Abstract
Background
Limited data exist on the epidemiology of cardiovascular risk factors in Saudi Arabia, particularly in relation to the differences between Saudi nationals and expatriates in Saudi Arabia. The aim of this analysis was to describe the current prevalence of cardiovascular risk factors among patients attending general practice clinics across Saudi Arabia.
Methods
In this cross-sectional epidemiological analysis of the Africa Middle East Cardiovascular Epidemiological (ACE) study, the prevalence of cardiovascular risk factors (hypertension, diabetes, dyslipidemia, obesity, smoking, abdominal obesity) was evaluated in adults attending primary care clinics in Saudi Arabia. Group comparisons were made between patients of Saudi ethnicity (SA nationals) and patients who were not of Saudi ethnicity (expatriates).
Results
A total of 550 participants were enrolled from different clinics across Saudi Arabia [aged (mean ± standard deviation) 43 ± 11 years; 71% male]. Nearly half of the study cohort (49.8%) had more than three cardiovascular risk factors. Dyslipidemia was the most prevalent risk factor (68.6%). The prevalence of hypertension (47.5%) and dyslipidemia (75.5%) was higher among expatriates when compared with SA nationals (31.4% vs. 55.1%, p = 0.0003 vs. p < 0.0001, respectively). Conversely, obesity (52.6% vs. 41.0%; p = 0.008) and abdominal obesity (65.5% vs. 52.2%; p = 0.0028) were higher among SA nationals vs. expatriates.
Conclusion
Modifiable cardiovascular risk factors are highly prevalent in SA nationals and expatriates. Programmed community-based screening is needed for all cardiovascular risk factors in Saudi Arabia. Improving primary care services to focus on risk factor control may ultimately decrease the incidence of coronary artery disease and improve overall quality of life.
The ACE trial is registered under NCT01243138.
Keywords: ACE study, Cardiovascular risk factors, Expatriates, Saudi Arabia
Abbreviations
- ACC
American College of Cardiology
- ACE
study Africa Middle East Cardiovascular Epidemiological Study
- AHA
American Heart Association
- BMI
body mass index
- BP
blood pressure
- CADISS
Coronary Artery Disease in Saudis study
- ESC
European Society of Cardiology
- HDL
high-density lipoprotein
- LDL
low-density lipoprotein
- NCEP
National Cholesterol Education Program
- SA
ethnic Saudi population
Introduction
Coronary artery disease is the leading cause of morbidity and mortality worldwide, especially in developing countries [1], [2], [3]. Conventional risk factors for atherosclerotic heart disease have been highlighted as potential modifiable targets for lowering cardiovascular disease risk [4], [5], [6]. However, many studies have focused on patients in developed countries, such as the United States [7], [8], [9]. Therefore, systemic epidemiological data on the prevalence of cardiovascular risk factors in developing countries is somewhat lacking [10], [11], [12].
Saudi Arabia has undergone a major economic transition and experienced significant urbanization in recent years [3], [13], and the proportion of individuals living in urban centers has doubled in the past decade [14], [15], [16]. This rapid urbanization has been associated with a rise in the burden of cardiovascular diseases; however, the national preventive health system and screening programs have trailed behind [17], [18], [19]. In particular, screening procedures targeted towards adults at risk of developing cardiovascular disease are very limited. In addition, data on the differences in the prevalence of cardiovascular risk factors between local citizens and expatriates are lacking. Thus, the aim of this analysis was to describe the current prevalence of cardiovascular risk factors among patients enrolled in the Africa Middle East Cardiovascular Epidemiological (ACE) study attending general practice clinics in Saudi Arabia. We also compared the prevalence of risk factors in the ethnic Saudi population (SA nationals) and expatriates.
Methods
ACE study design and objectives
The methods and primary results of the ACE study have been published previously [20]. In summary, the ACE study was a cross-sectional epidemiological study conducted in 98 clinics across 14 countries in the Africa and Middle East region between July 2011 and April 2012. In particular, the study was aimed at countries in the Africa and Middle East region where there was a paucity of systematic epidemiological data. Site selection was based upon the ability of a site to conduct clinical studies based on the availability of clinical research expertise, infrastructure, and ethical oversight. The primary objective of the ACE study was to estimate the prevalence of cardiovascular risk factors in outpatients attending general practice and other nonspecialist clinics in urban and rural communities [20]. All epidemiological data were saved and used under ethical approval. The ACE study was registered on clinicaltrials.gov (registration number NCT01243138).
Participant selection
Outpatients aged >18 years were enrolled; all patients provided written, informed consent. Pregnant women, lactating mothers, and outpatients with life-threatening conditions were excluded. In order to avoid selection bias, the study population was selected by a sampling technique based on enrolment of every fifth eligible outpatient seen by a physician or general practitioner on a particular day. The primary investigators of the study evaluated outpatients through history taking, physical examination, and laboratory investigations. Evaluations were typically undertaken over one clinic visit; however, for nonfasting outpatients during the first visit, a second visit was arranged to obtain fasting blood samples.
ACE Saudi Arabia
In Saudi Arabia, a total of 550 patients were enrolled, constituting about 13% of the entire ACE study cohort. This analysis was conducted in multiple clinics in urban and rural regions of the kingdom. In this post hoc analysis, patients were divided into two groups: SA nationals and expatriates.
Cardiovascular risk factor definitions
Dyslipidemia was recorded if patients were on treatment with a lipid-lowering drug or if a current fasting lipid profile measurement documented one or more of the following: high total cholesterol (≥240 mg/dL); high low-density lipoprotein (LDL)-cholesterol (based on associated risk factors: LDL-cholesterol ≥100–160 mg/dL); low high-density lipoprotein (HDL)-cholesterol (<40 mg/dL in males; <50 mg/dL in females); or high triglyceride level (≥200 mg/dL), according to the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) guidelines [21]. Outpatients on lipid-regulating treatments were considered to have controlled LDL-cholesterol if their values were at goal according to their risk category, based on the NCEP ATP III recommended LDL-cholesterol targets [7]. Lipids were also assessed according to American College of Cardiology (ACC)/American Heart Association (AHA) 2013 guidelines.
Arterial blood pressure (BP) was recorded as the higher of two consecutive measurements, taken once from each arm with a standardized automated BP measuring instrument after the outpatients had been sitting quietly for at least five minutes. Hypertension was defined as being on current antihypertensive drugs, or having an abnormal BP reading (BP ≥140/90 mmHg, and for diabetic patients ≥130/80 mmHg), according to the European Society of Cardiology (ESC) Cardiovascular Prevention Guidelines [22]. Outpatients on antihypertensive drugs were considered to have controlled BP if they had values below the targets set by the ESC guidelines [22].
The following modifiable cardiovascular risk factors were also recorded: diabetes mellitus [fasting blood glucose ≥126 mg/dL (7 mmol/L)], defined as per the American Diabetes Association criteria [23]; smoking, defined as current or past consumption of cigarettes, pipe, or water pipe (shisha); obesity, defined as body mass index (BMI) ≥30 kg/m2; and abdominal obesity, defined in-line with the International Diabetes Federation harmonized criteria as a waist circumference ≥94 cm in males and ≥80 cm in females [24]. Metabolic syndrome was defined as presence of three or more abnormal findings out of the following five: large waist circumference, elevated triglycerides, elevated BP, elevated fasting glucose, and reduced HDL [7].
Statistical methods
Categorical data are summarized using frequencies and percentages. Continuous data are reported as mean ± standard deviation or median (25th, 75th percentiles). Dichotomous data comparing the SA nationals versus expatriate subgroups were evaluated with a Chi-square test, a Fisher exact test was used to compare categorical data with small cells, and continuous variables were evaluated with an unpaired two-tailed student t test. The test was considered statistically significant if p ≤ 0.05. As this was an exploratory analysis, No multiplicity correction was applied.
Results
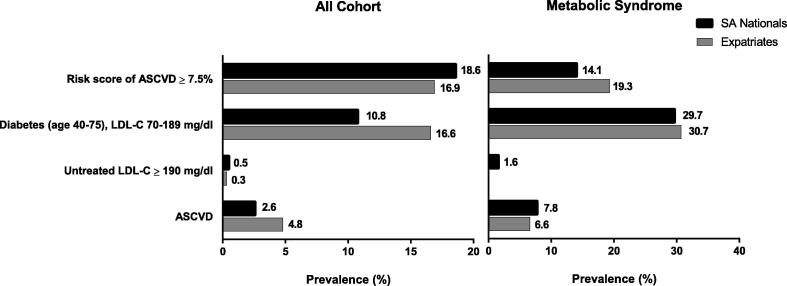
The ACE study enrolled 550 participant from different clinics across Saudi Arabia (35.3% SA nationals; 64.7% expatriates). Distribution of expatriates by nationality is given in Table S1. The mean age of the overall cohort was 43 ± 11 years and just over half (55%) were younger than 45 years. Among outpatients, nearly three-quarters of the study cohort (72.4%) were male (Table 1). Nearly 50% of all participants had three or more modifiable cardiovascular risk factors (Fig. 1) [either hypertension, diabetes, dyslipidemia, smoking, obesity (BMI ≥30 kg/m2), or abdominal obesity]. Only 15.6% of the total population had one cardiovascular risk factor; 24.0% had two risk factors; 16.9% had three risk factors; 17.6% had four risk factors; 11.3% had five risk factors; and 4.0% had all six risk factors.
Table 1.
Baseline characteristics of the study cohort.
| Total cohort (n = 550) |
SA nationals (n = 194) |
Expatriates (n = 356) |
p | |
|---|---|---|---|---|
| Male | 391 (72.4%) | 116 (61.1%) | 275 (78.6%) | < 0.001 |
| Age (y) | 43.2 (±10.5) | 40.8 (±11) | 44.5 (±10.0) | < 0.001 |
| Age groups | ||||
| 18–44 y | 301 (54.7%) | 117 (60.3%) | 184 (51.7%) | 0.143 |
| 45–64 y | 241 (43.8%) | 75 (38.7%) | 166 (46.6%) | |
| ≥65 y | 8 (1.5%) | 2 (1.0%) | 6 (1.7%) | |
| Body mass index (kg/m2) | 29.7 (±5.1) | 30.5 (±5.7) | 29.3 (±4.7) | 0.008 |
Data are presented as frequency (%) or mean (±SD) as appropriate.
Figure 1.
Prevalence of cardiovascular risk factors per patient.
Dyslipidemia was the most prevalent cardiovascular risk factor recorded in seven out of every 10 outpatients (68.6%) (Table 2). Median (25th, 75th percentile) lipid values in the overall cohort were 182 (160, 203) mg/dL, 104 (89, 123.5) mg/dL, 46 (39, 52) mg/dL, and 151 (114, 179) mg/dL for total cholesterol, LDL-cholesterol, HDL-cholesterol, and triglycerides, respectively (Table 3). Hypertension was recorded in 41.8% of outpatients and median (25th, 75th percentiles) systolic/diastolic values were 130 (120, 144)/80 (75, 90) mmHg, respectively. One quarter of outpatients had diabetes. The median (25th, 75th percentile) fasting plasma glucose was 5.5 (5.1, 6.2) mmol/L. The prevalence of obesity was 45.1% and median (25th, 75th percentile) waist circumference was 93 (87.3, 103) cm.
Table 2.
Modifiable cardiovascular risk factors: prevalence and distribution.
| Risk factor | Total cohort (n = 550) |
SA nationals (n = 194) |
95% confidence interval | Expatriates (n = 356) |
95% confidence interval | p-value |
|---|---|---|---|---|---|---|
| Hypertension | [550] 230 (41.8%) | [194] 61 (31.4%) | 25.0–38.5 | [356] 169 (47.5%) | 42.2–52.8 | <0.001 |
| Diabetes mellitus | [528] 137 (25.9%) | [178] 42 (23.6%) | 17.6–30.5 | [350] 95 (27.1%) | 22.6–32.1 | 0.192 |
| Dyslipidemia | [529] 363 (68.6%) | [178] 98 (55.1%) | 47.4–62.5 | [351] 265 (75.5%) | 70.7–79.9 | <0.001 |
| Obesity (BMI ≥ 30) | [550] 248 (45.1%) | [194] 102 (52.6%) | 45.3–59.8 | [356] 146 (41.0%) | 35.9–46.3 | 0.009 |
| Abdominal obesity | [550] 313 (56.9%) | [194] 127 (65.5%) | 58.3–72.1 | [356] 186 (52.2%) | 46.9–57.5 | 0.003 |
| Smoking | [550] 110 (20.0%) | [194] 42 (21.6%) | 16.1–28.1 | [356] 68 (19.1%) | 15.2–23.6 | 0.165 |
Data are presented as frequency (%). Data in square brackets are number of individuals with nonmissing data.
BMI = body mass index (in kg/m2).
Table 3.
Measurable parameters assessment (lipid values, glucose level, blood pressure, and abdominal circumference).
| Risk factor | Total cohort (n = 550) | SA nationals (n = 194) | Expatriates (n = 356) | p-value |
|---|---|---|---|---|
| Total cholesterol (mg/dL) | [529] 182 (160, 203) | [178] 182 (165, 206) | [351] 181 (157, 202) | 0.466 |
| Total cholesterol ≥240 mg/dL | 36 (6.8%) | 9 (5.1%) | 27 (7.7%) | 0.210a |
| LDL-cholesterol (mg/dL) | [528] 104 (89, 123.5) | [178] 104 (92, 118) | [350] 104 (87.4, 128) | 0.386 |
| LDL ≥ 100 mg/dL | 70 (13.3%) | 14 (7.9%) | 56 (16.0%) | 0.155a |
| HDL-cholesterol (mg/dL) | [527] 46 (39, 52) | [178] 49.9 (43, 54) | [349] 43 (37, 51) | < 0.001 |
| HDL < 40 (mg/dL) | 144 (27.3%) | 27 (15.2%) | 117 (33.5%) | < 0.001 |
| Triglycerides (mg/dL) | [529] 151 (114, 179) | [178] 155.5 (125, 190) | [351] 148 (110, 175) | 0.050 |
| Triglycerides ≥200 (mg/dL) | 71 (13.4%) | 30 (16.9%) | 41 (11.7%) | 0.187 |
| Fasting plasma glucose (mmol/L) | [528] 5.5 (5.1, 6) | [178] 5.5 (5, 6) | [350] 5.6 (5.1, 6.2) | 0.538 |
| Systolic blood pressure (mmHg) | [550] 130 (120, 144) | [194] 135 (122, 149) | [356] 130 (120, 144) | 0.136 |
| Diastolic blood pressure (mmHg) | [550] 80 (75, 90) | [194] 87 (78, 95) | [365] 82 (75, 91) | 0.007 |
| Waist circumference (cm) | [550] 93 (87.3, 103) | [194] 95 (85, 105) | [365] 92 (88, 101) | 0.354 |
Data are presented as frequency (%) or median (25th, 75th) as appropriate. Data in square brackets are number individuals with nonmissing data.
HDL = high-density lipoprotein; LDL = low-density lipoprotein.
Fisher Exact Test.
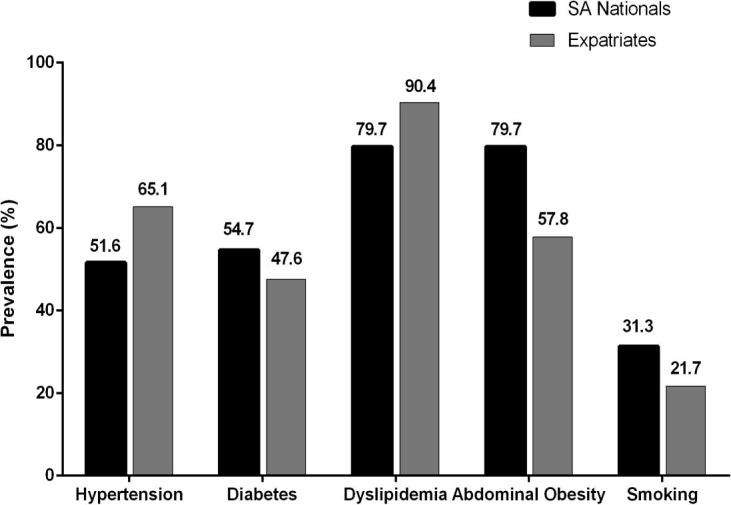
Saudi national subgroup analysis
SA nationals were younger and had a higher BMI compared with expatriates. The majority of patients were male in both cohorts (Table 1). The prevalence of hypertension and dyslipidemia was higher among expatriates compared with SA nationals with 47.5% [95% confidence interval (CI), 42.2–52.8] versus 31.4% (95% CI, 25.0–38.5), and 75.5% (95% CI, 70.7–79.9) versus 55.1% (95% CI, 47.4–62.5), respectively. The prevalence of obesity (BMI >30 kg/m2) and abdominal obesity were, however, higher among SA nationals, with 52.6% versus 41.0% in expatriates and 65.5% versus 52.2%, respectively (Table 2). The prevalence of diabetes and smoking were not significantly different between cohorts, with difference in prevalence of approximately 4% and 2% between SA nationals and expatriates, respectively (Table 2). Further gender- and age-specific were compared among both SA nationals and expatriates (Table S2).
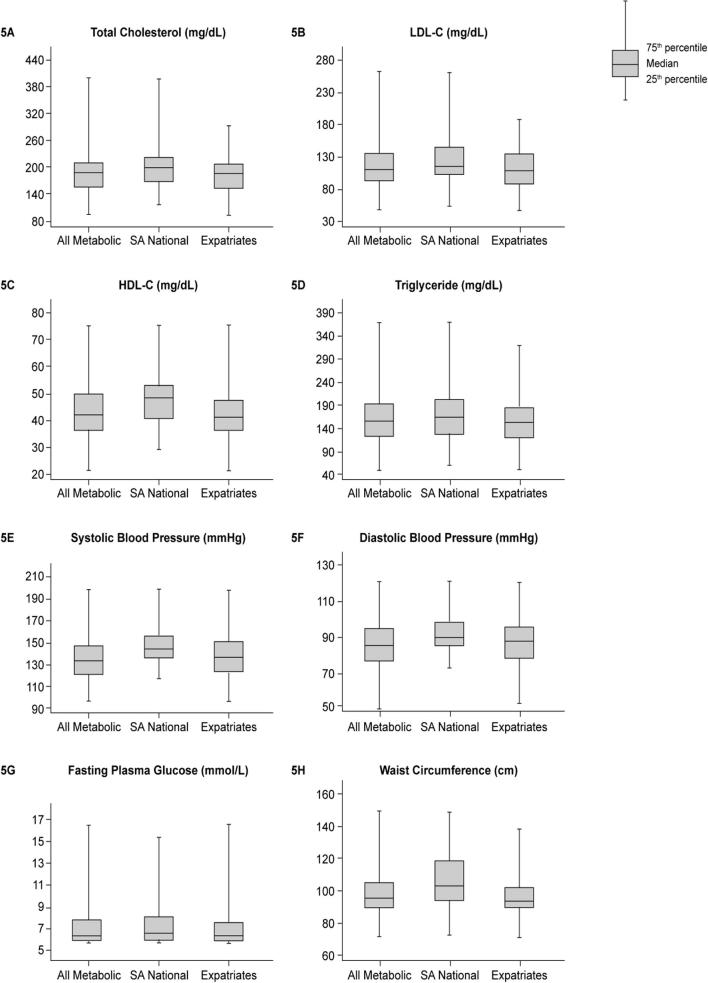
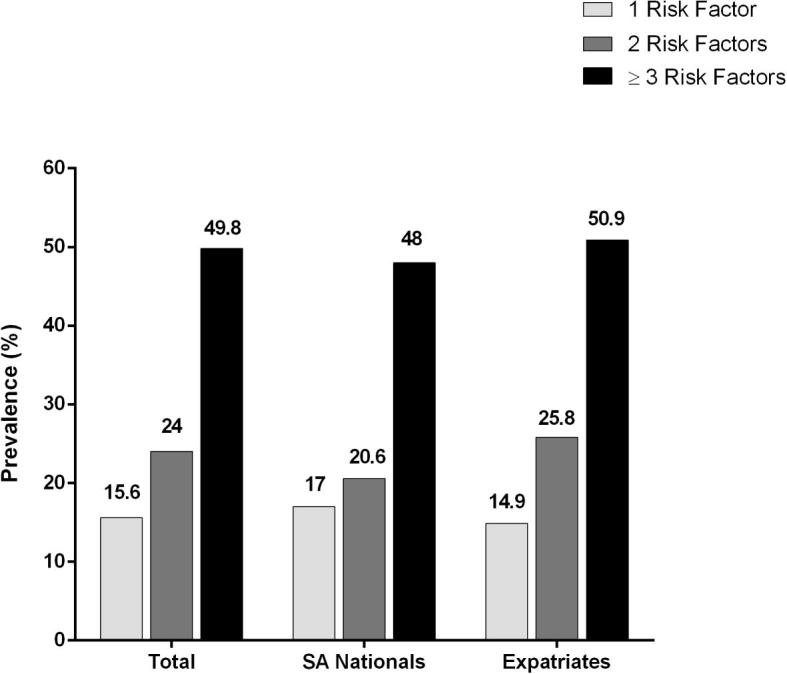
Differences were noted in prevalence of abnormal lipid profiles between SA nationals and expatriates and, in general, expatriates showed a higher prevalence of abnormal lipid profiles (Table 3). Based on 2013 ACC/AHA guidelines for initiation of lipid-lowering therapy [25], expatriates were eligible for initiation of statin therapy to nearly the same extent as SA nationals (Fig. 2). The prevalence of newly diagnosed hypertension and diabetes mellitus, highlighted during screening, was similar in the two cohorts of outpatients, but prevalence of newly diagnosed dyslipidemia (based on NCEP ATP III criteria) varied (Fig. 3).
Figure 2.
Eligibility of lipid-lowering medication according to the ACC/AHA guidelines. ASCVD = atherosclerotic cardiovascular disease; LDL-C = low-density lipiprotrein cholesterol.
Figure 3.
Prevalence of newly diagnosed hypertension, diabetes mellitus, and dyslipidemia.
Metabolic syndrome
The prevalence of metabolic syndrome in the outpatient cohort was 41.8%; 72.2% of these outpatients were expatriates. Among patients with a diagnosis of metabolic syndrome, dyslipidemia was the most common component (87.4%), followed by abdominal obesity (63.9%), hypertension (61.3%), diabetes mellitus (49.6%), and smoking (24.3%). Fig. 4 shows the distribution of these risk factors between SA nationals and expatriates.
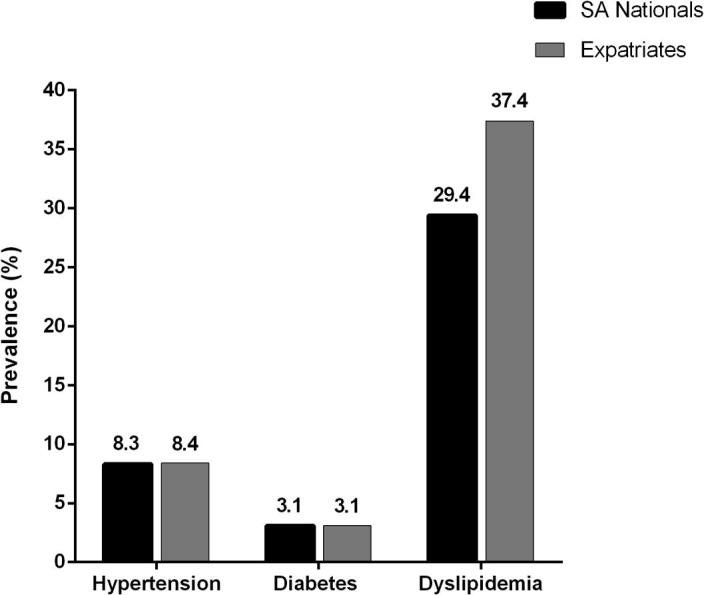
Figure 4.
Prevalence of cardiovascular risk factors in patients with metabolic syndrome. All metabolic (n = 230); SA nationals (n = 64); expatriates (n = 166).
The medians (25th, 75th percentile) of measurable parameters of metabolic syndrome are shown in Fig. 5. Median lipid values, BP, and waist circumference were lower among expatriates compared with SA nationals. Initiation of lipid-lowering therapy for patients not previously on lipid-lowering therapy (according to 2013 ACC/AHA guidelines [25]) was more frequent for outpatients with metabolic syndrome in the SA national compared with the expatriates group. Additionally, subgroup analysis for certain laboratory tests is shown in Table S3.
Figure 5.
Box plot of lipid profile, blood pressure, fasting plasma glucose, and waist circumference measures across patients with metabolic syndrome. HDL-C = high-density lipoprotein cholesterol; LDL-C = low-density lipoprotein cholesterol; SA = Saudi Arabia.
Discussion
Cardiovascular diseases represent a major health challenge for the contemporary Saudi population. The ACE Saudi Arabia study sheds light on the current status of risk factor management in Saudi Arabia among outpatients attending general practice clinics in this region. This analysis clearly demonstrates that there has been a significant increase in cardiovascular risk factor prevalence. In addition, a significant proportion of patients with modifiable risk factors have poor overall control, based on recommendations from international guidelines.
The urban population of Saudi Arabia has notably increased during the previous decade, with numbers expected to double in the next few years as a result of lifestyle changes and improved standards of healthcare [13]. This shift towards an increase in urban Saudi population, with an accompanying increase in the numbers of expatriates, will have profound implications for healthcare services, healthcare access, and resource utilization, as well as public health. Our analysis demonstrates that with the current risk factors, more resources are needed for risk factor detection and control to avoid an epidemic in atherosclerotic cardiovascular diseases.
In our study, dyslipidemia and abdominal obesity were the most prevalent risk factors, affecting approximately three-quarters of screened outpatients, followed by high rates of hypertension, diabetes, and smoking. These findings were observed in both genders and across different age groups. In addition, approximately half of the participants did not use appropriate management, and half of the outpatients who were on therapy for dyslipidemia still had poor lipid profile control. This is despite lipid-modifying medications being available without cost. Thus, future studies are needed to address the true barriers to risk factor control in a society where healthcare and medications are free of charge, making them largely accessible.
Al-Nozha et al. [17] estimated the prevalence of diabetes in the community-based Coronary Artery Disease in Saudis Study (CADISS). More than a decade later, the present study demonstrates that there has been little change in the prevalence of diabetes in the Saudi population. Similar observations were noted regarding diabetes control. Thus, there is an urgent need for a national prevention program that targets high-risk groups in an attempt to achieve better risk factor and diabetes control. In contrast, there has been a significant increase in the rate of hypertension, from 26.1% in the CADISS study [17], [26] to more than 40% in the present study. In addition, hypertension control is suboptimal in all outpatients. Thus, public health programs are needed to reduce salt intake and improve physical fitness, measures that have been shown to reduce hypertension incidence and improve BP control.
Several studies [18], [27], [28] have reported that patients with traditional cardiovascular risk factors have poor risk factor control. Numerous potential reasons could explain this, including limited assessment by healthcare workers, accessibility of healthcare facilities, and level of compliance. Furthermore, limited knowledge of some primary care physicians about cardiovascular risk factor management, advanced therapies, and new tools to help achieve better risk factor management may contribute to suboptimal risk factor management.
Public health approaches can be adopted by a number of organizations and associations and may play an important role in reducing the incidence of modifiable traditional cardiovascular risk factors. Variable reduction rates in prevalence of these risk factors may significantly reduce health expenditure and as a consequence, develop and provide a well-structured primary course of prevention. For example, increase in tobacco-free environments, establishment of additional taxes on smokers, restricted roles of manufacturers of tobacco-based products, and support and rehabilitation programs to those willing to quit. Furthermore, promoting healthy diet and physical activity through community-based awareness initiatives, including social media interaction will further contribute to risk reduction. Increased consumption of important food classes accompanied by a reduced intake of harmful substitutes like saturated fatty acids and drinks with high calorie intake are measures that will prove beneficial. Furthermore, adoption and supplementation of National Guidelines on physical activity to support and encourage physical activity for all age groups will be key to improving overall health outcomes [29].
Our analysis is a subgroup of the main ACE study including only patients recruited from Saudi sites. Few points are addressed in this analysis that are unique and were not studied in the entire cohort. First, our analysis showed individualized detailed estimates of the prevalence of cardiovascular risk factors and metabolic syndrome precisely for the population of Saudi Arabia. Second, we compared the risk factors burden between expatriates and SA nationals, which was very important for resource allocation, especially in regards to healthcare transformation planning. Finally, our paper highlights the patients’ eligibility to lipid-lowering medications according to the recent 2013 ACC/AHA guidelines, which were not previously studied in a Saudi population.
Our study is not without limitations. The ACE Saudi Arabia substudy enrolled outpatients that were randomly selected from different clinics in Saudi Arabia. Multiple attempts were made to obtain a representative sample. However, it is still possible that there might be some selection bias limiting the generalizability of the study findings. Further national surveys for traditional atherosclerotic heart disease, including larger sample size and with a structured database and periodically monitoring assessment, are needed. Although our study presented the situation of patients attending healthcare, the distribution of cardiovascular risk factors among study cohorts cannot represent the general population and only population-based surveys. Additionally, the analysis was an exploratory one; thus, the p values published may not be indicative of statistical significance, rather limited to identifying variables for further exploration in a properly designed randomized clinical trial.
Conclusion
This analysis clearly shows that there is a high prevalence of cardiovascular risk factors in the Saudi population. In addition, a significant proportion of patients with risk factors have poor overall control. Programmed community-based screening is needed for all cardiovascular risk factors in Saudi Arabia. Increased awareness and improved primary care services may decrease the incidence of coronary artery disease and improve overall quality of life.
Acknowledgments
Assistance with the formatting of the manuscript to journal style and proof reading was provided by Vatsala Malik of Engage Scientific (Horsham, UK) and funded by Pfizer. The Africa Middle East Cardiovascular Epidemiological (ACE) Study was sponsored by Pfizer.
Disclosure: Authors have nothing to disclose with regard to commercial support.
Footnotes
Peer review under responsibility of King Saud University.
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jsha.2017.03.004.
Appendix A. Supplementary data
References
- 1.Bonow R.O., Smaha L.A., Smith S.C., Jr, Mensah G.A., Lenfant C. World Heart Day 2002: the international burden of cardiovascular disease: responding to the emerging global epidemic. Circulation. 2002;106:1602–1605. doi: 10.1161/01.cir.0000035036.22612.2b. [DOI] [PubMed] [Google Scholar]
- 2.Levenson J.W., Skerrett P.J., Gaziano J.M. Reducing the global burden of cardiovascular disease: the role of risk factors. Prev Cardiol. 2002;5:188–199. doi: 10.1111/j.1520-037x.2002.00564.x. [DOI] [PubMed] [Google Scholar]
- 3.Yusuf S., Reddy S., Ounpuu S., Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104:2746–2753. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 4.Aldana S.G., Whitmer W.R., Greenlaw R., Avins A.L., Salberg A., Barnhurst M. Cardiovascular risk reductions associated with aggressive lifestyle modification and cardiac rehabilitation. Heart Lung. 2003;32:374–382. doi: 10.1016/s0147-9563(03)00106-7. [DOI] [PubMed] [Google Scholar]
- 5.Howard B.V., Van Horn L., Hsia J., Manson J.E., Stefanick M.L., Wassertheil-Smoller S. Low-fat dietary pattern and risk of cardiovascular disease: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:655–666. doi: 10.1001/jama.295.6.655. [DOI] [PubMed] [Google Scholar]
- 6.Joyner M.J., Green D.J. Exercise protects the cardiovascular system: effects beyond traditional risk factors. J Physiol. 2009;587:5551–5558. doi: 10.1113/jphysiol.2009.179432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alberti K.G., Eckel R.H., Grundy S.M., Zimmet P.Z., Cleeman J.I., Donato K.A. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 8.Anderson K.M., Odell P.M., Wilson P.W., Kannel W.B. Cardiovascular disease risk profiles. Am Heart J. 1991;121(1 Pt 2):293–298. doi: 10.1016/0002-8703(91)90861-b. [DOI] [PubMed] [Google Scholar]
- 9.Fox C.S., Coady S., Sorlie P.D., D'Agostino R.B., Sr, Pencina M.J., Vasan R.S. Increasing cardiovascular disease burden due to diabetes mellitus: the Framingham Heart Study. Circulation. 2007;115:1544–1550. doi: 10.1161/CIRCULATIONAHA.106.658948. [DOI] [PubMed] [Google Scholar]
- 10.Abegunde D.O., Mathers C.D., Adam T., Ortegon M., Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370:1929–1938. doi: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 11.Gaziano T.A. Cardiovascular disease in the developing world and its cost-effective management. Circulation. 2005;112:3547–3553. doi: 10.1161/CIRCULATIONAHA.105.591792. [DOI] [PubMed] [Google Scholar]
- 12.Gaziano T.A., Galea G., Reddy K.S. Scaling up interventions for chronic disease prevention: the evidence. Lancet. 2007;370:1939–1946. doi: 10.1016/S0140-6736(07)61697-3. [DOI] [PubMed] [Google Scholar]
- 13.Chadha S.L. Urban-rural differences in prevalence of coronary disease and its risk factors. Curr Sci. 1998;74:1069–1073. [PMC free article] [PubMed] [Google Scholar]
- 14.al-Nuaim AA, Bamgboye EA, al-Rubeaan KA, al-Mazrou Y. Overweight and obesity in Saudi Arabian adult population, role of socio-demographic variables. J Community Health 1997;22:211–23. [DOI] [PubMed]
- 15.Arnlov J., Evans J.C., Meigs J.B., Wang T.J., Fox C.S., Levy D. Low-grade albuminuria and incidence of cardiovascular disease events in nonhypertensive and nondiabetic individuals: the Framingham Heart Study. Circulation. 2005;112:969–975. doi: 10.1161/CIRCULATIONAHA.105.538132. [DOI] [PubMed] [Google Scholar]
- 16.Chadha S.L., Gopinath N., Shekhawat S. Urban-rural differences in the prevalence of coronary heart disease and its risk factors in Delhi. Bull World Health Organ. 1997;75:31–38. [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Nozha M.M., Arafah M.R., Al-Mazrou Y.Y., Al-Maatouq M.A., Khan N.B., Khalil M.Z. Coronary artery disease in Saudi Arabia. Saudi Med J. 2004;25:1165–1171. [PubMed] [Google Scholar]
- 18.Danaei G., Finucane M.M., Lu Y., Singh G.M., Cowan M.J., Paciorek C.J. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 19.Hakim I.A., Alsaif M.A., Alduwaihy M., Al-Rubeaan K., Al-Nuaim A.R., Al-Attas O.S. Tea consumption and the prevalence of coronary heart disease in Saudi adults: results from a Saudi national study. Prev Med. 2003;36:64–70. doi: 10.1006/pmed.2002.1130. [DOI] [PubMed] [Google Scholar]
- 20.Alsheikh-Ali A.A., Omar M.I., Raal F.J., Rashed W., Hamoui O., Kane A. Cardiovascular risk factor burden in Africa and the Middle East: the Africa Middle East Cardiovascular Epidemiological (ACE) study. PLoS One. 2014;9:e102830. doi: 10.1371/journal.pone.0102830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Cholesterol Education Program Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 22.Graham I., Atar D., Borch-Johnsen K., Boysen G., Burell G., Cifkova R. European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts) Eur J Cardiovasc Prev Rehabil. 2007;14(Suppl 2):S1–S113. doi: 10.1097/01.hjr.0000277983.23934.c9. [DOI] [PubMed] [Google Scholar]
- 23.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome. 2006. Available at: https://www.idf.org/webdata/docs/MetS_def_update2006.pdf. Accessed Nov 19, 2014.
- 25.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63(25 Pt B):2889–934. [DOI] [PubMed]
- 26.Al-Nozha M.M., Abdullah M., Arafah M.K., Khalil M.Z., Khan N.B., Al-Mazrou Y.Y. Hypertension in Saudi Arabia. Saudi Med J. 2007;28:77–84. [PubMed] [Google Scholar]
- 27.Bovet P., Shamlaye C., Gabriel A., Riesen W., Paccaud F. Prevalence of cardiovascular risk factors in a middle-income country and estimated cost of a treatment strategy. BMC Public Health. 2006;6:9. doi: 10.1186/1471-2458-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reid R.J., Anderson M.L., Fishman P.A., McClure J.B., Johnson R.L., Catz S.L. Relationship between cardiovascular risk and lipid testing in one health care system: a retrospective cohort study. BMC Health Serv Res. 2015;15:281. doi: 10.1186/s12913-015-0884-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013–2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.