Abstract
The meniscus roots are critical for meniscus function in preserving correct knee kinematics and avoiding meniscus extrusion and, consequently, in the progression of osteoarthritis. Several techniques exist for medial meniscus posterior root tear repair; however, current surgical techniques have been proved to fail to reduce meniscus extrusion, which has been shown to be associated with development of osteoarthritis, although significant improvements in the postoperative clinical findings have been achieved. This Technical Note describes an arthroscopic technique for the medial meniscus posterior root tear in which a pullout repair is augmented by a centralization technique to restore and maintain the medial meniscus function by efficiently reducing meniscus extrusion.
As the importance of the posterior root of the medial meniscus (MM) has been particularly recognized, surgeons have been trying to repair the medial meniscus posterior root tear (MMPRT). However, current surgical techniques for MMPRT repair have been proved to fail to reduce meniscus extrusion, which has been shown to be associated with development of osteoarthritis (OA),1 although significant improvements in the postoperative clinical findings have been achieved.2 Therefore, a surgical technique that efficiently reduces meniscus extrusion and maintains its position for a long period to repair the MMPRT should be developed. Recently, an arthroscopic centralization technique has been developed to restore and maintain the meniscus function by repairing or preventing extrusion of the meniscus by centralizing the midbody of the meniscus onto the rim of the tibial plateau. Good clinical and radiographic outcomes of this procedure for lateral meniscus extrusion have been reported.3, 4 This Technical Note describes an arthroscopic technique for the MMPRT in which a pullout repair is augmented by a centralization technique to restore and maintain the MM function by efficiently reducing meniscus extrusion.
Indications
This technique is indicated for the MMPRT with a complete radial tear 0 to less than 6 mm from the posterior bony attachment of the MM (LaPrade classification type 2A or 2B5). A trial of conservative therapy should be considered first in patients with normal lower extremity alignment without meniscus extrusion greater than 3 mm, bone marrow lesions, and cartilage damage. If patients have varus alignment (percent mechanical axis <50%), simultaneous high tibial osteotomy should be considered.
Surgical Technique
The patient is positioned supine on a standard operating table (Video 1). A nonsterile tourniquet is applied to the upper thigh of the operated leg.
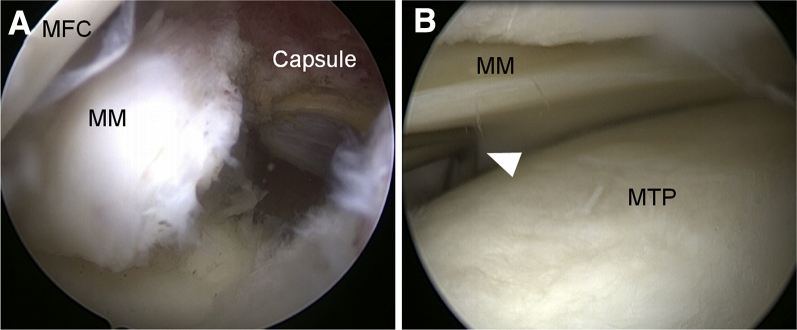
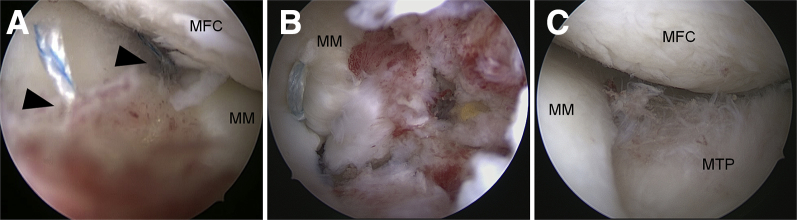
A standard arthroscopic examination is performed through routine anteromedial and anterolateral portals. Other injuries including osteochondral lesions are managed according to the injury status. The MMPRT is confirmed with arthroscopic viewing from the anterolateral portal (Fig 1A). Extrusion of the MM is also confirmed by pushing the midbody of the meniscus out of the rim of the medial tibial plateau by use of a probe (Fig 1B). A 3-cm skin incision is made at the anteromedial aspect of the proximal tibia, and the superficial medial collateral ligament is released at the distal tibial side with a rasp to provide sufficient working space.
Fig 1.
Arthroscopic images of left medial meniscus (MM) posterior root tear, with patient positioned supine. (A) The MM posterior root tear is confirmed with arthroscopic viewing from the anterolateral portal after fibrous tissues around the torn meniscus edge are removed. (MFC, medial femoral condyle.) (B) Extrusion of the MM is confirmed by pushing the midbody of the meniscus out of the rim of the medial tibial plateau (MTP) using a probe (arrowhead).
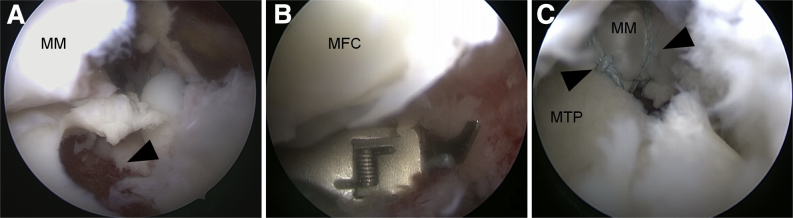
Fibrous tissues around the torn meniscus edge are removed, and adhesion around the torn meniscus edge is released with a motorized shaver. A Multi-use RetroConstruction Marking Hook with a RetroConstruction ACL guide (Arthrex, Naples, FL) is inserted from the anteromedial portal, with the marking hook placed over the attachment site of the MM posterior root. A 2.4-mm guidewire is inserted from the anteromedial aspect of the proximal tibia, and a 6-mm-diameter tunnel is then created with a cannulated drill (Fig 2A). The 6-mm-diameter tunnel allows the meniscus and bone to heal by pulling the torn edge of the MM posterior root into the tunnel.
Fig 2.
Arthroscopic images of left medial meniscus (MM) posterior root tear, with patient positioned supine. (A) A 6-mm-diameter tunnel (arrowhead) is created at the attachment site of the MM posterior root. (B) The loop end of the suture is passed through the meniscus approximately 5 mm from the torn edge with a suture passer. (MFC, medial femoral condyle.) (C) Two racking hitch knot sutures (arrowheads) are placed and shuttled transtibially through the tunnel to the anteromedial aspect of the proximal tibia. (MTP, medial tibial plateau.)
A PassPort Button Cannula (Arthrex) is inserted into the anteromedial portal to ease suture and instrument passage. A Knee Scorpion Suture Passer (Arthrex), preloaded with No. 2-0 FiberWire (Arthrex) in the bottom jaw of the instrument at the halfway point of the FiberWire, is inserted through the cannula. The loop end of the suture is passed through the meniscus approximately 5 mm from the torn edge (Fig 2B). Once the loop end of the suture is passed, it is grabbed with the Scorpion device and pulled out of the portal, creating a racking hitch knot, and the knot is drawn into the joint to securely hold the torn edge of the meniscus. The same procedure is repeated, and in total 2 sutures are placed. The sutures are then shuttled transtibially through the tunnel to the anteromedial aspect of the proximal tibia (Fig 2C).
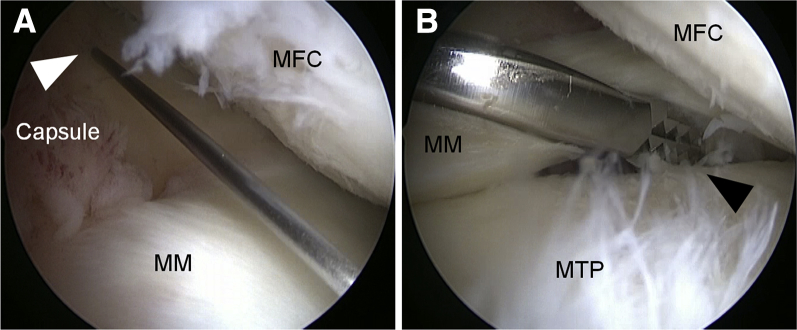
A midmedial portal is made with arthroscopic viewing from the anterolateral portal, 1 cm proximal to the MM and just anterior to the medial femoral condyle (Fig 3A). An arthroscopic rasp, usually used for shoulder Bankart repair, is inserted through the midmedial portal. The meniscotibial capsule under the MM is sufficiently released from the medial tibial plateau from anterior to posterior for mobilization of the MM to ease reduction of the torn posterior root to the anatomic insertion site, as well as reduction of the meniscus extrusion (Fig 3B).
Fig 3.
Arthroscopic images of left medial meniscus (MM) posterior root tear, with patient positioned supine. (A) A midmedial portal (arrowhead) is made with arthroscopic viewing from the anterolateral portal, 1 cm proximal to the MM and just anterior to the medial femoral condyle (MFC). (B) The meniscotibial capsule under the MM is released from the medial tibial plateau (MTP) from anterior to posterior with an arthroscopic rasp (arrowhead).
A JuggerKnot Soft Anchor loaded with a MaxBraid (Zimmer Biomet, Warsaw, IN) is inserted on the edge of the medial tibial plateau, as posterior as possible through the midmedial portal (Fig 4A). The extruded MM is easily moved away by the probe and protected by a cannula for the anchor. A Micro SutureLasso Small Curve with Nitinol Wire Loop (Arthrex) is then inserted through the midmedial portal. The tip of the Micro SutureLasso penetrates the capsule from superior to inferior at the margin between the meniscus and the capsule, slightly anterior to the insertion point of the anchor (Fig 4B). The anterior penetration allows the midbody of the MM to move posteriorly and consequently to ease reduction of the MMPRT. One strand of MaxBraid is passed into the wire loop, and the other limb of the wire loop is pulled to pass the MaxBraid from inferior to superior. The same procedure is repeated for another strand of MaxBraid to create a mattress suture configuration (Fig 4C).
Fig 4.
Arthroscopic images of left medial meniscus (MM) posterior root tear, with patient positioned supine. (A) A JuggerKnot Soft Anchor is inserted on the edge of the medial tibial plateau (MTP). (B) A Micro SutureLasso Small Curve is inserted and penetrates the capsule from superior to inferior at the margin between the meniscus and the capsule, slightly anterior to the insertion point of the anchor (arrow). (C) A mattress suture configuration is created at the margin between the meniscus and capsule (arrowheads). (MFC, medial femoral condyle.)
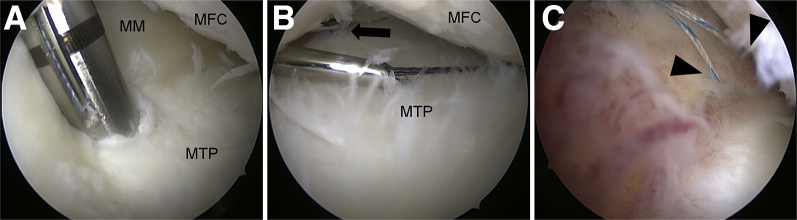
Another JuggerKnot Soft Anchor is inserted on the edge of the medial tibial plateau, 1 cm anterior to the first anchor, and the same procedure is repeated. The passed sutures are then tied through the midmedial portal by use of a self-locking sliding knot (Fig 5A). When the knot is being tied, sutures placed at the torn edge of the MM posterior root are also pulled to help reduce the extruded meniscus. The extruded MM is reduced and centralized with this centralization procedure.
Fig 5.
Arthroscopic images of left medial meniscus (MM) posterior root tear, with patient positioned supine. (A) The sutures are tied through the midmedial portal with a self-locking sliding knot (arrowheads). (B) After the suture ends for the MM posterior root tear are tied under adequate tension, reattachment of the MM posterior root to the insertion site is confirmed. (C) The extruded MM is reduced and centralized after augmentation of the pullout repair by arthroscopic centralization. (MFC, medial femoral condyle; MTP, medial tibial plateau.)
With arthroscopic viewing from the anterolateral portal, the suture ends for the MMPRT are finally tied over a TightRope ABS Button (Arthrex) under adequate tension. A final arthroscopic evaluation is performed to confirm reattachment of the MM posterior root to the insertion site (Fig 5B), adequate tension within the entire meniscus, and reduction of the extruded meniscus (Fig 5C). The tips and pitfalls of this technique are described in Table 1.
Table 1.
Tips and Pitfalls
| Tips | Pitfalls |
|---|---|
| • Position the transtibial tunnel for the pullout repair at the anatomic footprint of the MM posterior root insertion site. | • Instruments such as the tibial tunnel guide, suture passer, and rasp should be handled carefully to avoid chondral damage. |
| • Place a cannula in the portal to ease suture and instrument passage for the pullout repair. | • Pullout suture fixation before the centralization procedure makes it difficult to perform centralization. |
| • Use an arthroscopic rasp to release the meniscotibial capsule to mobilize the MM centrally and posteriorly. | • The Micro SutureLasso should penetrate the capsule at the margin between the meniscus and the capsule during the centralization procedure. Penetration of the meniscus body would result in overconstraint of the MM. |
| • Place capsular sutures for the centralization anterior to the anchor to allow the MM to move posteriorly and, consequently, to ease reduction of the MMPRT. |
MM, medial meniscus; MMPRT, medial meniscus posterior root tear.
Postoperative Rehabilitation
After surgery, the patient undergoes a routine postoperative protocol for meniscus repair. Namely, range-of-motion exercise without restriction is encouraged immediately after the operation. Partial weight bearing with a knee immobilizer and crutches is allowed for the first 4 weeks. After 4 weeks, partial weight bearing without the knee immobilizer is permitted, with a progression to full weight bearing at 6 weeks. Deep squatting over 90° is allowed after 3 months. Running is permitted after 3 months, and full athletic activities are allowed 6 months after surgery.
Discussion
The meniscus attaches strongly to the tibia through the meniscus root, and the meniscus roots are critical for meniscus function in preserving correct knee kinematics and in avoiding meniscus extrusion and, consequently, progression of OA.6 Particularly, the importance of repairing the MMPRT has been recognized. However, a recent meta-analysis examining the treatment effects of the MMPRT repair showed that, although significant improvements in the postoperative clinical findings were achieved, meniscus extrusion was not reduced, and current MMPRT repair surgical procedures did not prevent the progression of arthrosis completely.2 In addition, a more recent study showed that the number of patients with decreased extrusion was less than the number with increased extrusion, and patients with decreased meniscus extrusion have more favorable clinical and radiologic results after the MMPRT repair.7
There are several possible reasons the MMPRT repair has failed to reduce meniscus extrusion. One main reason could be that the MMPRT is commonly associated with degenerative changes. Therefore, the torn edge of the MMPRT would already be degenerated, and the sutures at the torn edge alone could not hold the MM at a reduced position, even with the reported secure fixation methods.8 Another reason could be adhesion of the extruded meniscus, together with the adjacent joint capsule, to the medial tibial plateau distal to the medial edge, thereby resulting in difficulty in reducing meniscus extrusion just by pulling the sutures.
Koga et al.3, 4 developed an arthroscopic centralization technique for lateral meniscus extrusion in which the midbody of the lateral meniscus is centralized and stabilized onto the rim of the lateral tibial plateau to restore and maintain the lateral meniscus function by repairing or preventing extrusion of the meniscus. They reported good 2-year clinical and radiologic outcomes of this procedure for lateral meniscus extrusion. We applied this technique to the MMPRT to augment the current pullout repair technique. The advantages of this technique are as follows: (1) Meniscus extrusion is reduced by the centralization technique itself regardless of pullout repair; thereby, the load-absorbing function of the MM can be restored. (2) Sutures for the centralization can share the load with those for the pullout repair, so the failure risk of the pullout sutures at the torn edge can be reduced (Table 2). On the other hand, this technique is more technically demanding and could present a risk to limit normal motion of the MM during knee extension-flexion. Moreover, this is a preliminary report, and further follow-up will be necessary to investigate the long-term effect of the centralization augmentation on clinical and radiologic outcomes. Nevertheless, the augmentation of the MMPRT repair by arthroscopic centralization can possibly reduce meniscus extrusion and maintain meniscus function and eventually prevent progression of OA.
Table 2.
Advantages and Limitations of Technique
| Advantages | Limitations |
|---|---|
| • Meniscus extrusion is reduced by the centralization technique itself regardless of pullout repair. | • The technique is technically demanding. |
| • The sutures for centralization can share the load with those for the pullout repair, so the failure risk of the pullout sutures at the torn edge can be reduced. | • The centralization could present a risk to limit normal motion of the MM during knee extension-flexion. |
MM, medial meniscus.
Acknowledgment
The authors thank Atsushi Okawa, M.D., Ph.D., for continuous support and Ronald G. Belisle for English correction.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Case of medial meniscus (MM) posterior root tear in a left knee. The MM posterior root tear, as well as extrusion of the MM, is confirmed. A 6-mm-diameter tunnel is created at the attachment site of the MM posterior root. A Knee Scorpion Suture Passer is used to create a racking hitch knot, and in total 2 sutures are placed. The sutures are then shuttled through the tunnel to the anteromedial aspect of the proximal tibia. A midmedial portal is made 1 cm proximal to the MM and just anterior to the medial femoral condyle. The meniscotibial capsule under the MM is released from the medial tibial plateau with an arthroscopic rasp. Two JuggerKnot Soft Anchors are inserted on the edge of the medial tibial plateau. A Micro SutureLasso is used to penetrate the capsule at the margin between the meniscus and the capsule, slightly anterior to the insertion point of the anchor. A suture relay is used to create a mattress suture configuration. The passed sutures are then tied with a self-locking sliding knot. The suture ends for the root tear are finally tied over a button. A final arthroscopic evaluation confirms that the posterior root is reattached to the insertion site and the extruded meniscus is centralized.
References
- 1.Berthiaume M.J., Raynauld J.P., Martel-Pelletier J. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64:556–563. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung K.S., Ha J.K., Ra H.J., Kim J.G. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc. 2016;24:1455–1468. doi: 10.1007/s00167-015-3832-0. [DOI] [PubMed] [Google Scholar]
- 3.Koga H., Muneta T., Yagishita K. Arthroscopic centralization of an extruded lateral meniscus. Arthrosc Tech. 2012;1:e209–e212. doi: 10.1016/j.eats.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koga H., Muneta T., Watanabe T. Two-year outcomes after arthroscopic lateral meniscus centralization. Arthroscopy. 2016;32:2000–2008. doi: 10.1016/j.arthro.2016.01.052. [DOI] [PubMed] [Google Scholar]
- 5.LaPrade C.M., James E.W., Cram T.R., Feagin J.A., Engebretsen L., LaPrade R.F. Meniscal root tears: A classification system based on tear morphology. Am J Sports Med. 2015;43:363–369. doi: 10.1177/0363546514559684. [DOI] [PubMed] [Google Scholar]
- 6.Lerer D.B., Umans H.R., Hu M.X., Jones M.H. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33:569–574. doi: 10.1007/s00256-004-0761-2. [DOI] [PubMed] [Google Scholar]
- 7.Chung K.S., Ha J.K., Ra H.J., Nam G.W., Kim J.G. Pullout fixation of posterior medial meniscus root tears: Correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017;45:42–49. doi: 10.1177/0363546516662445. [DOI] [PubMed] [Google Scholar]
- 8.LaPrade R.F., LaPrade C.M., Ellman M.B., Turnbull T.L., Cerminara A.J., Wijdicks C.A. Cyclic displacement after meniscal root repair fixation: a human biomechanical evaluation. Am J Sports Med. 2015;43:892–898. doi: 10.1177/0363546514562554. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Case of medial meniscus (MM) posterior root tear in a left knee. The MM posterior root tear, as well as extrusion of the MM, is confirmed. A 6-mm-diameter tunnel is created at the attachment site of the MM posterior root. A Knee Scorpion Suture Passer is used to create a racking hitch knot, and in total 2 sutures are placed. The sutures are then shuttled through the tunnel to the anteromedial aspect of the proximal tibia. A midmedial portal is made 1 cm proximal to the MM and just anterior to the medial femoral condyle. The meniscotibial capsule under the MM is released from the medial tibial plateau with an arthroscopic rasp. Two JuggerKnot Soft Anchors are inserted on the edge of the medial tibial plateau. A Micro SutureLasso is used to penetrate the capsule at the margin between the meniscus and the capsule, slightly anterior to the insertion point of the anchor. A suture relay is used to create a mattress suture configuration. The passed sutures are then tied with a self-locking sliding knot. The suture ends for the root tear are finally tied over a button. A final arthroscopic evaluation confirms that the posterior root is reattached to the insertion site and the extruded meniscus is centralized.