Abstract
Background
In Uganda, malaria vector control interventions and case management with Artemisinin Combination Therapies (ACTs) have been scaled up over the last few years as a result of increased funding. Data on parasitaemia prevalence among children less than 5 years old and coverage of interventions was collected during the first two Malaria Indicator Surveys (MIS) conducted in 2009 and 2014, respectively. In this study, we quantify the effects of control interventions on parasitaemia risk changes between the two MIS in a spatio-temporal analysis.
Methods
Bayesian geostatistical and temporal models were fitted on the MIS data of 2009 and 2014. The models took into account geographical misalignment in the locations of the two surveys and adjusted for climatic changes and socio-economic differentials. Parasitaemia risk was predicted over a 2 × 2 km2 grid and the number of infected children less than 5 years old was estimated. Geostatistical variable selection was applied to identify the most important ITN coverage indicators. A spatially varying coefficient model was used to estimate intervention effects at sub-national level.
Results
The coverage of Insecticide Treated Nets (ITNs) and ACTs more than doubled at country and sub-national levels during the period 2009–2014. The coverage of Indoor Residual Spraying (IRS) remained static at all levels. ITNs, IRS, and ACTs were associated with a reduction in parasitaemia odds of 19% (95% BCI: 18–29%), 78% (95% BCI: 67–84%), and 34% (95% BCI: 28–66%), respectively. Intervention effects varied with region. Higher socio-economic status and living in urban areas were associated with parasitaemia odds reduction of 46% (95% BCI: 0.51–0.57) and 57% (95% BCI: 0.40–0.53), respectively. The probability of parasitaemia risk decline in the country was 85% and varied from 70% in the North-East region to 100% in Kampala region. The estimated number of children infected with malaria declined from 2,480,373 in 2009 to 825,636 in 2014.
Conclusions
Interventions have had a strong effect on the decline of parasitaemia risk in Uganda during 2009–2014, albeit with varying magnitude in the regions. This success should be sustained by optimizing ITN coverage to achieve universal coverage.
Electronic supplementary material
The online version of this article (doi: 10.1186/s13071-017-2393-0) contains supplementary material, which is available to authorized users.
Keywords: Malaria, Malaria indicator survey, Spatio-temporal, Parasitaemia, ITNs, IRS, ACTs, Spatially varying, Bayesian kriging, Malaria interventions
Background
Although malaria is still a leading global health problem, its burden has been on a decline in recent years [1]. This decline which started in the early 1990s prior to the global campaign of scaling up of control interventions in mid-2000s continued through the post-scale-up period [2]. The downward trend of malaria burden in the pre-intervention period notwithstanding, sufficient evidence from randomized trials and field settings indicate that malaria decline during the post-scale-up period has been unprecedented [2–5]. For instance in sub-Saharan Africa (SSA) parasitaemia prevalence declined from 17% in 2010 to 13% in 2015 [1]. Also, during the period 2000–2015, declines in global malaria incidence and deaths of up to 37 and 60%, respectively were reported [3, 6]. These declines were mainly attributed to the impact of Insecticide Treated Nets (ITNs) and malaria case management with Artemisinin Combination Therapies (ACTs).
In spite of these higher declines in malaria at global level, slower declines were reported in the 15 most high burden countries, the majority of which are situated in SSA [1]. This region bears the heaviest burden and accounts for an estimated 90% of all malaria deaths mainly among children less than 5 years old. Uganda is ranked fourth among these high malaria burden countries and has some of the highest malaria transmission rates in the world [7]. Since 2006, Roll Back Malaria (RBM) has funded malaria control and prevention activities in the country and periodically supports the conducting of Malaria Indicator Surveys (MIS) [8]. The MIS are standardized nationally representative surveys that collect high quality data for estimating the prevalence of parasitaemia risk in children less than 5 years old and track the progress of interventions coverage. To date, two MIS have been conducted in Uganda; MIS 2009 and MIS 2014–15 [9, 10]. Findings from the first MIS revealed a high parasitaemia risk in most regions. Malaria was hyperendemic (prevalence 50–75%) in three regions, mesoendemic (prevalence 10–50%) in six, and only hypoendemic (prevalence < 10%) in one region [10]. Results of the second MIS showed tremendous improvement in the coverage of ITNs and ACTs intervention at all levels and a reduction of parasitaemia risk of 50%. Additionally, parasitaemia risk in the majority of regions had declined to mesoendemic and hypoendemic proportions [9]. The true effect of each intervention on parasitaemia reduction is not known at national and sub-national level, and yet a new framework has been adopted by the Ministry of Health (MoH) to speed up malaria control efforts. In this framework known as Uganda Malaria Reduction Strategic Plan (UMRSP) 2014–2020, ambitious targets have been set to reduce malaria mortality to near zero, morbidity to 30 cases per 1000 population, and parasite prevalence to less than 7% [8]. To achieve these targets and ensure efficient use of scarce resources and effective programming and implementation, it is vital to understand the effect that each intervention has had on parasitaemia risk decline.
Declines in malaria parasitaemia risk, morbidity and mortality have been achieved in other malaria endemic countries following scaling up of control interventions. Bhatt et al. [3] reported a reduction of 50% in Plasmodium falciparum prevalence and 40% in incidence of clinical disease in endemic African countries between 2000 and 2015. Similarly, the number of malaria cases and deaths decreased by more than 50% in southern African countries after introducing interventions during 2000–2008 [11]. In the Kilifi district of Kenya, parasitaemia prevalence declined from 35 to 1% after a mass distribution of ITNs and ACTs [11]. Also, Giardina et al. [12] demonstrated that ITNs and IRS were significantly associated with parasitaemia risk reduction in Rwanda, Tanzania, Senegal, Angola, Liberia and Mozambique.
Our study aims to estimate spatio-temporal trends of parasitaemia risk changes among children less than 5 years old in Uganda during 2009–2014, and to determine the effect of interventions on parasitaemia risk decline at national and subnational levels. We analyzed MIS data using Bayesian spatio-temporal geostatistical models. The results from this study provide insight on the effectiveness of interventions and can be used by MoH and Malaria Control Program (MCP) to evaluate interventions and optimize resources for achievement of objectives of UMRSP 2014–2020.
Methods
Country profile
Uganda is located in the great lakes region in East Africa neighboring Kenya, Tanzania, Rwanda, Democratic Republic of Congo, and South Sudan. It has a population of 37.1 million, all of which are at risk of malaria. Malaria is the leading cause of morbidity and mortality in the country, accounting for 3,631,939 (4,400,000–12,000,000) cases and 5921 (5300–17,000) deaths in 2015 [13]. The most dominant malaria parasite is Plasmodium falciparum, and the major transmission vectors are Anopheles gambiae and Anopheles funestus. In recent times, vector resistance to both pyrethroid and carbamates has been reported.
Data sources
Parasitological and interventions data were obtained from the MIS data of 2009 and 2014–2015. The two surveys were conducted at the peak of a high malaria transmission season towards the end of the long rainy season (December 2009 and December 2014–January 2015, respectively). The MIS are nationally representative surveys which employ a two-stage stratified cluster design. The clusters also known as census enumeration areas are selected at first stage with probability proportional-to-size sampling, and households are selected at second stage using systematic sampling. The surveys are designed to provide information on key malaria control indicators, such as the proportion of households having at least one ITN, the proportion of children under 5 years of age who slept under an ITN the previous night. Also, the survey is designed to produce key indicator estimates for urban and rural strata separately, as well as for the 10 regions/domains that constitute the country. The regions are: Kampala, Central 1, Central 2, East-Central, Mid-North, Mid-Western, North-East, South-Western and West Nile. At the first stage of sampling, 170 and 210 clusters were selected in 2009 and 2014, respectively. At the second stage, 28 households were selected from each cluster in both surveys resulting in a total of 4000 and 5880 households selected in the first and second survey, respectively [9, 10].
Coverage of ITNs was defined in terms of ownership and use indicators that were generated from data captured on the survey tools using standard definitions [14]. The following ITN ownership indicators were defined; proportion of households with at least one ITN, proportion of households with one ITN for every two people, and proportion of population with access to an ITN within their household. The ITN use indicators were: proportion of children less than 5 years of age who slept under an ITN, proportion of population that slept under an ITN, and proportion of ITNs used the night preceding the survey. IRS coverage was defined as the proportion of households that were sprayed during the last 12 and 6 months in the MIS 2009 and MIS 2014–2015, respectively. The wealth index derived from household possessions was used as a socioeconomic proxy. A case management indicator was defined as the proportion of fever episodes in children of less than 5 years old during the last 2 weeks preceding the survey which were treated with any Artemisinin Combination Therapies (ACTs). In addition, information on the location of the cluster (i.e. rural/urban) was obtained from survey data and from the Global Rural-Urban Mapping Project (GRUMP) database [15]. The GRUMP database provides gridded data at 1 km2 spatial resolution.
Malaria transmission depends on the environment which affects the disease distribution, seasonality, and transmission intensity. Environmental/climatic factors were extracted from Remote Sensing (RS) sources. Weekly day and night Land Surface Temperature (LST), bi-weekly Normalized Difference Vegetation index (NDVI) and land cover data were obtained from Moderate Resolution Imaging Spectroradiometer (MODIS) at 1 km2 spatial resolution. Dekadal rainfall data at 8 × 8 km2 resolution were extracted from the US Early Warning and Environmental Monitoring System (EWES). Altitude was obtained from the shuttle radar topographic mission using the digital elevation model. Also, distances from cluster centroids to major water bodies were estimated using ESRI’s ArcGIS 10.2.1 for Desktop. The high spatial resolution population data was downloaded from WorldPop [16]. Data from remote sensing sources was acquired for the 12 month period preceding the survey and the average (cumulative value for rainfall) was calculated and extracted for each cluster. The one-year period was considered long enough to capture the actual climatic conditions that affected malaria transmission throughout the year of the survey.
Statistical analysis
Bayesian geostatistical models were developed to predict parasitaemia risk at the two survey time points using environmental/climatic factors as predictors. Bayesian kriging was applied to obtain parasitaemia risk estimates over a 2 × 2 km2 resolution grid. Predictions were used to determine the probability of parasitaemia risk reduction between the two surveys.
The number of children infected with malaria in the two surveys was estimated by combining high spatial resolution population data obtained from WorldPop (www.worldpop.org) with the predicted pixel-level malaria prevalence estimates. The number of children less than 5 years old was estimated by multiplying population counts by a factor of 17.7%, the proportion of population under 5 years of age [17]. Regional estimates of the number of infected children were computed by aggregating pixel-level estimates at regional level. The number of infected children per pixel was obtained by multiplying pixel-wise spatially explicit prevalence estimates with high spatial resolution population estimates of number of children less than 5 years old. In both surveys, the population-adjusted prevalence was estimated by summing up estimates of the number of infected children per pixel divided by the total estimated number of children less than 5 years old.
The effects of interventions were estimated by modeling the change of parasitaemia risk between the two surveys on the logit scale as a function of the effect of intervention coverage at the second survey adjusted for socioeconomic status, cluster location, and the difference in environmental/climatic factors. Geographical misalignment of the locations between the two surveys was carried out by predicting parasitaemia risk of the first survey at the second survey locations. The prediction uncertainty was incorporated by fitting an error term in the model. A spatially varying coefficients model was used to estimate intervention effects at regional level and to account for potential interactions of interventions with endemicity level.
A spike and slab geostatistical Bayesian variable selection procedure was applied to select the most important ITN and environmental predictors that explain maximum variation in the change in parasitaemia risk between 2009 and 2014 [18]. Variables with the highest inclusion probability in the model were selected.
Descriptive analyses were carried out in STATA (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP). Geostatistical modeling was implemented in OpenBUGS version 3.2.3 (Imperial College and Medical Research Council, London, UK). Since implementing Bayesian kriging in OpenBUGS is very slow especially for large grids, we implemented it in R statistical software using posterior estimates of the model parameters obtained from OpenBUGS. Maps were produced in ESRI’s ArcGIS 10.2.1 (http://www.esri.com/en-us/home).
Parameter estimates were summarized by their posterior medians and their corresponding 95% Bayesian Credible Intervals (BCI). The effect of a predictor was considered to be statistically important if its 95% BCI did not include zero.
Detailed explanations of the fitted statistical models are presented in Additional files 1 and 2.
Results
A summary of the survey data is given in Tables 1 and 2, and maps of survey locations are presented in Fig. 1. A higher number of clusters, households, and children were tested in the second survey (Table 1).
Table 1.
Survey information and malaria intervention coverage indicators in 2009 and 2014
| Indicator | MIS 2009 | MIS 2014–2015 |
|---|---|---|
| Number of clusters | 170 | 210 |
| Number of households | 4421 | 5345 |
| Number of children tested | 3972 | 4939 |
| Interventions | % (95%CI) | % (95% CI) |
| Parasitaemia prevalence | 42.4 (37.7–47.0) | 19.0 (16.3–21.8) |
| Proportion of households with at least one ITN | 46.7 (42.7–50.6) | 90.2 (88.7–91.7) |
| Proportion of households with at least one ITN for every two people | 16.4 (14.2–18.5) | 62.3 (60.1–64.5) |
| Proportion of population with access to an ITN in their household | 32.2 (29.3–35.1) | 80.6 (78.9–82.4) |
| Proportion of the population that slept under an ITN the previous night | 26.3 (23.5–29.2) | 70.8 (68.9–72.8) |
| Proportion of children less than 5 years old who slept under an ITN the previous night | 32.9 (29.0–36.9) | 74.5 (72.2–76.9) |
| Proportion of existing ITNs used the previous night | 26.1 (23.3–28.9) | 70.4 (68.5–72.4) |
| Proportion of households sprayed in the last 6 months | 5.5 (3.0–7.9) | 5.2 (3.4–6.9) |
| Proportion of households with at least one ITN and/or sprayed by IRS in the last 12 months | 49.2 (45.3–53.1) | 90.5 (89.0–92.0) |
| Proportion of fever episodes treated with ACT | 23.3 (19.9–26.7) | 66.8 (63.2–70.5) |
Abbreviations: MIS Malaria Indicator Survey, TNs Insecticide Treated Nets, ACTs Artemisinin Combination Therapies, IRS Indoor Residual Spraying
Table 2.
Coverage of malaria intervention coverage indicators by region in 2009 and 2014
| Indicator | Central 1 | Central 2 | Kampala | East-Central | Mid-Eastern | North-East | Mid-North | West Nile | Mid-Western | South-Western | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2009 | 2014 | 2009 | 2014 | 2009 | 2014 | 2009 | 2014 | 2009 | 2014 | 2009 | 2014 | 2009 | 2014 | 2009 | 2014 | 2009 | 2014 | 2009 | 2014 | |
| Parasitaemia prevalence | 39.0 | 10.4 | 51.0 | 23.6 | 4.9 | 0.4 | 56.2 | 36.4 | 37.4 | 13.5 | 39.7 | 27.2 | 62.1 | 19.5 | 45.6 | 27.5 | 42.7 | 17.5 | 11.8 | 4.1 |
| Proportion of households with at least one ITN | 35.3 | 80.8 | 23.5 | 81.6 | 49.1 | 86.3 | 33.5 | 82.1 | 59.5 | 94.6 | 76.6 | 97.0 | 63.7 | 94.3 | 52.4 | 96.3 | 33.9 | 93.6 | 33.7 | 96.9 |
| Proportion of households with at least one ITN for every two people | 14.6 | 56.7 | 9.3 | 53.4 | 32.4 | 66.5 | 7.8 | 46.7 | 17.0 | 61.7 | 33.1 | 60.6 | 20.1 | 66.7 | 12.8 | 72.1 | 12.1 | 64.0 | 14.7 | 76.6 |
| Proportion of population with access to an ITN | 25.4 | 71.8 | 16.4 | 70.8 | 42.4 | 79.2 | 21.6 | 68.7 | 37.1 | 83.7 | 57.0 | 84.2 | 43.7 | 85.8 | 33.0 | 88.8 | 23.0 | 83.7 | 30.0 | 91.1 |
| Proportion of the population that slept under an ITN | 19.1 | 60.1 | 10.3 | 58.6 | 36.9 | 73.0 | 18.7 | 62.8 | 31.4 | 76.3 | 54.3 | 85.5 | 32.1 | 77.6 | 33.1 | 77.7 | 17.0 | 78.6 | 22.6 | 67.0 |
| Proportion of children less than 5 years old who slept under an ITN | 21.5 | 67.6 | 11.3 | 65.3 | 42.5 | 73.9 | 19.3 | 69.7 | 41.4 | 78.8 | 65.1 | 87.0 | 41.7 | 79.0 | 37.2 | 76.8 | 20.4 | 82.3 | 33.1 | 64.4 |
| Proportion of existing ITNs used the previous night | 19.1 | 59.6 | 10.3 | 58.5 | 36.7 | 72.7 | 18.7 | 62.6 | 31.1 | 75.9 | 52.5 | 84.3 | 32.0 | 77.1 | 32.9 | 77.0 | 16.8 | 78.5 | 22.6 | 66.6 |
| Proportion of households sprayed | 0.2 | 1.0 | 4.6 | 0.4 | 5.5 | 1.3 | 0.4 | 0.0 | 0.6 | 0.4 | 4.2 | 0.1 | 31.6 | 44.6 | 0.0 | 1.2 | 0.2 | 0.3 | 1.8 | 0.0 |
| Proportion of households with at least one ITN and/or sprayed by IRS in the last 12 months | 35.3 | 80.8 | 26.3 | 81.9 | 52.3 | 86.3 | 33.8 | 82.1 | 59.6 | 94.6 | 77.1 | 97.0 | 77.8 | 97.2 | 52.4 | 96.3 | 34.1 | 93.6 | 44.7 | 96.9 |
| Proportion of fever episodes treated with any artemisin combination therapy | 17.4 | 55.2 | 18.0 | 71.7 | 22.5 | 51.5 | 13.4 | 71.1 | 16.6 | 68.0 | 25.1 | 73.3 | 40.8 | 69.2 | 27.7 | 67.0 | 19.4 | 61.1 | 10.0 | 53.3 |
Abbreviations: ITNs Insecticide Treated Nets, ACTs Artemisinin Combination Therapies, IRS Indoor Residual Spraying
Fig. 1.
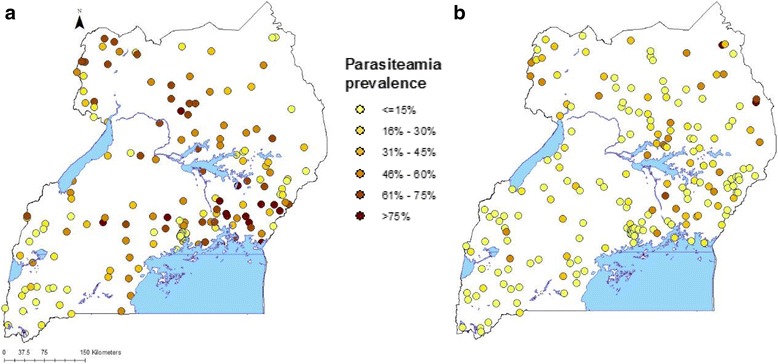
Observed malaria prevalence and survey locations of MIS 2009 (a) and MIS 2014–2015 (b)
Results show that at country level parasitaemia prevalence declined from 42.4% in 2009 to 19.0% in 2014, a decline of 50%. At regional level, the highest malaria reduction was observed in the regions of Kampala (91.8%), Central 1 (74.0%) and Mid-North (68.6%), and the lowest in the North-East region (30.2%) and East-Central region (35.2%).
Generally interventions coverage increased at country and regional levels (Additional file 3). At country level, ITN ownership (the proportion of households with at least one ITN and the proportion of households with at least one ITN for every two people) increased by four-fold. Among regions, the biggest increase in ITN ownership was reported in East-Central (six-fold), while the smallest was observed in Mid-North (two-fold). More so, the proportion of children less than 5 years old that slept under an ITN increased by more than two times at country level. The improvement in this indicator coverage was highest in Central 2 region (5.8 times) and lowest in North-East region (1.3 times).
Overall, the proportion of fever episodes treated with ACTs increased by three times. The highest increase was achieved in South-Western, East-Central and West Nile regions where coverage increased by more than five times. The least gain in ACTs coverage was observed in Mid-North region where it increased by almost two times. The national IRS coverage remained static at 5% except in the Mid-North region where an increase of 41% was achieved.
Spatio-temporal trends of parasitaemia risk during 2009–2014
The effects of the most important environmental factors identified through geostatistical variable selection are shown in Table 3. Results indicate that more environmental factors were related to parasitaemia risk in 2009 compared to 2014. Also, spatial correlation was stronger in 2009.
Table 3.
Posterior estimates of the effect of environmental factors on parasitaemia risk in 2009 and 2014
| Predictor | MIS 2009 | MIS 2014–2015 |
|---|---|---|
| OR (95% BCI) | OR (95% BCI) | |
| Day LSTb | ||
| < 27.84 / < 31.4 | 1 | 1 |
| 27.84–30.18 / 31.4–33.8 | 1.68 (1.44–2.14)a | 2.75 (2.03–3.64)a |
| > = 30.19 / > = 33.8 | 1.41 (1.28–1.76)a | 2.19 (1.79–3.39)a |
| Night LST | 1.55 (1.39–1.67)a | 1.44 (1.19–1.60)a |
| Area type | ||
| Rural vs urban | 7.80 (4.88–11.09)a | 3.70 (2.56–4.88)a |
| NDVI | 1.25 (1.10–1.51)a | |
| Rainfallb | ||
| < 17.11 / < 17.14 | 1 | |
| 17.11–18.49 / 17.14–18.79 | 1.13 (0.93–1.23) | |
| > = 18.50 / > = 18.79 | 1.39 (1.12–1.49)a | |
| Altitudeb | ||
| < 1098 | 1 | |
| 1098–1201 | 0.89 (0.81–0.95)a | |
| > = 1202 | 0.43 (0.38–0.47)a | |
| Land cover | ||
| Others | 1 | |
| Crops | 1.19 (1.13–1.43)a | |
| Spatial parameters | ||
| Spatial variance | 1.12 (0.99–1.20) | 0.54 (0.49–0.59) |
| Range (km) | 43.3 (12.2–57.8) | 43.8 (36.3–48.2) |
Abbreviations: MIS Malaria Indicator Survey, LST Land Surface Temperature, NDVI Normalized Difference Vegetation Index
aStatistically important effect
bCut-offs before and after the slash (/) are for 2009 and 2014 respectively
Figure 2 depicts the predicted parasitaemia risk in 2009 and 2014 over a 2 × 2 km2 resolution grid based on the 2.5th, median, and the 97.5th percentile posterior predictive distributions. Estimates suggest a high parasitaemia risk in 2009 where in some areas the predicted prevalence was over 80%. In 2014, parasitaemia risk was much lower in most parts of the country except in some areas of the East-Central, North-East and West Nile regions where the burden still remained high. The probability of parasitaemia decline in the country was 85%. The highest decline in malaria occurred in the regions of Central 2 and Kampala while the least was estimated in the North-East region (Fig. 3).
Fig. 2.
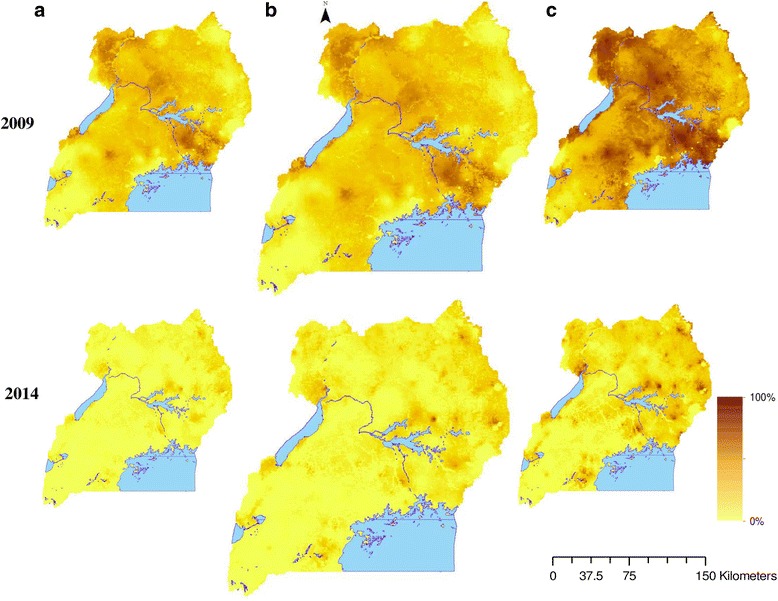
Predicted parasitaemia risk in 2009 and 2014. 2.5th percentile posterior predictive distribution (a), median posterior predictive distribution (b), 97.5th percentile posterior predictive distribution (c)
Fig. 3.
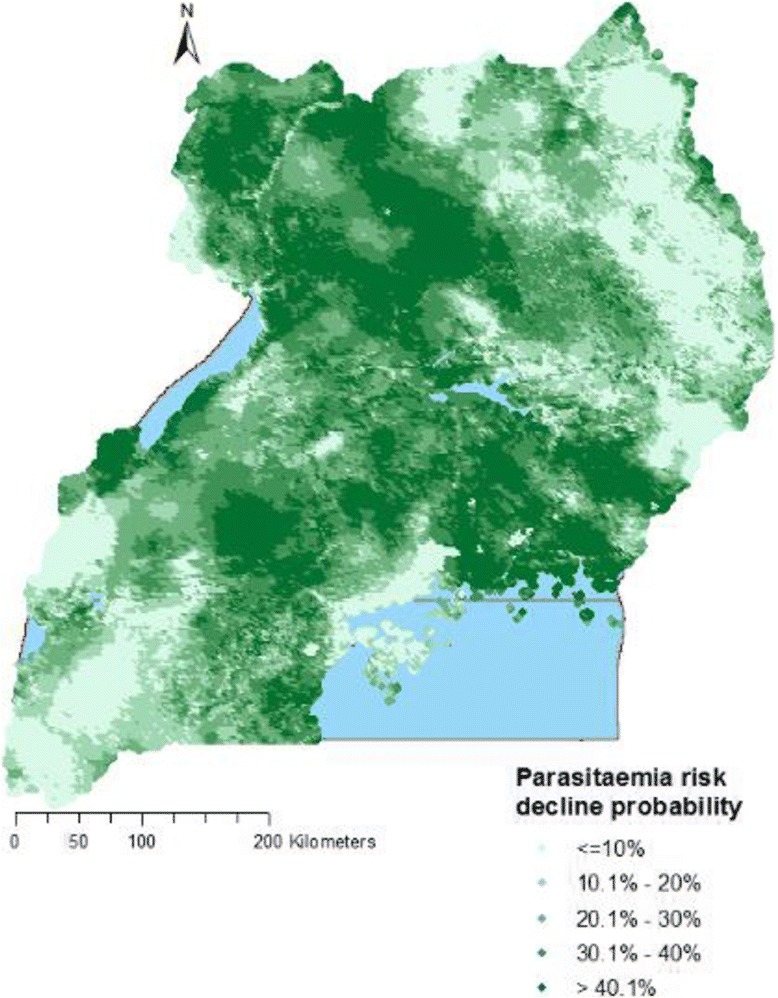
Probability of parasitaemia risk decline from 2009 to 2014
Overall, the number of infected children reduced from over 2,480,000 to less than 830,000 between 2009 and 2014 (Table 4). This translates into a reduction of over 66%. Reduction in the estimated number of infected children was achieved in all regions. The biggest reduction occurred in Kampala (86%), Central 1 (75%), Central 2 (74%), Mid-Eastern (71%) and Mid-North region (70%), whereas the least happened in North-East (44%). In both surveys, the highest and lowest numbers of infected children were estimated in the East-Central and Kampala regions, respectively. Overall, a reduction in population adjusted prevalence of over 26% was achieved. The highest reduction (39.4%) was observed in the East-Central region while the least one (5.0%) was registered in Kampala.
Table 4.
Estimated number of infected children and population adjusted prevalence in 2009 and 2014
| Region | No. of infected children in 2009 | No. of infected children in 2014 | Percentage reduction in no. of infected children | Population adjusted prevalence in 2009 | Population adjusted prevalence in 2014 | Population adjusted prevalence difference |
|---|---|---|---|---|---|---|
| (%) | % (95% BCI) | % (95% BCI) | (%) | |||
| North-East | 212,159 | 119,871 | 43.5 | 37.6 (37.4–37.8) | 23.3 (23.1–23.4) | 14.3 |
| West Nile | 276,237 | 106,377 | 61.5 | 56.8 (56.4–57.2) | 25.8 (25.5–26.0) | 31.0 |
| Mid-North | 332,162 | 98,846 | 70.2 | 52.4 (52.2–52.5) | 20.0 (19.8–20.2) | 32.4 |
| Mid-Western | 269,487 | 77,027 | 71.4 | 39.6 (39.3–39.9) | 12.9 (12.7–13.1) | 26.7 |
| Mid-Eastern | 274,376 | 79,734 | 70.9 | 46.3 (45.6–47.1) | 16.8 (16.4–17.2) | 29.5 |
| East-Central | 375,575 | 138,191 | 63.2 | 64.7 (64.3–65.1) | 25.3 (24.8–25.8) | 39.4 |
| Central 2 | 338,097 | 87,562 | 74.1 | 50.1 (49.8–50.3) | 14.4 (14.2–14.6) | 35.7 |
| Central 1 | 232,426 | 58,314 | 74.9 | 38.2 (37.8–38.6) | 10.6 (10.4–10.8) | 27.6 |
| South-Western | 148,799 | 56,819 | 61.7 | 22.2 (22.0–22.5) | 8.8 (8.6–9.1) | 13.4 |
| Kampala | 21,060 | 2895 | 86.3 | 5.9 (5.2–6.5) | 0.9 (0.8–1.1) | 5.0 |
| Overall | 2,480,373 | 825,636 | 66.7 | 44.0 (43.9–44.2) | 17.7 (17.6–17.7) | 26.3 |
Figure 4 further shows that the number of infected children in 2014 shrank considerably compared to 2009 in all regions except in the East-Central region. The map also depicts a strong statistically important reduction in concentration of infected children in Mid North region in 2014.
Fig. 4.
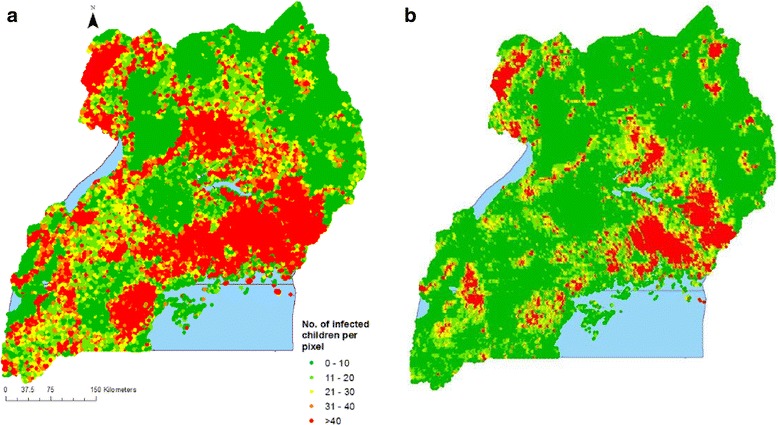
Distribution of estimated number of infected children per pixel in 2009 (a) and 2014 (b)
Results from geostatistical variable selection (Table 5) indicate that the proportion of population with access to an ITN in their household was the only indicator able to capture the effect of ITN interventions as it has the highest inclusion probability. This indicator was used to quantify the effect of ITNs on the parasitaemia odds change.
Table 5.
Posterior inclusion probability for ITN coverage indicator for MIS 2014
| Indicator | Probability of inclusion (%) |
|---|---|
| Proportion of households with at least one ITN | 5.8 |
| Proportion of households with at least one ITN for every two people | 6.1 |
| Proportion of population with access to an ITN in their household | 42.7 |
| Proportion of the population that slept under an ITN the previous night | 4.7 |
| Proportion of children under 5 years old who slept under an ITN the previous night | 12.3 |
| Proportion of existing ITNs used the previous night | 0.2 |
Abbreviations: MIS Malaria Indicator Survey, ITN Insecticide Treated Net
Effects of interventions on parasitaemia odds decline
The effects of interventions on the change of parasitaemia odds adjusted for socioeconomic status and changes in environmental conditions between the two surveys are showed in Table 6. Results demonstrate an important protective effect of interventions on the decrease of parasitaemia odds from 2009 to 2014. ITNs, IRS and ACTs were associated with a parasitaemia odds reduction of 19% (95% BCI: 18–29%), 78% (95% BCI: 67–84%), and 34% (95% BCI: 28–66%), respectively. Similarly, higher socio-economic status had a strong effect on parasitaemia odds reduction. More so, living in urban areas was associated with a decrease in malaria odds of 57% (95% BCI: 47–60%) compared to living in rural areas. On average, rainfall, day and night LST increased from 2009 to 2014, and these increases were significantly associated with increased parasitaemia odds. However, changes in the NDVI had no effect on changes in parasitaemia odds.
Table 6.
Posterior estimates for the effect of interventions adjusted for socio-economic status and changes in climatic/environmental conditions
| Covariate | OR (95% BCI) |
|---|---|
| Difference in LST (day) | 1.10 (1.02–1.13)a |
| Difference in LST (night) | 1.09 (1.03–1.18)a |
| Difference in NDVI | 1.00 (0.94–1.08) |
| Difference in rainfall | 1.14 (1.08–1.23)a |
| Area type (urban vs rural) | 0.43 (0.40–0.53)a |
| Wealth index | 0.54 (0.51–0.57)a |
| ITN | 0.81 (0.71–0.82)a |
| IRS | 0.22 (0.16–0.33)a |
| ACTs | 0.66 (0.34–0.72)a |
| Spatial variance | 0.63 (0.56–0.76) |
| Range (km) | 35.4 (24.3–37.0) |
Abbreviations: ITNs Insecticide Treated Nets, ACTs Artemisinin Combination Therapies, IRS Indoor Residual Spraying, LST Land Surface Temperature, NDVI Normalized Difference Vegetation Index
aStatistically important effect
Intervention effects on parasitaemia odds decline varied by region (Fig. 5). The effect of ITNs at regional level was significantly higher than the national effect in Mid-North and West Nile. ITNs’ effects were significantly lower in East-Central, Mid-Eastern, Mid-Western, and South-Western regions. Likewise, the effect of ACTs was significantly higher than the national average in most regions except in Central 1, Mid-North, Mid-Western, and West Nile regions.
Fig. 5.
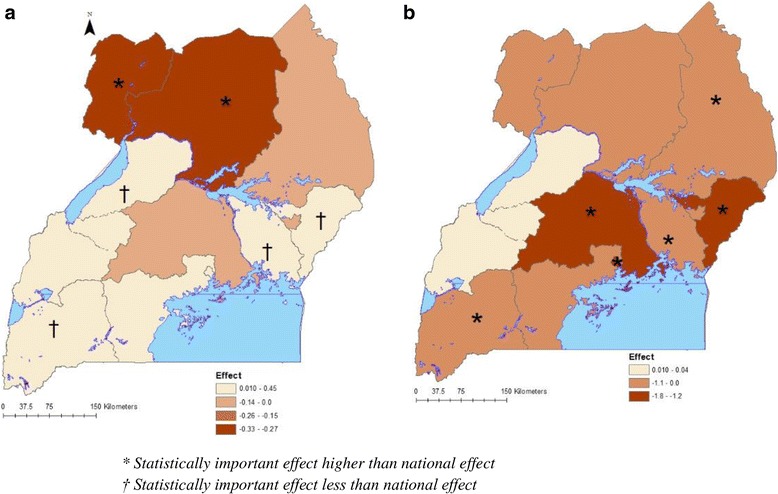
Spatially varying effects of interventions for ITNs (a) and ACTs (b)
Discussion
In this study we have determined the spatio-temporal trends of parasitaemia odds and the effect of control interventions on the change of parasitaemia risk in Uganda during 2009–2014. Furthermore, we estimated the probability of parasitaemia risk decline and the number of infected children at the two survey time points.
Our study results showed a strong ITNs effect on parasitaemia risk reduction during 2009–2014 following a two-fold increase in coverage in the 5 years. These results support findings in similar malaria endemic settings [3]. This protective effect can be attributed to the physical barrier provided by ITNs to block mosquitoes from infecting humans with Plasmodium sporozoites, thus preventing parasites from completing their development cycle [19]. Also, the insecticide in ITNs reduces the lifespan of vectors when they come into contact, thus decreasing the chances of transmission [6]. Furthermore, the high coverage and utilization registered in the country may have achieved a ‘mass effect’ that reduces the mosquito population and thus protects people in communities who are not using ITNs but live in close proximity to households with ITNs [20, 21].
The high increase in ITNs coverage can be credited to increased donor support that funded ITNs purchase and distribution through effective distribution outreach channels [8]. These channels include mass distribution campaigns, antenatal care clinics, Expanded Program for Immunization (EPI), and commercial sale of subsidized ITNs through the private sector. These distribution channels have had an immediate success of raising the proportion of households possessing at least one ITN from less than 50% to more than 90%. In spite of the high ITN coverage across the country, ITN effects on parasitaemia odds reduction varied with region. Effects were highest in regions which were initially the most high burdened in 2009. The varying effects of interventions could be explained by regional heterogeneities in malaria transmission rates [22], ecology, and access to health services [23].
Furthermore, case management with ACTs was strongly associated with parasitaemia risk reduction following a three-fold increase in coverage during the study period. Prompt treatment of malaria with ACTs suppresses and kills malaria parasites in the body which prevents progression to severe disease, thus reducing transmission and subsequently parasitaemia load in the population [24]. In line with our study findings, Bhatt et al. [3] also found that ACTs together with ITNs were the most impactful interventions on malaria risk reduction in African endemic countries during 2000–2015. Also, effects of ACTs also varied with region. However, despite the two-fold increase in ACTs coverage in the 5 years, its coverage was still lower than targeted. This could possibly be attributed to supply chain constraints [25], the semi-regulated private health facilities and drug stores and the inadequate laboratory diagnostic capacity in most of the lower level facilities [8].
Indoor residual house spraying also had a very strong effect on parasitaemia odds reduction despite its coverage remaining static between 2009 and 2014. The endophilic behavior of the predominant Anopheles spp. mosquitoes makes this intervention highly effective in Uganda as vectors are killed by the insecticide as they rest on house walls after taking a blood meal [26]. The static coverage is perhaps explained by the high costs involved in IRS implementation. This prompted NMCP to roll out IRS gradually initially starting in 2009 with the 10 most high malaria burden districts located in the Mid-North region [8]. Following a significant reduction in malaria transmission in the 10 districts [27], IRS was later extended to another 14 high burden districts in the North-East, Mid-Eastern, and East-Central regions. Effectiveness of IRS on malaria risk reduction has been reported in other studies in Uganda [27], Kenya [28], Bioko, Equatorial Guinea and Mozambique [29].
Our results further showed that urban areas were associated with a decreased parasitaemia risk compared to rural areas. This could be explained by uneven access to healthcare services between urban and rural areas in developing countries [30]. In Uganda, lower level health facilities, which are the major source of health services in rural areas, are poorly equipped and understaffed [31]. On the other hand, urban areas are served by a much bigger network of better equipped higher level facilities both public and private. Indeed urbanization is one of the reasons that has been suggested as a strong possible causal factor of the downward trend of malaria risk in the pre-intervention period [32]. The effect of urbanization on socio-economic and landscape changes mitigates the risk of malaria transmission. The inverse relationship between urbanization and malaria risk has also been reported in other malaria endemic settings [32–35].
Higher socio-economic status was strongly associated with parasitaemia odds reduction. Related to this finding, our results also showed that the highest probability of parasitaemia decline was attained in Kampala region and the lowest in the North-East region. The former is the capital city and the most developed region, while the latter is the least developed and most hard-to-reach region in Uganda. Socio-economic status affects the ability to afford healthcare services, better housing conditions, and knowledge of malaria prevention [36], which are important determinants of severity and outcome of the disease. These results are in agreement with other studies that reported a higher burden of malaria among poor countries [37] and in hard-to-reach areas [6, 37]. This finding augments evidence that malaria is a disease associated with poverty [38, 39] and low socio-economic development [39–42].
Furthermore, increased land surface temperature and rainfall between 2009 and 2014 were associated with a higher parasitaemia risk. This result is expected since malaria is a vector-borne disease sensitive to changes in climatic conditions [2]. Temperature influences the speed of development of mosquitoes and Plasmodium parasites [43]. Rainfall is the most important driver of mosquito population dynamics and malaria transmission because it provides the optimal humidity and medium for mosquito fertilization and breeding [44, 45].
Although a reduction in parasitaemia risk was achieved in all regions, nevertheless, parasitaemia risk was still high in the regions of North-East, West Nile, and East-Central compared to other regions. This disproportionately high risk in these regions in spite of the high intervention coverage might be attributed to low socio-economic development [46], and limited access to health services [23]. In the case of East-Central region, rice growing practiced in this region has been documented as a potential driver of malaria risk transmission due to the large swamps that provide a favorable habitat for mosquito breeding [47]. Similarly, other studies have reported a higher malaria risk in settings with low socio-economic status [42], poor access to health services [39], and rice paddies [48].
The strong reduction in the estimated number of malaria-infected children may also underline the effect of increases in interventions coverage [9], urbanization [49], and generally improving socio-economic conditions [50].
Conclusions
Our study demonstrates that malaria control interventions have had a strong effect on the decline of parasitaemia risk in Uganda during 2009–2014, albeit with varying magnitude in the regions. This success should be sustained by optimizing ITN coverage to achieve universal coverage and by timely replacing worn-out ITNs. NMCP should sustain the malaria prevention awareness campaigns through the use of Information, Education and Communication (IEC) materials to further promote the use of ITNs. In the high burden districts where IRS implementation is on-going, efforts should be made to ensure that all households are sprayed periodically every 6 months. NMCP should address the problems limiting ACTs coverage scale-up by providing free RDTs to all healthcare providers in line with the WHO ‘Test and Treat’ campaign, and increasing supervision for private health facilities. The varying intervention effects in different regions maybe an indication that interventions work differently in different regions of the country. This therefore calls for a better understanding of the environmental and entomological conditions in each region to tailor a combination of interventions suitable to local settings that will have maximum reduction on transmission. Also, in the regions where the risk remains disproportionately high, NMCP needs to conduct specific studies to understand human and/or vector behavior responsible for this problem. In these regions, other tools should be introduced such as chemoprevention especially in the high risk group of children less than 5 years and mass drug administration to reduce the parasite load in the population. In order to maximize intervention effects and avert reversal in malaria risk reduction, government and donor funded poverty reduction programs should prioritize regions/districts where socio-economic conditions are low. In summary, the ambitious targets of UMRSP 2014–2020 can be achieved if the country commits to implementing an integrated package to cover all aspects of disease prevention, management, and health. However, this will only be possible if the current funding portfolio is increased from the contemporary less than $1 average per head per year to the recommended $4 per head per year [51] equivalent to $140 million per year.
Additional files
Details of statistical models to estimate parasitaemia risk, effects of interventions on the change of parasitaemia risk, and spatially varying interventions effects. (DOCX 40 kb)
Joint posterior distributions of the fitted statistical models. (DOCX 32 kb)
Malaria intervention coverage in 2009 and 2014. Percentage of households with one ITN (a), percentage of households with at least 1 ITN for every two people (b), percentage of population with access to an ITN (c), percentage of population that slept under an ITN the previous night (d), percentage of children less than 5 years who slept under an ITN the previous night (e), proportion of fever episodes treated with any ACT (f). (PDF 211 kb)
Acknowledgments
We are grateful to Uganda Ministry of Health, MCP, Uganda Bureau of Statistics (UBOS), Makerere University School of Public Health, DHS MEASURE, PMI and the Global Fund.
Funding
This research was supported and funded by the Swiss Programme for Research on Global Issues for Development (r4d) project no. IZ01Z0–147,286 and the European Research Council (ERC) advanced grant project no. 323180.
Availability of data and materials
The DHS MEASURE program prohibits researchers from redistributing data as per their “Dataset Terms of Use”. However, the data are available in the DHS MEASURE program website (www.dhsprogram.com) upon request following data access instructions (http://dhsprogram.com/data/Access-Instructions.cfm). Also, data can be requested through the following contact; Tel: (301) 572–0851, E-mail: archive@dhsprogram.com.
Abbreviations
- ACTs
Artemisinin combination therapies
- BCI
Bayesian credible intervals
- DHS
Demographic health survey
- EWES
Environmental monitoring system
- GRUMP
Global rural-urban mapping project
- IRS
Indoor residual spraying
- ITNs
Insecticide treated nets
- LST
Land surface temperature
- MIS
Malaria indicator surveys
- MODIS
Moderate resolution imaging spectroradiometer
- MoH
Ministry of Health
- NDVI
Normalized difference vegetation index
- NMCP
National malaria control program
- PMI
President’s malaria initiative
- RS
Remote sensing
- SSA
Sub-Saharan Africa
- UMRSP
Uganda malaria reduction strategic plan (UMRSP)
- WHO
World Health Organization
Authors’ contributions
JS developed methodology, analyzed and synthesized data, fitted models, carried out data validation, and wrote the manuscript; BN participated in data analysis and synthesis; JK carried out data curation and participated in manuscript writing; BA carried out data curation and participated in manuscript writing; FM formulated research goals and objectives, participated in the process of acquisition of project financial support, and manuscript writing; SK formulated research goals and objectives, planned, coordinated, and executed research, and manuscript writing; PV formulated research goals and objectives, planned, coordinated, and executed research, spearheaded study methodology development, and manuscript writing. All authors read and approved the final manuscript.
Ethics approval and consent to participate
In this study we analyzed secondary data made available by the Demographic Health Survey (DHS) MEASURE. According to survey protocols and related documents of the two surveys, ethical approval was obtained from the Institutional Review Board of International Consulting Firm (ICF) of Calverton, Maryland, USA, and also from Makerere University School of Biomedical Sciences Higher Degrees Research and Ethics committee (SBS-HDREC), and the Uganda National Council for Science and Technology (UNCST). Details of ethical clearance are published in the Uganda MIS 2009 and MIS 2014–15 reports for the first and second survey, respectively [9, 10].
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (doi: 10.1186/s13071-017-2393-0) contains supplementary material, which is available to authorized users.
Contributor Information
Julius Ssempiira, Email: jssempiira@gmail.com.
Betty Nambuusi, Email: bettynambuusi@gmail.com.
John Kissa, Email: johnkissa@yahoo.com.
Bosco Agaba, Email: bbagaba_bosco@yahoo.com.
Fredrick Makumbi, Email: fmakumbi@musph.ac.ug.
Simon Kasasa, Email: skasasa@musph.ac.ug.
Penelope Vounatsou, Email: penelope.vounatsou@unibas.ch.
References
- 1.World Health Organization. World malaria report: 2016. 2016. Available: http://apps.who.int/iris/bitstream/10665/252038/1/9789241511711-eng.pdf.
- 2.Snow RW, Kibuchi E, Karuri SW, Sang G, Gitonga CW, Mwandawiro C, et al. Changing malaria prevalence on the Kenyan Coast since 1974: climate, drugs and vector control. PLoS One. 2015;10:e0128792. doi: 10.1371/journal.pone.0128792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatt S, Weiss DJ, Cameron E, Bisanzio D, Mappin B, Dalrymple U, et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. 2015;526:207–211. doi: 10.1038/nature15535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhattarai A, Ali AS, Kachur SP, Mårtensson A, Abbas AK, Khatib R, et al. Impact of artemisinin-based combination therapy and insecticide-treated nets on malaria burden in Zanzibar. PLoS Med. 2007;4:e309. doi: 10.1371/journal.pmed.0040309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lengeler C. Insecticide-treated bed nets and curtains for preventing malaria. Cochrane Database Syst Rev. 2004;(2):CD000363. [DOI] [PubMed]
- 6.WHO, UNICEF. WHO | Achieving the malaria MDG target: reversing the incidence of malaria 2000–2015. In: WHO 2015. Available: http://www.who.int/malaria/publications/atoz/9789241509442/en/. Accessed 10 June 2017.
- 7.Katureebe A, Zinszer K, Arinaitwe E, Rek J, Kakande E, Charland K, et al. Measures of malaria burden after long-lasting insecticidal net distribution and indoor residual spraying at three sites in Uganda: A prospective observational study. PLoS Med. 2016;13:e1002167. doi: 10.1371/journal.pmed.1002167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Malaria Control Program. Uganda Malaria Operational Plan. 2016. Available: https://www.pmi.gov/docs/default-source/default-document-library/malaria-operational-plans/fy16/fy-2016-uganda-malaria-operational-plan.pdf?sfvrsn=5
- 9.Uganda Bureau of Statistics and ICF International. Uganda Malaria Indicator Survey 2014–15. Kampala, Uganda, and Rockville, Maryland: UBOS and ICF International 2015. Available: https://dhsprogram.com/pubs/pdf/MIS21/MIS21.pdf. Accessed 30 May 2016.
- 10.Uganda Bureau of Statistics and ICF International. Uganda Malaria Indicator Survey 2009. Kampala, Uganda, and Rockville, Maryland: UBOS and ICF International.2010 Available: https://dhsprogram.com/pubs/pdf/MIS6/MIS6.pdf. Accessed 30 May 2016.
- 11.O’Meara WP, Mangeni JN, Steketee R, Greenwood B. Changes in the burden of malaria in sub-Saharan Africa. Lancet Infect Dis. 2010;10:545–555. doi: 10.1016/S1473-3099(10)70096-7. [DOI] [PubMed] [Google Scholar]
- 12.Giardina F, Kasasa S, Sié A, Utzinger J, Tanner M, Vounatsou P. Effects of vector-control interventions on changes in risk of malaria parasitaemia in sub-Saharan Africa: a spatial and temporal analysis. Lancet Glob Health. 2014;2:e601–e615. doi: 10.1016/S2214-109X(14)70300-6. [DOI] [PubMed] [Google Scholar]
- 13.WHO . World Malaria Report 2015. Geneva: WHO; 2015. [Google Scholar]
- 14.World Health Organisation. Household Survey Indicators for Malaria Control 2013. Available: http://www.malariasurveys.org/documents/Household%20Survey%20Indicators%20for%20Malaria%20Control.pdf.
- 15.Global Rural-Urban Mapping Project (GRUMP), v1 | SEDAC. Available: http://sedac.ciesin.columbia.edu/data/collection/grump-v1. Accessed 3 Feb 2017.
- 16.Worldpop dataset download. Worldpop. Available: http://www.worldpop.org.uk/. Accessed 30 May 2016.
- 17.Uganda Bureau of Statistics. The National Population and Housing Census 2014 - Main Report, Kampala, Uganda 2016. Available: http://www.ubos.org/onlinefiles/uploads/ubos/NPHC/NPHC%202014%20FINAL%20RESULTS%20REPORT.pdf. Accessed 14 Sep 2016.
- 18.Chammartin F, Scholte RG, Malone JB, Bavia ME, Nieto P, Utzinger J, et al. Modelling the geographical distribution of soil-transmitted helminth infections in Bolivia. Parasit Vectors. 2013;6:152. doi: 10.1186/1756-3305-6-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bueno-Mari R, Jimenez-Peydro R. Global change and human vulnerability to vector-borne diseases. Lausane: Frontiers Media SA; 2010. [DOI] [PMC free article] [PubMed]
- 20.Louis VR, Bals J, Tiendrebéogo J, Bountogo M, Ramroth H, De Allegri M, et al. Long-term effects of malaria prevention with insecticide-treated mosquito nets on morbidity and mortality in African children: randomised controlled trial. Tropical Med Int Health. 2012;17:733–741. doi: 10.1111/j.1365-3156.2012.02990.x. [DOI] [PubMed] [Google Scholar]
- 21.Maxwell CA, Msuya E, Sudi M, Njunwa KJ, Carneiro IA, Curtis CF. Effect of community-wide use of insecticide-treated nets for 3–4 years on malarial morbidity in Tanzania. Trop Med Int Health TM IH. 2002;7:1003–1008. doi: 10.1046/j.1365-3156.2002.00966.x. [DOI] [PubMed] [Google Scholar]
- 22.Okello PE, Van Bortel W, Byaruhanga AM, Correwyn A, Roelants P, Talisuna A, et al. Variation in malaria transmission intensity in seven sites throughout Uganda. Am J Trop Med Hyg. 2006;75:219–225. [PubMed] [Google Scholar]
- 23.Yeka. Malaria in Uganda: Challenges to control on the long road to elimination: I. Epidemiology and current control efforts 2012. Available: http://www.sciencedirect.com/science/article/pii/S0001706X11000611. Accessed 28 Nov 2016. [DOI] [PMC free article] [PubMed]
- 24.Baird JK. Real-world therapies and the problem of vivax malaria. N Engl J Med. 2008;359:2601–2603. doi: 10.1056/NEJMe0808729. [DOI] [PubMed] [Google Scholar]
- 25.Kiwanuka SN, Ekirapa EK, Peterson S, Okui O, Rahman MH, Peters D, et al. Access to and utilisation of health services for the poor in Uganda: a systematic review of available evidence. Trans R Soc Trop Med Hyg. 2008;102:1067–1074. doi: 10.1016/j.trstmh.2008.04.023. [DOI] [PubMed] [Google Scholar]
- 26.Becker N, Petric D, Zgomba M, Boase C, Minoo M, Dahl C, et al. Mosquitoes and their control. New York: Springer; 2010. [Google Scholar]
- 27.Bukirwa H, Yau V, Kigozi R, Filler S, Quick L, Lugemwa M, et al. Assessing the impact of indoor residual spraying on malaria morbidity using a sentinel site surveillance system in Western Uganda. Am J Trop Med Hyg. 2009;81:611–614. doi: 10.4269/ajtmh.2009.09-0126. [DOI] [PubMed] [Google Scholar]
- 28.Zhou G, Githeko AK, Minakawa N, Yan G. Community-wide benefits of targeted indoor residual spray for malaria control in the Western Kenya Highland. Malar J. 2010;9:67. doi: 10.1186/1475-2875-9-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kleinschmidt I, Schwabe C, Shiva M, Segura JL, Sima V, Mabunda SJA, et al. Combining indoor residual spraying and insecticide-treated net interventions. Am J Trop Med Hyg. 2009;81:519–524. [PMC free article] [PubMed] [Google Scholar]
- 30.Dolea C. Increasing access to health workers in remote and rural areas through improved retention: global policy recommendations. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- 31.Pariyo GW, Ekirapa-Kiracho E, Okui O, Rahman MH, Peterson S, Bishai DM, et al. Changes in utilization of health services among poor and rural residents in Uganda: are reforms benefitting the poor? Int J Equity Health. 2009;8:39. doi: 10.1186/1475-9276-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tatem AJ, Gething PW, Smith DL, Hay SI. Urbanization and the global malaria recession. Malar J. 2013;12:133. doi: 10.1186/1475-2875-12-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Omumbo JA, Guerra CA, Hay SI, Snow RW. The influence of urbanisation on measures of Plasmodium falciparum infection prevalence in East Africa. Acta Trop. 2005;93:11–21. doi: 10.1016/j.actatropica.2004.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ramroth H, Ndugwa RP, Müller O, Yé Y, Sié A, Kouyaté B, et al. Decreasing childhood mortality and increasing proportion of malaria deaths in rural Burkina Faso. Glob Health Action. 2009;2:1909. doi: 10.3402/gha.v2i0.1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang S-J, Lengeler C, Smith TA, Vounatsou P, Diadie DA, Pritroipa X, et al. Rapid urban malaria appraisal (RUMA) I: Epidemiology of urban malaria in Ouagadougou. Malar J. 2005;4:43. doi: 10.1186/1475-2875-4-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yadav K, Dhiman S, Rabha B, Saikia P, Veer V. Socio-economic determinants for malaria transmission risk in an endemic primary health centre in Assam, India. Infect Dis Poverty. 2014;3:19. doi: 10.1186/2049-9957-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Snow RW, Marsh K. Malaria in Africa: progress and prospects in the decade since the Abuja Declaration. Lancet. 2010;376:137–139. doi: 10.1016/S0140-6736(10)60577-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sachs J, Malaney P. The economic and social burden of malaria. Nature. 2002;415:680–685. doi: 10.1038/415680a. [DOI] [PubMed] [Google Scholar]
- 39.Tanner M, de Savigny D. Malaria eradication back on the table. Bull World Health Organ. 2008;86:82. doi: 10.2471/BLT.07.050633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Feachem R, Sabot O. A new global malaria eradication strategy. Lancet. 2008;371:1633–1635. doi: 10.1016/S0140-6736(08)60424-9. [DOI] [PubMed] [Google Scholar]
- 41.Greenwood BM, Fidock DA, Kyle DE, Kappe SHI, Alonso PL, Collins FH, et al. Malaria: progress, perils, and prospects for eradication. J Clin Invest. 2008;118:1266–1276. doi: 10.1172/JCI33996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Protopopoff N, Bortel WV, Speybroeck N, Geertruyden J-PV, Baza D, D’Alessandro U, et al. Ranking malaria risk factors to guide malaria control efforts in African highlands. PLoS One. 2009;4:e8022. doi: 10.1371/journal.pone.0008022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gullan PJ, Cranston PS. The Insects: An Outline of Entomology. 5. New York: Wiley-Blackwell; 2014. [Google Scholar]
- 44.Githeko AK, Ndegwa W. Predicting malaria epidemics in the Kenyan highlands using climate data: a tool for decision makers. Glob Change Hum Health. 2001;2:54–63. doi: 10.1023/A:1011943131643. [DOI] [Google Scholar]
- 45.Kynast-Wolf G, Hammer GP, Müller O, Kouyaté B, Becher H. Season of death and birth predict patterns of mortality in Burkina Faso. Int J Epidemiol. 2006;35:427–435. doi: 10.1093/ije/dyi150. [DOI] [PubMed] [Google Scholar]
- 46.Ministry of Finance. Uganda poverty status report 2014. Available: zotero://report/items/0_H927KNFD/html/report.html. Accessed 27 Nov 2016.
- 47.Pullan RL, Bukirwa H, Staedke SG, Snow RW, Brooker S. Plasmodium infection and its risk factors in eastern Uganda. Malar J. 2010;9:2. doi: 10.1186/1475-2875-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Diboulo E, Sié A, Vounatsou P. Assessing the effects of malaria interventions on the geographical distribution of parasitaemia risk in Burkina Faso. Malar J. 2016;15:228. doi: 10.1186/s12936-016-1282-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kigozi SP, Pindolia DK, Smith DL, Arinaitwe E, Katureebe A, Kilama M, et al. Associations between urbanicity and malaria at local scales in Uganda. Malar J. 2015;14:374. doi: 10.1186/s12936-015-0865-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tusting LS, Rek J, Arinaitwe E, Staedke SG, Kamya MR, Cano J, et al. Why is malaria associated with poverty? Findings from a cohort study in rural Uganda. Infect Dis Poverty. 2016;5:78. doi: 10.1186/s40249-016-0164-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Teklehaimanot A, McCord GC, Sachs JD. Scaling up malaria control in Africa: an economic and epidemiological assessment. Am J Trop Med Hyg. 2007;77:138–44. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Details of statistical models to estimate parasitaemia risk, effects of interventions on the change of parasitaemia risk, and spatially varying interventions effects. (DOCX 40 kb)
Joint posterior distributions of the fitted statistical models. (DOCX 32 kb)
Malaria intervention coverage in 2009 and 2014. Percentage of households with one ITN (a), percentage of households with at least 1 ITN for every two people (b), percentage of population with access to an ITN (c), percentage of population that slept under an ITN the previous night (d), percentage of children less than 5 years who slept under an ITN the previous night (e), proportion of fever episodes treated with any ACT (f). (PDF 211 kb)
Data Availability Statement
The DHS MEASURE program prohibits researchers from redistributing data as per their “Dataset Terms of Use”. However, the data are available in the DHS MEASURE program website (www.dhsprogram.com) upon request following data access instructions (http://dhsprogram.com/data/Access-Instructions.cfm). Also, data can be requested through the following contact; Tel: (301) 572–0851, E-mail: archive@dhsprogram.com.


