Abstract
There have been several techniques to repair the medial meniscus posterior root tears (MMPRTs) with the goal of restoring the anatomic and firm fixation of the meniscal root to bone. Many anatomic studies about the menisci also have been developed, so a better understanding of the anatomy could help surgeons perform correct fixation of the MMPRTs. The meniscal roots have ligament-like structures that firmly attach the menisci to the tibial plateau, and this structural concept is important to restore normal biomechanics after anatomic root repair. We present arthroscopic transtibial medial meniscus posterior root reconstruction using auto-gracilis tendon.
The medial meniscus posterior root tears (MMPRTs) lead to the loss of hoop tension and load transmissibility of the knee joint, and these result in a biomechanical condition much like total meniscectomy.1 Ultimately, the significant decrease in the contact area and increase in the contact pressure of the weight-bearing portion leads to accelerated joint degeneration; hence, the early detection and repair of MMPRTs is important.1, 2 The current techniques developed to repair MMPRTs are transtibial pullout repair and suture anchor repair with goals of restoring the native structure and function of the menisci.2, 3, 4, 5 Although clinical studies revealed considerable improvement in subjective clinical scores at minimal 2 years after transtibial pullout or suture anchor repairs, structural outcomes evaluated with magnetic resonance imaging (MRI) or second-look arthroscopy have reported somewhat disappointing results.2, 3, 5, 6, 7
Several anatomic studies to analyze the medial meniscus posterior root have been reported as a result of the growing interest in treatment of MMPRTs, and better understanding of the anatomy could help surgeons perform correct fixation of MMPRTs.8, 9, 10 Andrews et al.10 proved that the meniscus posterior root, or insertional ligament, firmly attached the menisci to the tibial plateau, and it had a ligament-like structure that transitions into the fibrocartilaginous structure of the meniscal body. We focused on this structural concept and developed a technique for suitable medial meniscus posterior root refixation. We describe the surgical technique of arthroscopic transtibial medial meniscus posterior root reconstruction using auto-gracilis tendon (Video 1).
Surgical Technique
Auto-Gracilis Tendon Harvest and Preparation
After confirmation for the MMPRT on arthroscopic examination, an approximately 3-cm longitudinal skin incision is made 2 cm medial to the tibial tuberosity and the sartorius fascia from pes anserinus is peeled; the gracilis tendon is then separated and extracted. The graft with a diameter of 4 mm is prepared by placing a no. 2 Ethibond suture (Ethicon, Somerville, NJ) in a whipstitch interlocking fashion. Then, the superficial medial collateral ligament is released from the distal tibial attachment by periosteal stripping while keeping the proximal tibial attachment and deep medial collateral ligament intact to provide sufficient working space as explained in a previous article.5 The soft tissue is detached from the previously incised area to allow direct placement of an anterior cruciate ligament reconstruction tibial tunnel guide (Linvatec) on the cortex.
Tibial Tunnel Preparation
Viewing from the anterolateral portal, the torn medial meniscus posterior root is debrided to refine the edge, and landmarks relevant to the insertion of the posterior root of the medial meniscus, including the posterior cruciate ligament insertion, medial tibial spine, and articular margin of the tibial plateau, are identified. The anterior cruciate ligament reconstruction tibial guide (Linvatec) tip is placed at the anatomic posterior root insertion via the anteromedial portal; a guide pin is then drilled through the guide from the medial side of the tibial tuberosity. After confirming that the tibial tunnel is suitable and the guide pin is well positioned, the guide pin is pulled back through. Next, a 6-mm FlipCutter (Arthrex, Naples, FL) is introduced into the anatomic root insertion from the exit of the tibial tunnel following the previously drilled tibial tunnel and then it is retro-drilled to the exit of the tibial tunnel, making a 6-mm-wide tibial tunnel (Fig 1).
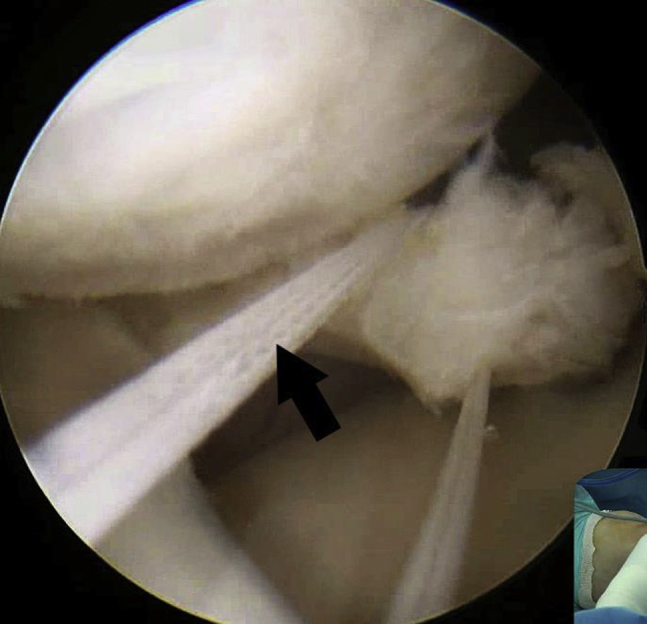
Fig 1.

Viewing from the anterolateral portal, a 6-mm-wide tibial tunnel is created using FlipCutter (Arthrex) at the anatomic medial meniscus posterior root insertion (black arrow) on the left knee.
Graft Passage and Fixation
The crescent-shaped suture hook (Linvatec), loaded with no. 1 polydioxanone (PDS) (Ethicon), is passed through the anteromedial portal, viewing from the anterolateral portal. The torn posterior horn is penetrated by the sharp tip of the suture hook 5 to 8 mm medial to the torn edge in a vertical direction from the femoral to the tibial side (Fig 2). Then, no. 1 PDS is advanced through the suture hook, and the tibial side of the no. 1 PDS is taken out through the anteromedial portal using a suture retriever. Using the shuttle relay method, the no. 1 PDS is exchanged with the FiberWire (Arthrex) (Fig 3). The FiberWire is replaced by the graft passing the torn posterior horn with the shuttle relay method (Fig 4). A suture-passing wire loop positioned anteriorly is inserted from the exit of the tibial tunnel to root insertion and taken out through the anteromedial portal to pass the graft. Next, both ends of the graft, connected to the suture-passing wire loop, are pulled out from outside of the anteromedial portal to the exit of the tibial tunnel (Fig 5). The displaced posterior horn is reduced and stabilized when the ends of the sutures of the graft are pulled through the tibia tunnel under adequate tension allowing physiological excursion, and the graft is firmly fixed using a 5.5-mm bioabsorbable interference screw (Arthrex) with the knee at 30° to 45° of flexion. A final arthroscopic evaluation is performed to confirm the reconstructed posterior root and tension of the entire medial meniscus (Fig 6).
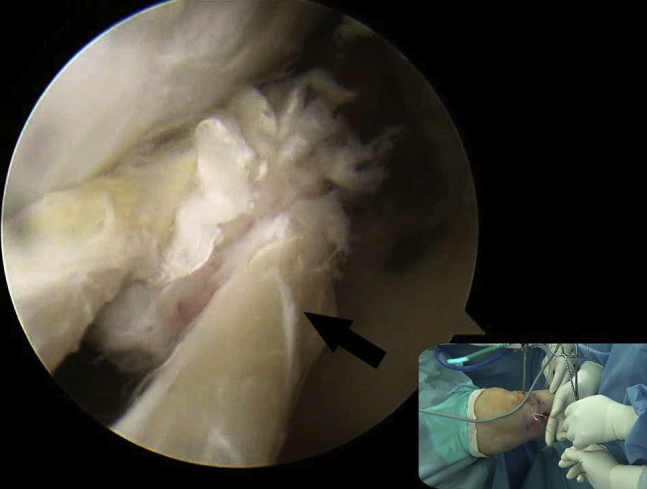
Fig 2.

Viewing from the anterolateral portal, the sharp tip of the suture hook with PDS is advanced to the torn posterior horn via the anteromedial portal. Then, the torn posterior horn is penetrated by the sharp tip of the suture hook 5-8 mm medial to the torn edge (black arrow) in a vertical direction on the left knee with valgus force at extension. (PDS, polydioxanone.)
Fig 3.
The previously passed no. 1 PDS is exchanged with the FiberWire (Arthrex) using the shuttle relay method on the left knee with valgus force at extension, viewing from the anterolateral portal. Outside the anteromedial portal, the no. 1 PDS and FiberWire are tied before the shuttle relay. Black arrow indicates FiberWire. (PDS, polydioxanone.)
Fig 4.
The FiberWire is replaced by the graft (black arrow) passing the torn posterior horn with the shuttle relay method on the left knee with valgus force at extension, viewing from the anterolateral portal. Outside the anteromedial portal, the graft is connected to the FiberWire before the shuttle relay.
Fig 5.

Viewing from the anterolateral portal, the auto-gracilis graft is taken out from outside the anteromedial portal to the exit of the tibial tunnel on the left knee with valgus force at extension by pulling out the suture-passing wire and both ends of the graft outside the tibial tunnel. The displaced posterior horn (white arrow) is reduced by pulling out both ends of the auto-gracilis graft (black arrow).
Fig 6.

Viewing from the anterolateral portal, the medial meniscus posterior horn is reduced and stabilized after the posterior root reconstruction on the left knee after tibial fixation.
Table 1 describes advantages and disadvantages of this technique. Pitfalls and tips are described in Table 2.
Table 1.
Advantages and Disadvantages of Medial Meniscus Root Reconstruction Using Auto-Gracilis Graft
| Advantages |
| 1. Reconstruction of the medial meniscus posterior root can restore hoop tension and prevent cartilage degeneration. |
| 2. Reconstruction using auto hamstring graft provides a more anatomic structural restoration for the insertional ligament. |
| 3. Posterior portals are not required for the procedures as a result of the widened working space and good visualization after superficial medial collateral ligament release. |
| Disadvantages |
| 1. Meniscal root reconstruction is technically demanding and a learning curve is in play. |
| 2. If the torn meniscal tissue is of poor quality, graft passage would be difficult. |
| 3. There could be donor site morbidity. |
Table 2.
Pitfalls and Tips
| Pitfalls |
| 1. It is difficult to make a posterior root footprint in the anatomic position and to perform root reconstruction under arthroscopy through a tight posteromedial joint space. |
| 2. The edge of torn meniscus can be damaged when the graft is passed through it using the shuttle relay method. |
| 3. If the meniscal extrusion is severe, it is difficult to reduce the displaced meniscal posterior horn. |
| Tips |
| 1. Superficial medial collateral ligament release is performed using a periosteum elevator to obtain increased medial compartment opening, which can provide better visualization and working space and avoid cartilage damage. |
| 2. The knot of the PDS suture is tied back and forth several times gradually to create space for graft passage in the torn meniscus. |
| 3. Meniscal release from coronary ligament and capsule using electrocautery would be helpful in reducing the displaced meniscal posterior horn. |
PDS, polydioxanone.
Discussion
The purpose of this Technical Note was to describe an arthroscopic transtibial anatomic reconstruction of the medial meniscus posterior root using an auto-gracilis graft. In MMPRTs, restoration of hoop tension with repair or refixation of the torn posterior root has been shown to be important for delaying the progression of the arthritis; thus, several fixation techniques including transtibial pullout repair and suture anchor repair have been conducted.2, 3, 4, 5 A recent systematic review concluded that transtibial pullout repair for MMPRT yielded good to excellent functional outcome in all scores used, and no study reported statistically significant progression of Kellgren-Lawrence grading at short-term follow-up.7 However, they reported that the unsatisfactory outcomes regarding healing rates and meniscal extrusion were found. They showed that reduced medial meniscal extrusion was achieved in only 56% and complete healing of the repaired root in only 62%.7 In the second-look arthroscopic results of transtibial pull-out repair reported by Seo et al.,11 they resulted in suture relaxation, tissue slacking and degeneration, and loose healing in all patients. Jung et al.12 used suture anchor for repair of MMPRT and reported that only 50% of 13 patients had complete healing on follow-up MRI. Chung et al.6 showed that 59% of the 39 patients included in transtibial repair revealed increased meniscal extrusion on postoperative MRI at 1 year after fixation.
Incomplete or failed healing and nonreduced meniscal extrusion may cause weak tensile strength and shock absorption, ultimately progressing to osteoarthritis, as discussed earlier.1, 2, 13 The main goal of medial meniscus posterior root repair is to restore the real anatomy and normal function of the meniscus; hence, better understanding of the anatomy could help slow or ultimately arrest the progression of osteoarthritis.8, 10, 14 Andrews et al.10 showed that there were structural transitions between the posterior roots (insertional ligaments) and the fibrocartilaginous body of the menisci, and these structural details would be important to understand the meniscal load-bearing mechanism in the knee. These strong attachments of the posterior root via insertional ligaments anchor the menisci and allow for the generation of hoop stress in the tissue. Park et al.15 revealed that histologic findings of a healthy medial meniscus posterior root resembled those of a healthy ligament or tendon, with an absence of fibrocartilage throughout the matrix except in the enthesis. They reported that a degenerative posterior root would lose the ability to withstand tensile stresses in the course of fibrocartilage formation, likely contributing to MMPRTs. In this respect, posterior root reconstruction using auto-graft would be an appropriate surgical approach, especially in degenerated and fibrocartilaginous roots with the goal of restoring the anatomic and firm fixation of the meniscal root to bone. However, if the meniscal extrusion is severe, it is difficult to reduce the displaced meniscal posterior horn pulling out of the graft. In this situation, meniscal release from coronary ligament and capsule using electrocautery would be helpful in reducing the displaced meniscal posterior horn. Another challenge is that the edge of the torn meniscus can be damaged when the graft is passed through it using the shuttle relay method. To overcome this, the present authors have made the knot of the PDS and moved it back and forth several times gradually to obtain a space for graft passage in the torn meniscus.
The conventional transtibial pullout repair for MMPRTs has resulted in a bungee effect, which is linked to the micromotion of the root repair caused by the long length of the meniscus suture construct. This bungee effect could lead to considerable displacement under cyclic loading and substantial negative effect on meniscal function.3, 13 The current root reconstruction technique can minimize the bungee effect because the tendon used for root reconstruction is passed through the whole tibial tunnel and fixed using an interference screw construct, and it is less prone to micromotion.
In summary, this arthroscopic medial meniscus posterior root reconstruction using auto-gracilis graft is anticipated to provide a more anatomic structural restoration than previous repair techniques.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
We describe the surgical technique of arthroscopic medial meniscus posterior root reconstruction using the auto-gracilis tendon on the left knee. After confirmation of medial meniscus posterior root tear on arthroscopic examination, an approximately 3-cm longitudinal skin incision is made 2 cm medial to the tibial tuberosity and the sartorius fascia from pes anserinus is peeled; then the gracilis tendon is separated and extracted. The graft with a diameter of 4 mm is prepared by placing a no. 2 Ethibond suture (Ethicon) in a whipstitch interlocking fashion. Then, the superficial medial collateral ligament is released from the distal tibial attachment by periosteal stripping while keeping the proximal tibial attachment and deep medial collateral ligament intact to provide sufficient working space. The soft tissue is detached from the previously incised area to allow direct placement of an anterior cruciate ligament reconstruction tibial tunnel guide (Linvatec) on the cortex. Viewing from the anterolateral portal, the torn medial meniscus posterior root is debrided to refine the edge, and landmarks relevant to the insertion of the posterior root of the medial meniscus, including the posterior cruciate ligament insertion, medial tibial spine, and articular margin of the tibial plateau, are identified. The anterior cruciate ligament reconstruction tibial guide (Linvatec) tip is placed at anatomic posterior root insertion via the anteromedial portal, a guide pin is then drilled through the guide from the medial side of the tibial tuberosity. After confirming that the tibial tunnel is suitable and the guide pin is well positioned, the guide pin is pulled back through. Next, a 6-mm FlipCutter (Arthrex) is introduced into the anatomic root insertion from the exit of the tibial tunnel following the previously drilled tibial tunnel, and then it is retro-drilled to the exit of the tibial tunnel making a 6-mm-wide tibial tunnel. The crescent-shaped suture hook (Linvatec), loaded with no. 1 polydioxanone (Ethicon), is passed through the anteromedial portal, viewing from the anterolateral portal. The torn posterior horn is penetrated by the sharp tip of the suture hook 5-8 mm medial to the torn edge in a vertical direction from the femoral side to the tibial. Then, no. 1 PDS is advanced through the suture hook, and the tibial side of the no. 1 PDS is taken out through the anteromedial portal using a suture retriever. Using the shuttle relay method, the no.1 PDS is exchanged with the FiberWire (Arthrex). The FiberWire is replaced by the graft passing the torn posterior horn with the shuttle relay method. A suture-passing wire loop positioned anteriorly is inserted from the exit of the tibial tunnel to root insertion and taken out through the anteromedial portal to pass the graft. Next, both ends of the graft, connected to the suture-passing wire loop, are pulled out from outside of the anteromedial portal to the exit of the tibial tunnel. The displaced posterior horn is reduced and stabilized when the ends of the sutures of the graft are pulled through the tibia tunnel under adequate tension, allowing physiological excursion, and then the graft is firmly fixed using a 5.5-mm bioabsorbable interference screw (Arthrex) with the knee at 30°-45° of flexion. A final arthroscopic evaluation is performed to confirm the reconstructed posterior root and tension of the entire medial meniscus. This root reconstruction technique can provide an effective and more anatomic structural restoration than previous repair techniques. (PDS, polydioxanone.)
References
- 1.Allaire R., Muriuki M., Gilbertson L., Harner C.D. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 2.Lee D.W., Ha J.K., Kim J.G. Medial meniscus posterior root tear: A comprehensive review. Knee Surg Relat Res. 2014;26:125–134. doi: 10.5792/ksrr.2014.26.3.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.LaPrade R.F., LaPrade C.M., James E.W. Recent advances in posterior meniscal root repair techniques. J Am Acad Orthop Surg. 2015;23:71–76. doi: 10.5435/JAAOS-D-14-00003. [DOI] [PubMed] [Google Scholar]
- 4.Lee D.W., Jang S.H., Ha J.K., Kim J.G., Ahn J.H. Meniscus root refixation technique using a modified Mason-Allen stitch. Knee Surg Sports Traumatol Arthrosc. 2013;21:654–657. doi: 10.1007/s00167-012-1992-8. [DOI] [PubMed] [Google Scholar]
- 5.Lee D.W., Kim M.K., Jang H.S., Ha J.K., Kim J.G. Clinical and radiologic evaluation of arthroscopic medial meniscus root tear refixation: Comparison of the modified Mason-Allen stitch and simple stitches. Arthroscopy. 2014;30:1439–1446. doi: 10.1016/j.arthro.2014.05.029. [DOI] [PubMed] [Google Scholar]
- 6.Chung K.S., Ha J.K., Ra H.J., Nam G.W., Kim J.G. Pullout fixation of posterior medial meniscus root tears: Correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017;45:42–49. doi: 10.1177/0363546516662445. [DOI] [PubMed] [Google Scholar]
- 7.Feucht M.J., Kuhle J., Bode G. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: A systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31:1808–1816. doi: 10.1016/j.arthro.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 8.Ellman M.B., LaPrade C.M., Smith S.D. Structural properties of the meniscal roots. Am J Sports Med. 2014;42:1881–1887. doi: 10.1177/0363546514531730. [DOI] [PubMed] [Google Scholar]
- 9.Smigielski R., Becker R., Zdanowicz U., Ciszek B. Medial meniscus anatomy—From basic science to treatment. Knee Surg Sports Traumatol Arthrosc. 2015;23:8–14. doi: 10.1007/s00167-014-3476-5. [DOI] [PubMed] [Google Scholar]
- 10.Andrews S.H., Rattner J.B., Jamniczky H.A., Shrive N.G., Adesida A.B. The structural and compositional transition of the meniscal roots into the fibrocartilage of the menisci. J Anat. 2015;226:169–174. doi: 10.1111/joa.12265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seo H.S., Lee S.C., Jung K.A. Second-look arthroscopic findings after repairs of posterior root tears of the medial meniscus. Am J Sports Med. 2011;39:99–107. doi: 10.1177/0363546510382225. [DOI] [PubMed] [Google Scholar]
- 12.Jung Y.H., Choi N.H., Oh J.S., Victoroff B.N. All-inside repair for a root tear of the medial meniscus using a suture anchor. Am J Sports Med. 2012;40:1406–1411. doi: 10.1177/0363546512439181. [DOI] [PubMed] [Google Scholar]
- 13.LaPrade R.F., LaPrade C.M., Ellman M.B., Turnbull T.L., Cerminara A.J., Wijdicks C.A. Cyclic displacement after meniscal root repair fixation: A human biomechanical evaluation. Am J Sports Med. 2015;43:892–898. doi: 10.1177/0363546514562554. [DOI] [PubMed] [Google Scholar]
- 14.Bhatia S., LaPrade C.M., Ellman M.B., LaPrade R.F. Meniscal root tears: Significance, diagnosis, and treatment. Am J Sports Med. 2014;42:3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 15.Park do Y., Min B.H., Choi B.H. The degeneration of meniscus roots is accompanied by fibrocartilage formation, which may precede meniscus root tears in osteoarthritic knees. Am J Sports Med. 2015;43:3034–3044. doi: 10.1177/0363546515605086. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
We describe the surgical technique of arthroscopic medial meniscus posterior root reconstruction using the auto-gracilis tendon on the left knee. After confirmation of medial meniscus posterior root tear on arthroscopic examination, an approximately 3-cm longitudinal skin incision is made 2 cm medial to the tibial tuberosity and the sartorius fascia from pes anserinus is peeled; then the gracilis tendon is separated and extracted. The graft with a diameter of 4 mm is prepared by placing a no. 2 Ethibond suture (Ethicon) in a whipstitch interlocking fashion. Then, the superficial medial collateral ligament is released from the distal tibial attachment by periosteal stripping while keeping the proximal tibial attachment and deep medial collateral ligament intact to provide sufficient working space. The soft tissue is detached from the previously incised area to allow direct placement of an anterior cruciate ligament reconstruction tibial tunnel guide (Linvatec) on the cortex. Viewing from the anterolateral portal, the torn medial meniscus posterior root is debrided to refine the edge, and landmarks relevant to the insertion of the posterior root of the medial meniscus, including the posterior cruciate ligament insertion, medial tibial spine, and articular margin of the tibial plateau, are identified. The anterior cruciate ligament reconstruction tibial guide (Linvatec) tip is placed at anatomic posterior root insertion via the anteromedial portal, a guide pin is then drilled through the guide from the medial side of the tibial tuberosity. After confirming that the tibial tunnel is suitable and the guide pin is well positioned, the guide pin is pulled back through. Next, a 6-mm FlipCutter (Arthrex) is introduced into the anatomic root insertion from the exit of the tibial tunnel following the previously drilled tibial tunnel, and then it is retro-drilled to the exit of the tibial tunnel making a 6-mm-wide tibial tunnel. The crescent-shaped suture hook (Linvatec), loaded with no. 1 polydioxanone (Ethicon), is passed through the anteromedial portal, viewing from the anterolateral portal. The torn posterior horn is penetrated by the sharp tip of the suture hook 5-8 mm medial to the torn edge in a vertical direction from the femoral side to the tibial. Then, no. 1 PDS is advanced through the suture hook, and the tibial side of the no. 1 PDS is taken out through the anteromedial portal using a suture retriever. Using the shuttle relay method, the no.1 PDS is exchanged with the FiberWire (Arthrex). The FiberWire is replaced by the graft passing the torn posterior horn with the shuttle relay method. A suture-passing wire loop positioned anteriorly is inserted from the exit of the tibial tunnel to root insertion and taken out through the anteromedial portal to pass the graft. Next, both ends of the graft, connected to the suture-passing wire loop, are pulled out from outside of the anteromedial portal to the exit of the tibial tunnel. The displaced posterior horn is reduced and stabilized when the ends of the sutures of the graft are pulled through the tibia tunnel under adequate tension, allowing physiological excursion, and then the graft is firmly fixed using a 5.5-mm bioabsorbable interference screw (Arthrex) with the knee at 30°-45° of flexion. A final arthroscopic evaluation is performed to confirm the reconstructed posterior root and tension of the entire medial meniscus. This root reconstruction technique can provide an effective and more anatomic structural restoration than previous repair techniques. (PDS, polydioxanone.)


