Abstract
Hamstring tendon autograft remains a popular graft choice for anterior cruciate ligament (ACL) reconstruction. Although there are a variety of autograft and allograft options available for ACL reconstruction, advantages of hamstring tendon autografts include decreased postoperative knee pain and an overall easier surgical recovery compared with bone patellar tendon bone autograft. In addition, 4-stranded (quadruple) hamstring grafts are among the strongest grafts biomechanically (at time equals zero). Although the technique of hamstring autograft harvest is relatively straightforward, it is critical to pay attention to several technical steps to avoid iatrogenic neurovascular damage as well as to avoid premature amputation of the graft while using a tendon stripper. In this Technical Note, we describe a technique of hamstring autograft harvest for ACL reconstruction for a quadruple (4-strand) hamstring graft using the gracilis and semitendinosus tendons.
The use of hamstring autograft for anterior cruciate ligament (ACL) reconstruction was first reported in 1934 with the use of the semitendinosus tendon.1 Advancements in surgical techniques have led surgeons to use 2 hamstring tendons for ACL autograft reconstruction with both the semitendinosus and gracilis tendons in a 4-stranded construct. Over 200,000 ACL reconstructions are performed annually in the United States,2 with the use of hamstring autografts and patellar tendon autografts among the most common choices for reconstruction.3
While all autograft choices for ACL reconstruction have strengths and weaknesses, advantages of hamstring tendon grafts specifically include reduced postoperative patellofemoral crepitation, anterior knee pain, extension loss, and donor site morbidity, as well as smaller skin incisions at the harvest site when compared to patellar tendon autografts.3 Despite this, some studies have shown increased joint laxity and functional hamstring weakness when compared with ACL reconstruction with patellar tendon grafts.3 Currently there is insufficient evidence to conclude which graft type produces superior long-term functional outcomes following ACL reconstruction.3
Knowledge of peri-hamstring neurovascular and musculoskeletal anatomy is crucial for a successful harvest with minimal postoperative morbidity. To ensure appropriate graft size and biomechanical function, it has been recommended to use grafts at least 8 mm in diameter to replicate the native ACL diameter.4 Hamstring tendons have been shown to have variable diameters, a characteristic of the graft that cannot be adjusted for, which can be problematic in the setting of a smaller tendon. In contrast, the width of the graft harvested from the central third of the patellar tendon can be modified as needed based on the patient's individual anatomy.5 To reach the minimum 8 mm overall graft diameter, the harvested semitendinosus and gracilis tendons are typically folded to create a 4-stranded graft, which results in the stiffest biomechanical construct compared to patellar tendon, quadriceps tendon, and Achilles tendon grafts.4
In this Technical Note, we describe a reproducible technique of hamstring autograft harvest for ACL reconstruction for a quadruple (4-strand) hamstring graft using the gracilis and semitendinosus tendons. A summary of key steps is provided in Table 1, and a summary of the technique is provided in Video 1.
Table 1.
Key Steps for Hamstring Autograft Harvest for Anterior Cruciate Ligament Reconstruction
| Identify anatomic landmarks |
| - Tibial tubercle |
| - Gerdy tubercle |
| - Lateral joint line |
| - Medial joint line |
| - Patellar borders |
| - Fibular head |
| Vertically oriented skin incision: approximately 3 cm |
| Identification of the pes anserine tendons |
| Identify and incise sartorial fascia |
| Reflect sartorial fascia to reveal gracilis and semitendinosus |
| Identify, separate, and dissect gracilis and semitendinosus tendons |
| Whip-stitch first tendon (gracilis) |
| Whip-stitch semitendinosus |
| Assess for soft tissue tethers |
| Perform additional dissection if necessary |
| Reassess for tethers |
| Release first tendon with tendon stripper: pass tendon stripper first and ensure at least 10-12 cm of free tendon |
| Release second tendon |
| Back table: graft preparation |
Technique
Patient Positioning
We perform this surgery under general anesthesia with the patient in the supine position. Prior to final positioning, the injured knee is examined under anesthesia to confirm the diagnosis of an ACL injury. If there is any concern over the diagnosis of an ACL injury, a diagnostic arthroscopy can be performed prior to harvesting the hamstring tendons.
After the examination under anesthesia, a padded nonsterile tourniquet is placed high on the operative thigh, and the patient is positioned such that the operative leg is hanging off of the end of the operating table in a leg holder (Arthrex, Naples, FL), with the contralateral leg in a well-leg holder. The foot of the bed is lowered, allowing the surgeon room to harvest the graft while seated. Alternatively, the leg can be kept on the operating table and placed into a figure-4 position. The operative leg is prepped and draped in standard fashion.
Graft Harvest
Osseous landmarks are drawn out, including the tibial tubercle, to aid in incision placement. The incision is placed along the pes anserinus (palpable) midway between the tibial tubercle and the posteromedial border of the tibia, and is approximately 2 to 3 cm in length (Fig 1). The skin is incised with a no. 10 scalpel. The incision is carried through the subcutaneous tissue to the sartorial fascia with blunt dissection to the level of the sartorial fascia (Fig 2). Care should be taken to avoid injury to the underlying superficial medial collateral ligament as well as to the infrapatellar and sartorial branches of the saphenous nerve. Injury to the medial collateral ligament can be avoided by visualizing this structure, and injury to the nerve branches can be avoided by using a knife for the skin incision only, followed by blunt dissection of the subcutaneous tissue down to the sartorial fascia. At this time, the rolled borders of the gracilis and semitendinosus tendons can usually be palpated with the pad of the surgeon's finger, just under the sartorial fascia. At the level of the pes, the gracilis tendon is located superior relative to the semitendinosus tendon, whereas the semitendinosus tendon has a bigger diameter compared to the gracilis tendon. A no. 15 scalpel is then used to make an “inverted L”-shaped incision in the sartorial fascia in line with the hamstring tendons, with the transverse limb of the L along the superior border of the gracilis and the longitudinal limb of the L along its attachment along the tibial crest. The sartorial fascial incision is extended distally along the tibial crest for approximately 2 cm. Using a tissue forceps and Metzenbaum scissors, the gracilis and semitendinosus tendons are dissected free from the sartorial fascia from the inside of the tissue flap (Fig 3). Once the 2 tendons have been clearly identified, each tendon is individually dissected away from the sartorial fascia and the free ends are whip-stitched with a no. 2 high-strength nonabsorbable suture (Ethicon, Somerville, NJ). It is critical to ensure that at least 10 cm of tendon are free from any extratendinous tethers, particularly adhesions to the medial head of the gastrocnemius. A combination of blunt and cautious sharp dissection (Metzenbaum scissors; Fig 4) is used to ensure that the tendons are free from any adhered soft tissue to avoid prematurely amputating the tendon while using the tendon stripper (Arthrex). Next, a tendon stripper (closed or open-ended; Arthrex) is used to release each tendon from its proximal musculotendinous attachment. Steady traction on the sutures on the free end of the tendon combined with an equally steady push of the tendon stripper toward the hamstring origin at the pelvis should allow for a smooth release of the tendon (Fig 5). Once free, the released tendon is taken to the back table for graft preparation. Typically the gracilis is harvested first, after which these steps are repeated for the semitendinosus (Fig 6).
Fig 1.

Intraoperative photograph (left leg) showing the location of the incision for semitendinosus and gracilis tendon harvest.
Fig 2.

Intraoperative photograph (left leg) showing the location of the sartorial fascia.
Fig 3.

Intraoperative photograph (left leg) showing the location of the semitendinosus and gracilis tendons after dissection free from the sartorial fascia.
Fig 4.

Intraoperative photograph (left leg) showing dissection of the gracilis from the sartorial fascia and from the semitendinosus, prior to harvesting.
Fig 5.

Intraoperative photograph (left leg) showing the use of the tendon stripper to harvest the gracilis tendon after whip-stitching the free end with a high-strength nonabsorbable suture (Ethicon).
Fig 6.
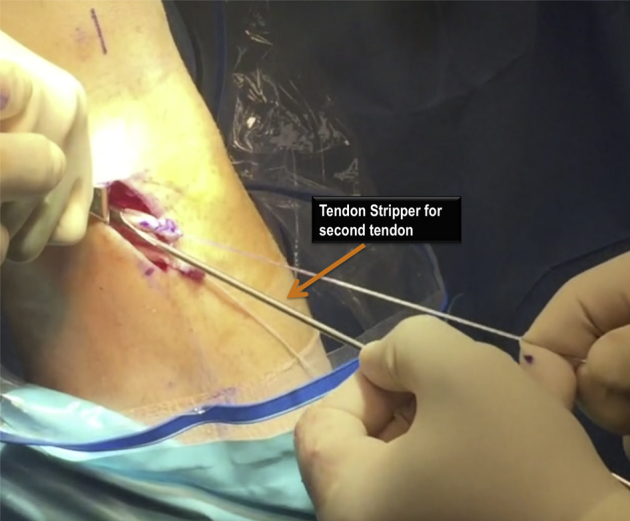
Intraoperative photograph (left leg) showing the use of the tendon stripper to harvest the semitendinosus tendon after whip-stitching the free end with a high-strength nonabsorbable suture (Ethicon); the gracilis tendon has previously been harvested.
At the back table, the muscle tissue is cleared off of each tendon, and the remaining free ends of each tendon are whip stitched. The graft can ultimately be prepared using any one of a number of different techniques based on surgeon preference.
Wound Closure
The wound is then copiously irrigated and closed in layers in standard fashion. Postoperative restrictions are dictated by the surgeon's rehabilitation protocol following ACL reconstruction.
Discussion
In this Technical Note, a reproducible technique for hamstring autograft harvest for ACL reconstruction with a quadruple (4-strand) hamstring autograft using the gracilis and semitendinosus tendons is described. Hamstring tendon grafts allow the surgeon to use an autograft harvested through a relatively small skin incision, resulting in minimal donor site morbidity and reduced extensor mechanism dysfunction when compared to patellar tendon autografts.3 Notably, knowledge of relevant surgical anatomy is of utmost importance to avoid iatrogenic neurologic injury while also ensuring complete harvesting of the hamstring tendons without premature amputation. The semitendinosus and gracilis originate from the ischial tuberosity and ischiopubic ramus, respectively, and converge distally prior to their insertion onto the proximal medial tibia, at a site medial and distal to the tibial tubercle.6 The 2 tendons become distinct structures at a point that is further medial and slightly proximal to their insertion; therefore, harvesting is facilitated by identifying each tendon in a distal to proximal direction. Care must be taken to avoid injury to the superficial medial collateral ligament, which lies deep to the tendons near this area of convergence.
The pes anserine insertion is in close proximity to the infrapatellar branch and sartorial branch of the saphenous nerve, and injury to these nerves have been reported as complications sustained during harvest.7 Iatrogenic damage can manifest clinically as hypoesthesia, dysesthesia, reflex sympathetic dystrophy, and painful neuroma at the site of injury. Additionally, anterior knee pain has been directly associated with damage to the branches of the saphenous nerve.7 In a retrospective case series of 164 patients, Sanders et al.8 reported that concomitant injuries to the sartorial branch and infrapatellar branch occurred in 32% of patients. Isolated paresthesias were reported in the sartorial branch and infrapatellar branch in 23% and 19% of the study population respectively. We suggest blunt dissection until the sartorial fascia is reached to reduce the risk of iatrogenic nerve damage.
Prior to using the tendon stripper to remove the grafts, the surgeon should have performed a thorough dissection of accessory insertions and fascial bands to prevent premature amputation of either tendon. Candal-Couto and Deehan performed an anatomic study on 10 cadaveric specimens to characterize the fascial attachments of the gracilis and semitendinosus. The authors reported high variability in accessory bands and identified bands between tendons, connections to the popliteal fascia, sartorius, gastrocnemius, pretibial fascia, and superficial fascia. Importantly, accessory bands also originated more than 10 cm proximally from the semitendinosus and gracilis.9 Tuncay et al.10 suggested that a primary reason for the premature division of the hamstring tendons is the fascial band between the semitendinosus to gracilis given its variable size and placement. We find that if each tendon has 10 to 12 cm of excursion, then premature amputation is unlikely. If excessive resistance is felt when advancing the tendon stripper, one should stop, reassess for additional bands, and then return to using the tendon stripping. A summary of pearls and pitfalls associated with quadruple (4-strand) hamstring autograft harvest for ACL reconstruction is provided in Table 2.
Table 2.
Pearls and Pitfalls Associated With Quadruple (4-Strand) Hamstring Autograft Harvest for Anterior Cruciate Ligament Reconstruction
| Pearls | • Four-stranded (quadruple) hamstring grafts are among the strongest grafts biomechanically (at time equals zero). |
| • Perform an examination under anesthesia and confirm the diagnosis of ACL injury prior to harvesting hamstring tendons | |
| • Understand the anatomy: the semitendinosus and gracilis originate from the ischial tuberosity and ischiopubic ramus, respectively | |
| • Release first tendon with tendon stripper: pass tendon stripper first and ensure at least 10-12 cm of free tendon | |
| ○ Steady traction on the sutures on the free end of the tendon combined with an equally steady push of the tendon stripper toward the hamstring origin at the pelvis should allow for a smooth release of the tendon | |
| Pitfalls | • Take care to avoid injury to the superficial medial collateral ligament, which lies deep to the tendons near this area of convergence; injury to the medial collateral ligament can be avoided by visualizing this structure |
| • The pes anserine insertion is in close proximity to the infrapatellar branch and sartorial branch of the saphenous nerve, and injury to these nerves are common complications during harvest; injury to the nerve branches can be avoided by using a knife for the skin incision only, followed by blunt dissection of the subcutaneous tissue down to the sartorial fascia | |
| • Prior to using the tendon stripper to remove the grafts, the surgeon should be confident in his or her dissection of accessory insertions and fascial bands to prevent premature amputation of the graft |
ACL, anterior cruciate ligament.
Overall, the use of semitendinosus and gracilis hamstring tendons for ACL reconstruction requires an in-depth knowledge of surgical anatomy for proper harvesting and preparation of the graft. This technique offers a viable alternative to the bone–patellar tendon–bone autograft.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: B.R.B. reports other from American Orthopaedic Society for Sports Medicine, nonfinancial support from Arthrex, CONMED Linvatec, DJ Orthopaedics, and Ossur; personal fees and nonfinancial support from SLACK; and nonfinancial support from Smith & Nephew and Tornier, outside the submitted work. N.N.V. reports other from American Orthopaedic Society for Sports Medicine; other from American Shoulder and Elbow Surgeons; nonfinancial support and other from Arthrex; personal fees, nonfinancial support, and other from Arthroscopy; other from Arthroscopy Association Learning Center Committee; nonfinancial support and other from Arthrosurface; personal fees and other from Cymedica; nonfinancial support and other from DJ Orthopaedics; personal fees from Minivasive; other from Journal of Knee Surgery; personal fees from Omeros; personal fees and nonfinancial support from Orthospace; nonfinancial support from Ossur; other from SLACK; personal fees, nonfinancial support, and other from Smith & Nephew; nonfinancial support from ConMed Linvatec; nonfinancial support from Miomed; nonfinancial support from Mitek; and personal fees and nonfinancial support from Vindico Medical-Orthopedics Hyperguide, outside the submitted work. C.B.J. reports other from American Journal of Sports Medicine, other from American Orthopaedic Society for Sports Medicine, personal fees from Cresco Lab, other from The Foundry, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical technique for left knee ACL reconstruction with hamstring autograft harvest, including graft preparation to create a quadruple-stranded hamstring autograft composed of the semitendinosus and gracilis tendons.
References
- 1.Davarinos N., O'Neill B.J., Curtin W. A brief history of anterior cruciate ligament reconstruction. Adv Orthop Surg. 2014;2014:6. [Google Scholar]
- 2.Mall N.A., Chalmers P.N., Moric M. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42:2363–2370. doi: 10.1177/0363546514542796. [DOI] [PubMed] [Google Scholar]
- 3.Goldblatt J.P., Fitzsimmons S.E., Balk E., Richmond J.C. Reconstruction of the anterior cruciate ligament: Meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy. 2005;21:791–803. doi: 10.1016/j.arthro.2005.04.107. [DOI] [PubMed] [Google Scholar]
- 4.Maeda A., Shino K., Horibe S., Nakata K., Buccafusca G. Anterior cruciate ligament reconstruction with multistranded autogenous semitendinosus tendon. Am J Sports Med. 1996;24:504–509. doi: 10.1177/036354659602400416. [DOI] [PubMed] [Google Scholar]
- 5.Ma C.B., Keifa E., Dunn W., Fu F.H., Harner C.D. Can pre-operative measures predict quadruple hamstring graft diameter? Knee. 2010;17:81–83. doi: 10.1016/j.knee.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Pagnani M.J., Warner J.J., O'Brien S.J., Warren R.F. Anatomic considerations in harvesting the semitendinosus and gracilis tendons and a technique of harvest. Am J Sports Med. 1993;21:565–571. doi: 10.1177/036354659302100414. [DOI] [PubMed] [Google Scholar]
- 7.Ruffilli A, De Fine M, Traina F, Pilla F, Fenga D, Faldini C. Saphenous nerve injury during hamstring tendons harvest: Does the incision matter? A systematic review. Knee Surg Sports Traumatol Arthrosc. June 23, 2016. [Epub ahead of print.] [DOI] [PubMed]
- 8.Sanders B., Rolf R., McClelland W., Xerogeanes J. Prevalence of saphenous nerve injury after autogenous hamstring harvest: An anatomic and clinical study of sartorial branch injury. Arthroscopy. 2007;23:956–963. doi: 10.1016/j.arthro.2007.03.099. [DOI] [PubMed] [Google Scholar]
- 9.Candal-Couto J.J., Deehan D.J. The accessory bands of Gracilis and Semitendinosus: an anatomical study. Knee. 2003;10:325–328. doi: 10.1016/s0968-0160(02)00154-0. [DOI] [PubMed] [Google Scholar]
- 10.Tuncay I., Kucuker H., Uzun I., Karalezli N. The fascial band from semitendinosus to gastrocnemius: The critical point of hamstring harvesting: An anatomical study of 23 cadavers. Acta Orthop. 2007;78:361–363. doi: 10.1080/17453670710013933. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for left knee ACL reconstruction with hamstring autograft harvest, including graft preparation to create a quadruple-stranded hamstring autograft composed of the semitendinosus and gracilis tendons.


