Abstract
Study Objective
We investigated if human reminder phone calls in the patient’s preferred language increase adherence with scheduled appointments in an inner-city chronic pain clinic. We hypothesized that language and cultural incongruence is the underlying mechanism to explain poor attendance at clinic appointments in underserved Hispanic populations.
Design
Pragmatic randomized controlled clinical trial
Setting
Innercity academic chronic pain clinic with a diverse, predominantly African-American and Hispanic population
Patients
All (n=963) adult patients with a scheduled first appointment between October 2014 and October 2015 at the Montefiore Pain Center in the Bronx, New York were enrolled.
Interventions
Patients were randomized to receive a human reminder call in their preferred language before their appointment, or no contact.
Measurements
We recorded patients’ demographic characteristics and as primary outcome attendance as scheduled, failure to attend and/or cancellation calls. We fit Bayesian and classical multinomial logistic regression models to test if the intervention improved adherence with scheduled appointments.
Main Results
Among the 953 predominantly African American and Hispanic/Latino patients, 475 patients were randomly selected to receive a language-congruent, human reminder call, while 478 were assigned to receive no prior contact, (after we excluded 10 patients, scheduled for repeat appointments). In the experimental group, 275 patients adhered to their scheduled appointment, while 84 cancelled and 116 failed to attend. In the control group, 249 patients adhered to their scheduled appointment, 31 cancelled and 198 failed to attend. Human phone reminders in the preferred language increased adherence (RR 1.89, CI95% [1.42, 1.42], (p<0.01). The intervention seemed particularly effective in Hispanic patients, supporting our hypothesis of cultural congruence as possible underlying mechanism.
Conclusions
Human reminder phone calls prior in the patient’s preferred language increased adherence with scheduled appointments. The intervention facilitated access to much needed care in an ethnically diverse, resource poor population, presumably by overcoming language barriers.
Keywords: adherence, clinic appointments, chronic pain, health care disparities, Hispanic/Latino, language barrier, access to care
Graphical Abstract
Culturally sensitive, language-congruent, patient-centered outreach can overcome barriers to access and engage minorities in an inner-city pain clinic. Above, the English-only-speaking provider fails to establish rapport and trust with his chronic pain patient. Below, culturally-sensitive, language-congruent staff engages the Latina patient in a warm patient-provider relationship already in the first telephone contact.

1 Introduction
Poor adherence with scheduled appointments (PASA) remains a particular concern in inner-city chronic pain clinics, with PASA rates up to 80%[1–3]. Not only is PASA a significant financial burden for the institution[4,5], it causes frustration for providers[6]. PASA is a waste of scarce resources, considering the already considerable wait times for chronic pain consultations [7]. Without the benefit of a cancellation call, PASA deprives other patients of the opportunity to schedule an appointment[8]. On the other hand, PASA may indicate barriers to healthcare[9], depriving our most vulnerable patients of needed specialized pain services[1,10,11]. The reasons for missed appointments often without a cancelation call, have long been studied[12], but remain elusive[13]. We identified language as a barrier to access of chronic pain services, specifically to adherence with scheduled appointments[1]. We hypothesized that patient concerns about cultural incongruence may be ameliorated by human outreach in the patient’s preferred language[1,7]. Based on retrospective cohort studies, we demonstrated that targeted health system improvements can improve access[2].
First generation Hispanic immigrants, i.e. those born outside the United States, may be especially vulnerable to discouraging experiences already during the pre-encounter process [7]. Actual or perceived discrimination in the pain clinic [14–17], for example concerns about opioid addiction or dependence triggered by minority status[18,19], can estrange patients[20] from their physicians and providers in addition to cultural and language barriers [2] and concerns about healthcare insurance coverage.
Disparities can arise in clinical encounters, if providers treat patients differently or if patients respond to (perceived) disparate treatment (demand side) [21], in our case patients may not adhere to scheduled appointments, if they feel not welcome or fear discrimination. With limited evidence available on how to influence the demand side of health care disparity in pain medicine[7,14,22], we postulated that native language personnel and unified clinics (seeing all patients in the same outpatient location with equitable access) helps to overcome such barriers, but that individualized outreach to patients by phone[13], in a language the patient understands, prior to scheduled appointments would establish a human rapport[23] before the actual encounter and improve adherence[1,2]. While PASA certainly imparts considerable costs to the institution[24], counter measures also consume resources and need to be justified to be financially sustainable considering the current pressures to cut cost[25].
We seek to investigate in sequential pragmatic clinical trials (PCT), which of the several language-targeted adjustments (Spanish certified staff, reminder calls in the preferred language, unified scheduling and clinic system for insured and uninsured, financial incentives to cover transport expenses…) to the appointment process [1,2] is most effective. In this first RCT, we investigate if a human reminder phone call, the day before their first appointment, in the patient’s preferred language (Spanish versus English), improves attendance in our inner-city academic chronic pain clinic in the Bronx, NY, serving a resource poor, racially and ethnically diverse, predominantly Hispanic population. As a secondary exploratory data analysis (also predefined before our pragmatic trial was begun), we hypothesized that calling the patients before the appointment in their preferred language is more effective in Spanish speaking patients than in English speaking patients.
1.1 Objectives
This is a pragmatic clinical trial to investigate if a language centered intervention (a human reminder phone call, the day before their first appointment, in the patient’s preferred language)
increases attendance at scheduled appointment in an inner-city academic pain clinic,
is more effective in Spanish speaking patients than in English speaking patients,
in patients scheduled for a first appointment in an inner-city chronic pain clinic.
2 Methods
2.1 Regulatory Review
In conducting this pragmatic trial to address healthcare disparities in pain medicine, we adhered to the research ethics principles of the Learning Health Care System Ethics Framework[26,27]. Our health systems investigation involved minimal risk for patients. Before the trial, chance (day of the week, staff available…) determined if patients received a reminder call before their appointment and in what language. The Albert Einstein College of Medicine Institutional Review Board approved the study and waived the requirement for informed consent. Our trial is registered with clinicaltrial.gov [ClinicalTrials.gov Identifier: NCT03101969].
2.2 Trial Population and Setting
All adult patients (age older or equal to 18 years) with a scheduled first appointment at the adult outpatient Pain Center at Montefiore Medical Center located in the Bronx, New York from October 2014 through October 2015 were included, regardless of race, ethnicity, and insurance status or if they attended, failed to attend, or cancelled the appointment. No patients were excluded except if they had had a previous appointment in our clinic. We limited our analysis to initial (first) scheduled appointments in the hope that by doing so we would single out the effect of our telephone outreach on establishing an early rapport with the patient, prior to the confounding influence of the first provider encounter.
2.3 Power Analysis and Patient Flow
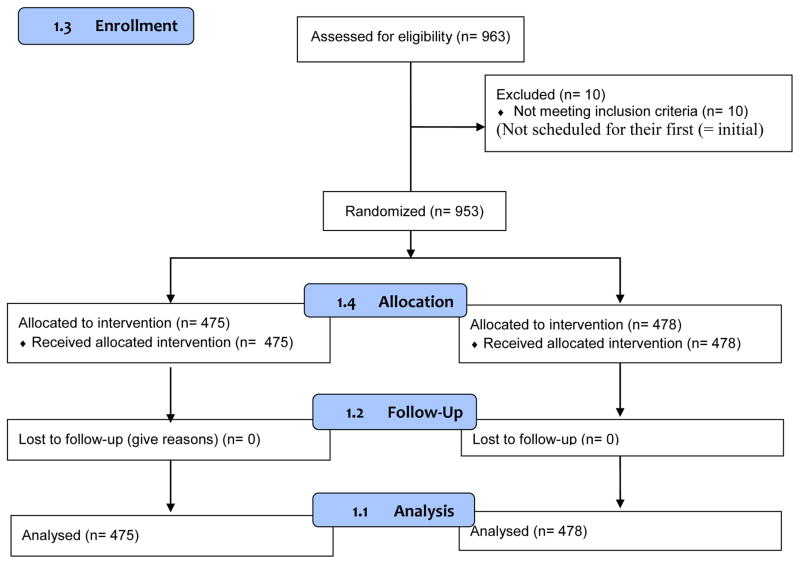
We planned for an enrollment of 1000 patients. In our power analysis, we estimated that if the proportion of failure to attend in the intervention group were 30% compared to a proportion of 50% in the control group, we would need 172 patients for a power of 90% and a confidence level of 99%. We present the patient recruitment and retention in a CONSORT flow chart (Figure 1: CONSORT Flow Chart). To increase the ecological validity of our study we engaged representatives of the participant predominantly Spanish population in the formulation of our a priori hypothesis and the study design and data collection [28], offered them co-authorship and when they declined, acknowledge their contribution in the acknowledgement, if they agreed.
Figure 1.
The CONSORT Flow Chart demonstrates the near 100% retention and complete data for our primary outcome, and also illustrates the origin of the data for the various tables.
2.4 Intervention
All patients scheduled for a first appointment were randomized to receive a human pre-appointment reminder phone call, the day before their scheduled appointment, in the patient’s preferred language, (or no prior contact). This phone call was administered either in English, for patients who self-identified as English speakers or non-English non-Spanish speakers; or in Spanish, for patients or respondents who interactively self-identified as Spanish speakers in the phone conversation. Front desk staff who administered the Spanish speaking phone calls was either a native Spanish speaker or has received credentials certifying their ability to communicate in Spanish. The initial appointment was scheduled in English or Spanish dependent on the staff receiving the call and the preferences of the person requesting the appointment; no consent was sought and randomization (to receive a reminder call or not) was not discussed with the person scheduling the initial appointment.
2.5 Randomization, Blinding and Allocation Concealment
Randomization was by computer generated tables. Neither the clinic personnel nor the providers (nurses or physicians) knew which intervention took place, (except if the patient revealed this spontaneously). Group allocation was concealed in opaque sealed envelopes, which were opened just prior to the phone call (to ensure allocation concealment.) Calls were made at random times, mostly in the afternoon. Only one attempt was made to call.
2.6 Primary Outcome
We termed our primary outcome adherence, (defined as attendance at a first scheduled appointment as recorded in the clinic records). Using the term adherence, (without prejudice on those patients who had the courtesy to cancel), we emphasized that attendance indicated that the patient was able to fulfill his or her need to see a pain specialist, while even with a cancellation, PASA implied that the need was possibly still unmet.
2.7 Data Collection
The language preferred by the patient, (used as predictor language in our secondary multivariate multinomial regression analysis), was identified interactively during the call, in response to expressed or inferred preferences by the patient or proxy, or (for those patients randomized to no call or not reached) as the preferred language routinely entered into Montefiore Hospital billing software on the patient’s first encounter with the hospital.
The caller documented the intervention executed according to randomization as [no call, or call] in a secure computerized repository, where the intervention the patient received was masked until data analysis. The caller also recorded (for the intervention group only) if the patients or a proxy were [reached or not reached].
Outcome and demographics for our study subjects were recorded automatically by operators blinded to the intervention and pulled directly from the clinic’s administrative billing database and hospital electronic health records. Clinic personnel document patient attendance routinely as [arrived, cancelled, no show)] on the day of the scheduled appointment. Our analyses utilized de-identified data. The following self-identified (where appropriate) demographic data were collected for each patient at the time of initial appointment booking: appointment date; patient age; patient gender; ethnicity (asked as: “Do you self-identify as Hispanic?” with responses of yes or no); race (White, Black, Other Race, Declined) primary spoken language (English, Spanish, other languages).
2.8 Statistical Analysis
To investigate the effect of our intervention (call versus no call) on our primary categorical multinomial outcome (adherence with scheduled appointment versus cancellation call versus failure to attend), we fit a multinomial log-linear model. To investigated if the intervention, (a human reminder phone call, the day before their first appointment, in the patient’s preferred language), improved outcomes (adherence with a scheduled appointment) differentially more in Spanish speaking patients, we conducted two stratified analyses of the effect of the intervention on outcome. Given the importance of language and cultural competence for the provider-physician interaction of Spanish-speaking patients [7,29–31], showing differential effect would support the notion that the culturally sensitive human call in the preferred language is the important element of the intervention as opposed to a reminder, which could have been automated or in English.
The first contrasting the subsets of patients who identified as Hispanic/Latino versus not, and the second contrasting the patients who reported Spanish as their preferred language, versus not. To the same end, we also fit additional multivariate multinomial logistic regressions including (1) ethnicity (Hispanic/Latino) and (2) language (preferred by the patient) and their interaction with treatment. We planned an intention-to-treat analysis, but as we had no attrition, this was not pertinent in our analysis; We did not think an intention to treat analysis of only those patients reached personally when called, was pertinent, because we wanted to test the human outreach intervention under realistic circumstances in a pragmatic setting and feel that the intervention (a call in the preferred language) reached the target also by leaving a message. The primary outcome analysis included all patients, who met the inclusion criteria. We analyzed the data using the statistical software package R, a public domain statistical software package in conjunction with the R software packages nnet[32] for the multinomial logistic regression. [33]. We used the probabilistic programming software Stan in conjunction with the R software packages rstan and rstanarm [33–35] to implement the Bayesian models with Stan’s Hamiltonian Monte Carlo algorithms. These are available under the General Public License of the Free Software Foundation[36] at no cost.
3 Results
3.1 Demographics
Patient recruitment and retention are reported in a CONSORT flow chart (Figure 1: CONSORT Flow Chart). Of 963 patients screened, 10 patients did not fit the inclusion criteria, because they were scheduled for their second, (not their first = initial) appointment in our clinic. We included and randomized n = 953 patients in our study. We stopped short of our planned enrollment of 1000, because of overwhelming clinical work due to the introduction of new electronic medical record system.
Characteristics of the population attending our inner-city pain clinic for an initial appointment are detailed in Table 1. Briefly, patients’ median age was about fifty, with two thirds were women, and one third identified as Hispanic and African-American respectively.
Table 1.
Table 1 details the demographics of the enrolled population by treatment group (experimental =“Call”, control =“NoCall”) and suggestes that the two groups are fairly similar in age, racial and gender distribution.
| Characteristics | Call | NoCall |
|---|---|---|
| n = 953 | 475 | 478 |
| Female sex (n) % | 308 (65) | 324 (68) |
| Age (yr) median(IQR) | 53 [44–62] | 52 [43–63] |
| Preferred Language n (%) | ||
| -English | 363 (76) | 390 (82) |
| -Spanish | 97 (20) | 76 (16) |
| -Other | 7 (1) | 6 (1) |
| -Unavailable | 8 (2) | 6 (1) |
| Ethnicity n (%) | ||
| -Hispanic/Latino | 153 (32) | 120 (25) |
| -Non_Hispanic/Latino | 190 (40) | 211 (44) |
| -Unknown | 132 (28) | 147 (31) |
| Race n (%) | ||
| -White | 66 (14) | 71 (15) |
| -Black | 138 (29) | 172 (36) |
| -Asian | 0 (0) | 6 (1) |
| -Multi-racial | 24 (5) | 24 (5) |
| -Other Race | 193 (41) | 137 (29) |
| -Unavailable | 54 (11) | 68 (14) |
3.2 Missing Data
The data for the primary outcome were complete, increasing our confidence in our inferences. Only affecting the secondary exploratory analysis, a few complementary demographics like language preference, race (Figure 1: CONSORT Flow Chart) were missing. In particular, we only were able to record the language used to contact the patient if a call was made and started doing so only after randomization number 207. We detail the missing demographic data in the supplementary online Table: Missing Demographic Data, available online.
3.3 Primary Outcome Analysis Results
The results of our pragmatic trial are summarized in Table 2: Patient Adherence. Among the 953 patients included in the analysis, 475 patients were assigned to the experimental group (and received a call in their own language prior to their scheduled first initial chronic pain clinic appointment), while 478 were assigned to the control group (and did not receive any call prior to their appointment). In the experimental group, we reached 255 (54%) patients in person, left 45 (9%) messages with relatives, voice messages for 137 (29%) patients, but had no contact with 38 (8%) patients. In the experimental group, 275 patients adhered to their scheduled appointment, while 84 cancelled the appointment and 116 failed to attend. In the control group, 249 patients adhered to their scheduled appointment, 31 cancelled the appointment and 198 failed to attend.
Table 2.
Table 2 contrasts patients’ adherence by treatment versus control group allocation. Among the 475 patients who received a call in their own language, 275 patients adhered to their scheduled pain clinic appointment, while among the 478 patients who were randomized for the control intervention (no call), only 249 attended as scheduled. Importantly, we found a stark difference in the number of patients who failed to attend without a cancellation call.
| Arrived | Canceled | No_Show | |
|---|---|---|---|
| Call | 275 | 84 | 116 |
| No Call | 249 | 31 | 198 |
In our primary analysis (multinomial regression), patients who received a call in their own language prior to their scheduled appointment were more likely to adhere with their scheduled appointment (RR 1.89, CI95% [1.42, 1.42]). (The baseline contrast was defined as failing to attend without cancellation call). This effect was statistically significant (p<0.01).
We explored the results further and found that patients who received a call were more likely to cancel their appointment versus failing to attend (RR 4.63, CI95% [2.89, 2.89]). (p<0.01, significant even after correction for multiple testing). For illustrative purposes in a dichotomous contrast, this would correspond for example to odds ratio of 1.26 for adherence, (defined as attending their scheduled appointment on time) versus non-adherence, (defined as canceling or failing to attend the scheduled appointment), assuming a baseline risk of 56% in the control group.
3.4 Secondary Exploratory Analyses and Multivariate Multinomial Logistic Regression
In two secondary exploratory data analyses, we stratified patients by ethnicity or preferred language, respectively. We compared the effect of our intervention in those patients who (1) identified as Hispanic or Latino, or (2) who noted Spanish as their preferred language versus in those who did not, reporting relative risk [RR] of attending a scheduled appointment. In Table 3: Enhanced Effect in Spanish Speaking Populations, we tabulate the results of both stratified analyses.
Table 3.
Table 3 contrasts effect of the intervention in two stratified analyses by ethnicity (first row) and by language preference (second row). Enhanced effect (reflecting improved adherence) is apparent as higher relative risk (RR) of attending a scheduled appointment in the patients who speak (better) Spanish. Suggesting enhanced effect (adherence), in both stratified analyses (row one and two), the RRs are higher in the left column (in the subpopulations who identify as Hispanic/Latino or who declared Spanish as their preferred language, respectively) versus in the right column (in those subpopulations who have no Spanish ancestry or language preference). We infer that calls in the preferred language (Spanish) lead to improved adherence specifically in Spanish speakers.
| Spanish Speakers | No Language Preference | |
|---|---|---|
| Spanish Preferred | 2.92 | 1.79 |
| Hispanic/Latino | 2.21 | 1.47 |
For Hispanics/Latinos, the intervention, a call before the appointment in the patients preferred language, increased the odds of arrival [RR 2.21] more than in the non-Hispanic/Latino population [RR 1.47]. Equally, our language targeted intervention increased the odds of adherence more in the Spanish speakers [RR 2.92] than in those who did not declare Spanish to be their preferred language [RR 1.79]. These effects in both strata were again statistically significant (p<0.01). We confirmed the increased effectiveness of our language targeted intervention in Spanish speaking subpopulations with a multivariate multinomial logistic regression. The RR (reflecting improved adherence) were again meaningfully higher in the Spanish speaking/Hispanic/Latino populations, (albeit the interaction terms were not statistically significant). In a sensitivity analysis, we repeated the analysis using different models (and software packages) and confirmed the results and inferences.
3.5 Summary of Results and Inferences
Our pragmatic trial supports the hypothesis that a call in the patient’s preferred language increase adherence with scheduled appointments in an inner-city pain clinic serving an immigrant indigent population. The aforementioned associations hold in subgroup analyses, which lend additional credence to our concept that the important component of the intervention is the attunement, which is in line with the importance of cultural and language concordance for patient-provider interactions, especially in the Hispanic immigrant populations[1,2,7,23]. We note that Spanish was only used in about 29 percent of the calls made.
4 Discussion
4.1 Summary of Main Findings
In our pragmatic trial, we demonstrated that a reminder call, in the patient’s preferred language increased adherence with scheduled first appointments in an inner-city chronic pain clinic. Our ethnically and racially diverse, resource-poor population included many patients of mixed Hispanic/Latino descent[37]. Patients who received a prior phone call in their own language (Spanish) were more likely to adhere to their scheduled appointment, and/or much more likely to at least cancel the appointment beforehand. We illustrate the inferred benefits of our culturally sensitive, language congruent initiatives in a graphical abstract (Graphical abstract). Furthermore, they may be more effective in the corresponding linguistic subpopulations. This secondary (unsurprising) finding supports the casual link between intervention and effect.
4.2 Novelty of Results in the Light of Prior Literature
To our knowledge, this is the first randomized trial to rigorously investigate the effectiveness of patient outreach to improve adherence with initial pain clinic appointments [1,14,38]. Our language centered intervention, while currently implemented at the Montefiore Pain Center, is not the standard of practice in the US [28]. In fact, we know of no other pain clinic which instituted similar procedures at present for their underserved immigrant population. The effectiveness of our simple intervention is remarkable because Spanish was only used in about 29 percent of the calls made. We speculate if calls by certified Spanish speaking personnel may be effective in enhancing adherence, even if Spanish is not used in the conversation, because the offer alone may convey a cultural sensitivity, that establishes the human bond.
4.3 Inferences for Clinical Practice
Recent systematic reviews reiterated the manifold and complex causes for rampant disparities[11] in pain among racial and ethnic minorities, involving patient, provider and system factors [10,14,39]. We previously showed that language figures prominently among the many barriers to access chronic pain services in under-served inner-city populations [1,40], but our analysis employed only data from an uncontrolled retrospective cohort. We also previously showed that a comprehensive initiative to address language barriers can improve adherence with scheduled appointments[2], but the retrospective nature of our observational cohort again precluded causal inference. As part of a comprehensive complex socioecological model [41], we developed a conceptional framework with a credible causal model for health care disparities in chronic pain, elements of which we tested in our present prospective controlled randomized pragmatic trial:
Language barriers limit access of Non-English-speaking patients to needed chronic pain services[1].
Specific interventions can enhance adherence or and reduce failure to attend without prior cancellation [2].
Our study therefore addresses the dearth of robust evidence on how to overcome barriers by influencing the demand side[22]. Using the rigorous methodological approach of a blinded randomized pragmatic trial, we tested our a priori hypothesis, enhancing our confidence in the internal validity of our pragmatic trial. We feel that the population we served, was randomly sampled and is characteristic of inner-city under-served populations seen by other academic pain clinics across the country. We had no attrition, cross-over, lost or missing data for our primary outcome, (which might otherwise have let to selection bias). Hence, our findings should be generalizable, especially as we engaged population representatives in our study design to improve the ecological validity of our research findings [28]. We hypothesize that a human outreach should be equally effective for populations with other preferred languages than Spanish.
4.4 Limitations of our Approach
We concede that our pragmatic trial only tested a small element of several moving parts implemented that led to improved adherence [2]. Specifically, we did not explore reasons for failure to attend, but instead used a pragmatic and easy to replicate intervention. We limited our investigation to the initial appointment, fearing that the intense interaction during a chronic pain appointment, with the promise for narcotic prescriptions and further interventions might act as a rather unpredictable confounder on the propensity of patients to attend subsequent appointment. We did not a priori exclude patients who were the non-English, non-Spanish speakers, (who did not get a phone call in their preferred language), a) because we wanted to conduct a pragmatic trial in a realistic setting with a simple intervention that could be easily replicated and b) overwhelmingly our patients preferred English or Spanish, c) language and ethnic identity are culturally sensitive topics, which patients often leave deliberately vague or respond to ambiguously; hence language preference could only be ascertained interactively during the intervention. We concede that our pragmatic trial tested the effectiveness of a human call in the setting of a clinic attuned to the needs of a diverse underserved population [2] and hence may be less effective in other settings, especially where language is less important? We further concede that we did not compare the human phone call in the patient’s preferred language to an automated reminder in English, [disregarding patients’ ability to understand that message][42]. This is especially important since cancellation alone would improve resource utilization and allow additional patients in need of a chronic pain consultation to be scheduled. An automated English call or text might be a suitable comparator for a follow up trial, aggravating any potential inability to understand on the side of the patient and any feeling of alienation by its impersonal character. Clearly even automated reminders are effective[38], but a systematic review compared human versus automated reminders and found the machine intervention less effective than human outreach[43], while a Cochrane review found text messaging reminders similar to telephone reminders in terms of cost effectiveness and their improved adherence[24]. Indeed, we still do not know if the human touch, the choice of language or the reminder per se is the “active ingredient” to improve adherence with scheduled appointments[7,20], or the ability to opt out. However, our secondary stratified analysis suggested that our intervention was even more effective in the subpopulation of patients who identify as Hispanic/Latino. The human making the call tuned the language of the reminder interactively to the responding person(s). If attunement[44] is helpful or critical to engage Latino patients to adhere with scheduled pain clinic appointments is admittedly conjecture, awaiting confirmation in further studies.
4.5 Economic Impact
The economic impact of decreasing the rate of patients failing to attend a scheduled appointment without even a cancellation call, from 41% to 24% may seem drastic, large and obvious to a pain clinic manager (Table 3: Patient Adherence), but was not formally analyzed in our study. Several benefits may result:
the clinic can see more patients, a significant financial windfall[5],
predictable scheduling allows more short-term, rational and efficient staffing[45],
reduced wait times improve patient satisfaction[20] and reduce provider stress[6].
The aforementioned benefits in our eyes clearly justify the additional minimal resources invested by a human phone call in the patient’s preferred language. We hypothesize that beyond the likely economic benefit, this outreach is an opportunity to engage our most vulnerable patients to build trust[20] and to avoid negative transference by providers with “frequent offenders”[6]. We speculate that the resulting enhanced patient-physician relationship will also improve adherence with subsequent treatment recommendations[46,47]; however, we concede that the latter hypothesis is again conjecture, warranting equally rigorous confirmation in future randomized trials.
4.6 Conclusion
In our pragmatic trial, an outreach human phone call in the patient’s primary language increased adherences with scheduled appointments in the ethnically diverse and resource poor population typically served by an inner-city academic chronic pain clinic. Our study exemplifies how a rational and rigorous scientific approach to improve health systems and to mitigate health care disparities can improve access to pain service, which continues to be an imperative priority [15]. It remains to be evaluated how much human phone reminders in the patient preferred language save in health care resources[14], if they provide a considerable economic benefit and if they are indeed effective through bolstering the patient provider relationship.
Supplementary Material
The Supplementary Table tabulates the missing data for the supplementary demographics, showing in the diagonal the number of missing observations for each variable, in the upper triangle of the table, the number of jointly observed and in the lower triangle the number of jointly missing observations for the corresponding variables. No data were missing for the primary outcome.
Highlights.
Poor attendance at scheduled pain clinic appointments indicate barriers to healthcare.
Phone calls in the patient’s primary language increase adherence and safe costs.
Rational and rigorous health systems research can improve access to pain service, while saving health care resources.
Targeted language-centered interventions to enhance adherence may be more effective in corresponding linguistic subpopulations.
Acknowledgments
We would like to acknowledge the contribution of Tiffany Rodriguez, in particular her suggestions on how to improve adherence, how to collect the data, what additional demographics and aspects to consider. This research is supported in part by the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), through CTSA grant numbers 5KL2TR001071-03 and UL1 TR001073. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Conflicts of Interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shaparin N, White R, Andreae M, Hall C, Kaufman A. A longitudinal linear model of patient characteristics to predict failure to attend an inner-city chronic pain clinic. J Pain. 2014;15:704–11. doi: 10.1016/j.jpain.2014.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andreae MH, White RS, Chen KY, Nair S, Hall C, Shaparin N. The Effect of Initiatives to Overcome Language Barriers and Improve Attendance: A Cross-Sectional Analysis of Adherence in an Inner City Chronic Pain Clinic. Pain Medicine. 2016;18:pnw161. doi: 10.1093/pm/pnw161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macharia WM, Leon G, Rowe BH, Stephenson BJ, Haynes RB. An overview of interventions to improve compliance with appointment keeping for medical services. Jama. 1992;267:1813–7. [PubMed] [Google Scholar]
- 4.Ulmer T, Troxler C. The economic cost of missed appointments and the open access system. Community Health Scholars. 2006 [Google Scholar]
- 5.Moore CG, Wilson-Witherspoon P, Probst JC. Time and money: Effects of no-shows at a family practice residency clinic. Fam Med. 2001;33:522–7. [PubMed] [Google Scholar]
- 6.Husain-Gambles M, Neal RD, Dempsey O, Lawlor DA, Hodgson J. Missed appointments in primary care: Questionnaire and focus group study of health professionals. Br J Gen Pract. 2004;54:108–13. [PMC free article] [PubMed] [Google Scholar]
- 7.Añez LM, Paris M, Jr, Bedregal LE, Davidson L, Grilo CM. Application of cultural constructs in the care of first generation latino clients in a community mental health setting. J Psychiatr Pract. 2005;11:221–30. doi: 10.1097/00131746-200507000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Akhter K, Dockray S, Simmons D. Exploring factors influencing non-attendance at the diabetes clinic and service improvement strategies from patients’ perspectives. Practical Diabetes. 2012;29:113–6. [Google Scholar]
- 9.Pieper B, DiNardo E. Pearls for practice. reasons for missing appointments in an outpatient clinic for indigent adults. Journal of the American Academy of Nurse Practitioners. 1998;10:359–64. doi: 10.1111/j.1745-7599.1998.tb00519.x. [DOI] [PubMed] [Google Scholar]
- 10.Green CR, Anderson KO, Baker TA, Campbell LC, Decker S, Fillingim RB, et al. The unequal burden of pain: Confronting racial and ethnic disparities in pain. Pain Med. 2003;4:277–94. doi: 10.1046/j.1526-4637.2003.03034.x. [DOI] [PubMed] [Google Scholar]
- 11.Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: Findings from a national sample. Med Care. 2002;40:52–9. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Barron WM. Failed appointments. who misses them, why they are missed, and what can be done. Prim Care. 1980;7:563–74. [PubMed] [Google Scholar]
- 13.Akhter K, Dockray S, Simmons D. Exploring factors influencing non-attendance at the diabetes clinic and service improvement strategies from patients’ perspectives. Practical Diabetes. 2012;29:113–6. doi: 10.1002/pdi.1670. [DOI] [Google Scholar]
- 14.Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: Causes and consequences of unequal care. J Pain. 2009;10:1187–204. doi: 10.1016/j.jpain.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Green C, Todd KH, Lebovits A, Francis M American Academy of Pain Medicine Council on Ethics. Disparities in pain: Ethical issues. Pain Med. 2006;7:530–3. doi: 10.1111/j.1526-4637.2006.00244.x. [DOI] [PubMed] [Google Scholar]
- 16.Muse IO, Joseph VA. Evidence of health care disparities in the perioperative setting. ASA Monitor. 2016;80:44–5. [Google Scholar]
- 17.White AA, Chanoff D. Seeing patients: Unconscious bias in health care. Harvard University Press; 2011. [Google Scholar]
- 18.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in us emergency departments. JAMA. 2008;299:70–8. doi: 10.1001/jama.2007.64. [DOI] [PubMed] [Google Scholar]
- 19.Burgess DJ, Phelan S, Workman M, Hagel E, Nelson DB, Fu SS, et al. The effect of cognitive load and patient race on physicians’ decisions to prescribe opioids for chronic low back pain: A randomized trial. Pain Med. 2014;15:965–74. doi: 10.1111/pme.12378. [DOI] [PubMed] [Google Scholar]
- 20.Lacy NL, Paulman A, Reuter MD, Lovejoy B. Why we don’t come: Patient perceptions on no-shows. Ann Fam Med. 2004;2:541–5. doi: 10.1370/afm.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Balsa AI, McGuire TG. Prejudice, clinical uncertainty and stereotyping as sources of health disparities. Journal of Health Economics. 2003;22:89–116. doi: 10.1016/s0167-6296(02)00098-x. doi: https://doi.org/10.1016/S0167-6296(02)00098-X. [DOI] [PubMed] [Google Scholar]
- 22.Ensor T, Cooper S. Overcoming barriers to health service access: Influencing the demand side. Health Policy Plan. 2004;19:69–79. doi: 10.1093/heapol/czh009. [DOI] [PubMed] [Google Scholar]
- 23.Egbert LD, Jackson SH. Therapeutic benefit of the anesthesiologist-patient relationship. Anesthesiology. 2013;119:1465–8. doi: 10.1097/ALN.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 24.Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Atun R, Car J. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Syst Rev. 2013;12:CD007458. doi: 10.1002/14651858.CD007458.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szczepura A. Access to health care for ethnic minority populations. Postgrad Med J. 2005;81:141–7. doi: 10.1136/pgmj.2004.026237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Califf RM, Sugarman J. Exploring the ethical and regulatory issues in pragmatic clinical trials. Clinical Trials (London, England) 2015;12:436–41. doi: 10.1177/1740774515598334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Faden RR, Kass NE, Goodman SN, Pronovost P, Tunis S, Beauchamp TL. An ethics framework for a learning health care system: a departure from traditional research ethics and clinical ethics. The Hastings Center Report. 2013;(Spec No):S16–27. doi: 10.1002/hast.134. [DOI] [PubMed] [Google Scholar]
- 28.Campbell LC, Robinson K, Meghani SH, Vallerand A, Schatman M, Sonty N. Challenges and opportunities in pain management disparities research: Implications for clinical practice, advocacy, and policy. J Pain. 2012;13:611–9. doi: 10.1016/j.jpain.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fernandez A, Schillinger D, Grumbach K, Rosenthal A, Stewart AL, Wang F, et al. Physician language ability and cultural competence. Journal of General Internal Medicine. 2004;19:167–74. doi: 10.1111/j.1525-1497.2004.30266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Suurmond J, Uiters E, Bruijne MC, de Stronks K, Essink-Bot M-L. Negative health care experiences of immigrant patients: A qualitative study. BMC Health Services Research. 2011;11:10. doi: 10.1186/1472-6963-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flores G, Laws MB, Mayo SJ, Zuckerman B, Abreu M, Medina L, et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;111:6–14. doi: 10.1542/peds.111.1.6. [DOI] [PubMed] [Google Scholar]
- 32.Venables WN, Ripley BD. Modern applied statistics with s. 4. New York: Springer; 2002. [Google Scholar]
- 33.R Development Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2008. [Google Scholar]
- 34.Stan Development Team. Stan: A c++ library for probability and sampling, version 2.5.0. 2014. [Google Scholar]
- 35.Gabry J, Goodrich B. Rstanarm: Bayesian applied regression modeling via stan. 2016. [Google Scholar]
- 36.License GGP Free software foundation. License Used by the Free Software Foundation for the GNU Project. 1991 See Http://WwwFsfOrg/Copyleft/GplHtml ( Http://WwwFsfOrg/Copyleft/GplHtml)
- 37.Alejandro Portes CT. Making sense of diversity: Recent research on hispanic minorities in the united states. Annual Review of Sociology. 1987;13:359–85. [Google Scholar]
- 38.Guy R, Hocking J, Wand H, Stott S, Ali H, Kaldor J. How effective are short message service reminders at increasing clinic attendance? A meta-analysis and systematic review. Health Serv Res. 2012;47:614–32. doi: 10.1111/j.1475-6773.2011.01342.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Betancourt JR, Renfrew MR. Unequal treatment in the us: Lessons and recommendations for cancer care internationally. J Pediatr Hematol Oncol. 2011;33(Suppl 2):S149–53. doi: 10.1097/MPH.0b013e318230dfea. [DOI] [PubMed] [Google Scholar]
- 40.Flores G. Language barriers to health care in the united states. N Engl J Med. 2006;355:229–31. doi: 10.1056/NEJMp058316. [DOI] [PubMed] [Google Scholar]
- 41.Salihu HM, Wilson RE, King LM, Marty PJ, Whiteman VE, et al. Socio-ecological model as a framework for overcoming barriers and challenges in randomized control trials in minority and underserved communities. International Journal of MCH and AIDS (IJMA) 2015;3:85–95. [PMC free article] [PubMed] [Google Scholar]
- 42.Junod Perron N, Dao MD, Righini NC, Humair J-P, Broers B, Narring F, et al. Text-messaging versus telephone reminders to reduce missed appointments in an academic primary care clinic: A randomized controlled trial. BMC Health Serv Res. 2013;13:125. doi: 10.1186/1472-6963-13-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hasvold PE, Wootton R. Use of telephone and sms reminders to improve attendance at hospital appointments: A systematic review. J Telemed Telecare. 2011;17:358–64. doi: 10.1258/jtt.2011.110707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Antshel KM. Integrating culture as a means of improving treatment adherence in the latino population. Psychology, Health & Medicine. 2002;7:435–49. doi: 10.1080/1354850021000015258. [DOI] [Google Scholar]
- 45.Price RS, Balcer LJ, Galetta SL. Education research: A new system for reducing patient nonattendance in residents’ clinic. Neurology. 2010;74:e34–6. doi: 10.1212/WNL.0b013e3181d31de4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kardas P, Lewek P, Matyjaszczyk M. Determinants of patient adherence: A review of systematic reviews. Front Pharmacol. 2013;4:91. doi: 10.3389/fphar.2013.00091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Butow P, Sharpe L. The impact of communication on adherence in pain management. Pain. 2013;154(Suppl 1):S101–7. doi: 10.1016/j.pain.2013.07.048. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The Supplementary Table tabulates the missing data for the supplementary demographics, showing in the diagonal the number of missing observations for each variable, in the upper triangle of the table, the number of jointly observed and in the lower triangle the number of jointly missing observations for the corresponding variables. No data were missing for the primary outcome.