Abstract
Preservation of the meniscus has been shown to influence the progression of degenerative changes of the knee. As more meniscus is preserved, the propensity for development of osteoarthritis is lessened. Surgical treatment of a torn discoid meniscus has typically been a subtotal meniscectomy or partial meniscectomy. Similar to tears of a normal meniscus, partial meniscectomy compared with subtotal meniscectomy of the discoid meniscus confers better long-term results. With the abnormal morphology predisposing the discoid meniscus to tearing, several characteristic tear patterns can be observed—the horizontal tear being commonly encountered. We present a technique that not only creates a more normal morphology of a discoid meniscus but also preserves the tissue by using an all-inside, intrameniscal repair technique. This technique restores the central rim of the meniscus in the setting of a horizontal cleavage plane, thus restoring a more normal meniscus morphology.
The discoid meniscus is a common anatomic variant and is usually associated with the lateral meniscus of the knee.1 It is estimated that around 1% to 3% of the pediatric population in the United States shows this variant, with approximately 10% to 20% of the cases showing bilaterally.2 Although most discoid meniscus variants are asymptomatic and do not require surgical intervention, the condition predisposes the meniscus to tearing. A symptomatic discoid meniscus can cause increased pain and mechanical symptoms, such as popping, snapping, giving way of the knee, and decreased knee extension.3 Past treatment for this condition has been partial or total meniscectomy; however, long-term results have shown a high prevalence of early degenerative changes.4, 5 Recently, long-term results of central partial meniscectomy and subtotal and total meniscectomy have suggested a decrease in degenerative changes after 10 years when partial meniscectomy is performed.4 Although degenerative changes were still present in 23% to 39% of these patients,4 the torn tissue was removed rather than repaired. Additional long-term studies report degenerative changes with subtotal meniscectomy for a torn discoid meniscus.5, 6 When presented with a torn discoid meniscus, efforts should be made to construct a meniscus that closely resembles the normal meniscus morphology. With the recent advancements of arthroscopic techniques and instruments, increasing opportunities to preserve more meniscal tissue can be exploited.
Past literature describes several tear patterns of the discoid meniscus with the horizontal tear frequently encountered.7 The goal of this technique is to debride and saucerize the central portion of the discoid tissue and to create the most normal meniscus morphology by means of an all-inside repair. The advantages and limitations of arthroscopic repair of a horizontal tear of a discoid meniscus are outlined in Table 1. Our described technique shows the operative repair of a horizontal tear of the inner portion of a lateral discoid meniscus. After debridement, a suture passing device is used to cinch the upper and lower tissue planes of the remaining central meniscus tissue to establish a normal, beveled morphology (Video 1).
Table 1.
Advantages, Limitations, Pearls, and Pitfalls
| Advantages |
| • Torn peripheral meniscus tissue is preserved to resemble the normal meniscus morphology |
| • All-inside technique spares additional incisions, tissue disruption, and does not require capsule fixation |
| • Full visualization of the repair is afforded by the all-inside, intrameniscal technique |
| • Full thickness, superior to inferior sutures compress both tissue planes evenly |
| • Efficient technique without neurovascular risk |
| • Implications and applications for repair of peripheral horizontal tears or cleavage planes in nondiscoid patients |
| Limitations |
| • Does not address a hypermobile (Wrisberg, type III) discoid meniscus because no capsular fixation is used |
| • Requires high-quality tissue and tears that extend into the peripheral third of the meniscus, which confers vascularity for healing |
| Pearls |
| • Careful central debridement will preserve tissue to establish normal morphology |
| • Use a rasp to gently debride the horizontal cleft to stimulate healing in the tissue |
| • Position the sutures 2-3 mm from the meniscocapsular junction through the peripheral aspect of the tear for effective cinching and tissue plane compression |
| • Use low-profile locking Weston knots to avoid chondral burden of knots |
| • Use valgus stress and figure-of-four positioning to optimize clearance for suture passing |
| Pitfalls |
| • Excessive debridement can eliminate the ability to create a normal meniscus shape |
| • Vertical needle trajectory may damage the articular cartilage |
| • Suture placement too medially or too laterally of the tear may not properly cinch the tissue planes together |
| • Inadequate chondral clearance for suture passing may result in iatrogenic chondral injury |
Surgical Technique
Imaging and Indications
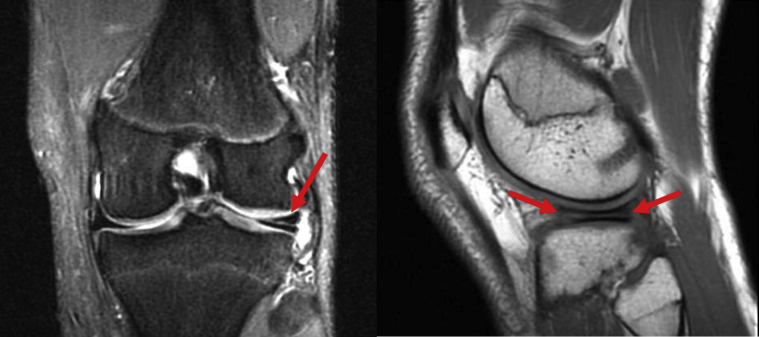
This technique is indicated for patients who are diagnosed with horizontal tear of a discoid meniscus. The repair technique of the horizontal tear can also be applied to the normal meniscus when this type of tear is encountered. Physical examination may be positive for joint line tenderness, McMurray test, Thessaly test, and other provocative maneuvers. Magnetic resonance imaging is most commonly used to identify both the discoid meniscus and the horizontal tear (Fig 1).
Fig 1.
A coronal T2 magnetic resonance image of the left knee (left) showing hyperintensity in the lateral meniscus (arrow) characteristic of a horizontal tear of a discoid lateral meniscus. Sagittal T1 magnetic resonance image (right) showing the horizontal tear (arrows).
Surgical Approach
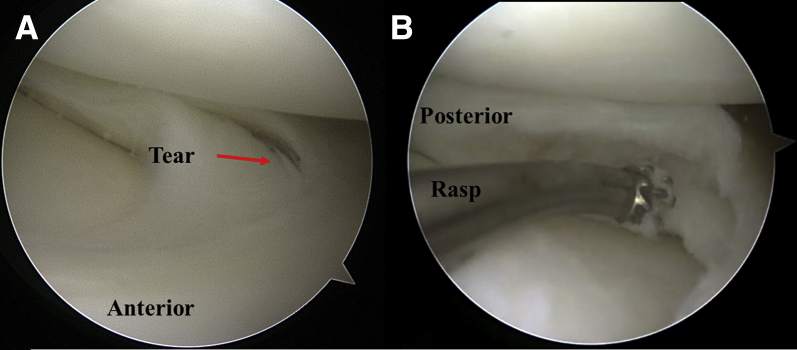
The procedure is performed with the patient under general anesthesia in the supine position. The knee is prepped and draped in a standard fashion. Standard anteromedial (AM) and anterolateral (AL) portals are established, and diagnostic arthroscopy is subsequently performed. The knee is placed in the figure-of-four position with the arthroscope in the AL portal, allowing full visualization of a torn, Watanabe type II discoid lateral meniscus (DLM) (Fig 1). Through the AM portal, the meniscus is probed to assess for hypermobility and to ensure stability of its peripheral attachments. After thorough inspection of the tear, this DLM shows a tear that breaches the superior surface of the meniscus and extends lateral into the body in a horizontal fashion (Fig 2).
Fig 2.
Left knee viewing from the anterolateral portal. Partial discoid lateral meniscus showing horizontal tear that breaches the superior tissue plane and extends laterally into the body of the meniscus (A). After the central tissue has been debrided, an arthroscopic rasp is used to freshen the cleavage (B).
Central Partial Discoid Meniscectomy
While viewing through the AL portal, an arthroscopic biter (Arthrex, Naples, FL) is used to remove the central tissue. The central tissue is removed to create the ellipse or saucer shape of the normal meniscus. Care is taken not to remove more than the estimated width of a normal meniscus. An arthroscopic shaver is then used to smooth and chamfer both superior and inferior tissue planes. Next, through the AM portal, an arthroscopic rasp is inserted between the 2 tissue planes of the DLM (Fig 2). The rasp is used to stimulate the tissue in the cleft. A spinal needle is then used to trephinate the capsular tissue for further stimulation to facilitate healing.
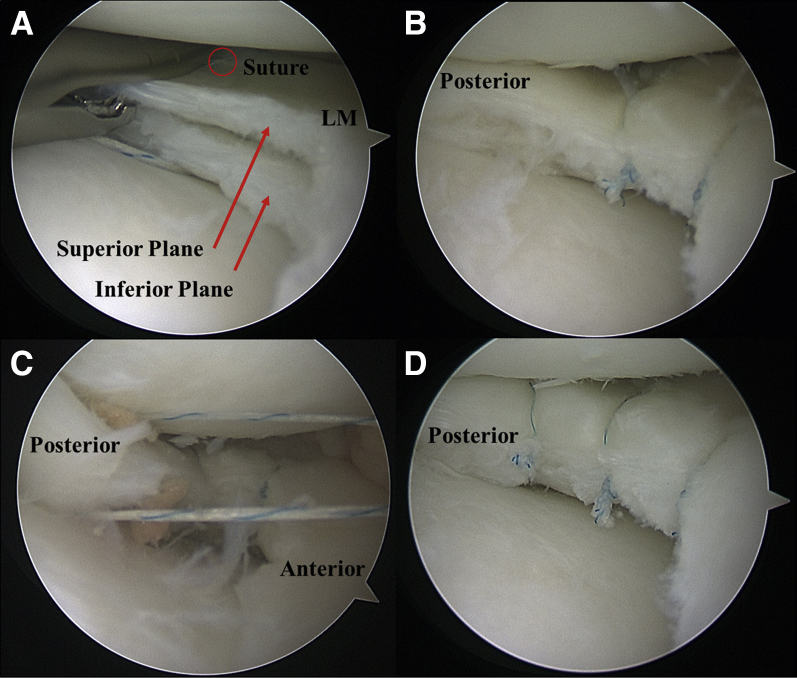
Repair of Horizontal Tear
Beginning centrally, a suture passing device is inserted through the AM portal to grasp the superior and inferior planes of the horizontal tear. The Novostitch (Ceterix, Fremont, CA) suture passing device used in this technique has a retractable lower jaw that improves the maneuverability, allowing for increased accuracy of suture placement. In addition, the needle exits in close alignment with the longitudinal axis of the device; thus the risk of iatrogenic chondral injury to the lateral femoral condyle is reduced. Another suture passing devices can be used in this repair; however, extra care must be taken when passing the suture. The first suture is placed centrally in the body of the lateral meniscus (Fig 3). The trajectory is aimed such that the suture passes through the lateral half of the width of the tear, compressing the 2 planes together. The suture is pulled medially from the AM portal. Another suture is placed anterior to the first (Fig 3). The Knee Scorpion (Arthrex) is shown with this suture, and the needle tip is carefully directed away from the articular cartilage (Video 1). Cartilage clearance can be optimized medially by valgus stress and laterally with the figure-of-four position. Using an arthroscopic knot pusher, 3 locking arthroscopic Weston knots followed by 2 alternating half hitches are used to cinch the 2 tissue planes into a single, continuous construct. The arthroscope is then placed through the AM portal and the suture passing device is placed through the AL portal to access the posterior section of the tear. A third suture is placed through both tissue planes and cinched in a similar fashion (Fig 3). The knots are carefully placed at the junction of the 2 planes so as to maintain a low-profile repair in addition to enabling the cinching of the repair. To maximize the healing potential, a marrow stimulation technique is applied to the femoral notch. After clearing the periosteal tissue just superior to the femoral anterior cruciate ligament insertion in the femoral notch, a Steadman awl is used to perforate the subchondral plate. The tourniquet released and marrow elements are visualized pouring into the joint space.
Fig 3.
Left knee, lateral meniscus (LM), viewing portal anterolateral (A, B, and D) and anteromedial (C). A suture passing device is shown with a vertical suture passing through both the inferior and superior tissue planes with the suture exiting superiorly, marked by the circle (A). Two sutures cinch the superior and inferior tissue planes of the horizontal tear (B). The third suture is placed through the posterior aspect of the horizontal tear (C), finalizing the repair construct and creating the shape of a normal meniscus (D).
Postoperative Rehabilitation
Postoperatively, a brace locked in extension is used for 4 weeks. The patient remains non-weight-bearing for the first week, progressing to weight bearing as tolerated for 4 weeks, and then to normal gait training after 4 weeks, unlocking the brace at this time once the patient achieves adequate quadriceps control, shown by no lag with a straight leg raise. After 6 weeks, the patient should achieve normal weight bearing. Range of motion should focus on achieving 0° to 90° for the first 4 weeks and progressing to normal range of motion thereafter without flexion loading beyond 90° until 6 weeks. Strength rehabilitation should focus on muscle control and isometric exercises for the first week after which quadriceps and hamstring exercises should escalate gradually. Squatting and hyperflexion are allowed at 4 months. Running is initiated at 3 months and return to sports at 4 months provided they have achieved full range of motion, strength, and neuromuscular control.
Discussion
Meniscectomy has long been associated with the development of osteoarthritis.8 In the setting of a DLM, partial meniscectomy results in less degenerative changes than subtotal meniscectomy. The application of this repair technique preserves additional meniscus tissue that would have otherwise been removed if a partial meniscectomy were performed. This saucerization and repair technique can be used as a meniscus sparing alternative to the traditional partial or subtotal meniscectomies that have been reported in the literature for a torn DLM.4, 9 As more meniscal tissue is removed, as in partial and subtotal meniscectomies, acceleration of osteoarthritis is increased, and thus the meniscus should be preserved when possible.4, 8
The described technique has several advantages (Table 1). First and foremost, preservation of meniscal tissue is achieved by repairing the horizontal tear. Secondly, the normal crescent shape of the meniscus is created by careful debridement of the central tissue of the DLM. As this construct more closely resembles the normal meniscus morphology, an advantage can be inferred from this technique. Furthermore, because no sutures are passed through the capsule, neurovascular risk is minimal. Limitations are related to the required devices used for suture passing. The needle follows a vertical trajectory for some devices, which necessitates careful positioning to avoid chondral injury. As shown in this technique, it is possible to use this style of device; however, with a needle trajectory away from the articular cartilage (horizontal trajectory), this concern is less relevant. If a suture passing device with a vertical trajectory is used, precise positioning for adequate cartilage clearance to avoid iatrogenic chondral damage is paramount and may not be advisable if this clearance cannot be achieved. Horizontal tears are common, and because this technique can be applied using general knee arthroscopy skills, the feasibility of this technique is high. This all-inside, intrameniscal repair technique restores an intact central rim in the setting of a delaminated horizontal cleavage plane, thus creating a more normal meniscus morphology.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: B.F. receives consultancy fees, has grants/grants pending from Stryker (research support), and receives fellowship support from Arthrex and Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
A technique for saucerization and repair of a horizontal tear of a discoid meniscus in a left knee is shown and explained. Inspection of the extent of the tear and assessment of meniscal stability is followed by careful debridement of the central discoid tissue. To preserve the meniscal tissue that encompasses the area of the normal meniscus, the horizontal tear is repaired using 3 vertical sutures passed through both the inferior and superior tissue planes. The sutures cinch the 2 tissue planes together, creating a single continuous construct.
References
- 1.Kushare I., Klingele K., Samora W. Discoid meniscus. Orthop Clin North Am. 2015;46:533–540. doi: 10.1016/j.ocl.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Hart E.S., Kalra K.P., Grottkau B.E., Albright M., Shannon E.G. Discoid lateral meniscus in children. Orthop Nurs. 2008;27:174–179. doi: 10.1097/01.NOR.0000320545.35858.04. [DOI] [PubMed] [Google Scholar]
- 3.Good C.R., Green D.W., Griffith M.H., Valen A.W., Widmann R.F., Rodeo S.A. Arthroscopic treatment of symptomatic discoid meniscus in children: Classification, technique, and results. Arthroscopy. 2007;23:157–163.e151. doi: 10.1016/j.arthro.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Ahn J.H., Kim K.I., Wang J.H., Jeon J.W., Cho Y.C., Lee S.H. Long-term results of arthroscopic reshaping for symptomatic discoid lateral meniscus in children. Arthroscopy. 2015;31:867–873. doi: 10.1016/j.arthro.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 5.Okazaki K., Miura H., Matsuda S., Hashizume M., Iwamoto Y. Arthroscopic resection of the discoid lateral meniscus: Long-term follow-up for 16 years. Arthroscopy. 2006;22:967–971. doi: 10.1016/j.arthro.2006.04.107. [DOI] [PubMed] [Google Scholar]
- 6.Kose O., Celiktas M., Egerci O.F., Guler F., Ozyurek S., Sarpel Y. Prognostic factors affecting the outcome of arthroscopic saucerization in discoid lateral meniscus: A retrospective analysis of 48 cases. Musculoskelet Surg. 2015;99:165–170. doi: 10.1007/s12306-015-0376-x. [DOI] [PubMed] [Google Scholar]
- 7.Elvey M.H., Konan S., House C.V., Patel R.V. Horizontal cleavage tear of discoid medial meniscus diagnosed on MRI and treated with arthroscopic partial resection. Knee Surg Sports Traumatol Arthrosc. 2011;19:1860–1867. doi: 10.1007/s00167-011-1487-z. [DOI] [PubMed] [Google Scholar]
- 8.Petty C.A., Lubowitz J.H. Does arthroscopic partial meniscectomy result in knee osteoarthritis? A systematic review with a minimum of 8 years' follow-up. Arthroscopy. 2011;27:419–424. doi: 10.1016/j.arthro.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 9.Chedal-Bornu B., Morin V., Saragaglia D. Meniscoplasty for lateral discoid meniscus tears: Long-term results of 14 cases. Orthop Traumatol Surg Res. 2015;101:699–702. doi: 10.1016/j.otsr.2015.06.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A technique for saucerization and repair of a horizontal tear of a discoid meniscus in a left knee is shown and explained. Inspection of the extent of the tear and assessment of meniscal stability is followed by careful debridement of the central discoid tissue. To preserve the meniscal tissue that encompasses the area of the normal meniscus, the horizontal tear is repaired using 3 vertical sutures passed through both the inferior and superior tissue planes. The sutures cinch the 2 tissue planes together, creating a single continuous construct.