Abstract
Cancer from the gastrointestinal tract and its associated excretory organs will occur in over 300,000 Americans in 2017, with colorectal cancer responsible for over forty percent of that burden; there will be over 150,000 deaths from this group of cancers in the same time period. Disparities among subgroups related to these cancers’ incidence and mortality exist. The epidemiology and risk factors associated with each cancer bear out differences for racial groups in the United States. Esophageal adenocarcinoma is more frequent in Non-Hispanic Whites, whereas esophageal squamous cell carcinoma with risk factors of tobacco and alcohol is more frequent among Blacks. Liver cancer has been most frequent among Asian/Pacific Islanders chiefly due to hepatitis B vertical transmission, but other racial groups show increasing rates due to hepatitis C and emergence of cirrhosis from non-alcoholic fatty liver disease. Gastric cancer incidence remains highest among Asian/Pacific Islanders likely due to gene-environment interaction. In addition to esophageal squamous cell carcinoma, cancers of the small bowel, pancreas and colorectum show the highest rates among Blacks, where the explanations for the disparity are not as obvious and are likely multifactorial, including socio-economic and health care access, treatment and prevention (vaccination and screening) differences, dietary and composition of the gut microbiome, as well as biological and genetic influences. Cognizance of these disparities in gastrointestinal cancer risk, as well as approaches that apply precision medicine methods to populations with the increased risk, may reduce the observed disparities for digestive cancers.
Keywords: cancer disparity, racial disparity, cancer epidemiology, cancer risk, African American, esophageal cancer, small bowel cancer, gastric cancer, hepatocellular carcinoma, colorectal cancer, anal cancer, pancreatic cancer
INTRODUCTION
The incidence and mortality from gastrointestinal (GI) cancers highlight health disparities for specific populations. For instance, it is well known that native Asians from specific countries have a high incidence of gastric cancer. However, their immigrant counterparts in the U.S. show a different incidence, likely due to changes in environmental influences from a new geographical location [1]. Another example is colorectal cancer (CRC); whereas native Africans have a very low incidence of this disease, African Americans portray a much higher one, and are at the highest incidence among U.S. racial/ethnic groups [2]. Immigrant populations to the U.S. have shown changes in GI cancer risk from their country of origin generally within 1–2 generations, suggesting that gene-environment interations are at play. Many GI cancers present with higher risk within Westernized countries, and the observed risk is suggested to originate from the more abundant availability of calories, red meat and fat, and subsequent interaction with the gut microbiome [3,4]. Genetically-susceptible populations might not demonstrate risk for GI cancers until a switch from legume and grain diets to the Westernized high caloric diets [5]. Other GI cancers, such as gastric cancer, are at high incidence in specific countries but low risk in the U.S., in part due to an evironment with low H. pylori prevalence [6]. Within the U.S., fundamental causes of health inequalities including socio-economic factors, insurance status, access to healthcare, screening and treatment biases are additional issues that contribute to GI cancer disparities [7]. Understanding the differential effects of cancer epidemiology among U.S. populations as they pertain to GI cancers is the focus of the present review. Because cancer data is more complete for Non-Hispanic Whites and Blacks in the U.S. than other racial/ethnic groups, this article emphasizes these two populations (Figure 1), although key data for Hispanic, Asian/Pacific Islander, and American Indian/Alaskan natives are also presented.
Figure 1.
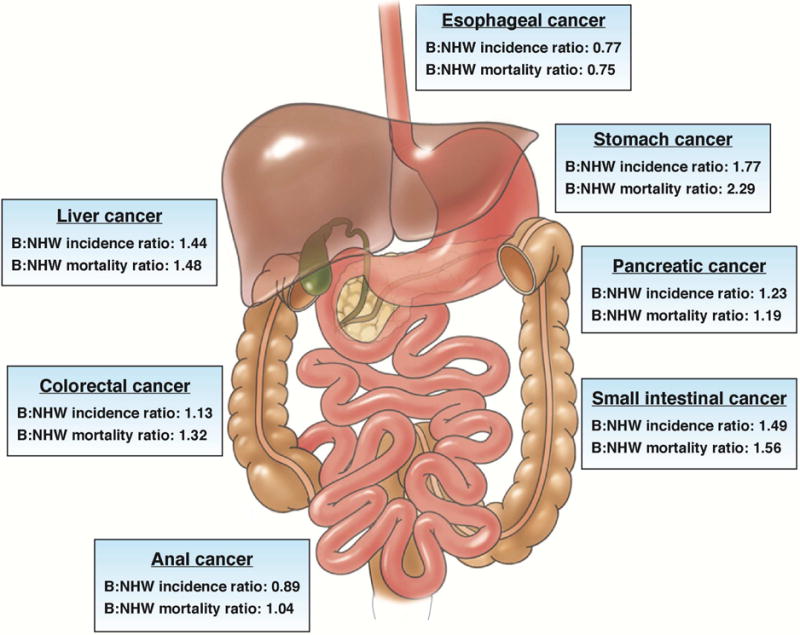
Black:Non-Hispanic White (NHW) ratios for seven gastrointestinal track cancers, both genders, for 2014. Data derived from seer.cancer.gov. Note the higher incidence and mortality ratio for NHWs for esophageal cancer, and same incidence and mortality ratio for both Blacks and NHWs for anal cancer. All other cancers show higher incidence and mortality ratios for Blacks as compared to NHWs. In some cases, the mortality ratio is more excessive than the incidence ratio for Blacks, including that for stomach, colorectal, and small intestinal cancer.
For 2017, GI cancers occurred in 310,440 people in the U.S., of which over 40 percent is CRC with 135,430 new cases. Similarly, death from CRC (50,260 people) is one-third of all GI cancer mortality (157,700 people) (Table 1) [8]. The overall number of GI cancers by each race is not entirely known, as some GI cancers are not broken down in datasets in this fashion. Among specific GI cancers, CRC is being closely monitored by the Centers for Disease Control (CDC) Health Disparity and Inequality Report (CHDIR), given that it is the GI cancer with the highest incidence and mortality, and it is potentially preventable [9]. In this manuscript, we pay particular attention to CRC disparities, even though other GI cancers also have important disparities that we highlight in each of the sections. Along with age and family history, common GI cancer risk factors include: smoking, excessive alcohol consumption, diet high in animal fat, obesity and genetic predisposition. Viruses also play key etiological factors for some GI cancers such as hepatocellular and anal cancers. How these risk factors lead to different outcomes in different populations remains to be further elucidated and is the subject of current research. Here, we highlight the epidemiology, risk factors, and approaches that might reduce cancer disparities for seven GI cancers. A comprehensive review of GI cancer disparities has not been published and is critical to identify knowledge gaps that should be addressed in order to optimize efforts to reduce disparities in the US.
Table 1.
Estimated new gastrointestinal cancer cases and deaths by gender, for all races and Blacks in the United States for 2017.
| Cancer | Overall Incidence | Male Incidence | Female Incidence | Black Male Incidence | Black Female Incidence | Overall Deaths | Black Male Deaths | Black Female Deaths |
|---|---|---|---|---|---|---|---|---|
| Esophageal* | 16,940 | 13,360 | 3,550 | 15,690 | 920 | |||
| Stomach | 28,000 | 17,750 | 10,250 | 10,960 | 1,160 | |||
| Small Intestine | 10,190 | 5,380 | 4,810 | 1,390 | ||||
| Pancreas | 53,670 | 27,970 | 25,700 | 3,230 | 3,490 | 43,090 | 2,390 | 2,550 |
| Liver and Intrahepatic Duct | 40,710 | 29,200 | 11,510 | 4,250 | 28,920 | 2,880 | 1,020 | |
| Gallbladder and Other Biliary | 11,740 | 5,320 | 6,420 | 3,830 | ||||
| Colorectal | 135,430 | 71,420 | 64,010 | 8,690 | 8,550 | 50,260 | 3,800 | 3,230 |
| Anus | 8,200 | 2,950 | 5,250 | 1,100 | ||||
| Other Digestive Organs | 5,560 | 2,300 | 3,260 | 2,460 | ||||
| Total Digestive System | 310,440 | 175,650 | 134,790 | 157,700 |
Data derived from Siegel RL, Miller KD, Jemal A. CA Cancer J Clin. 2017;67:7–30 and DeSantis CE, Siegel RL. Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, Jemal A. CA Cancer J Clin 2016;66:290–308. Blank cells are due to unobtainable data.
Includes adenocarcinoma and squamous cell carcinoma.
Esophageal Cancer
In 2017, there were 16,940 new cases and 15,690 deaths from esophageal cancer in the U.S. (Table 1). There are 2 primary histological sub-types of esophageal cancer: adenocarcinoma and squamous cell carcinoma (SCC). While SCC is the most common sub-type worldwide especially in East Asia, Africa and Southern Europe, esophageal adenocarcinoma is the most common sub-type in the U.S. and Northern Europe [10,11]. Of all esophageal cancers in the U.S., adenocarcinoma accounts for nearly 60%, while SCC accounts for about 34%, the remaining 6% are of other histological sub-types [12]. Overall, 5-year survival for all esophageal cancer sub-types is only 18% due to advanced disease often at presentation (Table 2). Males are about 3 times more likely to develop espophageal cancer than females (Table 3).
Table 2.
Stage distribution and 5-year survival of selected gastrointestinal cancers by race for 2006–2012.
| Cancer | Distribution for Localized Disease | Distribution for Regional Disease | Distribution for Distant Disease | 5-Year Survival Localized Disease | 5-Year Survival Regional Disease | 5-Year Survival Distant Disease | All Stage 5-Year Survival |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Esophageal* | White:20% | 31% | 38% | 44% | 24% | 5% | 19% |
| Black:18% | 31% | 40% | 22% | 17% | 4% | 12% | |
| All:20% | 31% | 38% | 41% | 23% | 5% | 18% | |
|
| |||||||
| Liver and Intrahepatic Duct | White:43% | 27% | 18% | 30% | 11% | 3% | 17% |
| Black:42% | 28% | 20% | 24% | 7% | 2% | 13% | |
| All:43% | 27% | 18% | 31% | 11% | 3% | 18% | |
|
| |||||||
| Pancreas | White:9% | 29% | 52% | 29% | 11% | 3% | 8% |
| Black:10% | 26% | 57% | 26% | 11% | 2% | 7% | |
| All:9% | 29% | 52% | 29% | 11% | 3% | 8% | |
|
| |||||||
| Colorectal | White:39% | 36% | 20% | 91% | 72% | 14% | 66% |
| Black:38% | 32% | 25% | 87% | 65% | 10% | 58% | |
| All:39% | 35% | 21% | 90% | 71% | 14% | 65% | |
Data derived from Siegel RL, Miller KD, Jemal A. CA Cancer J Clin. 2017;67:7–30. ‘All’ refers to all races assessed, including White, Black, Asian/Pacific Islander, American Indian/Alaskan Native, and Hispanic.
Includes adenocarcinoma and squamous cell carcinoma.
Table 3.
Gender-based incidence and mortality rate ratios per 100,000 (adjusted to the 2000 U.S. standard population) for selected gastrointestinal cancers for 2010–2014, with comparing Blacks to Non-Hispanic Whites (NHWs).
| Cancer | All Races | Asian/Paci fic Islander | American Indian/Ala skan | Hispanic | Black | NH White | Absolute Difference (Black-NHW) | Black:NHW Rate ratio |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Esophageal* | ||||||||
| Incidence | M:7.3 | 3.5 | 5.1 | 5.1 | 6.9 | 8.2 | −1.3 | 0.84 |
| F:1.7 | 0.8 | 1.4 | 1.1 | 2.3 | 1.8 | +0.5 | 1.28 | |
| Mortality | M:7.3 | 2.9 | 4.2 | 4.2 | 6.3 | 8.0 | −1.7 | 0.79 |
| F:1.5 | 0.7 | 1.1 | 0.8 | 1.9 | 1.6 | +0.3 | 1.19 | |
|
| ||||||||
| Stomach | ||||||||
| Incidence | M:9.9 | 14.0 | 13.7 | 13.5 | 13.6 | 8.2 | +5.4 | 1.66 |
| F:5.2 | 8.0 | 8.1 | 8.8 | 7.8 | 3.7 | +4.1 | 2.11 | |
| Mortality | M:4.4 | 7.1 | 4.9 | 3.4 | 8.6 | 3.4 | +5.2 | 2.53 |
| F:2.3 | 4.3 | 2.5 | 1.7 | 4.1 | 1.7 | +2.4 | 2.41 | |
|
| ||||||||
| Small Intestine | ||||||||
| Incidence | M:2.6 | 1.3 | 1.5 | 1.9 | 4.3 | 2.8 | +1.5 | 1.54 |
| F:2.0 | 0.9 | – | 1.5 | 3.4 | 2.1 | +1.3 | 1.62 | |
| Mortality | M:0.5 | 0.3 | – | 0.3 | 0.7 | 0.5 | +0.2 | 1.40 |
| F:0.3 | 0.2 | – | 0.2 | 0.5 | 0.3 | +0.2 | 1.67 | |
|
| ||||||||
| Liver and Intrahepatic Duct | ||||||||
| Incidence | M:13.3 | 20.2 | 18.7 | 20.6 | 16.7 | 10.4 | +4.3 | 1.61 |
| F:4.6 | 7.6 | 8.6 | 7.9 | 5.0 | 3.5 | +1.5 | 1.43 | |
| Mortality | M:9.2 | 14. | 10.1 | 13.8 | 13.0 | 8.0 | +5.0 | 1.63 |
| F:3.7 | 6.1 | 4.7 | 6.1 | 4.5 | 3.3 | +1.2 | 1.36 | |
|
| ||||||||
| Pancreas | ||||||||
| Incidence | M:14.2 | 11.0 | 11.1 | 12.3 | 17.0 | 14.6 | +2.4 | 1.16 |
| F:11.1 | 9.2 | 8.3 | 10.8 | 14.3 | 11.0 | +3.3 | 1.30 | |
| Mortality | M:12.6 | 8.2 | 7.1 | 10.0 | 15.0 | 12.8 | +2.2 | 1.17 |
| F:9.5 | 7.3 | 6.0 | 8.1 | 12.1 | 9.5 | +2.6 | 1.27 | |
|
| ||||||||
| Colorectal | ||||||||
| Incidence | M:46.0 | 40.2 | 45.5 | 41.5 | 56.4 | 45.9 | +10.5 | 1.23 |
| F:35.1 | 28.8 | 37.5 | 29.9 | 43.2 | 35.3 | +7.9 | 1.22 | |
| Mortality | M:17.7 | 12.4 | 14.0 | 15.8 | 25.3 | 17.3 | +8.0 | 1.46 |
| F:12.4 | 8.8 | 10.0 | 9.7 | 16.5 | 12.3 | +4.2 | 1.34 | |
|
| ||||||||
| Anal Cancer | ||||||||
| Incidence | M:1.5 | 0.5 | – | 0.9 | 2.2 | 1.6 | +0.6 | 1.38 |
| F:2.1 | 0.5 | 1.2 | 1.5 | 1.8 | 2.2 | −0.4 | 0.82 | |
| Mortality | M:0.2 | 0.1 | – | 0.1 | 0.3 | 0.2 | +0.1 | 1.50 |
| F:0.3 | 0.1 | – | 0.2 | 0.2 | 0.3 | −0.1 | 0.67 | |
Data derived seer.cancer.gov. ‘M’ = male; ‘F’ = female; NH = Non-Hispanic; ‘–‘ = number of cases too small to estimate ratios.
Includes adenocarcinoma and squamous cell carcinoma. For Black:NHW rate ratios, a ratio of “1” means that the Black rate and NHW rates are equal, and rates >1.0 means that Blacks have higher rates than NHWs, and rates <1.0 means NHWs have higher rates than Blacks.
Among racial and ethnic groups in the US, there are differences in the distribution of histological sub-types of esophageal cancer. In non-Hispanic Whites (NHWs), adenocarcinoma accounts for nearly 68% of esophageal cancers, whereas this sub-type accounts for only 15% of cases in Blacks. Conversely, while SCC accounts for 26% of esophageal cancer cases in NHWs, it accounts for 80% of cases in Blacks. Among Hispanics, the rates of SCC and adenocarcinoma are 41% and 53%, respectively [12]. Considering all esophageal cancer sub-types, Blacks are more likely to present with later stage disease [13] and have poor outcomes [14].
Reasons for differences in incidence by race/ethnicity are likely explained by different risk factors for each sub-type. Primary risk factors for SCC are alcohol and tobacco use [11,15]. Among Asians, variants in genes involved in alcohol metabolism confer increased risk of SCC [10]. A case-control study found that tobacco and alcohol use accounted for 94% of the difference in esophageal cancer annual incidence rates [16]. An epidemiological study suggested that population-specific screening and prevention programs are warranted for esophageal SCC in Black men exposed to alcohol and tobacco given that rates of SCC approached those for esophageal adenocarcinoma in NHW men with reflux disease, a group in whom screening is advocated [17]. A number of genome-wide association studies (GWAS) of esophageal SCC have been performed in Asian populations and identified functional variants in alcohol metabolizing genes, ALDH2 and ADH1B, that, when combined with lifestyle factors, significantly increase risk of SCC [18]. These genetic risk variants are only found in East Asian populations [19]. Moreover, variants in PLCE1 [20,21] were associated with SCC in 2 GWAS evaluations, and the allele frequencies of these variants are similar across populations [19], but have not been studied as risk factors in non-Asian populations.
Risk factors for esophageal adenocarcinoma include age, male gender, gastroesophageal reflux disease (GERD) especially erosive esophagitis, Barrett’s esophagus, obesity and tobacco use [11]. Non-steroidal anti-inflammatory drugs’ usage and H. pylori infection are protective against adenocarcinoma [11]. Regarding race/ethnicity, NHW men have the highest risk of esophageal adenocarcinoma and represent a group in which the American Gastroenterological Association (AGA) recommends consideration for endoscopic screening for Barrett’s esophagus on an individual basis, if multiple risk factors are present [22]. Reasons for increased risk in NHWs compared with Blacks could be due to higher rates of erosive esophagitis [23] and Barrett’s esophagus [24] in NHWs and/or decreased rates of H. pylori infection in Blacks [25]. GWAS for Barrett’s esophagus and esophageal adenocarcinoma in individuals of European descent have identified a number of genetic variants in CRTC1, BARX1, FOXP1, GDF7, TBX5 and HLA [26–28]. The risk variant in CRTC1 [26] has 30% higher allele frequency in European Americans compared with Blacks [29]; however, the other GWAS variants do not have large allele frequency differences or have higher frequency of the risk allele in Blacks and would not explain differences in risk between populations. Additional work is needed to understand the contribution of genetic variants in addition to known environmental risk factors for adenocarcinoma in Whites compared with other US populations.
Gastric cancer
Gastric cancer is the fourth most common malignancy in the world, after lung, breast and colorectal cancers, with about 75% of cases in Asia, predominantly in China [30,31]. Globally, gastric cancer rates in females are nearly half those encountered in males. It is worth noting, however, that while the incidence in females is lower than in males, the prognosis in females is generally poor (presenting with 8% and 13% more poorly-differentiated gastric cancer and signet ring carcinoma over males, respectively) and the age of onset is lower (55.0 years of age in females vs 57.9 years of age in males) [32].
Within the U.S., 28,000 new gastric cancer cases will be diagnosed in 2017 with 17,750 cases in males and 10,250 in females (Table 1). Incidence and death rates by race/ethnicity differ. During 2010–2014, Asian/Pacific Islander males displayed the highest incidence and mortality when compared to all other groups and genders, with 14.0 new cases/100,000 and 7.1 deaths per 100,000 (Table 3). Blacks developed gastric cancer at nearly the same rate as Asian/Pacific Islanders (Table 3). Hispanic females topped Asian/Pacific Islander females for the highest incidence, while in the same time period, NHW females have the lowest incidence (3.7/100,000) and mortality (1.7/100,000) rates. A direct comparison of such values for Black vs. NHW males revealed an absolute difference of +5.4 and +5.2 for incidence and mortality that translate into ratios of 1.66 and 2.53, respectively (Table 3). A similar pattern was observed when comparing these values for Black vs. NHW females where the absolute differences and ratios for incidence were +4.1 and 2.11, respectively, for mortality these values were +2.4 and 2.41, respectively (Table 3). U.S. population studies confirm that racial/ethnic minorities have a 40%–50% increase in risk of gastric cancer over NHWs, with race as an independent risk factor [25]. These differences highlight health disparities for which the contributing risk factors need to be investigated.
Risk factors differ between non-cardia and cardia gastric cancers. H. pylori infection is the primary risk factor for non-cardia cancer. H. pylori infection rates remain high in both Blacks and Hispanics [6]. This persistent high prevalence likely contributes to the Black and Hispanic high incidence and mortality from gastric cancer (Table 3). Non-cardia gastric cancer is associated with patient low socioeconomic status (SES) where general living conditions might be conducive to higher H. pylori infection and dissemination. While many studies have advocated eradication of H. pylori to reduce non-cardia gastric cancer incidence, strong evidence for this approach is still lacking [33]. Cardia gastric cancer tends to be encountered in patients with higher SES and associates strongly with smoking and obesity. Smoking is also a factor in non-cardia cancers, but its effect is relatively minor when compared to H. pylori infection. Diets rich in fruit and vegetables are suggested to have protective effects against gastric cancer while higher BMI is suggested to be a risk factor for cardia gastric cancer. Among Asians, low penetrance genetic variants in PSCA, PLCE1, PRKAA1 and MUC1 increase risk for gastric cancer and among Europeans, loss of function of ATM increases gastric cancer risk [34–36]. Inactivating mutations in the E-Cadherin gene (CDH1) leads to hereditary diffuse gastric cancer syndrome in a small fraction of individuals. This same gene is the target of inactivation through methylation in the presence of H. pylori infection [37]. Lynch syndrome and other patients with specific polyposis syndromes are also at high risk for gastric cancer.
Overall, a decrease or cessation of tobacco use, a balanced diet with more fruits and vegetables, reduction in obesity, and better monitoring of H. pylori infection could lower gastric cancer disparities within the U.S. population and lead to a lower burden of the disease especially in minority populations, such as Blacks and Hispanics. While screening programs for gastric cancer exist in high prevalence regions and have been shown to reduce gastric cancer mortality, screening in a low prevalence country like the US is debated. Based on higher incidence of gastric cancer among racial and ethnic minorities in the US, targeted screening programs should be considered.
Pancreatic cancer
In the U.S., Black men and women have the highest incidences of pancreatic cancer at 17.0 and 15.0/100,000 persons, respectively (Table 3). NHW and Hispanic women have incidences of 12.8 and 10.0/100,000, respectively, while it is higher in NHW men compared with Hispanic men: 14.6 vs. 12.3/100,000, respectively. In addition to their highest incidence, Blacks also have the worst pancreatic cancer prognosis of all U.S. populations (Table 2) [38] with more advanced stage and more non-resectable disease at presentation as well as less surgical treatment [39]. Pancreatic adenocarcinoma remains one of the most deadly cancers. The 5-year survival is a dismal 8% (Table 2). In 2017, it is estimated that there will be 53,670 cases and 43,090 deaths (Table 1). Most pancreatic adenocarcinomas present at an advanced stage likely accounting for poor survival rates.
Risk factors for pancreatic adenocarcinoma include genetic and non-genetic factors. Clustering of pancreatic cancer in families increases an individual’s risk up to 32-fold [40]. Hereditary syndromes (such as those due to germline mutations in STK11, BRCA1/2, PALB2, CDKN2A, and DNA repair genes) significantly increase pancreatic cancer risk, especially with family history of pancreatic cancer in a first-degree relative [41]. There is no data on differences in pancreatic cancer risk by race/ethnicity in these high-risk syndromes. GWAS studies have identified 16 chromosomal loci with significant associations with pancreatic cancer [42,43]. These studies have included only a modest number of Blacks [44,45]) limiting evaluation of associations in this high-risk population.
Non-genetic risk factors for pancreatic adenocarcinoma include tobacco use, diabetes, obesity and chronic pancreatitis [46,47]. A case-control study [48] found that tobacco use, diabetes and family history accounted for 46% of pancreatic cancer risk in Black men compared with 37% risk in White men. Among women, heavy alcohol use and elevated BMI accounted for most of the excess risk among Black women compared with White women. In contrast, a study using data from the prospective American Cancer Society Cancer Prevention Study [49] did not replicate these findings and concluded that known risk factors do not account for racial disparities in pancreatic cancer. Thus, the contribution of non-genetic risk factors to racial disparities is still unclear and additional studies are warranted. Addressing pancreatic cancer disparities is a challenge given that clinical presentation occurs late in the disease course and there are no established screening recommendations. Clearly, additional work in biomarker development and screening modalities is needed to address the overall cancer burden as well as disparities.
Small bowel cancer
Cancers of the small intestine are rare, accounting for only 0.5% of cancers and 1–2% of gastrointestinal neoplasms [8]. There are several types of small bowel cancers including neuroendocrine tumors (e.g., carcinoid), adenocarcinoma, lymphoma and sarcoma (e.g., gastrointestinal stromal tumor or GIST). In 2017, it is estimated that there will be 10,190 cases and 1,390 deaths from small bowel cancer in the US, with increasing incidence over time (Table 1). Five-year survival is 66.9% for all small bowel cancers. Overall, adenocarcinoma is the most common followed by carcinoid tumors [50].
In the US, Blacks have the highest incidence of small bowel cancers with an incidence of 3.4 and 4.3/100,000 for Black women and men, respectively [12]. The most common sub-types in Blacks are carcinoids and adenocarcinoma. The rates of small bowel cancer for NHW women and men are 2.1 and 2.8/100,000, while Hispanics and Asian/Pacific Islanders have even lower incidences for both genders (Table 3). Notably, small bowel GIST tumors show highest incidence among Asian/Pacific Islanders [51]. However, when considering GIST tumors in any part of the gastrointestinal tract, Blacks have highest incidence of all populations [52,53].
There are several known risk factors for small bowel adenocarcinoma including familial adenomatous polyposis (especially in the duodenum), Lynch syndrome, Peutz-Jeghers syndrome, juvenile polyposis syndrome, Crohn’s disease and celiac disease [54]. Given the rarity of small bowel adenocarcinoma in general, it is not known the extent to which these risk factors impact differences among races. It is unlikely, however, that celiac disease is a significant risk factor in Blacks given its low incidence in this population [55,56]. For small bowel neuroendocrine tumors, GWAS evaluations have identified risk variants upstream of ELK3, though the impact of these variants by race is not known [57]. Additional risks for neuroendocrine tumors include family history, BMI, diabetes and tobacco [58]. The extent to which these factors account for racial differences has not been established. As is the case in pancreatic cancer, there are no screening strategies for small bowel cancer given its low incidence. Evaluation of symptoms especially in at-risk populations is the only strategy currently employed.
Colorectal cancer
CRC is the third most common cancer worldwide, one of the leading causes of cancer-related deaths, and among the best studied GI cancers due to access to precursor lesions [4,59,60]. It is more common among Westernized nations than in other parts of the world. It is a multifactorial disease where genetics, epigenetics, diet, lifestyle and environment have been cited as risk factors. Heritable forms of CRC such as familial adenomatous polyposis and Lynch syndrome account for <5%, with another ~25% clustering in families suggestive of weaker Mendelian genetic inheritance [61,62]; however, the vast majority of CRCs are sporadic. Screening and surveillance guidelines for CRC include age and heritable components based on family history or an identified or suspected high risk syndrome that change the age and frequency for screening according to published guidelines. Guidelines previously did not include race as a factor even though there is evidence that this engenders increase risk for CRC [4,63]; however the 2017 U.S. Multisociety Task Force on Colorectal Cancer has concluded that race is a determinant that may lower the initial screening age [64]. In the CHDIR report [9], the CDC has concluded that CRC should be closely monitored in the population as it is common and exhibits large disparities, but is potentially preventable. Successful screening programs can greatly reduce current racial disparities for CRC incidence [65–69]. In 2017, there were 135,430 new cases that were relatively equally distributed between males (71,420) and females (64,010) in the U.S. population, as well as between males and females among Blacks (8,690 and 8,550, respectively) (Table 1). Overall CRC incidence has fallen since the mid-1980s for unclear reasons initially; further decrease has been accelerated with the implementation of national screening efforts in the U.S. [8]. However, the rate is on the rise for younger Americans and more so in young Blacks [70–72].
The overall number of deaths expected from CRC in 2017 is 50,260, demonstrating an overall mortality:incidence ratio of 37.1%. The Black mortality:incidence ratio was 40.7%, the higest among races in the U.S. (Table 1). Overall, as with incidence, CRC death rates have declined since the 1980s. Despite a rate of decline being observed for both Blacks and NHWs for CRC deaths, the timing and rate of decline are markedly different between the two groups. NHW males and females experienced a decline in CRC death rates beginning in the early 1980s, with continued steady decline since. Black males and females, who showed nearly identical rates to Whites around 1980, did not begin a decline in CRC deaths until the mid-1990s about 15 years later than NHWs, with a slow rate of decline that allowed generation of a growing disparity over time [8]. Interestingly, CRC death rates were slightly lower for Blacks than NHWs in the 1970s, markedly different than current data [8,73]. Thus, genetics is not the full story; however, gene-environment interaction could play a role as well as SES and health insurance access, given that since 1980, metabolic syndrome and obesity have risen disproportionately in minority populations, along with a growing income gap between the wealthiest and poorest quartiles of income.
As mentioned above, Blacks have the highest incidence and death rates for CRC, whereas Hispanics and Asian/Pacific Islanders have the lowest rates (Table 3). Furthermore, Blacks have a distribution of CRC that favors metastatic disease compared to NHWs (Table 2). For each of localized, regional, or distant CRC disease, Blacks show lower 5-year survival as compared to NHWs (Table 2). What is generating this disparity for CRC incidence and mortality in Blacks? The answer is likely multifactorial (Table 4). Environmental contributions amount to 65–70% of CRC risk. These include factors that directly or indirectly influence the colonic epithelium and colonic stem cells that become primed to commence the neoplastic process, and include high fat, red meat, high caloric diet, excess BMI, the use of tobacco products, alcohol intake, low serum levels of vitamin D and calcium, low intake of fish oils, and uniqueness of the gut microbiome makeup [4]. Additionally, the use of hormone replacement therapy and aspirin or NSAIDs that may reduce CRC risk are not as well utilized in minority populations. Many of these environmental factors are disproportionately and adversely represented in the U.S. Black population and are in theory, correctable. For instance, dietary swaps between U.S. Blacks (high fat, low fiber) and South Africans (low fat, high fiber) demonstrated marked reciprocal changes in mucosal biomarkers of cancer risk, changes in microbiota and metabolites known to affect cancer risk including increased butyurogenesis and suppressed secondary bile acid generation in U.S. Blacks on the South African diet [5]. Heritable factors contribute 25–30% of CRC risk. For known Mendelian disorders such as familial adenomatous polyposis or Lynch syndrome, there does not appear to be an excess of founder mutations or prevalence of these conditions among Blacks [62,74]. With Lynch syndrome, the cumulative risk for CRC in Blacks and NHWs with a germline mismatch repair mutation was nearly identical; however, the mutational spectrum of the mismatch repair genes was different, likely reflecting the genetic diversity of the Black population [62]. A family history of CRC or adenomatous polyps, even without evidence for a Mendelian disorder, lowers the age for screening to 40 years [63,64]. Many minority populations do not know or convey their paternal history of cancer or have fear of transmitting it to health care providers, and thus are less likely to be screened at 40 years of age [4].
Table 4.
Factors likely contributing to colorectal cancer disparities between Blacks and Whites
| Environmental factors | Diet | High fat & calories |
| Low fiber | ||
| High red & processed meats | ||
| Low vitamin D & calcium | ||
| Low fish oils | ||
| Co-morbid conditions | Obesity | |
| Metabolic syndrome | ||
| Type 2 diabetes | ||
| Habits | Lack of physical activity | |
| Tobacco use | ||
| Alcohol use | ||
| Medications | Non-steroidal anti-inflammatory drugs | |
| Aspirin | ||
| Hormone replacement therapy | ||
| Microbiome & metabolites | Microbial composition | |
| Bile acid, butyrate & other metabolite composition | ||
|
| ||
| Genetic factors | Mutations | Somatic mutations |
| Germline susceptibility variants | ||
| Microsatellite instability | Microsatellite instability including at tetranucleotide repeats | |
| Immunological factors | Immune cell infiltration especially intratumoral T cells | |
|
| ||
| Societal factors | Socioeconomics | Low socioeconomic status |
| Less education | ||
| Insurance and access to care | Health insurance coverage | |
| Access to medical care especially screening | ||
| Screening behaviors | Screening uptake & adherence | |
| Physician recommendation to screen | ||
Societal factors also play a role in racial CRC disparity incidence and mortality. Blacks tend to have: (a) lower SES, lower level of health insurance coverage, and lower level of education, and (b) less access to medical care, particularly prevention approaches [4]. Specific to CRC is the utilization of screening and surveillance, which has not been equally and uniformly applied or accessed by all populations. There is strong evidence that screening reduces morbidity and mortality from CRC, and with successful implementation and utilization, will likely reduce or eliminate the observed CRC disparity between Black and NHW populations [65,66,75,76]. While overall screening rates in the U.S. continue to rise, a disparity still exists for utilization among races. Screening in Blacks still lags behind NHWs, but is improving [8,73]. Diagnostic colonoscopy for follow-up of a CRC screening test lags behind among Black patients compared to NHW patients [77], and was even observed for the follow-up of frank rectal bleeding [78]. Diligent follow-up, as well as the use of patient navigators might improve the utilization of necessary CRC screening and diagnostic procedures [79,80].
Biological factors may contribute to some of the observed CRC disparity. Blacks tend to present 5–8 years younger on average with CRC (e.g. mean age of 62 vs. mean of age of NHWs at 69 years of age), and have a higher proportion of CRCs under the age of 50 years (10.6%) compared to NHWs (5.5%) [4,81]. As with over 50 years of age, Blacks showed the highest incidence for CRC in the 40–49 year age group, suggesting early triggers for neoplasia are present than any other racial group [71,72]. High risk adenomas (>9 mm), the precursor to most CRCs, appear to be more prevalent among Blacks beginning at age 50 years [82,83]. Additionally, Blacks show a higher proportion of both high risk adenomas and CRC in the proximal colon [4,75,82,83], a 7–15% more right colon distribution than NHWs. Proximal colon polyps, in particular, may be harder to spot at colonoscopy, and the reduction from CRC mortality with colonosocpy is lower than the left side of the colon [84–86], potentially amplifying the disparity.
Genetic factors may contribute to biological reasons for CRC disparity. Black patients display a higher frequency of KRAS mutations in tumors, increasing the aggressiveness of the CRC [87]. Mutations in the driver genes EPHA6 and FLCN were found exclusively in Black CRCs, suggesting a unique behavior modifying role for these CRCs [88]. Another study identified novel somatic alterations in well-known CRC genes (APC, BRAF, KRAS, and PIK3CA) among Blacks [89]. Microsatellite instability (MSI), a good prognostic biomarker caused by the hypermethylation of the DNA mismatch repair gene MLH1, shows a lower frequency among Blacks [81], although a meta-analysis did not reach statistical significance to show a difference [90]. Elevated microsatellite alterations at selected tetranucleotide repeats, a poor prognostic biomarker generated by inflammation-initiated nuclear-to-cytosolic transfer of the DNA mismatch repair protein MSH3, shows a higher frequency among Blacks [91,92]. MSH3 was also frequently somatically-mutated among a cohort of Blacks using whole exome sequencing [89]. Somatic epigenetic differences have not been adequately studied between races; insulin and TGFβ pathway genes (GAS7, BMP3, GPR75) were observed epigenetically inactivated among Blacks, but without comparison with their NHW counterparts [93,94]. GWAS evaluations for CRC have largely included patients of European descent; there is a lack of studies that show specific risk loci among U.S. Black patients. Of the more than 50 CRC risk loci identified to date [60], none show risk loci specific for Blacks, since only few patients of African descent have been included in such studies [95,96]. One study demonstrated that among 10 CRC risk alleles examined between Blacks and NHW CRC patients, there was significant heterogeneity with variation of risk between the populations at different chromosome loci [97,98].
Immunological factors could also play a role in biological causes of CRC disparities. Histological evaluation of Black CRCs as compared to NHW CRCs demonstrate: (a) an absence of high levels of CD8+ T cell counts in MSI tumors [81] and (b) lower infiltration of immune cells expressing granzyme B, a cytotoxic marker, particularly at the invasive borders of the tumor [99]. These observations of reduced immune function against cancer cells contribute to the aggressiveness of the tumor. Additionally, if the frequency of MSI is less among Black CRC patients, a process that generates novel immunogenic truncated proteins from frameshifted transcribed genes [100], the benefit from PD-1 immune checkpoint blockade that appears to be effective for MSI tumors [101,102] is relatively curtailed in this population.
Quality of care factors, particularly an endoscopist’s adenoma detection rate (ADR), contributes to patient outcome that contributes towards CRC mortality disparity. Increased ADR through proposective performance feedback has been shown to reduce interval CRCs (adjusted hazard ratio 0.63 [CI 0.45–0.68]) and cancer death (adjusted hazard ratio 0.50 [CI 0.27–0.95]) in patients undergoing screening colonscopy [103]. In a population-based cohort study examining Medicare patients age 66 to 75 years who received screening colonoscopy, 52.8% of Blacks as compared to 46.2% of NHWs received colonoscopy from physicians with lower polyp detection rates, despite no difference in the proportions of persons in either race receiving screening colonosocpy (Blacks 79.5% vs NHWs 80.7%) or polypectomy (Blacks 23.4% vs NHWs 24.7%) [104]. Furthermore, the probability of interval cancer was 7.1% in Blacks (adjusted hazard ratio 1.32 [CI 1015–1.51]), as compared to 5.8% in NHWs, 4.4% in Hispanics, and 3.8% in Asians [104]. Analysis suggested that variations in polyp detection rate cold not explain the differences between Blacks and NHWs, but that the disparity in risk for interval cancer was more pronounced for distal colorectal cancer than for proximal colon cancer [104].
The disparity for CRC in the U.S., particularly between Blacks and NHWs, is likely multifactorial (Table 4). It is not clear whether overcoming SES differences and providing equal access to health care can fully override some of the observed biological factors that make CRC more aggressive among Blacks. Reducing the high rate of metabolic syndrome disorders in this population should help. Several strategies have recently been outlined [105] to decrease the CRC disparity among Blacks, including: (a) improve patient education to reduce patient-level barriers to screening, (b) improve provider education for increasing recommendations for screening in Blacks, (c) implement patient navigation, which is cost-effective in increasing colonoscopic screening among Blacks, (d) increase the overall CRC screening rates among Blacks to be on par with screening rates for NHWs, and (e) modify the age of screening in Blacks due to the differences in observed biology, and which have been recommended by several organizations [4,75,105] and most recently by the 2017 U.S. Multi-Society Task Force on Colorectal Cancer recommendations [64]. The US Preventive Services Task Force recommends screening average risk persons at age 50 years of age, but recognizes CRC disparities and endorses efforts to ensure that specific populations at risk receive recommended screening and follow up [106]. Based on the higher incidence of proximal CRCs among Blacks, colonoscopy is preferred per ACG recommendations [75]. There is growing evidence that fully-implemented CRC screening would greatly reduce or abolish the observed CRC disparity [68,69,76]. Additionally, CRC screening should be from providers with high quality based on ADRs [103,104]. Inclusion of minority populations in clinical and comparative effectiveness trials for CRC should help identify subpopulation differences that can be addressed in personalized medicine approaches. Many past trials, including GWAS studies, CRC screening trials, and treatment trials have not utilized diverse populations in their cohorts. Overcoming patient, provider, and perceived barriers will be key for inclusion.
Liver cancer
The incidence of hepatocellular carcinoma (HCC) is increasing in the U.S. and has doubled over the last 2 decades. In the U.S., there was an estimated 40,710 new cases and 28,920 deaths in 2017 (Table 1). HCC is the third leading cause of cancer-related deaths worldwide. Gender distribution is nearly 3:1 with males making up 29,200 and females 11,510 cases in 2017 (Table 1). In addition to gender differences, the incidence of HCC differs among racial groups (Table 3). Chronic hepatitis B virus (HBV) correlates with HCC in most areas around the globe and in specific ethnic groups in the U.S., particularly Asian Americans, due to vertical transmission of HBV at birth [107]. Most patients in the U.S. who develop HCC have hepatitis C virus with cirrhosis, although other conditions that lead to cirrhosis (such as chronic alcoholic liver disease, non-alcoholic fatty liver disease (NAFLD), exposure to aflatoxin B1 or vinyl chloride or androgenic steroids, and untreated metabolic and inflammatory diseases (e.g. alpha-1 antitrypsin, Wilson’s, hemachromatosis, glycogen storage diseases, autoimmune chronic active hepatitis, primary biliary cirrhosis) in addition to HBV) can cause HCC [107]. New nucleotide/nucleoside and protease inhibitors that clear HCV viral loads theoretically should reduce HCC over time for those who can obtain the expensive treatment [108,109], but other conditions such as NAFLD will likely become the dominant etiology among populations in the U.S. Rates of NAFLD are highest among Hispanic patients compared to NHWs and Blacks [110,111], and without a clear definitive treatment path for NAFLD to date, a relative increased disparity could develop for HCC in Hispanics in the future. Variants for NAFLD risk exist in single nucleotide polymorphisms in or near PNPLA3 and PPP1R3B genes in Hispanic Americans and PNPLA3, NCAN, GCKR, and PPP1R3B genes in Blacks [112].
At present, the highest incidence and death rates for HCC in the U.S. are among Asian Americans, likely due to the prevalence of HBV vertical transmission, and Hispanics, likely due to NAFLD and HCV. Rates are next highest for American Indian/Alsakan natives and Blacks. With the growing risk factors from metabolic syndrome, obesity/diabetes and NAFLD, non-Asian populations may overtake the incidence and mortality of Asian Americans (Table 3). Influences such as HBV vaccination and treatment, HCV treatment, HCC surveillance in high risk populations, and societal efforts to curb obesity and treat metabolic syndrome with statins and metformin [113] may alter these populations’ risk projections.
Anal cancer
The incidence of anal cancer in 2017 in the U.S. was 8,200 new cases of which 5,250 were in females and 2,950 in males (Table 1). Anal cancer rates have been on the rise for the past three decades [114–116]. This increase has been attributed to the HIV epidemic, HPV infection, and changes in sexual behavior and attitudes [117]. The highest increase was noted in Black men [118], who show the highest incidence for anal cancer, followed by NHW women (Table 3). Black men also had a poor prognosis with lower survival rate. Their five-year survival rate with early stage anal cancer was 62% versus 79% for Caucasian men [119]. The overall expected deaths from anal cancer are 1,100 for 2017 (Table 1).
Histological sub-types of anal cancer include SCC and adenocarcinoma, each with different incidence, clinical features and risk factors. Women show higher rates of SCC and lower rates of adenocarcinoma than men [120]. Blacks appear to have lower rates of SCC than NHWs, but higher rates of adenocarcinoma. Anal cancer incidence was higher in men and Blacks aged <40 years [120]. Most anal cancers are of the SCC type, with adenocarcinoma only accounting for 9–14% of total diagnosed cases in the U.S. and are possibly extensions of rectal lesions [118]. Ninety percent of anal SCCs are caused by HPV infection, while only a small portion of adenocarcinoma is associated with HPV [120,121]. As such, little is known about the etiology of the adenocarcinoma type. Smoking is reported as a risk factor that correlates with anal cancer, especially in those with HPV infections [122,123].
HPV vaccination of both females and males will likely play a role in greatly reducing anal squamous cell carcinoma. However, not all patients have anal cancer as a result of HPV serotypes 16 and 18, which accounts for 70% of all cervical cancers, as other high risk serotypes have been detected among anal cancers [124]. One available vaccine also is effective against serotypes 6 and 11, and together with serotypes 16 and 18 account for 90% of all cases of genital warts. Black populations, particularly women, may have a higher HPV incidence than other U.S. populations [125,126], despite similar incident HPV infection rates. The prevalence disparity may be generated by slower clearance of HPV among African American women, taking 601 days on average to clear the virus compared to European American women requiring only 316 days [126]. Additional disparities might be generated with provider recommendation for HPV vaccination, age for commencement of the vaccine, and compliance with all doses of the HPV vaccination [127,128]. Educational programs for both providers and patients and their communities may mitigate these issues with vaccination.
CONCLUSIONS
Digestive tract cancers are among the most frequent and deadly cancers in Americans. Several GI tract cancers show disparate incidence and mortality rates within racial/ethnic populations of the U.S., with Blacks demonstrating the highest rates for five of seven cancers highligted in this article (esophageal squamous cell carcinoma, gastric, small bowel, pancreas, colorectal and anal cancer) (Figure 1 and Table 3). Some differences between races can be explained (e.g. vertical HBV transmission for HCC risk in Asians), while other causes for cancer disparity are likely multifactorial – from biological and genetic influences, dietary and microbiome make-up, to socio-economic, healthcare access, and biases toward treatment or screening. Strategies that involve knowledge and education of patients and physicians, reduction of obesity and ingestion of low fat and high fiber diets, moderation of alcohol and tobacco usage, and vaccination programs all will help curb incidence in all populations [129]. CRC, in particular, might have the current disparity between Blacks and NHWs greatly reduced with a fully-implemented screening and surveillance program in these populations. These strategies as well as the inclusion of diverse populations in clinical trials for digestive cancer prevention and care may highlight alternative and personalized medicine approaches to mitigate some of the observed disparities.
Acknowledgments
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. This work was supported by the United States Public Health Service (G12 MD007597 to HA and HB; K08 CA142892 to SSK; U01 CA162147, R01 DK067287, and R01 CA206010 to JMC) and the A. Alfred Taubman Medical Research Institute of the University of Michigan (to JMC).
Abbreviations
- NHB
Non-Hispanic Black
- NHW
Non-Hispanic White
- CRC
colorectal cancer
- SCC
squamous cell carcinoma
- HCC
hepatocellualr carcinoma
- HBV
hepatitis B virus
- HCV
hepatitis C virus
- HPV
human papilloma virus
- GI
gastrointestinal
- CDC
Center for Diseases Control
- CHDIR
CDC Health Disparity and Inequality Report
- SES
socio-economic status
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure of Potential Conflicts of Interest: No potential conflicts of interest are disclosed.
References
Author names in bold designate shared co-first authorship.
- 1.Kamineni A, Williams MA, Schwartz SM, et al. The incidence of gastric carcinoma in Asian migrants to the United States and their descendants. Cancer Causes Control. 1999;10:77–83. doi: 10.1023/a:1008849014992. [DOI] [PubMed] [Google Scholar]
- 2.O’Keefe SJ, Chung D, Mahmoud N, et al. Why do African Americans get more colon cancer than Native Africans? J Nutr. 2007;137:175S–182S. doi: 10.1093/jn/137.1.175S. [DOI] [PubMed] [Google Scholar]
- 3.Satia JA, Keku T, Galanko JA, Martin C, Doctolero RT, Tajima A, Sandler RS, Carethers JM. Diet, lifestyle, and genomic instability in the North Carolina Colon Cancer Study. Cancer Epidemiol Biomarkers Prev. 2005;14:429–436. doi: 10.1158/1055-9965.EPI-04-0486. [DOI] [PubMed] [Google Scholar]
- 4.Carethers JM. Screening for colorectal cancer in African Americans: Determinants and rationale for an earlier age to commence screening. Dig Dis Sci. 2015;60:711–21. doi: 10.1007/s10620-014-3443-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Keefe SJ, Li JV, Lahti L, Ou J, Carbonero F, Mohammed K, et al. Fat, fibre and cancer risk in African Americans and rural Africans. Nat Commun. 2015;6:6342. doi: 10.1038/ncomms7342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nguyen T, Ramsey D, Graham D, et al. The Prevalence of Helicobacter pylori Remains High in African American and Hispanic Veterans. Helicobacter. 2015;20:305–15. doi: 10.1111/hel.12199. [DOI] [PubMed] [Google Scholar]
- 7.Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51(Suppl):S28–40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- 8.Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017;67:7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 9.https://www.cdc.gov/mmwr/preview/ind2013_su.html#HealthDisparities2013
- 10.Ohashi S, Miyamoto S, Kikuchi O, Goto T, Amanuma Y, Muto M. Recent Advances From Basic and Clinical Studies of Esophageal Squamous Cell Carcinoma. Gastroenterology. 2015;149:1700–15. doi: 10.1053/j.gastro.2015.08.054. [DOI] [PubMed] [Google Scholar]
- 11.Rubenstein JH, Shaheen NJ. Epidemiology, Diagnosis, and Management of Esophageal Adenocarcinoma. Gastroenterology. 2015;149:302–17.e1. doi: 10.1053/j.gastro.2015.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seer.cancer.gov. Accessed June 2017.
- 13.Ashktorab H, Nouri Z, Nouraie M, Razjouyan H, Lee EE, Dowlati E, El-Seyed el-W, Laiyemo A, Brim H, Smoot DT. Esophageal carcinoma in African Americans: a five-decade experience. Dig Dis Sci. 2011;56:3577–82. doi: 10.1007/s10620-011-1853-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baquet CR, Commiskey P, Mack K, Meltzer S, Mishra SI. Esophageal cancer epidemiology in blacks and whites: racial and gender disparities in incidence, mortality, survival rates and histology. J Natl Med Assoc. 2005;97:1471–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Prabhu A, Obi KO, Rubenstein JH. Systematic review with meta-analysis: race-specific effects of alcohol and tobacco on the risk of oesophageal squamous cell carcinoma. Aliment Pharmacol Ther. 2013;38:1145–55. doi: 10.1111/apt.12514. [DOI] [PubMed] [Google Scholar]
- 16.Brown LM, Hoover RN, Greenberg RS, Schoenberg JB, Schwartz AG, Swanson GM, Liff JM, Silverman DT, Hayes RB, Pottern LM. Are racial differences in squamous cell esophageal cancer explained by alcohol and tobacco use? J Natl Cancer Inst. 1994;86:1340–5. doi: 10.1093/jnci/86.17.1340. [DOI] [PubMed] [Google Scholar]
- 17.Prabhu A, Obi K, Lieberman D, Rubenstein JH. The Race-Specific Incidence of Esophageal Squamous Cell Carcinoma in Individuals With Exposure to Tobacco and Alcohol. Am J Gastroenterol. 2016;111:1718–1725. doi: 10.1038/ajg.2016.346. [DOI] [PubMed] [Google Scholar]
- 18.Cui R1, Kamatani Y, Takahashi A, Usami M, Hosono N, Kawaguchi T, Tsunoda T, Kamatani N, Kubo M, Nakamura Y, Matsuda K. Functional variants in ADH1B and ALDH2 coupled with alcohol and smoking synergistically enhance esophageal cancer risk. Gastroenterology. 2009;137:1768–75. doi: 10.1053/j.gastro.2009.07.070. [DOI] [PubMed] [Google Scholar]
- 19.1000 Genomes Project Consortium. Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, Marchini JL, McCarthy S, McVean GA, Abecasis GR. A global reference for human genetic variation. Nature. 2015;526:68–74. doi: 10.1038/nature15393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abnet CC, Freedman ND, Hu N, Wang Z, Yu K, Shu XO, et al. A shared susceptibility locus in PLCE1 at 10q23 for gastric adenocarcinoma and esophageal squamous cell carcinoma. Nat Genet. 2010;42:764–7. doi: 10.1038/ng.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang LD, Zhou FY, Li XM, Sun LD, Song X, Jin Y, et al. Genome-wide association study of esophageal squamous cell carcinoma in Chinese subjects identifies susceptibility loci at PLCE1 and C20orf54. Nat Genet. 2010;4:759–63. doi: 10.1038/ng.648. [DOI] [PubMed] [Google Scholar]
- 22.American Gastroenterological Association. Spechler SJ, Sharma P, Souza RF, Inadomi JM, Shaheen NJ. American Gastroenterological Association medical position statement on the management of Barrett’s esophagus. Gastroenterology. 2011;140:1084–91. doi: 10.1053/j.gastro.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 23.El-Serag HB, Petersen NJ, Carter J, Graham DY, Richardson P, Genta RM, Rabeneck L. Gastroesophageal reflux among different racial groups in the United States. Gastroenterology. 2004;126:1692–9. doi: 10.1053/j.gastro.2004.03.077. [DOI] [PubMed] [Google Scholar]
- 24.Corley DA, Kubo A, Levin TR, Block G, Habel L, Rumore G, Quesenberry C, Buffler P. Race, ethnicity, sex and temporal differences in Barrett’s oesophagus diagnosis: a large community-based study, 1994–2006. Gut. 2009;58:182–8. doi: 10.1136/gut.2008.163360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dong E, Duan L, Wu BU. Racial and ethnic minorities at increased risk for gastric cancer in a regional US population study. Clin Gastroenterol Hepatol. 2017;15:511–517. doi: 10.1016/j.cgh.2016.11.033. [DOI] [PubMed] [Google Scholar]
- 26.Palles C, Chegwidden L, Li X, Findlay JM, Farnham G, Castro Giner F, et al. Polymorphisms near TBX5 and GDF7 are associated with increased risk for Barrett’s esophagus. Gastroenterology. 2015;148:367–78. doi: 10.1053/j.gastro.2014.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Su Z, Gay LJ, Strange A, Palles C, Band G, Whiteman DC, Lescai F, et al. Esophageal Adenocarcinoma Genetics Consortium; Wellcome Trust Case Control Consortium 2 Common variants at the MHC locus and at chromosome 16q24.1 predispose to Barrett’s esophagus. Nat Genet. 2012;44:1131–6. doi: 10.1038/ng.2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dai JY, de Dieu Tapsoba J, Buas MF, Onstad LE, Levine DM, Risch HA, Chow WH, Bernstein L, Ye W, Lagergren J, Bird NC, Corley DA, Shaheen NJ, Wu AH, Reid BJ, Hardie LJ, Whiteman DC, Vaughan TL. A newly identified susceptibility locus near FOXP1 modifies the association of gastroesophageal reflux with Barrett’s esophagus. Cancer Epidemiol Biomarkers Prev. 2015;24:1739–47. doi: 10.1158/1055-9965.EPI-15-0507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Levine DM, Ek WE, Zhang R, Liu X, Onstad L, Sather C, et al. A genome-wide association study identifies new susceptibility loci for esophageal adenocarcinoma and Barrett’s esophagus. Nat Genet. 2013;45:1487–93. doi: 10.1038/ng.2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Karimi P, Islami F, Anandasabapathy S, et al. Gastric cancer: descriptive epidemiology, risk factors, screening, and prevention. Cancer Epidemiol Biomarkers Prev. 2014;23:700–13. doi: 10.1158/1055-9965.EPI-13-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Martel C, Forman D, Plummer M. Gastric cancer: epidemiology and risk factors. Gastroenterol Clin North Am. 2013;42:219–40. doi: 10.1016/j.gtc.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 32.Kim HW, Kim JH, Lim BJ, et al. Sex Disparity in Gastric Cancer: Female Sex is a Poor Prognostic Factor for Advanced Gastric Cancer. Ann Surg Oncol. 2016;23:4344–4351. doi: 10.1245/s10434-016-5448-0. [DOI] [PubMed] [Google Scholar]
- 33.Ford AC, Forman D, Hunt R, et al. Helicobacter pylori eradication for the prevention of gastric neoplasia. Cochrane Database Syst Rev. 2015:CD005583. doi: 10.1002/14651858.CD005583.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Helgason H, Rafnar T, Olafsdottir HS, Jonasson JG, Sigurdsson A, Stacey SN, et al. Loss-of-function variants in ATM confer risk of gastric cancer. Nat Genet. 2015;47:906–10. doi: 10.1038/ng.3342. [DOI] [PubMed] [Google Scholar]
- 35.Saeki N, Saito A, Choi IJ, Matsuo K, Ohnami S, Totsuka H, et al. A functional single nucleotide polymorphism in mucin 1, at chromosome 1q22, determines susceptibility to diffuse-type gastric cancer. Gastroenterology. 2011;140:892–902. doi: 10.1053/j.gastro.2010.10.058. [DOI] [PubMed] [Google Scholar]
- 36.Sun H, Wu X, Wu F, Li Y, Yu Z, Chen X, Chen Y, Yang W. Associations of genetic variants in the PSCA, MUC1 and PLCE1 genes with stomach cancer susceptibility in a Chinese population. PLoS One. 2015;10:e0117576. doi: 10.1371/journal.pone.0117576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miyazaki T, Murayama Y, Shinomura Y, et al. E-cadherin gene promoter hypermethylation in H. pylori-induced enlarged fold gastritis. Helicobacter. 2007;12:523–31. doi: 10.1111/j.1523-5378.2007.00519.x. [DOI] [PubMed] [Google Scholar]
- 38.Khawja SN, Mohammed S, Silberfein EJ, Musher BL, Fisher WE, Van Buren G., 2nd Pancreatic cancer disparities in African Americans. Pancreas. 2015;44:522–7. doi: 10.1097/MPA.0000000000000323. [DOI] [PubMed] [Google Scholar]
- 39.Chang KJ, Parasher G, Christie C, Largent J, Anton-Culver H. Risk of pancreatic adenocarcinoma: disparity between African Americans and other race/ethnic groups. Cancer. 2005;103:349–57. doi: 10.1002/cncr.20771. [DOI] [PubMed] [Google Scholar]
- 40.Klein AP, Brune KA, Petersen GM, Goggins M, Tersmette AC, Offerhaus GJ, Griffin C, Cameron JL, Yeo CJ, Kern S, Hruban RH. Prospective risk of pancreatic cancer in familial pancreatic cancer kindreds. Cancer Res. 2004;64:2634–8. doi: 10.1158/0008-5472.can-03-3823. [DOI] [PubMed] [Google Scholar]
- 41.Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW, American College of Gastroenterology ACG clinical guideline: Genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015;110:223–62. doi: 10.1038/ajg.2014.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Amundadottir LT. Pancreatic Cancer Genetics. Int J Biol Sci. 2016;12:314–25. doi: 10.7150/ijbs.15001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang M, Wang Z, Obazee O, Jia J, Childs EJ, Hoskins J, et al. Three new pancreatic cancer susceptibility signals identified on chromosomes 1q32.1, 5p15.33 and 8q24.21. Oncotarget. 2016;7:66328–66343. doi: 10.18632/oncotarget.11041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Childs EJ, Mocci E, Campa D, Bracci PM, Gallinger S, Goggins M, et al. Common variation at 2p13.3, 3q29, 7p13 and 17q25.1 associated with susceptibility to pancreatic cancer. Nat Genet. 2015;47:911–6. doi: 10.1038/ng.3341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Willis JA, Olson SH, Orlow I, Mukherjee S, McWilliams RR, Kurtz RC, Klein RJ. A replication study and genome-wide scan of single-nucleotide polymorphisms associated with pancreatic cancer risk and overall survival. Clin Cancer Res. 2012;18:3942–51. doi: 10.1158/1078-0432.CCR-11-2856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hart AR, Kennedy H, Harvey I. Pancreatic cancer: a review of the evidence on causation. Clin Gastroenterol Hepatol. 2008;6:275–82. doi: 10.1016/j.cgh.2007.12.041. [DOI] [PubMed] [Google Scholar]
- 47.Bethea TN, Kitahara CM, Sonderman J, Patel AV, Harvey C, Knutsen SF, et al. A pooled analysis of body mass index and pancreatic cancer mortality in african americans. Cancer Epidemiol Biomarkers Prev. 2014;23:2119–25. doi: 10.1158/1055-9965.EPI-14-0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Silverman DT, Hoover RN, Brown LM, Swanson GM, Schiffman M, Greenberg RS, Hayes RB, Lillemoe KD, Schoenberg JB, Schwartz AG, Liff J, Pottern LM, Fraumeni JF., Jr Why do Black Americans have a higher risk of pancreatic cancer than White Americans? Epidemiology. 2003;14:45–54. doi: 10.1097/00001648-200301000-00013. [DOI] [PubMed] [Google Scholar]
- 49.Arnold LD, Patel AV, Yan Y, Jacobs EJ, Thun MJ, Calle EE, Colditz GA. Are racial disparities in pancreatic cancer explained by smoking and overweight/obesity? Cancer Epidemiol Biomarkers Prev. 2009;18:2397–405. doi: 10.1158/1055-9965.EPI-09-0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pourmand K, Itzkowitz SH. Small Bowel Neoplasms and Polyps. Curr Gastroenterol Rep. 2016;18:23. doi: 10.1007/s11894-016-0497-x. [DOI] [PubMed] [Google Scholar]
- 51.Goodman MT, Matsuno RK, Shvetsov YB. Racial and ethnic variation in the incidence of small-bowel cancer subtypes in the United States, 1995–2008. Dis Colon Rectum. 2013;56:441–8. doi: 10.1097/DCR.0b013e31826b9d0a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Coe TM, Fero KE, Fanta PT, Mallory RJ, Tang CM, Murphy JD, Sicklick JK. Population-Based Epidemiology and Mortality of Small Malignant Gastrointestinal Stromal Tumors in the USA. J Gastrointest Surg. 2016;20:1132–40. doi: 10.1007/s11605-016-3134-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tran T, Davila JA, El-Serag HB. The epidemiology of malignant gastrointestinal stromal tumors: an analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol. 2005;100:162–8. doi: 10.1111/j.1572-0241.2005.40709.x. [DOI] [PubMed] [Google Scholar]
- 54.Shenoy S. Genetic risks and familial associations of small bowel carcinoma. World J Gastrointest Oncol. 2016;8:509–19. doi: 10.4251/wjgo.v8.i6.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rubio-Tapia A, Ludvigsson JF, Brantner TL, Murray JA, Everhart JE. The prevalence of celiac disease in the United States. Am J Gastroenterol. 2012;107:1538–44. doi: 10.1038/ajg.2012.219. [DOI] [PubMed] [Google Scholar]
- 56.Choung RS, Ditah IC, Nadeau AM, Rubio-Tapia A, Marietta EV, Brantner TL, et al. Trends and racial/ethnic disparities in gluten-sensitive problems in the United States: findings from the National Health and Nutrition Examination Surveys from 1988 to 2012. Am J Gastroenterol. 2015;110:455–61. doi: 10.1038/ajg.2015.8. [DOI] [PubMed] [Google Scholar]
- 57.Du Y, Ter-Minassian M, Brais L, Brooks N, Waldron A, Chan JA, Lin X1, Kraft P, Christiani DC, Kulke MH. Genetic associations with neuroendocrine tumor risk: results from a genome-wide association study. Endocr Relat Cancer. 2016;23:587–94. doi: 10.1530/ERC-16-0171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Leoncini E, Carioli G, La Vecchia C, Boccia S, Rindi G. Risk factors for neuroendocrine neoplasms: a systematic review and meta-analysis. Ann Oncol. 2016;27:68–81. doi: 10.1093/annonc/mdv505. [DOI] [PubMed] [Google Scholar]
- 59.Grady WM, Carethers JM. Genomic and epigenetic instability in colorectal cancer pathogenesis. Gastroenterology. 2008;135:1079–1099. doi: 10.1053/j.gastro.2008.07.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Carethers JM, Jung BH. Genetics and genetic biomarkers in sporadic colorectal cancer. Gastroenterology. 2015;149:1177–1190. doi: 10.1053/j.gastro.2015.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Carethers JM, Stoffel EM. Lynch syndrome and Lynch syndrome mimics: The growing complex landscape of hereditary colon cancer. World J Gastroenterol. 2015;21:9253–61. doi: 10.3748/wjg.v21.i31.9253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Guindalini RS, Win AK, Gulden C, Lindor NM, Newcomb PA, Haile RW, Raymond V, Stoffel E, Hall M, Llor X, Ukaegbu CI, Solomon I, Weitzel J, Kalady M, Blanco A, Terdiman J, Shuttlesworth GA, Lynch PM, Hampel H, Lynch HT, Jenkins MA, Olopade OI, Kupfer SS. Mutation spectrum and risk of colorectal cancer in African American families with Lynch syndrome. Gastroenterology. 2015;149:1446–53. doi: 10.1053/j.gastro.2015.07.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Levin B, Lieberman DA, McFarland B, Andrews KS, Brooks D, Bond J, Dash C, Giardiello FM, Glick S, Johnson D, Johnson CD, Levin TR, Pickhardt PJ, Rex DK, Smith RA, Thorson A, Winawer SJ, American Cancer Society Colorectal Cancer Advisory Group, US Multi-Society Task Force.; American College of Radiology Colon Cancer Committee Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134:1570–95. doi: 10.1053/j.gastro.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 64.Rex DK, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, Kaltenbach T, Levin TR, Lieberman D, Robertson DJ. Colorectal Cancer Screening: Recommendations for Physicians and Patients From the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2017;153:307–323. doi: 10.1053/j.gastro.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 65.Carethers JM. Should African Americans be screened for colorectal cancer earlier? Nature Clinical Practice Gastroenterology & Hepatology. 2005;2:352–353. doi: 10.1038/ncpgasthep0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Naylor K, Ward J, Polite BN. Interventions to improve care related to colorectal cancer among racial and ethnic minorities: a systematic review. J Gen Intern Med. 2012;27:1033–46. doi: 10.1007/s11606-012-2044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ayanian JZ, Carethers JM. Bridging Behavior and Biology to Reduce Socioeconomic Disparities in Colorectal Cancer Risk. J Natl Cancer Inst. 2012;104:1343–1344. doi: 10.1093/jnci/djs356. [DOI] [PubMed] [Google Scholar]
- 68.Grubbs SS, Polite BN, Carney J, Jr, Bowser W, Rogers J, Katurakes N, Hess P, Paskett ED. Eliminating racial disparities in colorectal cancer in the real world: it took a village. J Clin Oncol. 2013;31:1928–30. doi: 10.1200/JCO.2012.47.8412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Richards CA, Kerker BD, Thorpe L, Olson C, Krauskopf MS, Silver LS, Weber TK, Winawer SJ. Increased screening colonoscopy rates and reduced racial disparities in the New York Citywide campaign: an urban model. Am J Gastroenterol. 2011;106:1880–1886. doi: 10.1038/ajg.2011.191. [DOI] [PubMed] [Google Scholar]
- 70.Amri R, Bordeianou LG, Berger DL. The conundrum of the young colon cancer patient Surgery. 2015;158:1696–1703. doi: 10.1016/j.surg.2015.07.018. [DOI] [PubMed] [Google Scholar]
- 71.Ashktorab H, Vilmenay K, Brim H, et al. Colorectal Cancer in Young African Americans: Is It Time to Revisit Guidelines and Prevention? Dig Dis Sci. 2016;61:3026–30. doi: 10.1007/s10620-016-4207-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Carethers JM. The increasing incidence of colorectal cancers diagnosed in subjects under age 50 among races: cracking the conundrum. Dig Dis Sci. 2016;61:2767–2769. doi: 10.1007/s10620-016-4268-1. [DOI] [PubMed] [Google Scholar]
- 73.DeSantis CE, Siegel RL, Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, Jemal A. Cancer statistics for African Americans, 2016: progress and opportunities in reducing racial disparities. CA Cancer J Clin. 2016;66:290–308. doi: 10.3322/caac.21340. [DOI] [PubMed] [Google Scholar]
- 74.Carethers JM. Racial and ethnic factors in the genetic pathogenesis of colorectal cancer. J Assoc Acad Minor Phys. 1999;10:59–67. [PubMed] [Google Scholar]
- 75.Agrawal S, Bhupinderjit A, Bhutani MS, Boardman L, Nguyen C, Romero Y, Srinivasan R, Figueroa-Moseley C, Committee of Minority Affairs and Cultural Diversity, American College of Gastroenterology Colorectal cancer in African Americans. Am J Gastroenterol. 2005;100:515–23. doi: 10.1111/j.1572-0241.2005.41829.x. [DOI] [PubMed] [Google Scholar]
- 76.Tammana VS, Laiyemo AO. Colorectal cancer disparities: issues, controversies and solutions. World J Gastroenterol. 2014;20:869–76. doi: 10.3748/wjg.v20.i4.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Laiyemo AO, Doubeni C, Pinsky PF, Doria-Rose VP, Bresalier R, Lamerato LE, Crawford ED, Kvale P, Fouad M, Hickey T, Riley T, Weissfeld J, Schoen RE, Marcus PM, Prorok PC, Berg CD. Race and colorectal cancer disparities: health-care utilization vs different cancer susceptibilities. J Natl Cancer Inst. 2010;102:538–46. doi: 10.1093/jnci/djq068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shields HM, Stoffel EM, Chung DC, Sequist TD, Li JW, Pelletier SR, Spencer J, Silk JM, Austin BL, Diguette S, Furbish JE, Lederman R, Weingart SN. Disparities in evaluation of patients with rectal bleeding 40 years and older. Clin Gastroenterol Hepatol. 2014;12:669–75. doi: 10.1016/j.cgh.2013.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chen LA, Santos S, Jandorf L, Cristie J, Castillo A, Winkel G, Itzkowitz S. A program to enhance completion of screening colonoscopy among urban minorities. Clin Gastroenterol Hepatol. 2008;6:443–50. doi: 10.1016/j.cgh.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 80.Jandorf L, Cooperman JL, Stossel LM, Itzkowitz S, Thompson HS, Villagra C, Thélémaque LD, McGinn T, Winkel G, Valdimarsdottir H, Shelton RC, Redd W. Implementation of culturally targeted patient navigation system for screening colonoscopy in a direct referral system. Health Educ Res. 2013;28:803–15. doi: 10.1093/her/cyt003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Carethers JM, Murali B, Yang B, Doctolero RT, Tajima A, Basa R, Smith EJ, Lee M, Janke R, Ngo T, Tejeda R, Ji M, Kinseth M, Cabrera BL, Miyai K, Keku TO, Martin CF, Galanko JA, Sandler RS, McGuire KL. Influence of race on microsatellite instability and CD8+ T cell infiltration in colon cancer. PLoS One. 2014;9:e100461. doi: 10.1371/journal.pone.0100461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lieberman DA, Williams JL, Holub JL, Morris CD, Logan JR, Eisen GM, Carney P. Race, Ethnicity, and Sex Affect Risk for Polyps >9 mm in Average-Risk Individuals. Gastroenterology. 2014;147:351–8. doi: 10.1053/j.gastro.2014.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Corley DA, Jensen CD, Marks AR, Zhao WK, de Boer J, Levin TR, Doubeni C, Fireman BH, Quesenberry CP. Variation of adenoma prevalence by age, sex, race, and colon location in a large population: implications for screening and quality programs. Clin Gastroenterol Hepatol. 2013;11:172–80. doi: 10.1016/j.cgh.2012.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M. Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med. 2011;154:22–30. doi: 10.7326/0003-4819-154-1-201101040-00004. [DOI] [PubMed] [Google Scholar]
- 85.Nishihara R, Wu K, Lochhead P, Morikawa T, Liao X, Qian ZR, Inamura K, Kim SA, Kuchiba A, Yamauchi M, Imamura Y, Willett WC, Rosner BA, Fuchs CS, Giovannucci E, Ogino S, Chan AT. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013;369:1095–105. doi: 10.1056/NEJMoa1301969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Xicola RM, Gagnon M, Clark JR, Carroll T, Gao W, Fernandez C, et al. Excess of proximal microsatellite-stable colorectal cancer in African Americans from a multiethnic study. Clin Cancer Res. 2014;20:4962–70. doi: 10.1158/1078-0432.CCR-14-0353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yoon HH, Shi Q, Alberts SR, Goldberg RM, Thibodeau SN, Sargent DJ, Sinicrope FA, Alliance for Clinical Trials in Oncology Racial Differences in BRAF/KRAS Mutation Rates and Survival in Stage III Colon Cancer Patients. J Natl Cancer Inst. 2015;107(10):djv186. doi: 10.1093/jnci/djv186. pii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Guda K, Veigl ML, Varadan V, Nosrati A, Ravi L, Lutterbaugh J, Beard L, Willson JK, Sedwick WD, Wang ZJ, Molyneaux N, Miron A, Adams MD, Elston RC, Markowitz SD, Willis JE. Novel recurrently mutated genes in African American colon cancers. Proc Natl Acad Sci U S A. 2015;112:1149–54. doi: 10.1073/pnas.1417064112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ashktorab H, Daremipouran M, Devaney J, Varma S, Rahi H, Lee E, Shokrani B, Schwartz R, Nickerson ML, Brim H. Identification of novel mutations by exome sequencing in African American colorectal cancer patients. Cancer. 2015;121:34–42. doi: 10.1002/cncr.28922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ashktorab H, Ahuja S, Kannan L, Llor X, Ellis N, Xicola RM, Adeyinka LO, Carethers JM, Brim H, Nouraie M. A meta-analysis of MSI frequency and race in colorectal cancer. Oncotarget. 2016;7:34546–34557. doi: 10.18632/oncotarget.8945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Carethers JM, Koi M, Tseng-Rogenski SS. EMAST is a Form of Microsatellite Instability That is Initiated by Inflammation and Modulates Colorectal Cancer Progression. Genes (Basel) 2015;6:185–205. doi: 10.3390/genes6020185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Devaraj B, Lee A, Cabrera BL, Miyai K, Luo L, Ramamoorthy S, Keku T, Sandler RS, McGuire K, Carethers JM. Relationship of EMAST and microsatellite instability among patients with rectal cancer. J Gastrointest Surg. 2010;14:1521–8. doi: 10.1007/s11605-010-1340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ashktorab H, Daremipouran M, Goel A, Varma S, Leavitt R, Sun X, Brim H. DNA methylome profiling identifies novel methylated genes in African American patients with colorectal neoplasia. Epigenetics. 2014;9:503–12. doi: 10.4161/epi.27644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ashktorab J, Wansley D, Rahi J, Varma S, Shokrani B, Lee E, Daremipouran M, Laiyemo A, Goel A, Carethers JM, Brim H. Toward a comprehensive and systemic methylome signature in colorectal cancers. Epigenetics. 2013;8:807–815. doi: 10.4161/epi.25497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lemire M, Qu C, Loo LW, Zaidi SH, Wang H, Berndt SI, et al. A genome-wide association study for colorectal cancer identifies a risk locus in 14q23.1. Hum Genet. 2015;134:1249–62. doi: 10.1007/s00439-015-1598-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wang H, Burnett T, Kono S, Haiman CA, Iwasaki M, Wilkens LR, Loo LW, Van Den Berg D, Kolonel LN, Henderson BE, Keku TO, Sandler RS, Signorello LB, Blot WJ, Newcomb PA, Pande M, Amos CI, West DW, Bézieau S, Berndt SI, Zanke BW, Hsu L, Genetics and Epidemiology of Colorectal Cancer Consortium (GECCO) Lindor NM, Haile RW, Hopper JL, Jenkins MA, Gallinger S, Casey G, Colon Cancer Family Registry (CCFR) Stenzel SL, Schumacher FR, Peters U, Gruber SB, Colorectal Transdisciplinary Study (CORECT) Tsugane S, Stram DO, Le Marchand L. Trans-ethnic genome-wide association study of colorectal cancer identifies a new susceptibility locus in VTI1A. Nat Commun. 2014;5:4613. doi: 10.1038/ncomms5613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kupfer SS, Anderson JR, Hooker S, Skol A, Kittles RA, Keku TO, Sandler RS, Ellis NA. Genetic heterogeneity in colorectal cancer associations between African and European americans. Gastroenterology. 2010;139:1677–85. 1685.e1–8. doi: 10.1053/j.gastro.2010.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kupfer SS, Skol AD, Hong E, Ludvik A, Kittles RA, Keku TO, Sandler RS, Ellis NA. Shared and independent colorectal cancer risk alleles in TGFβ-related genes in African and European Americans. Carcinogenesis. 2014;35:2025–30. doi: 10.1093/carcin/bgu088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Basa RCB, Davies V, Li X, Murali B, Shah J, Yang B, Li S, Khan MW, Tian M, Tejada R, Hassan A, Washington A, Mukherjee B, Carethers JM, McGuire KL. Decreased anti-tumor cytotoxic immunity among colon cancers from African Americans. PLoS One. 2016;11:e0156660. doi: 10.1371/journal.pone.0156660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Carethers JM. Hereditary, sporadic and metastatic colorectal cancers are commonly driven by specific spectrums of defective DNA mismatch repair components. Trans Am Clin Climatol Assoc. 2016;127:81–97. [PMC free article] [PubMed] [Google Scholar]
- 101.Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, Skora AD, Luber BS, Azad NS, Laheru D, Biedrzycki B, Donehower RC, Zaheer A, Fisher GA, Crocenzi TS, Lee JJ, Duffy SM, Goldberg RM, de la Chapelle A, Koshiji M, Bhaijee F, Huebner T, Hruban RH, Wood LD, Cuka N, Pardoll DM, Papadopoulos N, Kinzler KW, Zhou S, Cornish TC, Taube JM, Anders RA, Eshleman JR, Vogelstein B, Diaz LA., Jr PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. N Engl J Med. 2015;372:2509–2520. doi: 10.1056/NEJMoa1500596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Koi M, Carethers JM. The colorectal cancer immune microenvironment and approach to immunotherapies. Future Oncology. 2017 doi: 10.2217/fon-2017-0145. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kaminski MF, Wieszczy P, Rupinski M, Wojciechowska U, Didkowska J, Kraszewska E, Kobiela J, Franczyk R, Rupinska M, Kocot B, Chaber-Ciopinska A, Pachlewski J, Polkowski M, Regula J. Increased Rate of Adenoma Detection Associates With Reduced Risk of Colorectal Cancer and Death. Gastroenterology. 2017;153:98–105. doi: 10.1053/j.gastro.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 104.Fedewa SA, Flanders WD, Ward KC, Lin CC, Jemal A, Goding Sauer A, Doubeni CA, Goodman M. Racial and Ethnic Disparities in Interval Colorectal Cancer Incidence: A Population-Based Cohort Study. Ann Intern Med. 2017;166:857–866. doi: 10.7326/M16-1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kupfer SS, Carr RM, Carethers JM. Reducing colorectal cancer risk among African Americans. Gastroenterology. 2015;149:1302–1304. doi: 10.1053/j.gastro.2015.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Knudsen AB, Zauber AG, Rutter CM, Naber SK, Doria-Rose VP, Pabiniak C, Johanson C, Fischer SE, Lansdorp-Vogelaar I, Kuntz KM. Estimation of Benefits, Burden, and Harms of Colorectal Cancer Screening Strategies: Modeling Study for the US Preventive Services Task Force. JAMA. 2016;315:2595–609. doi: 10.1001/jama.2016.6828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365:1118–27. doi: 10.1056/NEJMra1001683. [DOI] [PubMed] [Google Scholar]
- 108.Reddy KR, Lim JK, Kuo A, Di Bisceglie AM, Galati JS, Morelli G, Everson GT, Kwo PY, Brown RS, Jr, Sulkowski MS, Akuschevich L, Lok AS, Pockros PJ, Vainorius M, Terrault NA, Nelson DR, Fried MW, Manns MP; HCV-TARGET Study Group All-oral direct-acting antiviral therapy in HCV-advanced liver disease is effective in real-world practice: observations through HCV-TARGET database. Aliment Pharmacol Ther. 2017;45:115–126. doi: 10.1111/apt.13823. [DOI] [PubMed] [Google Scholar]
- 109.Terrault NA, Zeuzem S, Di Bisceglie AM, Lim JK, Pockros PJ, Frazier LM, Kuo A, Lok AS, Shiffman ML, Ben Ari Z, Akushevich L, Vainorius M, Sulkowski MS, Fried MW, Nelson DR, HCV-TARGET Study Group Effectiveness of Ledipasvir-Sofosbuvir Combination in Patients With Hepatitis C Virus Infection and Factors Associated With Sustained Virologic Response. Gastroenterology. 2016;151:1131–1140.e5. doi: 10.1053/j.gastro.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sherif ZA, Saeed A, Ghavimi S, Nouraie SM, Laiyemo AO, Brim H, Ashktorab H. Global Epidemiology of Nonalcoholic Fatty Liver Disease and Perspectives on US Minority Populations. Dig Dis Sci. 2016;61:1214–25. doi: 10.1007/s10620-016-4143-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kalia HS, Gaglio PJ. The Prevalence and Pathobiology of Nonalcoholic Fatty Liver Disease in Patients of Different Races or Ethnicities. Clin Liver Dis. 2016;20:215–24. doi: 10.1016/j.cld.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 112.Palmer ND, Musani SK, Yerges-Armstrong LM, Feitosa MF, Bielak LF, Hernaez R, Kahali B, Carr JJ, Harris TB, Jhun MA, Kardia SL, Langefeld CD, Mosley TH, Jr, Norris JM, Smith AV, Taylor HA, Wagenknecht LE, Liu J, Borecki IB, Peyser PA, Speliotes EK. Characterization of European ancestry nonalcoholic fatty liver disease-associated variants in individuals of African and Hispanic descent. Hepatology. 2013;58:966–75. doi: 10.1002/hep.26440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Singal AG, El-Serag HB. Hepatocellular Carcinoma From Epidemiology to Prevention: Translating Knowledge into Practice. Clin Gastroenterol Hepatol. 2015;13:2140–51. doi: 10.1016/j.cgh.2015.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Soeberg MJ, Rogers K, Currow DC, et al. Trends in incidence and survival for anal cancer in New South Wales, Australia, 1972–2009. Cancer Epidemiol. 2015;39:842–7. doi: 10.1016/j.canep.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 115.van der Zee RP, Richel O, de Vries HJ, et al. The increasing incidence of anal cancer: can it be explained by trends in risk groups? Neth J Med. 2013;71:401–11. [PubMed] [Google Scholar]
- 116.Nielsen A, Munk C, Kjaer SK. Trends in incidence of anal cancer and high-grade anal intraepithelial neoplasia in Denmark, 1978–2008. Int J Cancer. 2012;130:1168–73. doi: 10.1002/ijc.26115. [DOI] [PubMed] [Google Scholar]
- 117.D’Souza G, Wentz A, Wiley D, et al. Anal Cancer Screening in Men Who Have Sex With Men in the Multicenter AIDS Cohort Study. J Acquir Immune Defic Syndr. 2016;71:570–6. doi: 10.1097/QAI.0000000000000910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Daling JR, Madeleine MM, Johnson LG, et al. Human papillomavirus, smoking, and sexual practices in the etiology of anal cancer. Cancer. 2004;101:270–80. doi: 10.1002/cncr.20365. [DOI] [PubMed] [Google Scholar]
- 119.Johnson LG, Madeleine MM, Newcomer LM, et al. Anal cancer incidence and survival: the surveillance, epidemiology, and end results experience, 1973–2000. Cancer. 2004;101:281–8. doi: 10.1002/cncr.20364. [DOI] [PubMed] [Google Scholar]
- 120.Serrano B, de Sanjose S, Tous S, et al. Human papillomavirus genotype attribution for HPVs 6, 11, 16, 18, 31, 33, 45, 52 and 58 in female anogenital lesions. Eur J Cancer. 2015;51:1732–41. doi: 10.1016/j.ejca.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 121.Alemany L, Saunier M, Alvarado-Cabrero I, et al. Human papillomavirus DNA prevalence and type distribution in anal carcinomas worldwide. Int J Cancer. 2015;136:98–107. doi: 10.1002/ijc.28963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Morris VK, Rashid A, Rodriguez-Bigas M, et al. Clinicopathologic Features Associated With Human Papillomavirus/p16 in Patients With Metastatic Squamous Cell Carcinoma of the Anal Canal. Oncologist. 2015;20:1247–52. doi: 10.1634/theoncologist.2015-0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ramamoorthy S, Luo L, Luo E, Carethers JM. Tobacco smoking and risk of recurrence for squamous cell cancer of the anus. Cancer Detect Prev. 2008;32:116–20. doi: 10.1016/j.cdp.2008.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ramamoorthy S, Liu Y-T, Luo L, Miyai K, Lu Q, Carethers JM. Detection of multiple human papillomavirus genotypes in anal carcinoma. Infect Agent Cancer. 2010;5:17. doi: 10.1186/1750-9378-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Castle PE, Gage JC, Partridge EE, Rausa A, Gravitt PE, Scarinci IC. Human papillomavirus genotypes detected in clinician-collected and self-collected specimens from women living in the Mississippi Delta. BMC Infect Dis. 2013;13:5. doi: 10.1186/1471-2334-13-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Banister CE, Messersmith AR, Cai B, Spiryda LB, Glover SH, Pirisi L, Creek KE. Disparity in the persistence of high-risk human papillomavirus genotypes between African American and European American women of college age. J Infect Dis. 2015;211:100–8. doi: 10.1093/infdis/jiu394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mohammed KA, Geneus CJ, Osazuwa-Peters N, Adjei Boakye E, Tobo BB, Burroughs TE. Disparities in Provider Recommendation of Human Papillomavirus Vaccination for U.S. Adolescents. J Adolesc Health. 2016;59:592–598. doi: 10.1016/j.jadohealth.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 128.Rahman M, Hirth JM, Berenson AB. Adherence to ACIP Recommendation for Human Papillomavirus Vaccine Among US Adolescent Girls. J Community Health. 2017;42:385–389. doi: 10.1007/s10900-016-0267-6. [DOI] [PubMed] [Google Scholar]
- 129.Polite BN, Adams-Campbell LL, Brawley OW, Bickell N, Carethers JM, Flowers CR, Foti M, Gomez SL, Griggs JJ, Lathan CS, Li CI, Lichtenfeld L, McCaskill-Stevens W, Paskett ED. Charting the future of cancer health disparities research: a position statement from the American Association for Cancer Research, the American Cancer Society, the American Society of Clinical Oncology, and the National Cancer Institute. J Clin Oncology. 2017 Jul;24:JCO2017736546. doi: 10.1200/JCO.2017.73.6546. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]


