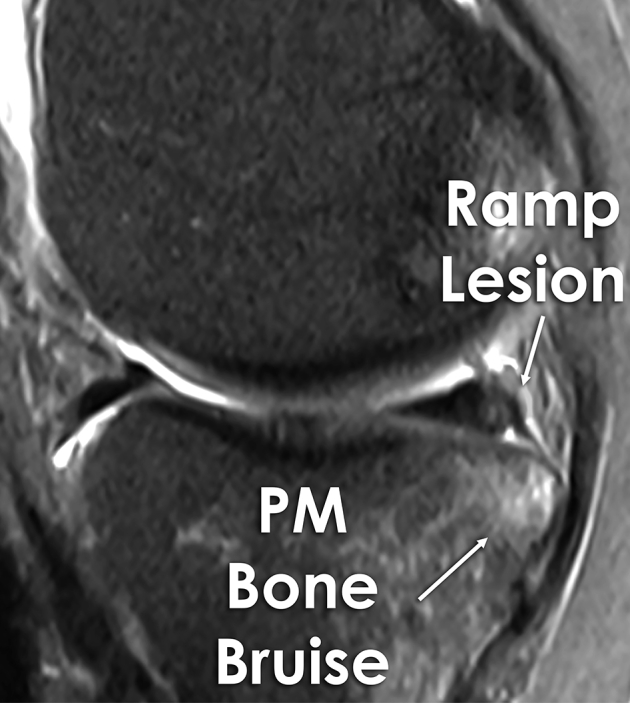
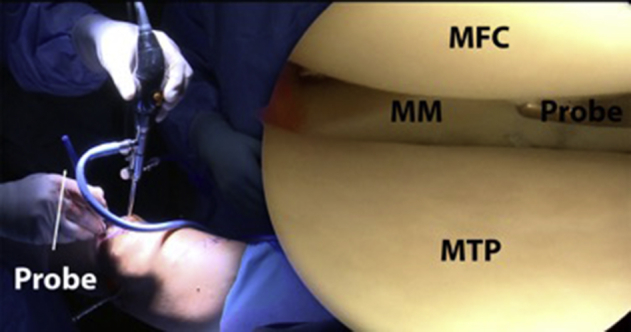
A commercially available device (SharpShooter, Stryker, Kalamazoo, MI) is used to place sutures (no. 2 FiberWire) into the meniscus. For medial meniscus ramp lesions, entry from the anterolateral portal decreases the risk of damaging the neurovascular structures and optimizes the direction of the needle as it exits the capsule. With application of a valgus force, the cannula is directed toward the tear under arthroscopic visualization (Fig 5A). Slight advancement of the needle allows visualization of the precise entry location (Fig 5B).
Fig 5.
Suture placement for inside-out meniscus ramp repair in a right knee. (A and B) Images of suture shuttling device with corresponding arthroscopic placement of cannula with vertical suture mattress technique as viewed from the anteromedial portal and with the suture shuttling device from the anterolateral portal (MFC, medial femoral condyle; MM, medial meniscus; MTP, medial tibial plateau).
For tears at the meniscocapsular junction, the first needle is usually passed through the meniscus and the second through the adjacent capsule to create a vertical or oblique pattern. The knee is placed in 10° to 20° of flexion during needle advancement through the meniscus and capsule; after passage, knee flexion of 70° to 90° may assist in needle retrieval. The cannula is redirected to deliver the second needle and place the suture adjacent to the first. It is important to keep slight tension on the suture to avoid inadvertent damage to the suture during advancement of the second needle.
An assistant should be prepared to retrieve the suture needles using a heavy needle driver. Optimal lighting and retraction allow visualization of the needles as they are delivered through the capsule. Sutures are typically placed sequentially from posterior to anterior; however, if there is difficulty visualizing the first needle, an anterior suture may be placed because it is typically easier to locate and can help to guide the expected delivery location of subsequent posterior sutures.
In a similar fashion, multiple sutures are placed between 3 and 5 mm apart (Fig 4). Sutures may be placed above the meniscus (i.e. femoral-sided) and below the meniscus (i.e. tibial sided). Typically, femoral-sided sutures are placed first. Sometimes, this will create a “puckering” of the meniscus superiorly and resultant gapping of the tear on the tibial side. This should be reduced with tibial-sided sutures placed in a similar fashion. Compared to all-inside meniscal repair, the inside-out repair technique results in smaller holes in the meniscus during suture passage, allowing for the passage of a greater number of sutures and fixation points without creating as much iatrogenic meniscal damage.
As the assistant retrieves the needles, the needles are promptly cut from the suture and the paired sutures are tagged with a hemostat. Use of an Allis clamp to grasp the hemostats through the hemostat finger holes allows organization of the sequentially passed sutures. However, rather than delaying knot tying until completion of suture passage, sutures can also be tied immediately after passage. Care to avoid overtightening of the sutures is important, and the meniscus can be directly visualized arthroscopically during knot tying. The meniscocapsular junction is probed to ensure stability following completion of the repair (Fig 6).
Fig 6.
Surgeon confirming stability of the repair construct using a probe placed through the anteromedial portal following inside-out repair of a meniscal ramp lesion in a right knee. If needed, additional sutures can be placed at this point to ensure adequate fixation. (MFC, medial femoral condyle; MM, medial meniscus; MTP, medial tibial plateau).
Completion of concurrent procedures, such as ACL reconstruction, is then performed. At the completion of the procedure, the medial incision is thoroughly irrigated and closed in a standard layered fashion.
Postoperative Rehabilitation
A full review of rehabilitation is beyond the scope of this article and is strongly influenced by concomitant procedures. However, a brief overview of the rehabilitation protocol for repair of ramp lesions with a concurrent ACL reconstruction is provided.
The patient is allowed weight bearing as tolerated with the aid of crutches for approximately 2 weeks. Physical therapy is initiated on postoperative day one with a focus on edema control, unrestricted knee range of motion, and gait training with crutches. During the first 6 weeks, the patient's primary exercises are patellar mobilizations, both active knee range of motion and wall slides, and quadriceps activation exercises. Crutches are discontinued once the patient is able to ambulate without a limp and perform a straight leg raise without knee extension sag, and typically occurs approximately 2 weeks after surgery. Closed-chain strengthening exercises are initiated after 6 weeks with training periodization focused on first developing muscular endurance, followed by strength and power. Patients may begin straight-ahead running exercises at 5 months, with restrictions on pivoting and twisting. In our practice, gradual return to play progression is initiated after 6 months following the successful completion of a functional sports test. Return to sports or activity is allowed when the patient achieves normal strength, stability, and knee range of motion comparable to the contralateral side; this typically occurs at 7 to 9 months postoperatively.
Discussion
This Technical Note describes our preferred surgical technique for treatment of meniscal ramp lesions, which are defined as a tear of the peripheral attachment of the posterior horn of the medial meniscus at the meniscocapsular junction.1 Treatment of these injuries in the acute setting is recommended in order to maximize healing potential as well as to restore native biomechanics and thereby minimize the risk of injury to associated intra-articular structures.
Both the inside-out7 and all-inside8 techniques to repair ramp lesions have yielded good results in the literature. While the inside-out technique is more technically demanding, this approach affords greater versatility in suture placement and allows the surgeon to pass a greater number of sutures, thereby creating a stronger repair.7, 9 Given the posteromedial location of the ramp lesions, the saphenous neurovascular bundle is at an increased risk during the performance of the inside-out technique of meniscus repair.10 We recommend directly visualizing the posterior capsule to avoid iatrogenic injury to these structures. The all-inside technique has also demonstrated good results and has some advantages: it is less technically demanding, involves a lower risk of neurovascular injury, requires no additional incisions, and is a good option for surgeons with an inexperienced surgical team. Li et al. specifically reported on 23 ramp lesions treated with an all-inside device with a mean follow-up of 14 months.11 The mean Lysholm score improved from 64.4 ± 4.5 preoperatively to 91.2 ± 4.6 postoperatively.11 However, the all-inside technique does have the risks of anchor irritation, meniscal body tears from larger holes created by device insertion, and implant failure.12
The improved outcomes observed in studies when the repair is performed concurrently with an ACL reconstruction have been hypothesized to be related to the biological augmentation of the repair from factors in the bone marrow released within the joint.9 A recent study reported that the concentrations of vascular endothelial growth factor (VEGF) and its angiogenetic receptor VEGF receptor 2 (VEGFR2) were significantly greater after ACL reconstruction than after partial meniscectomy.13 These results indicate a more favorable healing environment when meniscal repairs are performed concurrently with an ACL reconstruction. The authors recommend consideration should be given to biologic augmentation due to the potential positive effects, especially if this procedure is being performed in the absence of other intra-articular reconstructive procedures. A bone marrow stimulation technique known as a marrow venting procedure may be performed by using a microfracture awl to create holes in the notch.14 Additionally, platelet-rich plasma may be injected into the intra-articular space following repair completion and incision closure.
In conclusion, we recommend repair of meniscal ramp lesions, especially in the setting of ACL tears, via the reproducible inside-out technique described in this article. Further biomechanical and clinical studies are indicated to better understand the contribution of ramp lesions to joint laxity and to clarify the precise injury location. It is believed that concurrent repair of ramp lesions at the time of ACL reconstruction protects the graft from increased forces that may be experienced in the setting of meniscal deficiency. Further, despite early promising results of meniscal ramp lesion repair, longer-term studies with increased sample sizes are necessary to evaluate the efficacy and outcomes of meniscal ramp lesion repairs.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: L.E. receives support from Arthrex, Ossur, Siemans, Smith and Nephew, Health East, and a National Institutes of Health grant R-13 for biologics. R.F.L. receives support from Arthrex, Ossur, Siemans, Smith and Nephew, Health East, and a National Institutes of Health grant R-13 for biologics. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is placed in the supine position on the operating table. After the induction of general anesthesia, a bilateral knee examination is performed to assess for range of motion and evaluate for any concurrent ligament instability. A well-padded high-thigh tourniquet is subsequently placed on the operative knee, which is positioned into a leg holder. Standard anterolateral and anteromedial portals are created. A diagnostic arthroscopy is then performed. This patient has an acute right knee complete anterior cruciate ligament tear and combined medial meniscus ramp lesion. The posteromedial capsule is pushed away with the aid of a probe to demonstrate the ramp lesion. To perform an inside-out meniscal repair, a posteromedial approach is taken. The interval between the posteromedial joint capsule (anterior), medial gastrocnemius (posterior), and the semimembranosus (inferior) is developed as described by Chahla et al.4 A suture shuttling device is used to place sutures into the meniscus. With the surgeon applying a valgus force to the joint, the cannula is directed toward the tear under arthroscopic visualization. The surgeon places the knee in 30° of flexion as he or she passes the needle through the meniscus. Once the needle is through the posterior capsule, flexing the knee to 70° to 90° may assist in needle retrieval. The cannula is then redirected to deliver the second needle and place the suture adjacent to the first. It is important to keep slight tension on the suture to avoid inadvertent puncture and laceration of the suture with the second needle. The second suture is placed similarly to the first to create a vertical, oblique, or horizontal pattern. In a similar fashion, multiple sutures are placed between 3 and 5 mm apart. Both femoral- and tibial-sided sutures may be placed. The sutures are clamped, and the individual suture pairs are tied at the end of the procedure. The repair is then checked at the meniscocapsular junction to ensure stability. At the end of the procedure, the incision is thoroughly irrigated and closed in a standard layered fashion.
References
- 1.Bollen S.R. Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament: A previously unrecognised association. J Bone Joint Surg Br. 2010;92:222–223. doi: 10.1302/0301-620X.92B2.22974. [DOI] [PubMed] [Google Scholar]
- 2.Liu X., Feng H., Zhang H., Hong L., Wang X.S., Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39:832–837. doi: 10.1177/0363546510388933. [DOI] [PubMed] [Google Scholar]
- 3.Sonnery-Cottet B., Conteduca J., Thaunat M., Gunepin F.X., Seil R. Hidden lesions of the posterior horn of the medial meniscus: A systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42:921–926. doi: 10.1177/0363546514522394. [DOI] [PubMed] [Google Scholar]
- 4.Strobel M. Springer; New York, NY: 1988. Manual of Arthroscopic Surgery. [Google Scholar]
- 5.Chahla J., Dean C.S., Moatshe G. Meniscal ramp lesions: Anatomy, incidence, diagnosis, and treatment. Orthopaed J Sports Med. 2016;4 doi: 10.1177/2325967116657815. 2325967116657815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DePhillipo N.N., Cinque M.E., Chahla J., Geeslin A., LaPrade R.F. Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in anterior cruciate ligament reconstruction patients. Am J Sports Med. 2017 doi: 10.1177/0363546517704426. (in press) [DOI] [PubMed] [Google Scholar]
- 7.Nelson C.G., Bonner K.F. Inside-out meniscus repair. Arthrosc Tech. 2013;2:e453–e460. doi: 10.1016/j.eats.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haas A.L., Schepsis A.A., Hornstein J., Edgar C.M. Meniscal repair using the FasT-Fix all-inside meniscal repair device. Arthroscopy. 2005;21:167–175. doi: 10.1016/j.arthro.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 9.Hutchinson I.D., Moran C.J., Potter H.G., Warren R.F., Rodeo S.A. Restoration of the meniscus: Form and function. Am J Sports Med. 2014;42:987–998. doi: 10.1177/0363546513498503. [DOI] [PubMed] [Google Scholar]
- 10.Rodeo S. Arthroscopic meniscal repair with use of the outside-in technique. Instr Course Lect. 2000;49:195–206. [PubMed] [Google Scholar]
- 11.Li W.P., Chen Z., Song B., Yang R., Tan W. The FasT-Fix repair technique for ramp lesion of the medial meniscus. Knee Surg Relat Res. 2015;27:56–60. doi: 10.5792/ksrr.2015.27.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grant J.A., Wilde J., Miller B.S., Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: A systematic review. Am J Sports Med. 2012;40:459–468. doi: 10.1177/0363546511411701. [DOI] [PubMed] [Google Scholar]
- 13.Galliera E., De Girolamo L., Randelli P. High articular levels of the angiogenetic factors VEGF and VEGF-receptor 2 as tissue healing biomarkers after single bundle anterior cruciate ligament reconstruction. J Biol Regul Homeost Agents. 2011;25:85–91. [PubMed] [Google Scholar]
- 14.Dean C.S., Chahla J., Matheny L.M., Mitchell J.J., LaPrade R.F. Outcomes after biologically augmented isolated meniscal repair with marrow venting are comparable with those after meniscal repair with concomitant anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:1341–1348. doi: 10.1177/0363546516686968. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed in the supine position on the operating table. After the induction of general anesthesia, a bilateral knee examination is performed to assess for range of motion and evaluate for any concurrent ligament instability. A well-padded high-thigh tourniquet is subsequently placed on the operative knee, which is positioned into a leg holder. Standard anterolateral and anteromedial portals are created. A diagnostic arthroscopy is then performed. This patient has an acute right knee complete anterior cruciate ligament tear and combined medial meniscus ramp lesion. The posteromedial capsule is pushed away with the aid of a probe to demonstrate the ramp lesion. To perform an inside-out meniscal repair, a posteromedial approach is taken. The interval between the posteromedial joint capsule (anterior), medial gastrocnemius (posterior), and the semimembranosus (inferior) is developed as described by Chahla et al.4 A suture shuttling device is used to place sutures into the meniscus. With the surgeon applying a valgus force to the joint, the cannula is directed toward the tear under arthroscopic visualization. The surgeon places the knee in 30° of flexion as he or she passes the needle through the meniscus. Once the needle is through the posterior capsule, flexing the knee to 70° to 90° may assist in needle retrieval. The cannula is then redirected to deliver the second needle and place the suture adjacent to the first. It is important to keep slight tension on the suture to avoid inadvertent puncture and laceration of the suture with the second needle. The second suture is placed similarly to the first to create a vertical, oblique, or horizontal pattern. In a similar fashion, multiple sutures are placed between 3 and 5 mm apart. Both femoral- and tibial-sided sutures may be placed. The sutures are clamped, and the individual suture pairs are tied at the end of the procedure. The repair is then checked at the meniscocapsular junction to ensure stability. At the end of the procedure, the incision is thoroughly irrigated and closed in a standard layered fashion.