Abstract
Young men who have sex with men (YMSM), particularly YMSM who are racial/ethnic minorities, are disproportionately affected by the HIV epidemic in the United States. These HIV disparities have been linked to demographic, social, and physical geospatial characteristics. The objective of this scoping review was to summarize the existing evidence from multilevel studies examining how geospatial characteristics are associated with HIV prevention and care outcomes among YMSM populations. Our literature search uncovered 126 peer-reviewed articles, of which 17 were eligible for inclusion based on our review criteria. Nine studies examined geospatial characteristics as predictors of HIV prevention outcomes. Nine of the 17 studies reported HIV care outcomes. From the synthesis regarding the current state of research around geospatial correlates of behavioral and biological HIV risk, we propose strategies to move the field forward in order to inform the design of future multilevel research and intervention studies for this population.
Keywords: neighborhoods, multilevel model, disparities, gay, youth
Young men who have sex with men (YMSM) are disproportionately affected by the HIV epidemic in the United States. From 2000–2010, the annual number of new HIV diagnoses among YMSM more than doubled (Johnson et al., 2014). In 2014, adolescent and young adult men who have sex with men accounted for 90% of new infections among people aged 13 to 24, and 31% of all new infections among men who have sex with men (CDC, 2015). Once diagnosed with HIV, surveillance data also suggest that youth and sexual minorities living with HIV are less likely to be linked to care, retained in care, or virally suppressed (Hall, Walker, Shah, & Belle, 2012). Given these trends, researchers and advocates have called for greater efforts to address the prevention and care needs of YMSM.
An enduring characteristic of the HIV epidemic has been its disproportionate impact on populations who are socially marginalized due to their race/ethnicity, socioeconomic status, gender, and/or sexual orientation (Bauermeister, Zimmerman, & Caldwell, 2011; Brennan et al., 2012; Johns, Bauermeister, & Zimmerman, 2010; Johnson, Hu, Sharpe, & Dean, 2009; Latkin, German, Vlahov, & Galea, 2013; Millett, Peterson, Wolitski, & Stall, 2006; Oster et al., 2011; Sharpe, Stallworth, Miller, Dean, & Fenton, 2009; Villarruel, Guilamo-Ramos, & Bauermeister, 2012). Researchers have noted that HIV prevalence and incidence among MSM is often concentrated in spaces characterized by a higher density of racial, ethnic, sexual, and gender minorities and among populations living in socioeconomically challenged contexts (Egan et al., 2011; Frye et al., 2014; Koblin et al., 2013; Miller et al., 2016; Mustanski, Birkett, Kuhns, Latkin, & Muth, 2015; Tobin, Latkin, & Curriero, 2014). Although most HIV intervention research has focused on MSM living in urban areas, there is a dearth of research that addresses HIV risk among MSM living in rural areas, despite substantial evidence of significant HIV risk among rural MSM (Oh & Perencevich, 2011). Rates of HIV infection are slightly lower among MSM in non-Metropolitan Statistical Areas (MSAs): non-MSA MSM are affected by HIV at 75%–95% the rates of their urban peers in all regions. HIV infection rates among non-MSA MSM are also substantially higher than the general population (CDC, 2013). Most importantly, researchers have provided strong evidence that the availability of HIV prevention services (e.g., HIV testing) among MSM decreases as the degree of rurality increases (Sanchez et al., 2015). Taken together, these findings highlight the importance of understanding how structural factors (e.g., poverty, racism, and sexual prejudice) shape access to high-quality HIV prevention and care services and contribute to HIV disparities across geographic areas.
Among YMSM in the United States, racial/ethnic minorities disproportionately account for new HIV cases. Recent NHBS data showed 26% of African American MSM youth (18–24 years) tested HIV-positive, compared to only 3% of White MSM youth (Wejnert et al., 2013). Racial/ethnic minority YMSM are also more likely to reside in urban centers characterized by poverty and racial/ethnic segregation, increasing their exposure to social discrimination and disadvantage (Adimora & Auerbach, 2010; Dale et al., 2016; Kipke, Weiss, & Wong, 2007; Wiewel et al., 2015). Although HIV disparities are often attributed to individual-level characteristics (e.g., greater risk behaviors), analyses by Millett and others (Ayala, Bingham, Kim, Wheeler, & Millett, 2012; Millett et al., 2011; Millett, Flores, Peterson, & Bakeman, 2007; Millett et al., 2012; Oster et al., 2011) illustrate that racial/ethnic disparities in HIV persist despite lower reported engagement in risk behaviors. In light of these findings, the National HIV/AIDS Strategy for the United States (White House, 2010), first released in 2010 and updated in 2015, called for community-level approaches to reduce HIV-related health disparities and health inequities, and an intensification of prevention efforts in communities where HIV is heavily concentrated.
Attributing HIV risk behaviors to individual-level decision-making has been criticized due to its tendency to create a quantified, narrow explanation of behavior, and for its lack of attention to the differences in the social contexts in which these behaviors occur (Caceres, Aggleton, & Galea, 2008; Dworkin & Ehrhardt, 2007; Easton et al., 2007; Gupta, Parkhurst, Ogden, Aggleton, & Mahal, 2008; Mustanski, Newcomb, Du Bois, Garcia, & Grov, 2011). Informed by a complex interplay of individual, intrapersonal, and cultural/contextual factors, Díaz and Ayala (2001) noted that the individual-level perspective to HIV prevention and care had “failed to note that ‘who you are’—not in terms of individual identity, but in terms of social location within a context of social oppressive factors—determines to a great extent what you can and cannot do” (p. 4). Acknowledging that individuals do not live in a systemic vacuum, Díaz and Ayala (2001) highlighted how structural factors are associated with health risks:
“We must first acknowledge that HIV risk is not simply an intra-individual factor or the property of certain individuals. In other words, HIV is not transmitted simply because there are risky individuals who practice risky behaviors on account of their individual personal deficits in morality, cognition or behavioral skills. Rather, our findings demand a conceptualization of ‘health risk’ as a characteristic of socially produced contexts. These are social contexts of risk where individuals lose their power to enact their protective intentions, or where unsafe practices are perhaps the only viable and adaptive survival strategy. While individuals’ values, cognitions, emotions and skills do become an integral part of the social contexts in which they participate, risk is the product of such social and contextual participation, rather than simply a personal trait that individuals bring along and enact across all situations and circumstances.” (p.24)
As HIV research embraced a more comprehensive view of risk, researchers sought to situate HIV risk within geographies of space and place (Buot, Docena, Raterno, Bittner, Burlew, Nurtidinov & Robbins, 2014; Johnson & Longurst, 2009). Although often used interchangeably in day-to-day conversations, space refers to a specific physical location, whether it be a specific point (e.g., an address) or area (e.g., city) with geographic boundaries. Place, rather, is a social construction; the interpersonal exchanges and dynamics that result in physical and social resources within space. This also includes the development, evolution, and implementation of norms and behaviors within a given space. In examining both space and place within HIV prevention and care outcomes, researchers have begun to explore when, where, and how structural factors increase communities’ disproportionate exposure to risk due to the physical and social characteristics of their environments (Caceres et al., 2008; Latkin, Weeks, Glasman, Galletly, & Albarracin, 2011; Parker, Easton, & Klein, 2000). For the purposes of this review, we use the term “geospatial” to refer to environmental characteristics that describe space and place.
Public health has a long history of examining geographic variability across health outcomes using geospatially-defined datasets (e.g., Census, surveillance reports). These datasets have allowed social epidemiologists to describe how geospatial indicators are related to health disparities and inequalities across diverse geographic locations (Diez-Roux & Mair, 2010). Furthermore, recent advances in statistical modeling (e.g., multilevel modeling, geospatial analyses) have made it possible to link geospatial and individual-level datasets (e.g., participant surveys, medical records), and test complex relationships between individuals and their environments. In light of this complexity, researchers have proposed different pathways to contextualize the geospatial characteristics of the environment and HIV risk behaviors (Frye et al., 2006; Latkin et al., 2013), including increased exposure to negative physical (e.g., number of venues offering alcohol, distance to resources), demographic (e.g., concentrated socioeconomic disadvantage, racial/ethnic segregation), and social (e.g., sexual prejudice, crime) characteristics.
Physical characteristics of the built environment may define and limit access to social settings whereby individuals interact with each other in their communities (Kelling & Coles, 1996). Physical characteristics include the presence of health-promotive institutions (e.g., community organizations, hospitals) within a geographic area, as well as the distance between an individual and these services. Marginalized communities may be limited by the physical characteristics of their environments, making access to services more difficult. The quality of an environment’s physical characteristics has also been implicated in HIV/STI risk studies. In one study, Cohen et al. (2000) developed a “broken window” index, comprised of assessments of housing quality, graffiti, trash, and public school deterioration, and explored the association between this index and the number of gonorrhea cases across geospatial boundaries. Even after controlling for socioeconomic markers such as unemployment, income, and educational level, the “broken window” index continued to predict gonorrhea rates.
Social factors may also contribute to the health of communities and its residents. Structural factors that promote inequities (e.g., income inequality, LGBT discrimination) may fuel disparities in HIV prevalence by limiting access to care, straining resources within social networks, and exposing individuals to HIV and sexuality-related stigma (Frye et al., 2015; Holtgrave et al., 2014; Magnus et al., 2010; Nelson, Walker, DuBois, & Giwa, 2014). These structural factors can also lead to social disorganization (i.e., areas characterized by greater impoverishment and suboptimal infrastructure), which are hypothesized to result in higher rates of problem behaviors (e.g., crime). As a result, individuals living in chronically disinvested areas may be more prone to adopt maladaptive coping behaviors (e.g., transactional sex, substance use) (Bruce et al., 2015; Halkitis et al., 2013; Oldenburg, Perez-Brumer, Reisner, & Mimiaga, 2015), and to experience disruptions in their linkage and retention to HIV prevention and care services (Fortenberry, Martinez, Rudy, Monte, & Adolescent Trials Network, 2012; Frew et al., 2015; Goswami et al., 2016; Hightow-Weidman et al., 2011; Kahana et al., 2015; Philbin et al., 2014).
Beyond the structural measures of space and place, theorists from a variety of disciplines have also noted the importance of considering the mechanisms through which different geospatial characteristics result in individual risk behaviors (Kawachi, 2000). For instance, researchers have noted that geospatial characteristics may affect HIV transmission by shaping individuals’ social and sexual networks (Cooper et al., 2015; Linton et al., 2016; Rothenberg, Muth, Malone, Potterat, & Woodhouse, 2005). For example, prior data suggest that individuals may be more likely to select sex partners who live in closer geographic proximity. This dynamic impacts how HIV is concentrated within sexual networks and affects individuals’ risk for HIV (Rothenberg et al., 2005). In addition, the perceptions of the environment are posited to mediate the associations between geospatial indicators and individual well-being. Past research has found that, after controlling for demographic variables, individuals who perceive a higher sense of community and neighborhood participation were more likely to report fewer risk behaviors (Kawachi, 2000; Latkin et al., 2013; Sampson, Raudenbush, & Earls, 1997). At present, however, the mechanisms through which geospatial factors influence risk-taking among YMSM remain understudied. Thus, there is a pressing need to better understand and address the social-ecological framework of YMSM’s environments.
The objective of this review was to summarize the existing evidence on multilevel studies examining HIV prevention and care outcomes among YMSM populations. Specifically, this review sought to display the breadth of studies for YMSM that combined geospatial factors with either HIV prevention and/or HIV care outcomes. Studies reviewed focused on geospatial characteristics above and beyond individual-level correlates. We recognize that geospatial characteristics might affect HIV prevention and care outcomes differently; for example, the uptake of PrEP (HIV prevention) may be related to a different set of geospatial factors (e.g., physical access) than those associated with viral suppression among HIV-positive individuals (HIV care). Consequently, our review examined HIV prevention behaviors separately from HIV treatment and care outcomes. This review summarizes the current state of the research, proposes new areas of inquiry, and informs the design of future multi-level intervention studies for this population.
METHODS
This review included studies published during the previous six years (January 2010–April 2016) that analyzed spatial factors as correlates of HIV prevention (e.g., testing behavior, sexual risk behavior) and care (e.g., HIV incidence, ART use, viral suppression) outcomes among YMSM. This time-frame was selected for three reasons. First, in 2011 Mustanski et al. published a socioecological review of HIV risk among YMSM in the Annual Review of Sex Research, focusing on papers published up to and including 2010. Thus, the current review extends on Mustanski et al. by focusing on the period 2010–2016. Second, this timeframe aligns with the implementation of the 2010 National HIV/AIDS Strategy (NHAS), which underscored the importance of understanding disparities in HIV/AIDS and examining how community characteristics shape and localize the epidemic. Four decades into the HIV epidemic, the NHAS was the first official national HIV strategy for the United States. NHAS recognized the importance of setting forward a concerted set of research and programmatic priorities for HIV prevention and care that specifically mentioned the need to understand and intervene on structural correlates of HIV. Finally, the HIV prevention and care landscape has changed dramatically over the past six years, with several efficacious biomedical interventions now available (e.g. treatment as prevention (TasP) and pre-exposure prophylaxis (PrEP)). With new biomedical interventions comes potentially new structural factors to consider (e.g. access to care for new interventions). Consequently, we were interested in understanding how spatial factors are associated with HIV related outcomes in this new landscape of HIV prevention and care.
We employed a scoping review methodology (Arksey & O’Malley, 2005). Whereas a systematic review focuses on answering a well-defined question based on the quality of the evidence presented within a particular type of study design and derives consensus on the magnitude of the reported associations across the reviewed studies, a scoping review aims to map out and synthesize key concepts in a complex area of research where the available evidence encompasses a variety of study designs (Colquhoun et al., 2014). We employed the five step procedure proposed by Arksey and O’Malley (2005) for a comprehensive scoping review: (1) identification of domains to be explored, (2) search of existing databases, (3) selection of studies, (4) charting and extraction of data from studies, and (5) collating and summarizing the results.
In this review, we employed the term YMSM to refer to cis-gender male youth (ages 15–29) who may express same-sex attractions and/or engage in same-sex sex behaviors, yet may or may not identify as gay, bisexual, queer and/or questioning (GBQQ). Although this age range included young men in differing developmental stages (e.g., adolescence and emerging adulthood), we purposefully used the term YMSM to align with Centers for Disease Control and Prevention (CDC) surveillance definitions of youth, and the primary definition used to target prevention activities towards this age group. Therefore, to be eligible for inclusion, quantitative studies had to target or report having a subsample of YMSM ages 15–29, be conducted in the United States, and had to focus on HIV prevention and/or care outcomes. Studies with broader samples that were inclusive of YMSM were also eligible. Prevention outcomes included: HIV testing, condom use, number of partners with whom YMSM had condomless anal sex (CAS), CAS with one or more partner with serodiscordant status, and PrEP use. Care outcomes included: HIV and/or STI incidence, anti-retroviral therapy (ART) use and adherence, linkage and retention in HIV care, and viral suppression.
To be eligible for inclusion in the review, a study must have assessed at least one geospatial factor (conceptualized to include both space and place) as a predictor or covariate and be focused on United States-based samples. Inclusion was restricted to U.S. studies to reduce potential confounding that could result from blending differing geopolitical and cultural definitions of space and place. Given the nature of our scoping review, we employed a broad definition of geospatial indicators using Agnew and Duncan’s (1989) characterization of space and place. Space was defined as location (i.e., where an activity or institution is spaced relative to others; e.g., distance between two spaces, density of resources within an area) and locales (i.e., spaces where social interactions are given meaning and foster specific norms and behaviors; e.g., clubs, clinic, workplace). Place was defined as identification and sense of belonging with a space (e.g., attachment to a community, sense of belonging to a neighborhood). Studies that included geospatial indicators pertaining to these domains were considered during our scoping review of the literature, irrespective of the unit of analysis used to measure space (e.g., counties, census tracts, cities).
Comprehensive search strategies were completed using a broad range of relevant databases including: PubMed, CINAHL, PsycInfo, Google Scholar, and Sociological Abstracts. The search strategy combined controlled vocabulary (e.g., Medical Subject Headings) and keywords describing structural barriers, geospatial characteristics, HIV prevention and risk characteristics, and YMSM. Although some relevant content may have been published in grey literature, local publications, bulletins of international, regional, and national organizations, and conference proceedings, we only examined studies that were peer-reviewed and published in the academic literature.
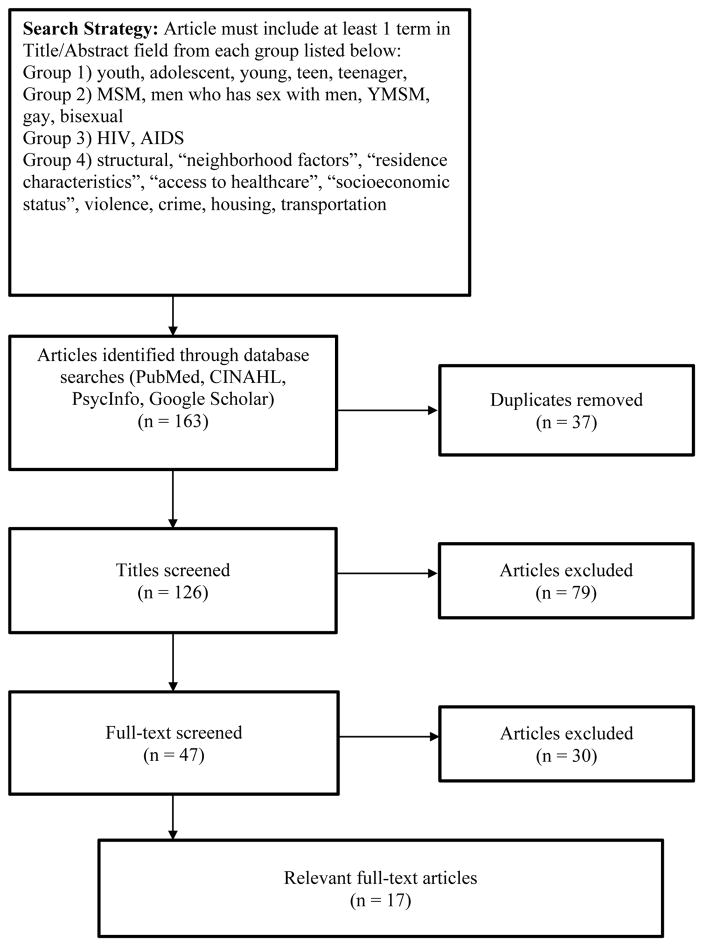
We obtained 163 citations from search terms, 37 citations of which were removed due to duplicate entries. Two authors (JB & DC) independently screened the remaining 126 abstracts for potential inclusion. Upon abstract review, 79 additional studies were excluded because they did not fit the parameters of study inclusion. Full text versions of the remaining 47 articles deemed relevant were extracted for further review. An additional 30 articles were excluded after full-text review due to a lack of geospatial measures, a focus only on methodological issues, and/or provision of only descriptive data about the areas under study. We included 17 quantitative articles in this review (see Figure 1 for a synthesis of the search process).
Figure 1.
Search strategy and disposition of citations. To be included, articles had to contain one or more of certain terms in the title or abstract. Then, articles were screened based on the criteria described in the figure.
RESULTS
Sociodemographic composition of study samples
The following information from the 17 peer-reviewed quantitative articles was abstracted: author name and publication year; study population; sample size; proportion of youth ages 15–29; proportion of racial/ethnic minorities; study location; study description, and primary analytic strategy employed (see Table 1). Most studies recruited participants as part of ongoing studies, and individual-level sample sizes ranged from 167 to 1,891 participants. Most studies used a neighborhood-level boundary for their geospatial unit of analysis and participant-level data as their individual-level unit of analysis; however, two studies used archival data and an aggregate unit of analysis to make inferences: Forsyth and Valdiserri (2015) included data from the 50 U.S. states as their unit of analysis, whereas Goswami et al. (2016) used ZIP code tabulation areas (ZCTAs) as their unit of analysis.
Table 1.
Multilevel studies including YMSM in the United States
| Citation | Sample Size | % 15–29 | % Racial/Ethnic Minority | Location | Design/Year(s) Data Collected | Analytic Strategy |
|---|---|---|---|---|---|---|
| Bauermeister et al. (2015) | 328 | 100% | 73% | Detroit Metro | Observational study (2013) | Random-intercept linear mixed model |
| Bauermeister et al. (2016) | 319 | 100% | 74% | Detroit Metro | Observational study (2013) | Random-intercept linear mixed model |
| Buot et al. (2014) | N/A | N/A | N/A | 80 U.S. Cities | Observational study (1990, 2000) | Student’s T-tests comparing highest and lowest quartiles (OR) |
| Duncan et al. (2014) | 598 | 100% | >70% | New York City | Observational Cohort study (2009–2011) | Bivariate analyses (Chi-square) |
| Eberhart et al. (2013) | 1,704 | ~25% | ~85% | Philadelphia | Retrospective Cohort study (2008–2011) | Logistic Regression |
| Eberhart et al. (2015) | 1,404 | ~25% | ~80% | Philadelphia | Retrospective Cohort study (2008–2009) | Logistic Regression |
| Forsyth & Valdiserri (2015) | N/A | N/A | N/A | 50 U.S. states | Observational study (N/A) | Multiple Regression |
| Frew et al. (2015) | 547 | 12.4% | 92% | Atlanta | Single-Group Quasi-Experimental Intervention (2013) | Random-intercept linear mixed model |
| Frye et al. (2010) | 385 | 100% | 79% | NYC | Observational study (1999–2000) | General estimating equations (GEE) mixed-model |
| Goswami et al. (2016) | 8,413 | N/A | N/A | Atlanta | Observational study (2006–2010) | Multiple Regression |
| Kahana et al. (2016) | 1,891 | 100% | 88% | 20 NIH Adolescent Trial Network sites | Observational study (2009–2012) | Random-intercept linear mixed model |
| Kelly et al. (2012) | 584–641 | 31% | ~38% | NYC | Observational study (2005) | Random-intercept linear mixed model |
| Mustanski et al. (2015) | 167 | 100% | 87% | Chicago | Observational Cohort study (2011–2012) | ANOVA |
| Phillips et al. (2015) | 376 | 100% | 83.5% | Chicago | Observational Cohort study (2011–2012) | Cluster Analysis and Random-intercept linear mixed model |
| Raymond et al. (2014) | 353 | 21.8% | 46.7% | San Francisco | Observational study (2008–2009) | Logistic/Poisson Regressions |
| Sullivan et al. (2015) | 562 | ~41% | 46.20% | Atlanta | Prospective Observational Cohort Study (2010–2012) | Cox Proportional Hazard Regression |
| Surratt et al. (2015) | 503 | 3.6% | 86.5% | South Florida | Observational Study (2010–2012) | Logistic Regression |
The demographic composition of participants included in these studies was diverse with respect to age and racial/ethnic composition. Seven studies focused solely on adolescents and young adults between the ages of 15 and 29. Ten studies focused solely on MSM samples. In eleven studies, racial/ethnic minorities accounted for over 50% of the samples included in the analyses. The majority of studies selected for review were located in large metropolitan areas in the United States (e.g., Atlanta, New York, Philadelphia, San Francisco, Chicago, Detroit); three studies recruited across several US cities.
Analytic methods employed across studies
Overall, most studies employed cross-sectional observational methods to examine the associations between geospatial characteristics and HIV outcomes, with 10 studies analyzing data collected during and/or after 2010. Methodologically, nearly half of the studies (n=7) employed multilevel modeling techniques (e.g., random-intercept linear mixed models, GEE) to account for the clustered, multilevel nature of variables. In the remaining 10 studies, geospatial descriptors were included as clustering variables and/or predictors in analysis of variance and/or regression approaches.
Geospatial indicators extracted from this review were organized into three main categories: demographic characteristics (e.g., income, unemployment, poverty, racial heterogeneity, percent foreign-born), physical characteristics (e.g., availability of HIV services, distance to clinics, public transportation), social characteristics (e.g., income inequality as measured by the GINI ratio, crime, LGBT stigma, HIV prevalence, STI incidence). These indicators were typically extracted from geo-mapped Census, community-level, and public health surveillance datasets, and linked to participants’ location. Although these categories are inextricably tied to each other—and therefore overlap—this organization of geospatial characteristics was adopted in order to facilitate interpretation of findings. In four studies, participants’ subjective assessments of their environment were also included as covariates in analyses alongside geospatial indicators, often positing them as theoretical mediators between the geospatial indicators and HIV outcomes. Consequently, perceived community characteristics were included in this review.
Outcomes
We abstracted the HIV-related outcomes, geospatial indicators included in the study, and the major findings associated to these indicators into a database. We then categorized each study based on whether they were focused on HIV prevention outcomes (n=9 studies; see Table 2), or HIV incidence and care outcomes (n=9 studies; see Table 3).
Table 2.
Studies Examining HIV Prevention Outcomes
| Citation | HIV Outcome(s) | Geospatial Indicators | Main Results |
|---|---|---|---|
| Bauermeister et al. (2015) | HIV Testing (Any HIV test in lifetime) Condomless anal sex (30 days) with 1+ serodiscordant or serounknown partners |
Demographic Characteristics Concentrated Socioeconomic Disadvantage Physical Characteristics Distance to Nearest ASO Distance to Nearest LGBT Bar Distance to Nearest LGBT Center |
Likelihood of HIV testing was greater among YMSM living in more disadvantaged areas and in closer proximity to AIDS Service Organizations. Likelihood of CAS with serodiscordant or serounknown partners was higher in areas with less socioeconomic disadvantage, and further away from nearest ASO. |
| Bauermeister et al. (2016) | Transactional sex with casual partners to overcome socioeconomic needs (lifetime) |
Demographic Characteristics Concentrated Socioeconomic Disadvantage |
Transactional sex with casual partners associated with greater neighborhood socioeconomic disadvantage. This association attenuated (mediation) once individual-level risk behaviors were included in the analysis. |
| Duncan, Kapadia, & Halkitis (2014) | Condomless oral sex (prior 30 days) Condomless anal sex (prior 30 days) |
Social Characteristics Concordance of sexual partners across participants’ residential, social, sexual areas |
YMSM who had concordance across all borough contexts (residential, social and sexual) were more likely to report condomless oral sex. No association between borough concordance and condomless anal sex. |
| Frew et al., (2015) | Willingness to engage in routine HIV testing through a community-based intervention |
Demographic Characteristics % Black residents % Residents aged 25 years or more % Residents over the age of 18 who have a high school diploma Median household income Male employment rate Social Characteristics HIV prevalence Physical Characteristics Number of HIV-related services in community % Vacant households |
Greater willingness to test for HIV was associated with areas where fewer HIV services were available. Greater willingness to test for HIV was also associated with neighborhood characterized by having a greater proportion of Black residents, greater proportion of youth under 25 living in area, and lower median household income. |
| Frye et al., (2010) | Consistent condom use during insertive anal sex (IAS) or receptive anal sex (RAS) in prior 6 months |
Demographic Characteristics Age Distribution (% 18–24 years) % Racial Composition Ethnic heterogeneity % Foreign Born Concentrated poverty Median household income % High school graduates % Unemployed Social Characteristics % Residential instability % Same-sex households Physical Characteristics % Vacant housing |
Consistent condom use for IAS was associated with greater percentage of same-sex headed households. Consistent condom use for RAS was associated with greater percentage of same-sex headed households. |
| Kelly et al., (2012) | Condomless IAI (past 3 months) Condomless RAI (past 3 months) Use of substances during sex (past 3 months) |
Demographic Characteristics Concentrated disadvantage Social Characteristics Gay Enclave Identity Residential stability |
Living in a gay enclave was associated with the use of substances during sex. Partial mediation effects were observed, suggesting that living in a gay enclave was associated with condomless IAI and use of substances during sex, respectively, through possession of a gay-centric network. |
| Mustanski et al., (2015) | Sexual network composition (i.e., concurrency, density, multiplexity, racial assortativity) |
Social Characteristics % HIV prevalence among males ages 15–24 |
Black YMSM had a significantly higher proportion of sexual partners from high HIV prevalence areas compared to Latino, White, and Other YMSM. |
| Phillips et al., (2015) | Condomless anal sex (past 6 months) HIV-positive sex partner (past 6 months) Anonymous sex partner (past 6 months) Met partner online (past 6 months) Sex in exchange for money (past 6 months) Use alcohol during sex (past 6 months) Use drugs during sex (past 6 months) |
Demographic Characteristics % Black % Hispanic Ethnic heterogeneity % Male % Residents are 65 years or older % Residents without a high school degree % Living in poverty % Single-parent households % Foreign-born Social Characteristics % Moved in last year % Same-sex households Violent Crimes Drug Arrests Physical Characteristics Transit Score Walk Score % Vacant buildings |
Eleven community clusters were extracted from neighborhood data. Differences were observed between community clusters around use of alcohol during sex, meeting a partner online, and having sex with a HIV-positive partner. |
| Raymond et al., (2014) | Number of acts of CAS with one or more discordant or HIV status unknown partners (past 6 months) |
Social Characteristics Neighborhood HIV prevalence |
Mean number of potentially serodiscordant CAS acts was associated with lower neighborhood HIV prevalence for White MSM, but not for Black MSM. |
Table 3.
Studies Examining HIV Incidence and Care Outcomes
| Citation | HIV Outcome(s) | Geospatial Indicators | Main Results |
|---|---|---|---|
| Buot et al., (2014) | HIV incidence (5-year average of CDC reported incidence in each city) |
Demographic Characteristics Living Wage estimates Segregation indices Social Characteristics Household GINI coefficients % with health insurance Crime Indices Anti-MSM stigma (same-sex bans) |
HIV incidence associated with cities characterized by higher income inequality, lower living wage estimates, high unemployment, high poverty, low home ownership, and high cost of living. HIV incidence was also associated with cities with fewer high school graduates, higher Black segregation, and low marriage rates. MSM-attributed HIV incidence was associated with greater income inequality, poverty, segregation, and skewed GINI ratio. |
| Eberhart et al., (2013) | Linkage to Care (documentation of one or more CD4 or viral load test results after diagnosis) Linked < 90 days (documentation of one or more CD4 or viral load test results in first 90 days after diagnosis) Retained in Care (at least one medical visit with a provider with prescribing privileges in each 6-month interval, with a minimum of 60 days between visits) Virally Suppression (HIV-1 RNA < 200 copies/ml) |
Physical Characteristics Distance to nearest care site Social Characteristics HIV hot spots (i.e., density of HIV cases in area) |
Living in a HIV hot spot was negatively associated with linkage to care, retention in care and viral suppression. Proximity to care was associated with greater likelihood of being virally suppressed. No association between proximity to care and linkage to care or retention in care was found in multivariable models. |
| Eberhart et al., (2015) | Living in a poor retention in care hotspot Living in a poor viral suppression hotspot |
Demographic Characteristics Economic deprivation Physical Characteristics Distance to medical care sites and pharmacies Density of medical care sites and pharmacies Access to public transit |
Probability of residing in poor retention area was associated with lower economic deprivation, and greater public transit lines. Probability of residing in poor retention in care area was associated with further distance to medical care sites and distance to 5 nearest pharmacies. Probability of residing in a poor viral suppression area was associated with greater economic deprivation and further distance to 5 closest pharmacies. |
| Forsyth & Valdiserri (2015) | Estimated rate of AIDS (Stage 3 HIV Infection) per 100,000 MSM |
Social Characteristics LGBT population density % Homeless youth Marriage equality laws HIV criminalization State-level access to health insurance GINI Index Syphilis rate |
AIDS diagnosis rates among MSM were associated with a lower estimated LGBT population density, with a greater GINI income inequality score, and higher syphilis rate. |
| Goswami et al. (2016) | Linkage to Care (percentage of individuals diagnosed with HIV between 2006–2010 who were linked to care within 3 months of diagnosis) Viral Suppression (percentage of individuals diagnosed with HIV between 2006–2010 who were virally suppressed by end of 2011). |
Demographic Characteristics Poverty level Educational attainment Social Characteristics Income inequality Physical Characteristics Public transit access Car ownership HIV provider availability Residential vacancy Alcohol outlet density |
Linkage to care was associated with car ownership in high-poverty areas; no association between linkage to care and car ownership was observed for low-poverty areas. Viral suppression was associated with high car ownership in low poverty areas. Greater number of bus stops was associated with viral suppression in high poverty areas. |
| Kahana et al., (2016) | Being on ART currently Being on ART for at least 6 month Missed HIV care appointments (past year) Viral Suppression (prior 6 months) |
Demographic Characteristics Socioeconomic disadvantage % Blacks % Latinos Social Characteristics Crime index % HIV prevalence among youth ages 13–24 % Rural |
Likelihood of being currently on ART was associated with living in a less socioeconomic disadvantaged area, and in counties with greater HIV prevalence among 13–24 year olds. ART use for at least 6 months was more likely among youth living in more disadvantaged areas and living in counties with greater HIV prevalence among 13–24 year olds. Missed appointments were associated with counties with greater HIV prevalence among 13–24 year olds. Viral suppression was more likely among youth living in counties with greater HIV prevalence among 13–24 year olds. |
| Phillips et al., (2015) | HIV Status HIV Incidence (new cases among males 15–24 per 100,000 between 2009–2010) HIV Prevalence (cases among males 15–24 per 100,000 between 2009–2010) Chlamydia Incidence (total cases reported by health department in 2013) |
Demographic Characteristics % Black % Hispanic Ethnic heterogeneity % Male % Residents are 65 years or older % Residents without a high school degree % Living in poverty % Moved in last year % Single-parent households % Foreign-born Social Characteristics % Same-sex households Violent Crimes Drug Arrests Physical Characteristics Transit Score Walk Score % Vacant buildings |
Eleven community clusters were extracted from neighborhood data. Differences were observed between community clusters around HIV incidence and prevalence, and chlamydia rates. Clusters with higher walk scores and fewer vacant buildings were less likely to contain HIV-positive individuals. |
| Sullivan et al., (2015) | HIV incidence (new cases between 2010–2014) |
Demographic Characteristics Percent living in poverty Median household income % Of adults with HS degree % Unemployed % Non-Hispanic Black Population density Social Characteristics Violent crime rate % Male same-sex households Male: female sex ratio HIV diagnosis rate Physical Characteristics Alcohol outlet density |
Higher HIV incidence was associated with the percent of Non-Hispanic Blacks. Median household income and % Non-Hispanic Black mediated the racial disparity between Non-Hispanic White and Black men. |
| Surratt et al. (2015) | ART Adherence (percent of doses missed based on self-reported use in past 7 days) |
Demographic Characteristics Area-level Poverty |
Area-level poverty was associated with better adherence in bivariate analyses. Greater spatial disorder was associated with diversion-related non-adherence. Recent homelessness and greater number of diverters in social network size mediated the association between spatial disorder and non-adherence. |
HIV Prevention Outcomes
Nine papers included HIV prevention outcomes, including HIV testing behaviors (n=2) and sexual risk behaviors (n=8). The HIV prevention studies are subdivided into behavioral outcomes (i.e., sexual behaviors that may increase exposure to HIV; n=6) or contextual outcomes (i.e., risky characteristics of the sexual partners or sexual episodes; n=4). Behavioral outcomes included having had insertive and/or receptive CAS, and CAS with serodiscordant or serounknown partners. Contextual outcomes included having sex with partners that could increase the potential for HIV transmission (e.g., partner is HIV-positive, partner lives in a high HIV prevalence area, anonymous sex partner), having sex while using alcohol and drugs, or engaging in transactional sex. Most of the sexual behavior studies focused on sexual risk correlates as outcomes. Only one paper (Sullivan et al., 2015) measured PrEP eligibility, yet did not describe any associations between geospatial indicators and PrEP.
HIV Testing
In both studies examining HIV testing behavior, geospatial demographic characteristics (e.g., racial/ethnic heterogeneity) were assessed. To measure socioeconomic disadvantage, Bauermeister et al. (2015) measured disadvantage using a standardized composite score from five indicators of Census data (i.e., percent of households in poverty, percent of households receiving public aid, percent of single-headed households with children under the age of 18, percent of unemployment, and percent of residents over the age of 25 who do not have a high school degree). Frew et al. (2015), on the other hand, examined similar indicators from Census data, yet did not make a composite disadvantage score. In both studies, the probability of HIV testing was positively associated with geospatial indicators. In the Bauermeister et al. (2015) study, however, the researchers did not include their estimate of percent of racial/ethnic segregation in the multivariate model because of multicollinearity with the socioeconomic disadvantage score (r = .75). In Frew et al.’s (2015) study, HIV testing was not associated with the percent of residents who are Black. They found no association between HIV testing and percent of residents who were 25 years of age or older, high school completion by age 18, the male unemployment rate, or median household income.
Both studies also examined physical indicators of space and measured availability of HIV services in the region. Bauermeister et al. (2015) operationalized nearest distance to AIDS Service Organizations (ASO) or LGBT venues, whereas Frew et al. (2015) assessed the number of available HIV services in the region. In both studies, HIV testing was positively associated with availability of HIV services. Frew and colleagues also examined the percentage of vacant households and HIV prevalence, yet these indicators were not associated with HIV testing.
Behavioral sexual risk
Across the four studies (Duncan, Kapadia, & Halkitis, 2014; Frye et al., 2010; Kelly, Carpiano, Easterbrook, & Parsons, 2012; Phillips et al., 2015) that examined CAS as an outcome, three measured demographic characteristics, two included physical characteristics, and four assessed social characteristics (see Table 2).
Only one study found a direct association between geospatial characteristics and CAS. Frye et al. (2010) measured area-level demographic characteristics (e.g., concentrated poverty and median household income, percent of high school graduates, percent unemployed, percent of 18 to 24 year olds, racial composition and ethnic heterogeneity, percent foreign born), social characteristics (e.g., residentially unstable, same-sex headed households), as well as physical characteristics (e.g., percent vacant housing). In their multivariate results, Frye et al. (2010) found a positive association between consistent condom use for receptive and insertive anal sex, respectively, and a larger proportion of same-sex headed households in the area. There was no association with the remaining characteristics and CAS outcomes in their study. There was no direct association between the geospatial characteristics and CAS outcomes in the three other studies.
Only one study tested for an indirect association between geospatial characteristics and CAS. Kelly et al. (2012) measured both socioeconomic (e.g., concentrated disadvantage) and social characteristics (e.g., residential stability, area is identified as a gay enclave), and found evidence of a partial, indirect (mediational) significant association between geospatial characteristics and CAS. Their mediational analysis linked MSM’s likelihood of engaging in insertive CAS and living in a gay enclave when participants’ social networks were more ‘gay-centric’ (i.e., a greater number of gay men in their social network). This mediational pathway was not observed for receptive CAS.
Two studies (Bauermeister et al., 2015; Raymond et al., 2014) discussed the likelihood of engaging in CAS with one or more serounknown or serodiscordant partners. In the Bauermeister et al. (2015) study, demographic and physical characteristics were examined. The likelihood of CAS with serodiscordant partners was more likely among YMSM who lived in areas with less socioeconomic disadvantage and who resided further away from the nearest ASO. In the second study, Raymond et al. (2014) measured HIV prevalence as a social characteristic of the area and its association with likelihood of serodiscordant partners. Their results suggested a racial interaction effect: CAS serodiscordant acts were more likely in areas with lower HIV prevalence among White MSM; however, this association was not observed for Black MSM.
Contextual sexual risk
Four papers examined the association between geospatial characteristics and contextual sexual risk outcomes. There was varying support for an association between geospatial correlates and having sex with partners that could increase the potential for HIV transmission (e.g., partner is HIV-positive or lives in a high HIV prevalence area, anonymous sex partner, exchanging sex for money) across the four studies (Bauermeister, Eaton, & Stephenson, 2016; Kelly et al., 2012; Mustanski et al., 2015; Phillips et al., 2015) that examined these outcomes. Three studies measured demographic and social characteristics and one included physical characteristics (see Table 2).
Two studies observed an association between socioeconomic disadvantage and contextual sexual risk. Examining the lifetime prevalence of transactional sex with casual sex partners, Bauermeister et al. (2016) noted that YMSM were more likely to report transactional sex if they lived in more socioeconomically disadvantaged areas in metropolitan Detroit, yet this association dissipated once individual-level risk factors (e.g., homelessness, substance use) were included in their model, suggesting full mediation.
Phillips et al. (2015) created clusters using geospatial demographic, social, and physical characteristics to describe different areas in the city of Chicago (see Table 2). Extracting 11 different clusters, the researchers found significant variability in YMSM’s likelihood of using alcohol during sex, meeting a partner online, and having sex with a HIV-positive partner based on what cluster they lived in. Phillips et al (2015) also examined sex in exchange for money; however, they found no differences in transactional sex rates across the clusters representing areas in Chicago. Using a similar dataset as Phillips et al. (2015), Mustanski et al (2015) found that, compared to other racial/ethnic groups in their sample, Black YMSM were more likely to report that a greater proportion of their sexual partners came from areas with a higher HIV prevalence among 15 to 24 year olds.
Similar to the insertive CAS findings described above, Kelly et al. (2012) also found partial mediation evidence whereby MSM’s likelihood of using substances during sex was associated with living in a gay enclave if their network was ‘gay-centric’; however, there was no association between use of substances during sex and demographic or social characteristics.
HIV Incidence and Care Outcomes
Among the nine papers examining HIV prevalence/incidence and/or HIV care-related behaviors (see Table 3), four included HIV prevalence and/or incidence as an outcome. Studies examining HIV care-related behaviors measured different milestones within the HIV continuum of care: four studies focused on linkage and/or engagement in care, two studies examined ART use and adherence, and four studies assessed viral suppression outcomes.
HIV Prevalence and/or Incidence
Support was observed for a direct association between geospatial characteristics and HIV outcomes across the four studies that examined prevalence and/or incidence rates (Buot et al., 2014; Forsyth & Valdiserri, 2015; Phillips et al., 2015; Sullivan et al., 2015). Three studies measured demographic characteristics, four included social characteristics, and two assessed physical characteristics (see Table 3).
Two studies found associations between demographic and social characteristics and HIV incidence. Buot et al. (2014) noted that MSM-attributed HIV incidence was greater in cities with greater income inequality, poverty, and racial/ethnic segregation (as measured by the GINI ratio). Similarly, Sullivan et al. (2015) noted that higher HIV incidence in Atlanta was associated with greater percentage of non-Hispanic Blacks. Moreover, in seeking to explain the racial disparity between non-Hispanic White and Black men, Sullivan and his team found that the percent of non-Hispanic Blacks and household income mediated the racial disparity in HIV incidence.
Phillips et al. (2015) found an association between physical characteristics and HIV prevalence. Areas with lower walkability and greater number of vacant buildings were more likely to have a greater number of HIV-positive individuals living within its region. No other associations were found between HIV prevalence and demographic, social, or physical characteristics (see Table 3).
Support was also found for an association between AIDS diagnosis rate and geospatial characteristics. Forsyth and Valdiserri (2015) pooled data from the 50 states in the United States and found that the rate of AIDS diagnosis among MSM was greater in states with lower LGBT population density, greater income inequality, and higher syphilis rates. There was no association between AIDS diagnosis rate and the remaining state-level characteristics (e.g., percent of homeless youth, marriage equality laws, HIV criminalization, or state-level access to health insurance).
Linkage and engagement in care
Four studies focused on linkage and/or engagement in care (Eberhart et al., 2013; Eberhart et al., 2015; Goswami et al., 2016; Kahana et al., 2016). Three studies included indicators reflecting demographic characteristics. Three studies measured social and physical characteristics (see Table 3).
Eberhart and colleagues (2013) found an association between both linkage to and engagement in care, and geospatial physical and social characteristics. Specifically, Eberhart et al.’s analysis noted that participants living with HIV were less likely to be linked to or retained in care if they lived in areas with greater density of HIV cases (which they termed geospatial “hotspots”). In their multivariable analyses, distance to nearest care site was not associated with linkage to or retention in care.
Eberhart and colleagues (2015) found an association between linkage to or engagement in care and geospatial demographic and physical characteristics. Specifically, they observed that the probability of residing in areas characterized by low retention in care was associated with less economic deprivation. Furthermore, the probability of residing in low retention in care areas was greater in regions with more public transit availability, and in areas further away from medical care sites and pharmacies.
Goswami and colleagues (2016) found some support for an association between linkage to care and the demographic and physical characteristics of the area. Individuals were more likely to link to care if they lived in areas with greater car ownership, but only if they also lived in high-poverty areas. There was no association between linkage to care and remaining physical characteristics (e.g., public transit access, HIV provider availability, residential vacancy, alcohol outlet density) or social characteristics (e.g., income inequality).
Kahana and colleagues (2016) examined linkage to care, as measured by missing one or more HIV medical appointments, and demographic (e.g., socioeconomic disadvantage, representation of Blacks and Latinos in area) and social (e.g., Crime index, urbanity, HIV prevalence among youth ages 13 to 24) characteristics. In their analysis, youth living with HIV were more likely to miss one or more HIV medical appointments if they lived in counties characterized by a high prevalence of HIV cases among youth ages 13 to 24. No other association was observed.
ART use and adherence
Two studies (Kahana et al., 2016; Surratt, Kurtz, Levi-Minzi, & Chen, 2015) examined ART use and adherence. Both studies measured demographic characteristics of the areas, and found a positive association between socioeconomic disadvantage and ART use and/or adherence. Kahana et al. (2016) found that youth were more likely to currently be on ART if they lived in more economically advantaged areas; however, when they measured ART use over six or more months, they found that ART adherence was more likely among youth living in more economically disadvantaged areas. Similarly, Surratt et al. (2015) noted that ART adherence is associated with greater area poverty; however, this association became non-significant in subsequent models. In fact, the authors found that recent homelessness and greater number of recreational drug users (i.e., diverters) in participants’ social networks mediated the association between area disorder and ART non-adherence.
Kahana et al. (2016) also examined whether ART was associated with social (e.g., Crime index, HIV prevalence among youth ages 13 to 24) characteristics. Youth were more likely to currently be on ART, as well as more likely to be ART adherent, if they lived in counties characterized by a high prevalence of HIV cases among youth ages 13 to 24. No other associations were observed by demographic or social characteristics in their analysis.
Viral Suppression
Four studies assessed viral suppression outcomes (Eberhart et al., 2013; Eberhart et al., 2015; Goswami et al., 2016; Kahana et al., 2016), each noting a direct association between geospatial characteristics and viral suppression outcomes. Three studies included indicators reflecting demographic characteristics. Three studies included physical and social characteristics (see Table 3).
Eberhart and colleagues’ study in 2013 found that participants living with HIV were less likely to be virally suppressed if they lived in HIV hotspots. However, HIV-positive participants were more likely to be virally suppressed if they lived in closer proximity to a care site.
In a subsequent study, Eberhart and colleagues (2015) found an association between viral suppression and geospatial characteristics. Specifically, they observed that the probability of residing in areas characterized by having low viral suppression was associated with greater economic deprivation. Furthermore, the probability of residing in low viral suppression area was greater in areas further away from pharmacies. They did not observe an association between viral suppression and the remaining physical characteristics measured in their study (e.g., distance or density to medical care sites, or access to public transit).
In Goswami et al.’s (2016) study, viral suppression was associated with higher car ownership in lower poverty areas and with a higher number of bus stops in high poverty areas. There was no association between viral suppression and remaining physical characteristics (e.g., HIV provider availability, residential vacancy, alcohol outlet density), or social and demographic characteristics.
Kahana et al. (2016) found that viral suppression was more likely among youth who resided in counties characterized by a high prevalence of HIV cases among youth ages 13 to 24. No other associations were observed by demographic or social characteristics in their analysis.
DISCUSSION
Acknowledging that individuals do not live in a social vacuum (Díaz & Ayala, 2001; Frye et al., 2006; Parker, 2001), scholars and policy-makers have called for greater attention to identifying and addressing the structural vulnerabilities fueling HIV disparities among YMSM. In accordance with the scoping review methodology, our intention was not to demonstrate the relative contributions of geospatial covariates of HIV prevention and care. We also did not seek to provide evidence of the strengths of associations given the range in populations and sample sizes of the studies reviewed, nor compare effect sizes. Rather, the scoping review intended to illustrate the range of geospatial factors that have been shown to be associated with HIV prevention and care, as a necessary step to informing the development of multilevel interventions. The collective findings of the studies reviewed suggest that geospatial characteristics are associated with HIV-related prevention and care outcomes; however, we did not find consensus across studies. For HIV prevention outcomes, there was greater consensus of an association between geospatial characteristics and HIV testing and contextual risk behaviors. There was less consensus in studies examining geospatial characteristics and CAS outcomes. Consensus regarding the role of geospatial characteristics on HIV incidence and care outcomes was more evident across studies reviewed. Below, we outline several factors that may have influenced the variability between studies.
Researchers tested how spatial indicators were associated with HIV-related prevention and care outcomes, often relying on archival geo-mapped data to test relationships. Although the inclusion of these geospatial indicators in the analyses acknowledges that structural factors shape the demographic, physical, and social contexts where individuals interact, the reliance on archival data may limit our ability to measure complex mechanisms and advance our theoretical understanding of how individual, network, and geospatial characteristics jointly contribute to HIV prevention and care among YMSM. Investment in longitudinal studies where researchers are able to collect data across these different levels is warranted. Although the design of these multilevel studies will require careful attention (see Koblin et al. (2013) for a review on these methodological considerations), the conceptual definitions for space and place will also be critical. Geospatial data can be operationalized based on political (e.g., states, counties, cities), geographic (e.g., zip codes, Census tracts), and/or social (e.g., neighborhoods) definitions. These distinctions will be important to untangle conceptually as the field moves forward, as each geospatial indicator might convey a different meaning of what constitutes space or place in a dataset. For example, a study using a politically-defined data (e.g., Census tracts) to characterize neighborhoods may diverge from the sociocultural boundaries assigned by residents to the same space. Moreover, recent data suggest that the characteristics of spaces where youth and MSM reside, work, socialize, and have sex may be quite different from each other (Duncan et al., 2014; Koblin, Egan, Nandi, Sang, Cerda, Tieu, Ompad, Hoober & Frye, 2016; Tobin et al., 2014). As a result, new methods that account for the role of diverse geospatial locations (e.g., home, sexual spaces, social spaces) on health outcomes are warranted. These new approaches will also require the consideration of virtual spaces and their interface with YMSM’s navigation of physical spaces, particularly given the increasing popularity of geospatially-focused phone applications that inform YMSM’s partner-seeking behaviors and pursuit of HIV prevention and care resources (Grov, Breslow, Newcomb, Rosenberger & Bauermeister, 2014; Muessig, Nekkanti, Bauermeister, Bull & Hightow-Weidman, 2015).
Socioeconomic and demographic characteristics were most often included in studies, perhaps due to the availability of public geo-mapped datasets (e.g., U.S. Census, American Community Survey) that routinely measure these indicators. Contrary to the assumption that greater socioeconomic deprivation is an indicator of poor health, we found that studies including socioeconomic disadvantage as a predictor in multilevel models often noted that participants living in economically strained areas were more likely to adopt HIV prevention and care recommendations. One possible explanation for these findings might be that youth living in socioeconomically constrained environments may be cognizant of their heightened risk, either by introspection (e.g., perceived susceptibility) and/or by observing their environment (e.g., knowing community members who live with HIV), and actively seek to mitigate that risk (e.g., greater HIV testing). Similarly, Kahana et al. (2016) noted that the inverse association between disadvantage and HIV care outcomes might be confounded by the availability of supplemental government programs (e.g., Ryan White, Medicaid) and other publicly funded entitlements geared to address the high-burden of HIV in these locations. As a result, it is possible that the association between greater socioeconomic disadvantage and HIV prevention and care outcomes may differ if these researchers had included a geospatial indicator quantifying the amount of publicly-supported infrastructure within these impoverished areas. Unfortunately, these mediational pathways remain unexamined and should be tested in future research. As noted, the majority of the studies included in the review employed cross-sectional designs; utilizing longitudinal study designs would help resolve the endogeneity created by the placement of HIV prevention services in areas of high need.
Physical characteristics (e.g., access to transportation; distance and/or density of HIV services) were most often associated with HIV prevention and care behaviors across studies. Greater availability of physical resources (e.g., access to transportation, greater proximity to HIV services) were associated with increased odds of adopting HIV prevention and care recommendations, whereas physical deficits (e.g., housing vacancy, limited availability of medical services and pharmacies) were associated with poorer HIV-related behaviors. These findings underscore the importance of employing geographic information system (GIS) approaches to identify areas of need, and documenting how the built environment may be associated with HIV prevention and care behaviors (Geanuracos et al., 2007). Future research examining how investment in the physical environment improves and/or hinders HIV prevention and care strategies is needed, as it may inform public policy efforts.
Compared to the demographic and physical characteristics, fewer studies examined the association between social characteristics and HIV outcomes. The absence of these associations, however, may be due in part to the limited measurement of these indicators in existing and publicly available datasets. Income inequality, LGBT stigma, and LGBT visibility stood out in our review as salient social indicators. Across studies that measured income inequality (e.g., GINI ratio or male:female ratio of earnings), greater income inequality was associated with poorer HIV outcomes (Buot et al., 2014; Forsyth & Valdiserri, 2015). Among studies examining enacted stigma (e.g., LGBT discriminatory policies), no association was found between LGBT bans (e.g., marriage) and HIV outcomes (Buot et al., 2014; Forsyth & Valdiserri, 2015). However, when LGBT visibility (e.g., density of LGBT populations, spaces denoted as gayborhoods or gay enclaves) was included as a geospatial predictor, mixed findings were observed across HIV prevention and care outcomes. Frye et al. (2010), for example, noted greater consistent condom use among YMSM living in areas with a greater percentage of same-sex headed households. Kelly et al. (2012), on the other hand, noted that living in an area denoted a gay enclave increased the odds of engaging in substance use during sex in their sample. It is possible that the variation across studies may be ascribed to different historical and contextual characteristics not easily measured through quantitative markers and/or not necessarily replicable across communities. Similar to mixed-methods work carried out during the descriptive phase of community needs assessments (Brawner, Reason, Goodman, Schensul, & Guthrie, 2015), research examining how and under what conditions social characteristics are associated with the health and well-being of sexual minority communities in inferential studies is warranted.
Although most studies examined constructs related to the demographic, physical, and/or social context simultaneously, it is important to recognize that these complex structural forces are often intertwined – creating statistical challenges including multicollinearity and confounding. Concentrated socioeconomic disadvantage and racial/ethnic segregation are often highly correlated in the United States (House & Williams, 2003; Kawachi, Daniels, & Robinson, 2005; Williams & Jackson, 2005). For example, Bauermeister et al. (2015) noted that they were unable to include racial/ethnic segregation in metro Detroit as a covariate in their models because of its high correlation with socioeconomic disadvantage. Furthermore, these sociodemographic characteristics may result in systematic under-investment in infrastructure (e.g., transportation, quality housing) and social characteristics (e.g., residential stability, crime). For instance, racial/ethnic composition of certain areas seemed to contextualize the associations observed across several studies (Buot et al., 2014; Frew et al., 2015; Mustanski et al., 2015; Raymond et al., 2014; Sullivan et al., 2015). Consequently, identifying specific structural indicators associated with HIV is vital to inform key components in multilevel interventions. Future research should consider to what extent the accumulation of negative structural factors within a geospatial context results in greater HIV vulnerability.
Communities possess myriad forms of resources, yet a climate of scarcity may nevertheless breed intolerance, disrupt equitable access to community resources (e.g., social support, civic engagement, LGBT attachment), and promote dynamics (e.g., compulsory masculinity or machismo, sexual prejudice, HIV stigma) that fuel social marginalization (Bruce, Harper, & Adolescent Medicine Trials Network for, 2011; D’Augelli, 1998; Díaz, Ayala, & Bein, 2004; Harper & Schneider, 2003; Huebner et al., 2014; Ramirez-Valles, 2002; Ramirez-Valles, Kuhns, Campbell, & Diaz, 2010). Under these circumstances, the composition and dynamics of YMSM’s sexual networks may be modified and lead YMSM to be situated within networks that have a greater HIV risk concentration (e.g., density of HIV in sexual network, drug availability) (Bauermeister, 2008; Egan et al., 2011; Kelly et al., 2010; Schneider et al., 2013; Tobin et al., 2014). In our review, we found some support for these mediation pathways. For example, Kelly et al. (2012) found that the association between living in areas identified as “gay enclaves” and insertive anal sex and substance use during sex were mediated by having social networks with greater density of gay men. Similarly, Surratt et al. (2015) found that the association between area-level poverty and ART adherence was mediated by recent experiences of homelessness and having a greater number of individuals who use prescribed drugs for recreational purposes (‘diverters’) within the social network. Undoubtedly, greater efforts to test these mediational pathways are warranted in future research.
Through these structural factors and community processes, YMSM may have increased odds of experiencing HIV risk correlates, including substance abuse and psychological distress, limited use of HIV services, and experiences of discrimination and micro-aggressions (Mustanski et al., 2011). This is particularly problematic if we are to consider the role that these correlates may play in encouraging YMSM to engage in safer sex behaviors, get routinely tested for HIV/STIs, and/or link to and remain in care. Finally, individual-level sociodemographic characteristics may further inform these associations. Given the racial/ethnic HIV/STI disparities observed among YMSM, for example, it is vital to recognize that Black, Latino and other racial/ethnic minority YMSM are also more likely to be socially marginalized by their racial/ethnic and sexual communities (Diaz & Ayala, 2001). This synergy results in cumulative minority statuses that may exacerbate social isolation and result in greater HIV/STI vulnerability by disrupting their access to community resources and social capital potentially available within their racial/ethnic communities and sexual minority communities.
Methodologically, the majority of studies employed cross-sectional designs with urban samples in their analyses and/or only measured geospatial indicators at a single point in time. Given the dynamic changes (e.g., clinic closures, redevelopment, gentrification) that may occur within a space and across participants’ residential location over time (Cooper et al., 2015; Linton et al., 2016), future research should seek to examine how temporal multilevel changes are associated with HIV prevention and care outcomes among YMSM. Finally, although our review included YMSM from most states and territories in the United States, they may not constitute representative samples within each region, have limited representation of rural areas (Kakietek, Sullivan, & Heffelfinger, 2011; Metheny & Stephenson, 2016), and not be generalizable due to endogeneity bias (i.e., individuals may not be able to self-select into their communities of choice). Greater attention to recent methodological innovations and approaches—including measuring changes over time, propensity to have geospatial concurrency across life domains, and improved measurement of these geospatial indicators—may help to overcome some of these existing limitations in the literature (Koblin et al., 2013).
We acknowledge that our review has several limitations. First, our findings may be subject to publication bias given that unpublished studies offering weak or null effects are not reported as often in the scientific literature. Nonetheless, as the demand for peer-reviewed evidence-based findings increases, we present the evidence in a peer-reviewed scholarly journal in hopes that their evidence informs ongoing programmatic efforts. Second, we excluded descriptive geospatial studies and qualitative studies, as we were focused on reviewing quantitative studies that sought to make statistical inferences between geospatial characteristics and HIV prevention and care outcomes. Nevertheless, we recognize that many of the dynamic, multilevel processes described qualitatively in the literature may help to strengthen the measurement of geospatial indicators, as well as the theoretical inferences and conclusions made in multilevel quantitative studies. A review of this rich body of literature may be warranted. Third, we aligned our scoping review with the release of the National HIV/AIDS Prevention Strategy in the United States. Therefore, our criteria for peer-reviewed journal publications excluded studies prior to 2010. Fourth, only a limited of studies examined or made mention to PrEP and Treatment as Prevention (TasP) when operationalizing condomless anal sex. Given the wealth of recent evidence illustrating the efficacy of PrEP and TasP as HIV prevention modalities, examining how geospatial indicators are associated with PrEP and TasP among YMSM should be prioritized, particularly as these data may inform where to increase access to these biomedical technologies (Eaton, Driffin, Bauermeister, Smith & Conway-Washington, 2015). Finally, the variety in outcome operationalization and intervention strategies did not allow us to perform a meta-analysis. Efforts geared towards standardizing the measurement of HIV prevention and care outcomes across studies are warranted, as they might help us better compare findings in future studies. Moreover, although most studies included a substantial proportion of YMSM, most of the findings are not specific to YMSM samples. As more multi-level HIV studies are published with similar outcomes among YMSM, we hope that measuring effect sizes attributable to geospatial characteristics will be possible. Furthermore, although the HIV disparity faced by YMSM is substantial, our responses will require the development and testing of a cohesive theoretical framework that organizes how geospatial characteristics affect the psychosocial development of YMSM. In the absence of such a framework, our ability to derive consensus across studies’ findings and point to multilevel intervention opportunities will remain limited.
Our review focused on geospatial indicators among YMSM living in the United States. Our hope is that this work may be used as a starting point to examine the multilevel mechanisms affecting the sexual well-being of YMSM and other populations in other regions. As research on space and place continues to grow on a global scale and there is an increase in research on the epidemiology of HIV among MSM in resource-poor settings internationally, it will be important to understand how the aforementioned geospatial constructs are operationalized in other cultures and populations. Couched in the wider sexual and reproductive health literature, this review aligns with a growing interest in understanding how structural factors shape a range of sexual and reproductive health outcomes. Geospatial indicators of social advancement (e.g., social indicators of women’s education attainment) within a community, for example, may shape sexual and reproductive health directly through increased health literacy and health decision making, improve understanding of the opportunity costs associated with childbearing, and encourage health service utilization and modern contraceptive use (Bongaarts, 2010; Cleland et al. 2011; Do & Kurimoto 2012; Jewkes 2002; Antai & Adaji 2012). More egalitarian gender norms and gender equity within a community may support reductions in attitudes that privilege large families, limit men’s control over women’s health decision-making, improve couple communication, and encourage innovative fertility behavior such as modern contraceptive use (DeRose & Ezeh 2010; Nanda et al. 2013). Lastly, increased economic development within a community, including labor-market conditions and infrastructure development, may increase the availability, access and utilization of health services within communities (Bongaarts, 2010). While this body of research is focused almost exclusively on women in resource poor environments, it would be useful to draw parallels and examine how these geospatial indicators are associated with the well-being of YMSM in other settings (particularly among YMSM in resource poor settings).
These limitations notwithstanding, our review highlights the importance of the ways in which structural characteristics are associated with HIV prevention and care. Across the 17 studies reviewed, we found that geospatial indicators were both direct and indirect correlates of HIV prevention and care outcomes among YMSM. The findings of our review align with the vision of the National HIV/AIDS Prevention Strategy’s call to intensify prevention efforts through community-level approaches in communities where HIV is heavily concentrated. Multi-level HIV prevention and care efforts seeking to address the social contexts where YMSM live and interact are warranted. Alongside policy-level efforts to reduce concentrated poverty, racial segregation, and LGBT stigma across the United States, multilevel strategies that focus on strengthening the accessibility to, and quality of, HIV prevention and care resources within specific communities are recommended. Moreover, given the mediating role of network-level characteristics in the association between geospatial characteristics and HIV prevention and care outcomes, network-level interventions that focus on strengthening YMSM’s existing networks and creating opportunities to bridge resources across social networks may be warranted. Taken together, these multilevel strategies may create opportunities for YMSM to build community capacity and social capital, as well as reduce community-level inequities through resource sharing. Finally, informed by our conceptual model, we encourage researchers invested in understanding and addressing the multilevel correlates of HIV prevention and care to expand their ongoing efforts to include mediational pathways that examine how structural factors exacerbate HIV vulnerability of YMSM across the United States.
Acknowledgments
Drs. Bauermeister and Stephenson are supported by a National Institutes of Health project (R01DA041032; U01MD011274). Dr. Eaton was supported by two National Institutes of Health projects (R01MH094230; R01NR013865). The content is solely the responsibility of the authors and does not represent the official views of the funding agencies.
Contributor Information
José A. Bauermeister, University of Pennsylvania.
Daniel Connochie, University of Pennsylvania.
Lisa Eaton, University of Connecticut.
Michele Demers, University of Michigan.
Rob Stephenson, University of Michigan.
References
- Adimora AA, Auerbach JD. Structural interventions for HIV prevention in the United States. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):S132–135. doi: 10.1097/QAI.0b013e3181fbcb38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antai D, Adaji S. Community-level influences on women’s experience of intimate partner violence and terminated pregnancy in Nigeria: a multilevel analysis. BMC Pregnancy Childbirth. 2012;12:128. doi: 10.1186/1471-2393-12-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- Ayala G, Bingham T, Kim J, Wheeler DP, Millett GA. Modeling the impact of social discrimination and financial hardship on the sexual risk of HIV among Latino and Black men who have sex with men. Am J Public Health. 2012;102(Suppl 2):S242–249. doi: 10.2105/AJPH.2011.300641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA. Latino gay men’s drug functionality: the role of social networks and social support. J Ethn Subst Abuse. 2008;7(1):41–65. doi: 10.1080/15332640802081943. [DOI] [PubMed] [Google Scholar]
- Bauermeister JA, Eaton L, Andrzejewski J, Loveluck J, VanHemert W, Pingel ES. Where You Live Matters: Structural Correlates of HIV Risk Behavior Among Young Men Who Have Sex with Men in Metro Detroit. AIDS Behav. 2015;19(12):2358–2369. doi: 10.1007/s10461-015-1180-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Eaton L, Stephenson R. A multilevel analysis of neighborhood socioeconomic disadvantage and transactional sex with casual partners among young men who have sex with men living in Metro Detroit. Behavioral Medicine. 2016;42:197–206. doi: 10.1080/08964289.2015.1110560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Zimmerman MA, Caldwell CH. Neighborhood disadvantage and changes in condom use among African American adolescents. J Urban Health. 2011;88(1):66–83. doi: 10.1007/s11524-010-9506-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bongaarts J. The causes of educational differences in fertility in sub-Saharan Africa. Vienna yearbook of population research. 2010:31–50. [Google Scholar]
- Brawner BM, Reason JL, Goodman BA, Schensul JJ, Guthrie B. Multilevel Drivers of Human Immunodeficiency Virus/Acquired Immune Deficiency Syndrome Among Black Philadelphians Exploration Using Community Ethnography and Geographic Information Systems. Nursing research. 2015;64(2):100–110. doi: 10.1097/Nnr.0000000000000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan J, Kuhns LM, Johnson AK, Belzer M, Wilson EC, Garofalo R Adolescent Medicine Trials Network for HIVAI. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health. 2012;102(9):1751–1757. doi: 10.2105/AJPH.2011.300433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce D, Harper GW Adolescent Medicine Trials Network. Operating without a safety net: gay male adolescents and emerging adults’ experiences of marginalization and migration, and implications for theory of syndemic production of health disparities. Health Educ Behav. 2011;38(4):367–378. doi: 10.1177/1090198110375911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce D, Kahana SY, Bauermeister JA, Nichols SL, Hightow-Weidman LB, Heinze JE … Adolescent Medicine Trials Network for, H. I. V. A. I. Neighborhood-level and individual-level correlates of cannabis use among young persons living with HIV/AIDS. Drug Alcohol Depend. 2015;151:173–180. doi: 10.1016/j.drugalcdep.2015.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buot ML, Docena JP, Ratemo BK, Bittner MJ, Burlew JT, Nuritdinov AR, Robbins JR. Beyond race and place: distal sociological determinants of HIV disparities. PloS one. 2014;9(4):e91711. doi: 10.1371/journal.pone.0091711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caceres CF, Aggleton P, Galea JT. Sexual diversity, social inclusion and HIV/AIDS. AIDS. 2008;22(Suppl 2):S45–55. doi: 10.1097/01.aids.0000327436.36161.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. HIV Surveillance Report. 2013 Retrieved from http://www.cdc.gov/hiv/library/reports/surveillance.
- CDC. HIV and Young Men Who Have Sex With Men. 2015 Retrieved from http://www.cdc.gov/healthyyouth/sexualbehaviors/pdf/hiv_factsheet_ymsm.pdf.
- Cleland JG, Ndugwa RP, Zulu EM. Family planning in sub-saharan africa: Progress or stagnation? [Planning familial en Afrique subsaharienne: Progrès ou stagnation?] Bulletin of the World Health Organization. 2011;89(2):137–143. doi: 10.2471/BLT.10.077925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen D, Spear S, Scribner R, Kissinger P, Mason K, Wildgen J. “Broken windows” and the risk of gonorrhea. Am J Public Health. 2000;90(2):230–236. doi: 10.2105/AJPH.90.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, Kastner M, Moher D. Scoping reviews: time for clarity in definition, methods and reporting. Journal of Clinical Epidemiology. 2014;67(12):1291–1294. doi: 10.1016/j.jclinepi.2014.03.013. [DOI] [PubMed] [Google Scholar]
- Cooper HL, Linton S, Haley DF, Kelley ME, Dauria EF, Karnes CC, … Bonney LE. Changes in Exposure to Neighborhood Characteristics are Associated with Sexual Network Characteristics in a Cohort of Adults Relocating from Public Housing. AIDS Behav. 2015;19(6):1016–1030. doi: 10.1007/s10461-014-0883-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Augelli AR. Developmental implications of victimization of lesbian, gay, and bisexual youths. Stigma and sexual orientation: Understanding prejudice against lesbians, gay men, and bisexuals. 1998:187–210. [Google Scholar]
- Dale SK, Bogart LM, Galvan FH, Wagner GJ, Pantalone DW, Klein DJ. Discrimination and Hate Crimes in the Context of Neighborhood Poverty and Stressors Among HIV-Positive African-American Men Who Have Sex with Men. J Community Health. 2016;41(3):574–583. doi: 10.1007/s10900-015-0132-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRose LF, Ezeh AC. Decision-making patterns and contraceptive use: evidence from Uganda. Population Research and Policy Review. 2010;29(3):423–439. [Google Scholar]
- Diaz R, Ayala G. Social Discrimination and Health: The Case of Latino Gay Men and HIV Risk. 2001. Retrieved from New York. [Google Scholar]
- Diaz RM, Ayala G, Bein E. Sexual risk as an outcome of social oppression: data from a probability sample of Latino gay men in three U.S. cities. Cultur Divers Ethnic Minor Psychol. 2004;10(3):255–267. doi: 10.1037/1099-9809.10.3.255. [DOI] [PubMed] [Google Scholar]
- Diez-Roux A, Mair C. Neighborhoods and health. Annals of the New York Academy of Sciences. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Do M, Kurimoto N. Women’s empowerment and choice of contraceptive methods in selected African countries. Int Perspect Sex Reprod Health. 2012;38(1):23–33. doi: 10.1363/3802312. [DOI] [PubMed] [Google Scholar]
- Duncan DT, Kapadia F, Halkitis PN. Examination of spatial polygamy among young gay, bisexual, and other men who have sex with men in New York City: the P18 cohort study. Int J Environ Res Public Health. 2014;11(9):8962–8983. doi: 10.3390/ijerph110908962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin SL, Ehrhardt AA. Going beyond “ABC” to include “GEM”: critical reflections on progress in the HIV/AIDS epidemic. Am J Public Health. 2007;97(1):13–18. doi: 10.2105/AJPH.2005.074591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton LA, Driffin DD, Bauermeister JA, Smith H, Conway-Washington C. Minimal awareness and stalled uptake of Pre-Exposure Prophylaxis (PrEP) among at risk, HIV-negative, black men who have sex with men. AIDS Patient Care STDs. 2015;29:423–30. doi: 10.1089/apc.2014.0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easton D, Iverson E, Cribbin M, Wilson E, Weiss G Community Intervention Trial For Youth G. Space: the new frontier in HIV prevention for young men who have sex with men. AIDS Educ Prev. 2007;19(6):465–478. doi: 10.1521/aeap.2007.19.6.465. [DOI] [PubMed] [Google Scholar]
- Eberhart MG, Yehia BR, Hillier A, Voytek CD, Blank M, Frank I, Metzger DS, Brady KA. Behind the cascade: Analyzing spatial patterns along the HIV care continuum. J Acquir Immune Defic Syndr. 2013;64(Suppl 1):S42–51. doi: 10.1097/QAI.0b013e3182a90112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberhart MG, Yehia BR, Hillier A, Voytek CD, Fiore DJ, Blank M, … Brady KA. Individual and community factors associated with geographic clusters of poor HIV care retention and poor viral suppression. J Acquir Immune Defic Syndr. 2015;69(Suppl 1):S37–43. doi: 10.1097/QAI.0000000000000587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan JE, Frye V, Kurtz SP, Latkin C, Chen M, Tobin K, … Koblin BA. Migration, neighborhoods, and networks: approaches to understanding how urban environmental conditions affect syndemic adverse health outcomes among gay, bisexual and other men who have sex with men. AIDS Behav. 2011;15(Suppl 1):S35–50. doi: 10.1007/s10461-011-9902-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsyth AD, Valdiserri RO. A State-Level Analysis of Social and Structural Factors and HIV Outcomes Among Men Who Have Sex With Men in the United States. AIDS Educ Prev. 2015;27(6):493–504. doi: 10.1521/aeap.2015.27.6.493. [DOI] [PubMed] [Google Scholar]
- Fortenberry JD, Martinez J, Rudy BJ, Monte D Adolescent Trials Network for HIVAI. Linkage to care for HIV-positive adolescents: a multisite study of the adolescent medicine trials units of the adolescent trials network. J Adolesc Health. 2012;51(6):551–556. doi: 10.1016/j.jadohealth.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frew PM, Archibald M, Schamel J, Saint-Victor D, Fox E, Smith-Bankhead N, … del Rio C. An Integrated Service Delivery Model to Identify Persons Living with HIV and to Provide Linkage to HIV Treatment and Care in Prioritized Neighborhoods: A Geotargeted, Program Outcome Study. JMIR Public Health and Surveillance. 2015;1(2):e16. doi: 10.2196/publichealth.4675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye V, Egan JE, Van Tieu H, Cerda M, Ompad D, Koblin BA. “I didn’t think I could get out of the fucking park.” Gay men’s retrospective accounts of neighborhood space, emerging sexuality and migrations. Soc Sci Med. 2014;104:6–14. doi: 10.1016/j.socscimed.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye V, Koblin B, Chin J, Beard J, Blaney S, Halkitis P, … Galea S. Neighborhood-level correlates of consistent condom use among men who have sex with men: A multi-level analysis. AIDS and Behavior. 2010;14:974–985. doi: 10.1007/s10461-008-9438-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye V, Latka MH, Koblin B, Halkitis PN, Putnam S, Galea S, Vlahov D. The urban environment and sexual risk behavior among men who have sex with men. J Urban Health. 2006;83(2):308–324. doi: 10.1007/s11524-006-9033-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye V, Nandi V, Egan J, Cerda M, Greene E, Van Tieu H, … Koblin BA. Sexual orientation- and race-based discrimination and sexual HIV risk behavior among urban MSM. AIDS Behav. 2015;19(2):257–269. doi: 10.1007/s10461-014-0937-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geanuracos CG, Cunningham SD, Weiss G, Forte D, Reid LM, Ellen JM. Use of geographic information systems for planning HIV prevention interventions for high-risk youths. Am J Public Health. 2007;97(11):1974–1981. doi: 10.2105/AJPH.2005.076851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Breslow AS, Newcomb ME, Rosenberger JG, Bauermeister JA. Gay and bisexual men’s use of the internet: Research from the 1990s through 2013. J of Sex Research. 2014;51(4):390–409. doi: 10.1080/00224499.2013.871626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goswami ND, Schmitz MM, Sanchez T, Dasgupta S, Sullivan P, Cooper H, … Waller LA. Understanding Local Spatial Variation Along the Care Continuum: The Potential Impact of Transportation Vulnerability on HIV Linkage to Care and Viral Suppression in High-Poverty Areas, Atlanta, Georgia. J Acquir Immune Defic Syndr. 2016;72(1):65–72. doi: 10.1097/QAI.0000000000000914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet. 2008;372(9640):764–775. doi: 10.1016/S0140-6736(08)60887-9. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Moeller RW, Siconolfi DE, Storholm ED, Solomon TM, Bub KL. Measurement model exploring a syndemic in emerging adult gay and bisexual men. AIDS Behav. 2013;17(2):662–673. doi: 10.1007/s10461-012-0273-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall HI, Walker F, Shah D, Belle E. Trends in HIV diagnoses and testing among U.S. adolescents and young adults. AIDS Behav. 2012;16(1):36–43. doi: 10.1007/s10461-011-9944-8. [DOI] [PubMed] [Google Scholar]
- Harper GW, Schneider M. Oppression and discrimination among lesbian, gay, bisexual, and Transgendered people and communities: a challenge for community psychology. Am J Community Psychol. 2003;31(3–4):243–252. doi: 10.1023/a:1023906620085. [DOI] [PubMed] [Google Scholar]
- Hightow-Weidman LB, Jones K, Wohl AR, Futterman D, Outlaw A, Phillips G, 2nd … Group, Y. o. C. S. I. S. Early linkage and retention in care: findings from the outreach, linkage, and retention in care initiative among young men of color who have sex with men. AIDS Patient Care STDS. 2011;25(Suppl 1)(Suppl 1):S31–38. doi: 10.1089/apc.2011.9878. [DOI] [PubMed] [Google Scholar]
- Holtgrave DR, Kim JJ, Adkins C, Maulsby C, Lindsey KD, Johnson KM, … Kelley RT. Unmet HIV service needs among Black men who have sex with men in the United States. AIDS Behav. 2014;18(1):36–40. doi: 10.1007/s10461-013-0574-1. [DOI] [PubMed] [Google Scholar]
- Huebner DM, Kegeles SM, Rebchook GM, Peterson JL, Neilands TB, Johnson WD, Eke AN. Social oppression, psychological vulnerability, and unprotected intercourse among young Black men who have sex with men. Health Psychol. 2014;33(12):1568–1578. doi: 10.1037/hea0000031. [DOI] [PubMed] [Google Scholar]
- Jewkes R. Intimate partner violence: Causes and prevention. The Lancet. 2002;359(9315):1423–1429. doi: 10.1016/S0140-6736(02)08357-5. [DOI] [PubMed] [Google Scholar]
- Johns MM, Bauermeister JA, Zimmerman MA. Individual and Neighborhood Correlates of HIV testing among african american youth transitioning from adolescence into young adulthood. AIDS Educ Prev. 2010;22(6):509–522. doi: 10.1521/aeap.2010.22.6.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson A, Hall H, Hu X, Lansky A, Holtgrave D, Mermin J. Trends in diagnoses of HIV infection in the United States, 2002–2011. JAMA. 2014;312(4):432–434. doi: 10.1001/jama.2014.8534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson A, Hu X, Sharpe T, Dean H. Disparities in HIV/AIDS diagnoses among racial and ethnic minority youth. The Journal of Equity in Health. 2009;2(1):4–18. [Google Scholar]
- Johnston L, Longhurst R. Space, place, and sex: geographies of sexualities. Plymouth, United Kingdom: Rowman & Littlefield Publishers; 2010. [Google Scholar]
- Kahana SY, Fernandez MI, Wilson PA, Bauermeister JA, Lee S, Wilson CM, Hightow-Weidman LB. Rates and correlates of antiretroviral therapy use and virologic suppression among perinatally and behaviorally HIV-infected youth linked to care in the United States. J Acquir Immune Defic Syndr. 2015;68(2):169–177. doi: 10.1097/QAI.0000000000000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahana SY, Jenkins RA, Bruce D, Fernandez MI, Hightow-Weidman LB, Bauermeister JA Adolescent Medicine Trials Network. Structural Determinants of Antiretroviral Therapy Use, HIV Care Attendance, and Viral Suppression among Adolescents and Young Adults Living with HIV. PloS one. 2016;11(4):e0151106. doi: 10.1371/journal.pone.0151106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakietek J, Sullivan PS, Heffelfinger JD. You’ve got male: internet use, rural residence, and risky sex in men who have sex with men recruited in 12 U.S. cities. AIDS Educ Prev. 2011;23(2):118–127. doi: 10.1521/aeap.2011.23.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I. Social Cohesion and Health. In: Tarlov AR, St Peter RF, editors. The Society and Population Health Reader: A State and Community Perspective. New York: The New Press; 2000. pp. 57–74. [Google Scholar]
- Kawachi I, Daniels N, Robinson DE. Health disparities by race and class: why both matter. Health Aff (Millwood) 2005;24(2):343–352. doi: 10.1377/hlthaff.24.2.343. [DOI] [PubMed] [Google Scholar]
- Kelling GL, Coles CM. Fixing broken windows. Restoring order and reducng crime on our communities. New York: The Free Press; 1996. [Google Scholar]
- Kelly BC, Carpiano RM, Easterbrook A, Parsons JT. Sex and the community: the implications of neighbourhoods and social networks for sexual risk behaviours among urban gay men. Sociol Health Illn. 2012;34(7):1085–1102. doi: 10.1111/j.1467-9566.2011.01446.x. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Amirkhanian YA, Seal DW, Galletly CM, Difranceisco W, Glasman LR, … Rosado N. Levels and Predictors of Sexual HIV Risk in Social Networks of Men who Have Sex with Men in the Midwest. AIDS Educ Prev. 2010;22(6):483–495. doi: 10.1521/aeap.2010.22.6.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin BA, Egan JE, Nandi V, Sang JM, Cerda M, Tieu HV, Ompad DC, Hoober DR, Frye V. Congruence of home, social and sex neighborhoods among men who have sex with men, NYCM2M Study. J Urban Health. 2016 doi: 10.1007/s11524-016-0074-5. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin BA, Egan JE, Rundle A, Quinn J, Tieu HV, Cerda M, … Frye V. Methods to measure the impact of home, social, and sexual neighborhoods of urban gay, bisexual, and other men who have sex with men. PloS one. 2013;8(10):e75878. doi: 10.1371/journal.pone.0075878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C, Weeks M, Glasman L, Galletly C, Albarracin D. A dynamic social systems model for considering structural factors in HIV prevention and detection. AIDS Behav. 2011;14:222–238. doi: 10.1007/s10461-010-9804-y.A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, German D, Vlahov D, Galea S. Neighborhoods and HIV: a social ecological approach to prevention and care. Am Psychol. 2013;68(4):210–224. doi: 10.1037/a0032704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linton SL, Cooper HL, Luo R, Karnes C, Renneker K, Haley DF, … Wingood GM. Changing Places and Partners: Associations of Neighborhood Conditions With Sexual Network Turnover Among African American Adults Relocated From Public Housing. Archives of Sexual Behavior. 2016:1–12. doi: 10.1007/s10508-015-0687-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnus M, Kuo I, Phillips G, 2nd, Shelley K, Rawls A, Montanez L, … Greenberg AE. Elevated HIV prevalence despite lower rates of sexual risk behaviors among black men in the District of Columbia who have sex with men. AIDS Patient Care STDS. 2010;24(10):615–622. doi: 10.1089/apc.2010.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metheny N, Stephenson R. Disclosure of Sexual Orientation and Uptake of HIV Testing and Hepatitis Vaccination for Rural Men Who Have Sex With Men. Ann Fam Med. 2016;14(2):155–158. doi: 10.1370/afm.1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller RL, Janulis PF, Reed SJ, Harper GW, Ellen J, Boyer CB Adolescent Trials Network. Creating Youth-Supportive Communities: Outcomes from the Connect-to-Protect(R) (C2P) Structural Change Approach to Youth HIV Prevention. J Youth Adolesc. 2016;45(2):301–315. doi: 10.1007/s10964-015-0379-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millett GA, Ding H, Marks G, Jeffries WLt, Bingham T, Lauby J, … Stueve A. Mistaken assumptions and missed opportunities: correlates of undiagnosed HIV infection among black and Latino men who have sex with men. J Acquir Immune Defic Syndr. 2011;58(1):64–71. doi: 10.1097/QAI.0b013e31822542ad. [DOI] [PubMed] [Google Scholar]
- Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21(15):2083–2091. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WLt, Wilson PA, … Remis RS. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–348. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: a critical literature review. Am J Public Health. 2006;96(6):1007–1019. doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muessig KE, Nekkanti M, Bauermeister JA, Bull S, Hightow-Weidman LB. A systematic review of recent smartphone, internet, and web 2.0 interventions to address the HIV continuum of care. Current HIV/AIDS Reports. 2015;12(1):173–190. doi: 10.1007/s11904-014-0239-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Birkett M, Kuhns LM, Latkin CA, Muth SQ. The Role of Geographic and Network Factors in Racial Disparities in HIV Among Young Men Who have Sex with Men: An Egocentric Network Study. AIDS Behav. 2015;19(6):1037–1047. doi: 10.1007/s10461-014-0955-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48(2–3):218–253. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanda G, Schuler SR, Lenzi R. The influence of gender attitudes on contraceptive use in Tanzania: new evidence using husbands’ and wives’ survey data. J Biosoc Sci. 2013;45(3):331–344. doi: 10.1017/S0021932012000855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson LE, Walker JJ, DuBois SN, Giwa S. Your blues ain’t like mine: considering integrative antiracism in HIV prevention research with black men who have sex with men in Canada and the United States. Nurs Inq. 2014;21(4):270–282. doi: 10.1111/nin.12055. [DOI] [PubMed] [Google Scholar]
- Ohl ME, Perencevich E. Frequency of human immunodeficiency virus (HIV) testing in urban vs. rural areas of the Untied States: Results from a nationally-representative sample. BMC public health. 2011;11:681. doi: 10.1186/1471-2458-11-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldenburg CE, Perez-Brumer AG, Reisner SL, Mimiaga MJ. Transactional Sex and the HIV Epidemic Among Men Who have Sex with Men (MSM): Results From a Systematic Review and Meta-analysis. AIDS Behav. 2015;19(12):2177–2183. doi: 10.1007/s10461-015-1010-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oster AM, Wiegand RE, Sionean C, Miles IJ, Thomas PE, Melendez-Morales L, … Millett GA. Understanding disparities in HIV infection between black and white MSM in the United States. AIDS. 2011;25(8):1103–1112. doi: 10.1097/QAD.0b013e3283471efa. [DOI] [PubMed] [Google Scholar]
- Parker R. Sexuality, culture, and power in HIV/AIDS research. Annual Review of Anthropology. 2001;30:163–179. doi: 10.1146/annurev.anthro.30.1.163. [DOI] [Google Scholar]
- Parker RG, Easton D, Klein CH. Structural barriers and facilitators in HIV prevention: a review of international research. AIDS. 2000;14(Suppl 1):S22–32. doi: 10.1097/00002030-200006001-00004. [DOI] [PubMed] [Google Scholar]
- Philbin MM, Tanner AE, DuVal A, Ellen JM, Xu J, Kapogiannis B … Adolescent Trials Network. Factors affecting linkage to care and engagement in care for newly diagnosed HIV-positive adolescents within fifteen adolescent medicine clinics in the United States. AIDS Behav. 2014;18(8):1501–1510. doi: 10.1007/s10461-013-0650-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips G, II, Birkett M, Kuhns L, Hatchel T, Garofalo R, Mustanski B. Neighborhood-Level Associations with HIV Infection Among Young Men Who Have Sex with Men in Chicago. Archives of Sexual Behavior. 2015;44(7):1773–1786. doi: 10.1007/s10508-014-0459-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez-Valles J. The protective effects of community involvement for HIV risk behavior: a conceptual framework. Health Educ Res. 2002;17(4):389–403. doi: 10.1093/her/17.4.389. [DOI] [PubMed] [Google Scholar]
- Ramirez-Valles J, Kuhns LM, Campbell RT, Diaz RM. Social integration and health: community involvement, stigmatized identities, and sexual risk in Latino sexual minorities. J Health Soc Behav. 2010;51(1):30–47. doi: 10.1177/0022146509361176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymond HF, Chen YH, Syme SL, Catalano R, Hutson MA, McFarland W. The role of individual and neighborhood factors: HIV acquisition risk among high-risk populations in San Francisco. AIDS and Behavior. 2014a;18:346–356. doi: 10.1007/s10461-013-0508-y. [DOI] [PubMed] [Google Scholar]
- Rothenberg R, Muth SQ, Malone S, Potterat JJ, Woodhouse DE. Social and geographic distance in HIV risk. Sex Transm Dis. 2005;32(8):506–512. doi: 10.1097/01.olq.0000161191.12026.ca. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Sanchez TH, Sineath RC, Kahle EM, Tregear SJ, Sullivan PS. The Annual American Men’s Internet Survey of Behaviors of Men Who Have Sex With Men in the United States: Protocol and Key Indicators Report 2013. JMIR Public Health and Surveillance. 2016;2(1):e3. doi: 10.2196/publichealth.5476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider JA, Cornwell B, Ostrow D, Michaels S, Schumm P, Laumann EO, Friedman S. Network mixing and network influences most linked to HIV infection and risk behavior in the HIV epidemic among black men who have sex with men. Am J Public Health. 2013;103(1):e28–36. doi: 10.2105/AJPH.2012.301003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpe TT, Stallworth JM, Miller KS, Dean HD, Fenton K. HIV/AIDS and ethnic and racial minority youth: Current issues. The Journal of Equity in Health. 2009;2:1–3. [Google Scholar]
- Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, … Peterson JL. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Annals of epidemiology. 2015;25(6):445–454. doi: 10.1016/j.annepidem.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surratt HL, Kurtz SP, Levi-Minzi MA, Chen M. Environmental Influences on HIV Medication Adherence: The Role of Neighborhood Disorder. Am J Public Health. 2015;105(8):1660–1666. doi: 10.2105/AJPH.2015.302612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin KE, Latkin CA, Curriero FC. An examination of places where African American men who have sex with men (MSM) use drugs/drink alcohol: a focus on social and spatial characteristics. Int J Drug Policy. 2014;25(3):591–597. doi: 10.1016/j.drugpo.2013.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarruel AM, Guilamo-Ramos V, Bauermeister J. HIV Prevention with Latinos: Theory, Research, and Practice. Oxford University Press; 2012. Reducing HIV Sexual Risk for Latino Adolescents. [Google Scholar]
- Wejnert C, Le B, Rose CE, Oster AM, Smith AJ, Zhu J Gabriela Paz-Bailey for the NSG. HIV infection and awareness among men who have sex with men-20 cities, United States, 2008 and 2011. PloS one. 2013;8(10):e76878. doi: 10.1371/journal.pone.0076878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White House. National HIV/AIDS Strategy for the United States. Washington D.C: 2010. [Google Scholar]
- Wiewel E, Bocour A, Kersanske L, Bodach S, Xia Q, Braunstein S. The Association Between Neighborhood Poverty and HIV Diagnoses Among Males and Females in New York City, 2010–2011. Public health reports (Washington, DC: 1974) 2015;131(2):290–302. doi: 10.1177/003335491613100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Jackson PB. Social sources of racial disparities in health. Health Affairs. 2005;24(2):325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]