Myeloproliferative neoplasms (MPNs) including polycythemia vera (PV), essential thrombocythemia (ET), and myelofibrosis (MF) are clonal, progressive, hematological malignancies resulting in the risk of vascular events, splenomegaly, and significant symptom burden, with a high prevalence of fatigue.1,2 These neoplasms are primarily treated with pharmacologic interventions and, despite therapeutic advances in the pharmacologic treatment of MPNs,3 there remains a significant symptom burden, particularly with regard to residual fatigue and constitutional symptoms, even in JAK-inhibitor responders.4,5
There is a need to explore non-pharmacologic approaches (e.g., yoga, diet, meditation) for managing MPN symptom burden. Yoga has proved an effective method to improve a variety of physical and psychosocial outcomes (e.g., fatigue, anxiety and sleep disruption) in those diagnosed with other cancer types.6,7 However, there have been no studies conducted to date which explore the use of yoga in MPN patients. Our prior research indicates that 40% of MPN patients have attempted yoga in order to alleviate fatigue with 63% reporting success at reducing fatigue.8 Yoga, particularly online yoga, may be a feasible approach for MPN cancer patients as it eliminates or addresses many of the commonly-reported barriers to participating in in-person interventions, including fatigue, pain, transportation and scheduling difficulties.9 Therefore, the purpose of this study was to: 1) examine the feasibility (i.e., acceptability, demand, practicality) of a 12-week, home-based, online yoga intervention among MPN patients, 2) to explore the preliminary effects of yoga on symptom burden among MPN patients and, if successful, 3) to generate an effect size to power an efficacy randomized control trial (RCT).
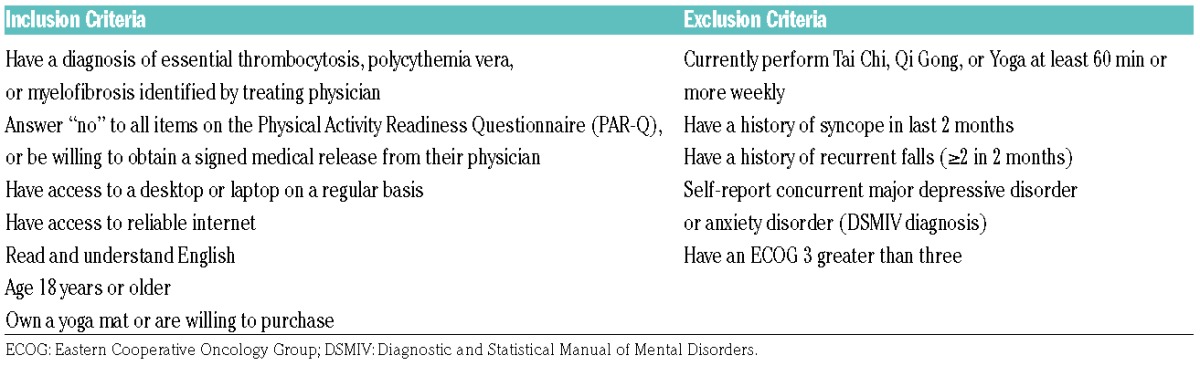
MPN patients (targeted enrollment of 55) were recruited using internet-based strategies (e.g., social media, forums). Inclusion/exclusion criteria are presented in Table 1. Patients participated in a 12-week, home-based, online yoga intervention. They were asked to complete 60 minutes of yoga each week from a prescription (delivered via Udaya.com [Sofia, Bulgaria]) of progressively mild to moderate intensity (and limited use of prone positions to avoid pressure on enlarged spleen or liver). Participants selected options rated as either “beginner” or “intermediate” (some developed especially for this study) based on preference and capacity.
Table 1.
Inclusion/Exclusion Criteria.
Study participants were asked to complete online surveys (via Qualtrics [Provo, UT, USA]) at four time points: baseline (week 1), mid-point (week 7), post-intervention (week 12), and follow-up (week 16). Feasibility (i.e., acceptability, demand, and practicality) was measured following guidelines from Bowen and colleagues.10 We defined feasibility of recruitment as achieving 100% (N=55) of enrollment within 6 months. Acceptability was measured with a satisfaction survey (>70% satisfied with the intervention), intent to continue participating in yoga (>70% with intent to continue), and self-reported perceived appropriateness for the MPN patient. Demand was measured using adherence to the intervention (≥60 minutes/week of yoga participation throughout the 12-week study). Participants were asked to complete a daily log specifying the number of minutes of yoga which they participated in. Objective online yoga minutes were collected through Clicky.com (Portland, OR, USA), an online web analytic software. Practicality was measured with an objective analysis of study participants’ ability to complete study-related activities (>70% completing daily logs and online surveys).
Symptom burden was measured through the Myeloproliferative Neoplasm Symptom Assessment Form Total Symptom Score (MPN-SAF TSS). Patient-reported outcomes included pain intensity, anxiety, depression, sleep disturbance, and sexual function measured using the National Institutes of Health (NIH) Patient Reported Outcomes Measurement Information System (PROMIS).
Patient-reported PROMIS outcomes were scored using the NIH PROMIS Scoring tools. Raw scores for each measure were converted to standardized t-scores for analysis. Changes in symptom data were assessed using paired t-tests and effect sizes (ES).
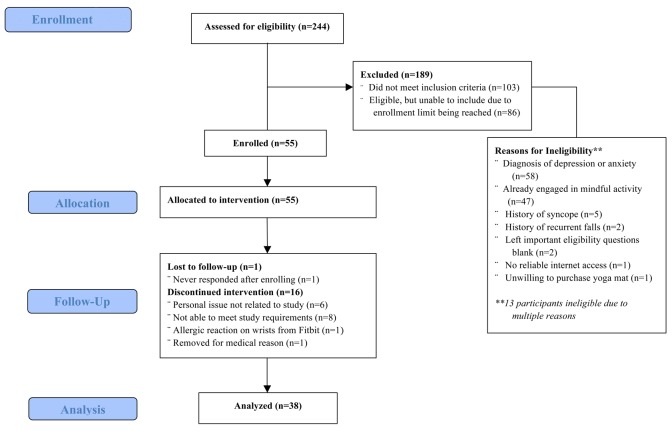
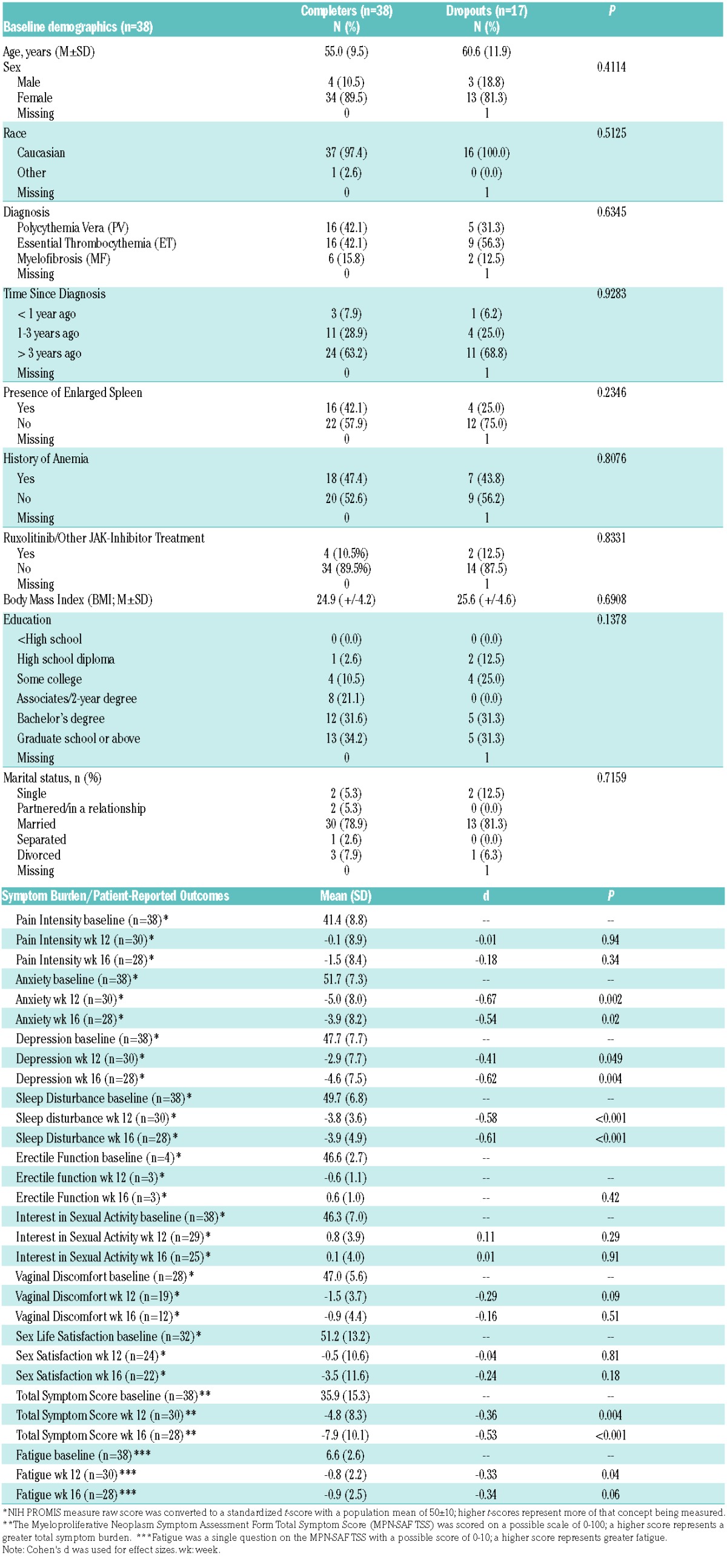
We enrolled 55 MPN patients within 2 weeks, of whom 38 (69%) completed the 12-week intervention. There were no significant differences in baseline demographics between those that completed the intervention (n=38) and those that dropped out (n=17). Figure 1 describes study participant enrollment and Table 2 describes participant demographics at baseline. More than half of those ineligible (n=103) for our study were categorized as such because they reported that they had major depressive disorder, anxiety disorder, and/or post-traumatic stress disorder (n=58).
Figure 1.
Enrollment. Consort flow diagram detailing the flow of study participants
Table 2.
Baseline Demographics and Changes in Myeloproliferative Neoplasm (MPN) Outcomes.
Yoga was well accepted among MPN patients: 68% (n=21/28) of responding participants felt either satisfied or very satisfied with online yoga and 75% (n=23/31) felt that it was helpful for coping with MPN-related symptoms. While only 43% (n=13/31) of MPN patients reported that they were likely to continue their online yoga practice (i.e., demand), 82% (n=25/31) of patients would recommend participating in online yoga to other MPN patients. Additionally, 75% of participants (n=23/31) also reported that they felt safe while participating in online yoga. Although there was 1 adverse event reported (i.e., irritated enlarged spleen), modifications for this participant were provided (altered poses) which alleviated the problem. This information suggests that online yoga may be safe for MPN patients.
Weekly yoga participation averaged ~50 minutes, with 37% of participants adhering to the prescribed intervention of ≥60 min/week (i.e., demand). There were no significant weekly differences between self-reported yoga minutes and objective yoga minutes measured using Clicky, except during week 11 of the intervention (P=0.049). Although slightly less than 40% of participants completed ≥60 minutes/week of yoga, the average participation was just marginally lower (i.e., 10 minutes) than what we prescribed. The completion of ~50 minutes/week (self-report) is promising, especially considering the high levels of fatigue reported in this population.11
Of those that completed the 12-week intervention, 82% (n=31/38) completed the mid-point questionnaire, 79% (n=30/38) completed the post-intervention questionnaire, 74% (n=28/38) completed the follow-up questionnaire and 78% (n=356/456) of the daily logs were completed (i.e., practicality). Other studies in cancer patients utilizing daily reporting have described mixed compliance rates from 41% (daily reporting of sleep) to 88% (daily reporting of quality of life [QoL]).12,13 The relatively high compliance of MPN patients in completing their daily logs demonstrates the practicality of online yoga for these patients.
Table 2 describes pre-post changes in symptom burden and patient-reported outcomes. There were significant improvements in total symptom burden, anxiety, depressive symptoms, sleep disturbance and fatigue after the 12-week intervention as well as significant improvements in outcomes at follow up (i.e., week 16), except for fatigue. Additionally, there were no significant differences in outcomes between those who averaged less than the 60 min/week prescribed weekly yoga duration and those who averaged more. These findings are promising and provide the justification to explore the effectiveness of using yoga to improve symptom burden in MPN patients in a randomized controlled trial.
There are limitations to note, including: 1) the potential for selection bias due to the study being advertised as an online yoga study, 2) the lack of a control group for determining effectiveness, 3) the potential bias in excluding those diagnosed with major depressive disorder, anxiety disorder, and/or posttraumatic stress disorder (which was done to reduce risk in our remote delivery intervention), 4) the self-reported nature of many outcome variables (i.e., questionnaires, daily logs, etc.), which has inherent limitations (e.g., participant recall and social desirability bias), 5) the potential bias in our study sample being primarily of a normal body mass index (BMI), female, and well-educated, which is not representative of the typical MPN patient population,14 and 6) the fact that 17 study participants dropped out of the study, although there were no significant differences at baseline between those that completed the intervention and those that dropped out.
There is unique potential in using online yoga in MPN treatment compared to other cancers due to the scarcity of MPN-specific treatments, the wide dispersion of individuals with this diagnosis, and the chronic nature of the disease. Many MPN patients are left traveling outside of their home state in order to seek their respective treatment. Online, home-based yoga could be an accessible complementary treatment for patients who do not reside in proximity to the center in which they are being treated. Limitations based on the exclusion of nearly a fourth of those screened in our study was not surprising; depressive symptoms have been reported in up to 63% of MPN patients in other studies.8,11,13 Procedures for including a broader range of emotional/mental health compromised individuals will be developed for future studies, particularly because these very symptoms of emotional distress are known to be alleviated with mind-body practices such as yoga.6,7
A 12-week, home-based, online yoga intervention is feasible in MPN patients and shows preliminary promise for improving symptom burden. Participants experienced significant improvements in total symptom burden, anxiety, depression, sleep disturbance and fatigue, with no differences in outcomes between those who completed more or less than the prescribed 60 minutes of yoga each week. This is the first study to explore a complementary approach in MPN patients. Future studies should include a larger, more diverse sample (e.g., MPN patients with clinical levels of depression and anxiety, those with an overweight/obese BMI, more males, and those with lower education levels) in a randomized controlled trial in order to confirm the effectiveness of online yoga. Additionally, the minimum dose of yoga for improving symptom burden in MPN patients should be explored. Findings from this study will inform a randomized controlled trial to determine the efficacy of using online yoga to improve fatigue in MPN patients.
Supplementary Material
Acknowledgments
The authors would like to thank Udaya for their partnership and non-financial support of the study.
Footnotes
Funding: this study was generously supported by philanthropic funds donated to the Mayo Clinic for MPN Research.
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Mehta J, Wang H, Iqbal SU, Mesa R. Epidemiology of myeloproliferative neoplasms in the United States. Leuk Lymphoma. 2014;55(3):595–600. [DOI] [PubMed] [Google Scholar]
- 2.Mesa RA, Niblack J, Wadleigh M, et al. The burden of fatigue and quality of life in myeloproliferative disorders (MPDs): An international internet-based survey of 1179 MPD patients. Cancer. 2007;109(1):68–76. [DOI] [PubMed] [Google Scholar]
- 3.Mascarenhas JO, Talpaz M, Gupta V, et al. Primary analysis of a phase II open-label trial of INCB039110, a selective JAK1 inhibitor, in patients with myelofibrosis. Haematologica. 2017;102:327–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geyer H, Scherber R, Kosiorek H, et al. Symptomatic profiles of patients with polycythemia vera: Implications of inadequately controlled disease. J Clin Oncol. 2016;34(2):151–159. [DOI] [PubMed] [Google Scholar]
- 5.Mesa R, Verstovsek S, Kiladjian J, et al. Changes in quality of life and disease-related symptoms in patients with polycythemia vera receiving ruxolitinib or standard therapy. Eur J Haematol. 2016;97(2):192–200. [DOI] [PubMed] [Google Scholar]
- 6.Buffart LM, Van Uffelen JG, Riphagen II, et al. Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer. 2012;12(1):559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harder H, Parlour L, Jenkins V. Randomised controlled trials of yoga interventions for women with breast cancer: a systematic literature review. Support Care Cancer. 2012;20(12):3055–3064. [DOI] [PubMed] [Google Scholar]
- 8.Scherber RM, Senyak Z, Dueck AC, et al. High prevalence of mood disorders in MPNs and their possible role in MPN related fatigue. Blood. 2014;124(21):3173. [Google Scholar]
- 9.Waart H, Harten WH, Buffart LM, Sonke GS, Stuiver MM, Aaronson NK. Why do patients choose (not) to participate in an exercise trial during adjuvant chemotherapy for breast cancer?. Psychooncology. 2016;25(8):964–970. [DOI] [PubMed] [Google Scholar]
- 10.Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scherber R, Dueck AC, Johansson P, et al. The myeloproliferative neoplasm symptom assessment form (MPN-SAF): International prospective validation and reliability trial in 402 patients. Blood. 2011;118(2):401–408. [DOI] [PubMed] [Google Scholar]
- 12.Harper FW, Heath EI, Gleason ME, et al. Physicians’ use of patients’ daily reports of quality of life to evaluate treatment response in phase I cancer trials. J Cancer Ther. 2012;3(5):582–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Min YH, Lee JW, Shin Y, et al. Daily collection of self-reporting sleep disturbance data via a smartphone app in breast cancer patients receiving chemotherapy: a feasibility study. J Med Internet Res. 2014;16(5):e135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mesa RA, Schwager S, Huang J, et al. Weight loss, splenomegaly, and hypocholesterolemia in myeloproliferative neoplasms: Patterns and relevance from the pre JAK2 inhibitor era. Blood. 2009;114(22):3918. [Google Scholar]
- 15.Geyer HL, Kosiorek H, Dueck AC, et al. Associations between gender, disease features and symptom burden in the MPN population: An analysis by the MPN QOL International Working Group. Haematologica. 2017;102(1):85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.