Abstract
Left atrial appendage (LAA) aneurysm is an extremely rare anomaly. So far, less than one hundred cases only have been reported worldwide. Revelation modes are dominated by complications such as arrhythmias and thromboembolic events. We herein report a pediatric case of huge congenital LAA aneurysm with an original revelation mode that has never been described before in medical literature.
Keywords: Aneurysm, Hiccups, Left atrial appendage
Introduction
Left atrial appendage (LAA) aneurysm is an extremely rare anomaly. Revelation modes are dominated by complications such as arrhythmias and thromboembolic events. We herein report a case of huge LAA aneurysm with an original revelation.
Case report
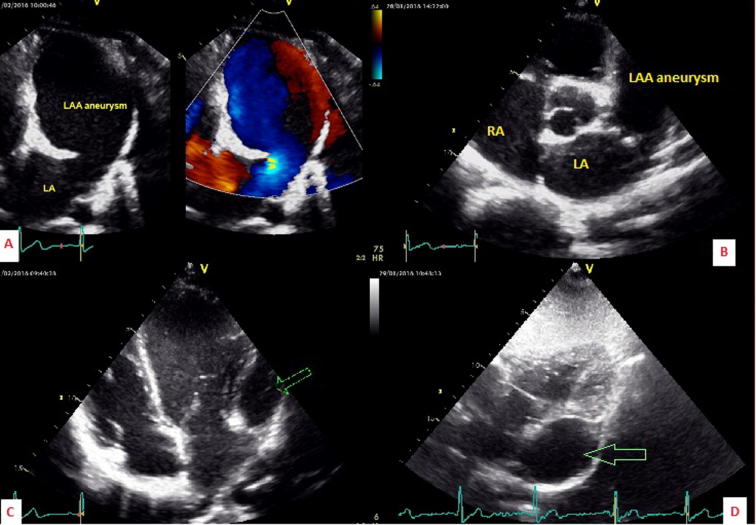
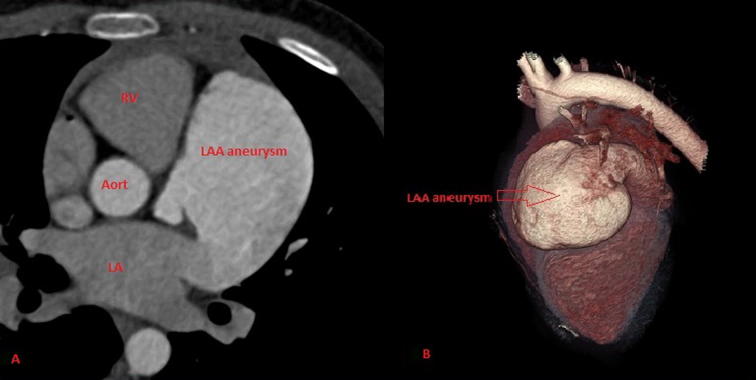
A 14-year-old boy presented to us with persistent hiccups that began about 1 month before. He had a history of pericardial effusion that was diagnosed at the age of 3 years. Physical examination was normal. Electrocardiography revealed sinus rhythm and left ventricular hypertrophy. Chest X-ray (Fig. 1) showed left heart border bulging. Transthoracic echocardiography (Fig. 2) showed an intrapericardial free-echo formation in the lateral side of left cavities. This formation was very large and measured 69 mm × 48 mm and widely communicated with the left atrium via an 18-mm neck. This cavity seemed like a “third ventricle” and had a protodiastolic filling from the left atrium and tele-diastolic and systolic full drainage in the left atrium. There was no spontaneous contrast or thrombus. This finding corresponds to a giant LAA aneurysm. Interestingly, size of the cavities, left and right ventricular functions, cardiac valves, and pulmonary veins were normal. There was no septal defect nor pulmonary hypertension. Cardiac CT scan (Fig. 3) confirmed echocardiographic data and showed normal coronary arteries with no pericardial abnormality. Because of the symptomatic nature of the patient and aneurysm size, we indicated surgical treatment. The patient was referred to a cardiac surgeon who performed an LAA aneurysm excision under cardiopulmonary bypass. The postoperatory course was uneventful and we principally noted disappearance of hiccups. Histological examination confirmed that it is an LAA aneurysm.
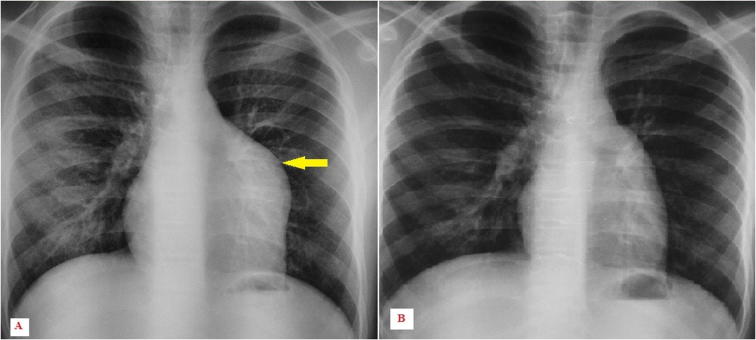
Figure 1.
(A) Left heart border bulging. (B) Postoperatory result.
Figure 2.
Left atrial appendage (LAA) aneurysm in (A) apical modified two-chamber, (B) short axis, (C) apical four-chamber, and (D) subcostal views. LA = left atrium; RA = right atrium; V = ventricle.
Figure 3.
Computed tomography scan. (A) Huge left atrial appendage (LAA) aneurysm widely communicating with the left atrium (LA). (B) Volume rendering technique reconstruction. Aort = aorta; RV = right ventricle.
Discussion
LAA aneurysm is an extremely rare cardiac anomaly with no more than hundred cases reported around the world [1]. Of the reported cases, only about two-fifth are congenital. The mean age of diagnosis is the third decade of life. Pediatric presentations, as in our patient, are more uncommon [2].
LAA aneurysm may be asymptomatic, detected incidentally during cardiac imaging [3]. Other revelation modes include palpitation, supraventricular arrhythmia, dyspnea, and thromboembolic events [2], [4], [5]. The symptoms appear habitually at the adult age with increasing aneurysm size. In this patient with original LAA aneurysm, persistent hiccups was the circumstance of discovery.
A chronic hiccup, defined by persistence of hiccups for more than 48 hours, is often associated with a serious underlying pathology. Cardiovascular etiologies of chronic hiccups include pericarditis, myocardial infarction, aortic dissection, and cardiac stimulator complication [6]. In our case, the large size of LAA aneurysm with compression/irritation of the left phrenic nerve can explain the occurrence of persistent hiccups. This was confirmed by the spectacular disappearance of hiccups after aneurysm excision.
Although echocardiography remains the standard method for the diagnosis of LAA aneurysms, sometimes it presents a real challenge. LAA aneurysm can be misdiagnosed by many cardiologists. Differential diagnosis may include left atrial diverticula, dilatation of the pulmonary artery [7], or a pericardial cyst [5].
In the case of our patient, we suppose that the pericardial effusion diagnosed 11 years before probably corresponded to the aneurysm. However, it may not have been large at that time, which is why the cardiologist mistook it as an effusion.
The LAA aneurysm must fulfill the following criteria: normal atrium, direct continuity with blood flow through the atrium itself, no pericardial defect, and histologically must present elements of normal atrial appendage [8]. Transesophageal echocardiography has a better sensitivity than transthoracic echocardiography (90% vs. 45%, respectively) [2]. Cardiac computed tomography and/or magnetic resonance imaging may be helpful for the diagnosis and detection of associated congenital anomalies. In fact, congenital LAA aneurysm can be isolated or associated with other congenital anomalies such as atrial septal defect, ventricular septal defect, anomalous renal artery, and Noonan syndrome [2]. Thromboembolic complication is frequent in LAA aneurysms. It is enhanced by atrial fibrillation. In our patient, despite the large size of the aneurysm, we were surprised by the absence of thrombi or at least spontaneous contrast in the left appendage. This finding is explained by sinus rhythm, the large aneurysm neck, and the very good aneurismal circulating flow leading to a full “washing” of the LAA aneurysm. Surgical assessment of LAA aneurysm is the recommended option even in asymptomatic patients. Surgery with cardiopulmonary bypass is safe. However, small aneurysms without thrombus can be excised or stapled using minimally invasive endoscopic techniques [9], [10].
In conclusion, huge LAA aneurysm is a rare but curable etiology of chronic hiccups.
Conflicts of interest
The authors have no conflicts of interest to declare.
Disclosure: Authors have nothing to disclose with regard to commercial support.
Footnotes
Peer review under responsibility of King Saud University.
References
- 1.Gan G.C., Bhat A., Desai H., Eshoo S. Giant left atrial appendage aneurysm. Heart Lung Circ. 2015;24:e81–e85. doi: 10.1016/j.hlc.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 2.Aryal M.R., Hakim F.A., Ghimire S., Ghimire S., Giri S., Pandit A. Left atrial appendage aneurysm: a systematic review of 82 cases. Echocardiography. 2014;31:1312–1318. doi: 10.1111/echo.12667. [DOI] [PubMed] [Google Scholar]
- 3.Tanoue Y., Kado H., Shiokawa Y., Sagaw K. Left atrial appendage aneurysm in a child. Ann Thorac Surg. 2004;77:721–723. doi: 10.1016/S0003-4975(03)01160-3. [DOI] [PubMed] [Google Scholar]
- 4.Chockalingam A., Alagesan R., Nandakumar M., Gnanavelu G. Massive left atrial appendage aneurysm presenting as supraventricular tachycardia. Indian Heart J. 2003;55:379–381. [PubMed] [Google Scholar]
- 5.Kuiten W.M., de Heer L.M., van Aarnhem E.E., Onsea K., van Herwerden L.A. Giant left atrial appendage: a rare anomaly. Ann Thorac Surg. 2013;96:1478–1480. doi: 10.1016/j.athoracsur.2013.01.038. [DOI] [PubMed] [Google Scholar]
- 6.Kolodzik P.W., Eilers M.A. Hiccups (singultus): review and approach to management. Ann Emerg Med. 1991;20:565–573. doi: 10.1016/s0196-0644(05)81620-8. [DOI] [PubMed] [Google Scholar]
- 7.Pome G., Pelenghi S., Grassi M., Vignati G., Pellegrini A. Congenital intrapericardial aneurysm of the left atrial appendage. Ann Thorac Surg. 2000;69:1569–1571. doi: 10.1016/s0003-4975(00)01175-9. [DOI] [PubMed] [Google Scholar]
- 8.Gold J.P., Afifi H.Y., Ko W., Horner H., Hahn R. Congenital giant aneurysm of the left atrial appendage: diagnosis and management. J Cardiac Surg. 1996;11:147–150. doi: 10.1111/j.1540-8191.1996.tb00030.x. [DOI] [PubMed] [Google Scholar]
- 9.Kiaii B., Doll N., Kuehl M., Mohr F.W. Minimal invasive endoscopic resection of a giant left atrial appendage aneurysm. Ann Thorac Surg. 2004;77:1437–1438. doi: 10.1016/S0003-4975(03)01303-1. [DOI] [PubMed] [Google Scholar]
- 10.Burke R.P., Mark J.B., Collins J.J., Jr., Cohn L.H. Improved surgical approach to left atrial appendage aneurysm. J Card Surg. 1992;7:104–107. doi: 10.1111/j.1540-8191.1992.tb00786.x. [DOI] [PubMed] [Google Scholar]