Abstract
Over 22 million Americans are current users of marijuana; half of US states allow medical marijuana, and several allow recreational marijuana. The objective of this study was to evaluate the impact marijuana has on hospitalizations, emergency department (ED) visits, and regional poison center (RPC) calls in Colorado, a medical and recreational marijuana state. This is a retrospective review using Colorado Hospital Association hospitalizations and ED visits with marijuana-related billing codes, and RPC marijuana exposure calls. Legalization of marijuana in Colorado has been associated with an increase in hospitalizations, ED visits, and RPC calls linked with marijuana exposure. From 2000 to 2015, hospitalization rates with marijuana-related billing codes increased from 274 to 593 per 100,000 hospitalizations in 2015. Overall, the prevalence of mental illness among ED visits with marijuana-related codes was five-fold higher (5.07, 95% CI: 5.0, 5.1) than the prevalence of mental illness without marijuana-related codes. RPC calls remained constant from 2000 through 2009. However, in 2010, after local medical marijuana policy liberalization, the number of marijuana exposure calls significantly increased from 42 to 93; in 2014, after recreational legalization, calls significantly increased by 79.7%, from 123 to 221 (p <0.0001). The age group <17 years old also had an increase in calls after 2014. As more states legalize marijuana, it is important to address public education and youth prevention, and understand the impact on mental health disorders. Improvements in data collection and surveillance methods are needed to more accurately evaluate the public health impact of marijuana legalization.
Keywords: Marijuana, Cannabis, Emergency department, Emergency room, Hospitalizations, Poison center, Colorado, Legalization
1. Introduction
In 2011, the Drug Abuse Warning Network (DAWN) estimated marijuana was involved in over 455,668 emergency department (ED) visits in the US, an increase of 62% from 2004. This represented 38.3% of visits involving illicit drugs, second only to cocaine (Substance Abuse and Mental Health Services Administration, 2013). Since 2011, 8 states have legalized retail marijuana, and another 12 have legalized medical marijuana. After the 2016 elections, more than half of US states have now passed legislation to allow medical marijuana and 8 have legalized recreational marijuana (Crary, 2016). Commercialization of marijuana has become a multi-billion dollar industry: in Colorado alone, it is estimated that legalization of marijuana has had a $2.4 billion impact on the state (Light et al., 2016).
The impact marijuana legalization has on various related health outcomes has only begun to be evaluated. Estimates on the prevalence of marijuana use have not appeared to significantly change in the US. According to the 2015 National Survey on Drug Use and Health, an estimated 22.2 million (8.3%) Americans aged 12 years or older are currently users of marijuana (Center for Behavioral Health Statistics and Quality, 2016). In Colorado, past month use increased from 10.1% in 2008/2009 to 16.6% in 2014/2015 (Center for Behavioral Health Statistics and Quality, 2016; Substance Abuse and Mental Health Services Administration, 2010). Initial reports of adolescent marijuana use have gone up in Washington, while have not changed in Colorado (Cerda et al., 2017). Unintentional pediatric exposures have gone up in states that have legalized medical marijuana (Wang et al., 2014). Medical marijuana laws are associated with lower state-level opioid related hospital admissions and overdose mortality rates (Bachhuber et al., 2014; Shi, 2017). As more states legalize marijuana, it is imperative to evaluate the public health impact going forward.
Colorado legalized medical marijuana in 2000 with the passing of Amendment 20 (CO Const. Amend. 20 Art. XVIII §14, 2016). Commercialization of medical marijuana increased in 2010, after the U.S. Attorney General’s Ogden Memorandum said that they would not prosecute individuals for medical marijuana legal at the state level (Odgen, 2009). Amendment 64 was passed in 2012, allowing dispensary sales of retail/recreational marijuana to begin on January 1, 2014 (CO Const. Amend. 64 Art. XVIII §16, 2012). The objective of this study was to examine the impact marijuana has had on hospitalizations, emergency department (ED) visits, and regional poison center (RPC) calls in Colorado.
2. Methods
2.1. Objectives
Our primary objective was to compare rates of hospitalizations and ED visits with marijuana-related billing codes and RPC calls with mention of marijuana across time periods. Our secondary objective was to compare the primary diagnosis categories of hospitalizations and ED visits with marijuana-related billing codes to hospitalizations and ED visits without marijuana-related billing codes.
2.2. Colorado Hospital Association data source
Rates of hospitalizations and emergency department (ED) visits in Colorado were obtained from the Colorado Hospital Association (CHA) Discharge Data which collects discharge data from hospitals in the state of Colorado (CHA Databank, 2015). In this database, ED visits that resulted in admissions to the hospital were counted as hospitalizations, making each hospitalization and ED visit mutually exclusive. Hospitalizations and ED visits for both Colorado residents and nonresidents were included in this analysis. CHA hospitalization data were abstracted from January 1, 2000 through September 30, 2015. CHA ED visit data were not reliably collected until 2011. Therefore, ED visits were abstracted from January 1, 2011 through September 30, 2015.
Hospitalizations and ED visits possibly associated with marijuana were identified using four International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) marijuana-related billing codes: E854.1 - Accidental poisoning by psychodysleptics (hallucinogens); 969.6 - Poisoning by psychodysleptics (hallucinogens); 305.20–305.23 – Nondependent cannabis abuse unspecified, continuous, episodic, and in remission; and 304.30–304.33 - Cannabis dependence unspecified, continuous, episodic, and in remission (Practice Management Information Corporation [PMIC], 2015a; Practice Management Information Corporation [PMIC], 2015b; Practice Management Information Corporation [PMIC], 2015c; Practice Management Information Corporation [PMIC], 2015d). For codes E854.1 and 969.9, psychodysleptics include cannabis derivatives, lysergide (LSD), marijuana derivatives, mescaline, psilocin, and psilocybin (Practice Management Information Corporation [PMIC], 2015c; Practice Management Information Corporation [PMIC], 2015d). Hospitalizations and ED visits with marijuana-related billing codes were defined as those listing one or more marijuana-related ICD-9-CM codes within the first three listed diagnoses.
For the secondary objective, hospitalizations and ED visits were grouped into 18 broad categories based on the first billing code listed in each record, which was considered the primary diagnosis. The Healthcare Cost and Utilization Project’s (HCUP) Multiple Level Clinical Classification Software (CCS) was used for this categorization (Healthcare Cost and Utilization Project, 2015). Records with marijuana-related codes in the primary diagnosis categorize as mental illness; therefore, these records were excluded from all primary diagnosis analyses to prevent overestimating the mental illness category with the exposure. Hospitalizations and ED visits with marijuana-related billing codes were defined as those listing one or more marijuana-related ICD-9-CM codes within any of the up to 30 listed diagnosis codes.
2.3. Regional poison center data
RPC human exposure calls for all ages in Colorado were obtaining from the National Poison Data System (NPDS) from January 1, 2000 through December 31, 2015. NPDS serves as the data repository for the American Association of Poison Control Centers, and collects exposure case reports for all participating regional poison centers (RPC) in the United States. Variables collected included age, gender, substance(s) involved, reason for exposure (intentional versus unintentional exposure), route of exposure (inhaled, ingested, other), medical outcome, patient disposition, and clinical effects.
Human marijuana exposure calls to Colorado poison center were queried from NPDS using the single generic code that includes all types of marijuana (0083000). Calls abstracted with missing data elements, exposures unrelated to marijuana, or exposures indicating “Medical Review Officer” were validated through a review of the call case notes by a pharmacist and physician. Exposures indicating synthetic marijuana analogs or pharmaceutical THC medications (i.e. Marinol®, dronabinol, cannabidiol) were not included in these analyses.
Annual counts of poison center calls with possible marijuana exposures were stratified into four age categories: 0–8 years, 9–17 years, 18–24 years, 25 years or older and unknown age. Unknown ages included ages recorded as teens, 20s, unknown adult (≥20 yrs), unknown child (≤19 yrs), and unknown. These age categories were stratified by intentionality of the exposure to marijuana (unintentional vs. intentional). Unintentional exposures included environmental exposures, food poisonings, unintentional misuses, and unintentional therapeutic errors. Intentional exposures included adverse drug reactions, adverse food reactions, intentional abuses or misuses, and suspected suicides.
Beginning in 2014 the RPC started systematically collecting more specific information on the types of marijuana exposures, allowing categorization into smokable, edibles, dermal products, and marijuana extracts. The type of marijuana was examined by age category from July 1, 2014 to December 31, 2015.
2.4. Statistical analysis
The SAS version 9.4 (SAS Institute Inc., Cary, NC) statistical software package was used for all statistical analyses. Annual rates of hospitalizations and ED visits with marijuana-related billing codes were calculated by multiplying the proportion of hospitalizations and ED visits with marijuana-related billing codes among all hospitalizations and ED visits by 100,000. Rates were compared across years and significant differences were determined with a Wald Chi-square test using univariate Poisson regression. A Bonferroni correction was used to adjust for multiple comparisons. There were 15 comparisons among hospitalizations and 4 comparisons among ED visits making the p values required for significance ≤0.003 and 0.0125 respectively. The prevalence of the top 10 CCS diagnosis categories was calculated for hospitalizations and ED visits with marijuana-related billing codes (in any of the listed billing codes) and compared to the prevalence of the same diagnosis categories for hospitalizations and ED visits without marijuana-related billing codes through prevalence ratios and 95% confidence intervals (95% CI). Hospitalizations and ED visits with marijuana-related billing codes in the primary diagnosis were not included in these prevalence ratios.
Counts of RPC calls related to marijuana exposures were quantified and compared across years. To determine significant differences in numbers of calls related to marijuana across years, a Wald Chi-square test was performed using univariate Poisson regression. A Bonferroni correction was used to adjust for multiple comparisons. There were 15 comparisons making the p value required for significance ≤0.003.
Data obtained from CHA and RPC were collected and analyzed as part of public health surveillance activities.
3. Results
3.1. Hospitalizations and emergency department visits
There were a total of 7,438,905 hospitalizations from January 1, 2000 through September 30, 2015, where 25,192 (0.3%) hospitalizations had marijuana-related billing codes within the first three diagnosis codes and 86,597 (1.2%) hospitalizations had marijuana-related billing codes in any listed diagnosis code. There were 84 (0.001%) hospitalizations excluded because both codes for nondependent cannabis abuse (305.20–305.23) and cannabis dependence (304.30–304.33) were recorded and 119 (0.001%) hospitalizations excluded that did not categorize into one of the 18 primary diagnosis categories in the Clinical Classification Software (CCS) due to coding errors. An additional 1942 (0.03%) hospitalizations had marijuana-related billing codes in the primary diagnosis and were excluded.
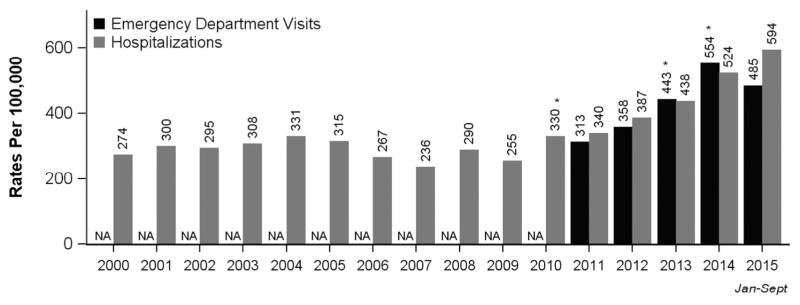
Rates of hospitalizations with marijuana-related billing codes within the first three diagnosis codes increased from 274 per 100,000 hospitalizations in 2000 prior to any marijuana legalization to 593 per 100,000 hospitalizations in 2015 after two years of recreational marijuana legalization (Fig. 1). The highest increase in rates of hospitalization was 29% between 2009 and 2010, and 25% from 2013 to 2014. The increase in rates between 2009 and 2010 was statistically significant (p = 0.002). There was a marginal statistically significant increase in rates from 2013 to 2014 (p = 0.006). January through June 2015 the rate of hospitalizations with marijuana-related billing codes within the first three diagnosis codes increased by 13.4% to 594 per 100,000 from 2014 (p = 0.0364); however, after considering multiple comparisons this increase was not significant.
Fig. 1.
Rates of hospitalizations (HD) and emergency department (ED) visits with marijuana- related billing codes in the first three diagnosis codes in Colorado. *Rates significantly increased from the previous year at a p value of <0.003 for hospitalizations and <0.0125 for ED visits. †lCD-9-CM codes 305.20–305.23, 304.30–304.33, 969.6, and E854.1 were used to determine HD and ED visits with marijuana-related billing codes within the first three diagnosis codes. ‡Data source: Colorado Hospital Association Discharge Data
There were a total of 7,517,236 ED visits from January 1, 2011 to September 30, 2015 where 32,899 (0.4%) ED visits had marijuana-related billing codes within the first three diagnosis codes and 61,063 (0.8%) ED visits had marijuana-related billing codes in any listed diagnosis code. There were 6 (0.00008%) ED visits excluded because both codes for nondependent cannabis abuse (305.20–305.23) and cannabis dependence (304.30–304.33) were recorded and 79,889 (1.1%) ED visits excluded that did not categorize into one of the 18 categories within the CCS due to coding errors and missing primary diagnoses. An additional 5087 (0.07%) ED visits had marijuana-related billing codes in the primary diagnosis and were excluded.
Rates of ED visits with marijuana-related billing codes within the first three diagnosis codes increased from 313 per 100,000 ED visits in 2011 to 478 per 100,000 in 2015, with the highest rate occurring in 2014 (554 per 100,000 ED visits) (Fig. 1). The rates of ED visits significantly increased from 2012 to 2013 (p = 0.003) and from 2013 to 2014 (p = 0.0005); however, the rates decreased by 12.5% from 2014 to 2015 though it was nonsignificant (p = 0.0324).
When evaluating primary diagnosis categories involving marijuana, the overall prevalence of mental illness was five-fold higher (5.03, 95% CI: 4.96, 5.09) and nine-fold higher (9.67, 95% CI: 9.59, 9.74) among ED visits and hospitalizations with marijuana-related billing codes compared to the prevalence of mental illness without marijuana-related billing codes in ED visits and hospitalizations respectively (Tables 1 and 2). The prevalence of unclassified codes and E codes was two-fold higher (2.09, 95% CI: 1.97, 2.22) among ED visits with marijuana-related billing codes compared to ED visits without marijuana-related billing codes (Table 1). This category included the code for altered mental status (780.97) which was likely driving this finding. Among hospitalizations there were a 16% higher (1.16, 95% CI: 1.14, 1.18), an 18% higher (1.18, 95% CI: 1.13, 1.23), and a 6% higher (1.06, 95% CI: 1.02, 1.10) prevalence of injury and poisonings, diseases of the nervous system and sense organs, and endocrine, nutritional, and metabolic diseases and immunity respectively among hospitalizations with marijuana-related billing codes compared to hospitalizations without marijuana-related billing codes (Table 2).
Table 1.
Percentage and prevalence of the top ten primary diagnoses of emergency department (ED) visits with marijuana-related billing codesa compared to ED visits without marijuana-related billing codes in Colorado from 2011 through September 2015 (N = 7,432,254).c
| Prevalence of primary diagnoses of ED visits, N (%) | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Primary diagnosis categories | With marijuana-related codesa | Without marijuana-related codes | Prevalence ratio (95% CI) | |||
| Mental illness | 17,802 | (29.1) | 432,161 | (5.8) | 5.03 | (4.96–5.09) |
| Symptoms, signs, and ill-defined conditions and factors influencing health status | 8472 | (13.9) | 1,083,907 | (14.5) | 0.95 | (0.93–0.97) |
| Injury and poisoning | 7032 | (11.5) | 1,473,427 | (19.8) | 0.58 | (0.57–0.59) |
| Marijuana-associated codesb | 5087 | (8.3) | 0 | (0.00) | – | – |
| Diseases of the nervous system and sense organs | 4251 | (7.0) | 739,970 | (9.9) | 0.70 | (0.68–0.72) |
| Diseases of the respiratory system | 3508 | (5.7) | 1,003,357 | (13.5) | 0.43 | (0.41–0.44) |
| Diseases of the digestive system | 3533 | (5.8) | 459,355 | (6.2) | 0.94 | (0.90–0.96) |
| Diseases of the circulatory system | 2914 | (4.8) | 426,082 | (5.7) | 0.84 | (0.80–0.86) |
| Diseases of the musculoskeletal system and connective tissue | 2612 | (4.3) | 496,555 | (6.7) | 0.64 | (0.61–0.66) |
| Diseases of the genitourinary system | 1995 | (3.3) | 436,173 | (5.8) | 0.56 | (0.53–0.58) |
| Unclassified codes and E codes | 1075 | (1.8) | 62,688 | (0.8) | 2.09 | (1.97–2.22) |
Marijuana-related ICD-9-CM codes included 304.3, 305.2, 969.6, and E854.1 in any of the listed 30 diagnosis codes.
Marijuana-related ICD-9-CM codes included 304.3, 305.2, 969.6, and E854.1 in the primary diagnosis. These ED visits were excluded prevalence ratio calculations.
Data details: Colorado Hospital Association (CHA), 2015 data is January 1, 2015 through September 30, 2015. NA = data not available. An individual can be represented more than once in the data; therefore, the rate is hospitalizations or ED visits with marijuana-related billing codes per 100,000 hospitalizations or ED visits.
Table 2.
Percentage and prevalence of the top ten primary diagnoses of hospitalizations with marijuana-related billing codesa compared to hospitalizations without marijuana-related Codes in Colorado from 2000 through September 2015 (N = 7,436,760).c
| Prevalence of primary diagnoses of hospitalizations, N (%) | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Primary diagnosis categories | With marijuana-related codesa | Without marijuana-related codes | Prevalence ratio (95% CI) | |||
| Mental illness | 39,768 | (45.9) | 349,231 | (4.7) | 9.67 | (9.59–9.74) |
| Injury and poisoning | 9072 | (10.5) | 662,178 | (9.0) | 1.16 | (1.14–1.18) |
| Complications of pregnancy, childbirth, and the puerperium | 5936 | (6.8) | 1,095,543 | (14.9) | 0.46 | (0.45–0.47) |
| Diseases of the digestive system | 6184 | (7.1) | 653,731 | (8.9) | 0.80 | (0.78–0.82) |
| Diseases of the circulatory system | 5282 | (6.1) | 893,965 | (12.2) | 0.50 | (0.49–0.51) |
| Diseases of the respiratory system | 3529 | (4.1) | 580,105 | (7.9) | 0.52 | (0.50–0.53) |
| Endocrine, nutritional, and metabolic diseases and immunity | 2759 | (3.2) | 220,077 | (3.0) | 1.06 | (1.02–1.10) |
| Diseases of the nervous system and sense organs | 2258 | (2.6) | 162,210 | (2.2) | 1.18 | (1.13–1.23) |
| Marijuana-associated codesb | 1942 | (2.2) | 0 | (0.00) | – | – |
| Diseases of the musculoskeletal system and connective tissue | 1799 | (2.1) | 501,112 | (6.8) | 0.30 | (0.29–0.32) |
| Infectious and parasitic diseases | 1963 | (2.3) | 165,053 | (2.2) | 1.01 | (0.96–1.05) |
Marijuana-related ICD-9-CM codes included 304.3, 305.2, 969.6, and E854.1 in the any of the listed 30 diagnosis codes.
Marijuana-related ICD-9-CM codes included 304.3, 305.2, 969.6, and E854.1 in the primary diagnosis. These hospitalizations were excluded prevalence ratio calculations.
Data details: Colorado Hospital Association (CHA), 2015 data is January 1, 2015 through September 30, 2015. NA = Data not available. An individual can be represented more than once in the data; therefore, the rate is hospitalizations or ED visits with marijuana-related codes per 100,000 hospitalizations or ED visits.
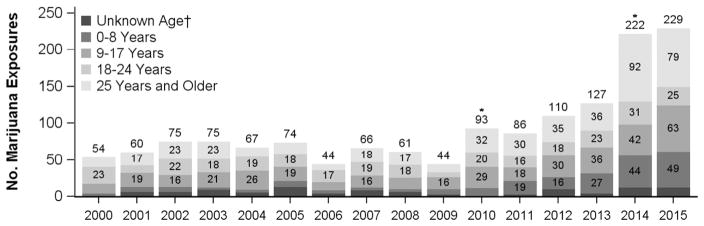
3.2. Regional poison center calls
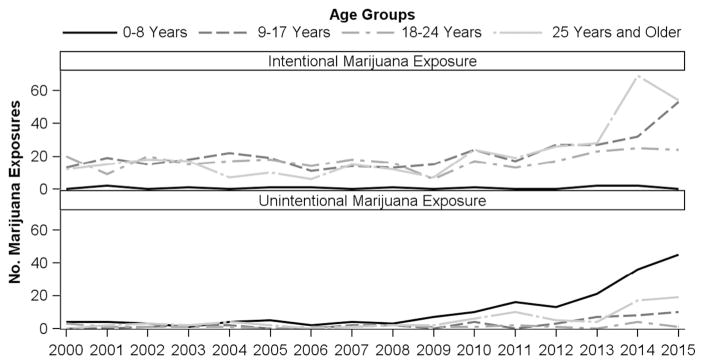
There were 1487 human marijuana exposure RPC calls from 2000 to 2015. There were 114 (7.7%) with missing age or non-specific ages that were indicated as unknown age in the age stratified analysis. RPC calls remained constant from 2000 through 2009. In 2010 after medical marijuana liberalization, exposure calls related to marijuana significantly increased from 44 to 93 (p < 0.0001), and in 2014 after recreational marijuana legalization, calls significant increased by 79.7%, from 123 to 221 (p < 0.0001) (Fig. 2). Age groups of <17 years of age and >25 years of age showed increased numbers of marijuana exposure calls after 2014, while ages 18 through 24 remained fairly constant. Examination of intentionality of RPC calls with marijuana exposures showed that both intentional and unintentional marijuana exposures have increased from 2010 through 2015 (Data not shown). However, when intentionality was stratified by age the numbers of RPC calls involving unintended marijuana exposures increased from 2008 to 2014 among children 0–8 years of age while the number of RPC calls involving intentional marijuana exposures increased among those 9 years and older from 2013 to 2015 (Fig. 3). Examination of the type of marijuana products consumed revealed that edible and smokable marijuana products were the most common type of marijuana involved in exposure calls from July 1, 2014 through December 31, 2015 (N = 326): 130 (39.9%) calls involving edibles, 131 (40.2%) with smokable products, and 65 (19.9%) other marijuana products. Edible calls were the most common type of marijuana exposure calls in children ≤8 years of age (52.1%) and also 25 years and older (39.8%).
Fig. 2.
Annual regional poison center human exposure calls related to marijuana from January 1, 2000 through December 31, 2015, divided by age groups. *Counts significantly increased from previous year with a p value <0.003. †Unknown age includes calls with ages recorded as teens, 20s, unknown adult (≥20 yrs), unknown child (≤19 yrs), and unknown age. ‡Human marijuana exposure calls to RPC were determined by the presence of the generic code Marijuana - 0083000 from the National Poison Data System or marijuana exposure mentioned in RPC case notes.
Fig. 3.
Annual regional poison center human exposure calls related to marijuana from January 1, 2000 through December 31, 2015, divided by age groups and intentionality. *Human marijuana exposure calls to RPC were determined by the presence of the generic code Marijuana- 0083000 from the National Poison Data System or marijuana exposure mentioned in RPC case notes.
4. Discussion
Legalization of marijuana in Colorado has been associated with a trend of increasing hospitalizations and ED visits coded with marijuana-related billing codes, and RPC exposure calls related to marijuana. While this is not necessarily surprising due to the increased availability of marijuana in Colorado, the reasons and the public health consequences of these increases merit further investigation. One potential contributing factor to this increase may be increased honesty regarding marijuana use among patients in a legalized environment. Another contributing factor may be changes in healthcare provider behaviors around collecting marijuana-use medical histories, ordering urine toxicology screens, or documenting marijuana-related outcomes. The variety of marijuana products available in the commercialized market, including high potency concentrates and THC-infused edible marijuana products, may play a role in this increase. High potency cannabis has been associated with increased first-episode psychosis (Di Forti et al., 2015). Due to differing pharmacokinetic and pharmacodynamic profiles, edible products can lead to delayed and severe psychoactive effects from unintentional overconsumption (Lamy et al., 2016; Huestis, 2005; Hancock-Allen et al., 2015). An increase in some specific diagnoses related to marijuana has been previously described after marijuana legalization in Colorado (cyclic vomiting, hash oil burns, pediatric marijuana exposures) (Wang et al., 2014; Kim et al., 2015; Bell et al., 2015; Wang et al., 2011; Wang et al., 2016). Additional research, including medical record abstraction, is necessary to fully understand the details of these individual cases and relationship to specific medical and behavioral health conditions.
Rates began rising after the Ogden Memorandum and subsequent increases in commercialization of medical marijuana in 2010, and increased further in 2014, the first year of recreational marijuana. However, the reason for the substantial decrease in ED visits with marijuana-related codes in January through September 2015 is less clear. It is unlikely due to decrease in sales, as sales continue to be robust and continue to set revenue records through 2016 (Wallace, 2016). If this trend continues into 2016, it may provide evidence of the public learning safe consumption of marijuana products. Further evidence of this learning effect is provided by the discrepancy in the increased rates of ED visits with marijuana-related billing codes for Colorado tourists compared to residents (Kim et al., 2016).
RPC calls related to marijuana are also an important indicator for population level impacts of marijuana legalization. Marijuana exposure calls show a similar increasing trend as hospitalizations and ED visits with marijuana-related billing codes starting in 2010. The largest increases in calls were in the 0 to 8 and over 25 years age range. Analyses of intentionality indicate large increases in unintentional marijuana exposures calls to RCP in young children beginning in 2010 and continuing to 2015. This trend and the consequences to young children have been further documented by Wang et al. (Wang et al., 2014; Wang et al., 2011; Wang et al., 2016). These increases have underscored the need for policy actions on child resistant packaging and public education regarding safe storage of marijuana products. The increase in calls to RPC related to intentional marijuana exposures among adults over 25 years in 2014 may be reflective of uninitiated users experimenting with edible products that have unknowing delayed effects to the inexperienced user. The subsequent decrease in 2015 in this same age category further supports the hypothesis of a learning effect among Colorado adults in safe use of marijuana products.
Among primary diagnosis categories, mental illness was more prevalent in ED visits and hospitalizations with marijuana-related billing codes. Examination of the role marijuana plays in mental health driven healthcare encounters is critical given the relationship between drug use disorders and mental health disorders (Aspis et al., 2015; Hanna et al., 2016; Grant et al., 2016). While it is unclear whether this finding is reflective of changes due to a legal market, it clearly prioritizes the consequences of marijuana use within a mental health population as a priority area for further research. Further investigation is necessary to ascertain the role of marijuana in the casual chain of the mental health diagnosis, ED visits and hospitalizations.
4.1. Limitations
There are some limitations to the use and interpretation of CHA and RPC data. Although CHA does collect data from a large portion of representative Colorado healthcare facilities, it does not include all hospitals and healthcare facilities in Colorado. Thus some healthcare encounters resulting from marijuana exposure may be missed in this dataset, particularly healthcare encounters at inpatient mental health facilities, long-term care facilities, military hospitals, and other outpatient treatment settings.
The true association behind the patient’s marijuana use or exposure and their reason for the healthcare encounter or RPC is not determined by these summary data; marijuana cannot be viewed as the direct cause of these ED visits, hospitalizations, or RPC calls. The data do not directly evaluate the causal relationships between hospitalizations or ED visit and marijuana exposure, and may overestimate the healthcare burden due to marijuana use.
The higher prevalence ratio of hospitalizations with and without mental illness diagnosis, compared to the prevalence ratio for ED visits, could be partially accounted for by screening bias during the healthcare evaluation. Patients who are hospitalized or have mental health evaluations and diagnosis often have a more thorough questioning around substance abuse habits and frequently urine toxicology screening. Increased drug use in the community and increased patient comfort with reporting their use likely increase the chance that a marijuana billing code is included in the top three diagnosis codes in these patients. Furthermore, patients presenting with substance use disorders, a common co-occurring disposition with mental health disorders, could be admitted into detoxification programs (Mark et al., 2010). These may account for the higher number of mental health patients who either admit or screen positive for marijuana use. In addition it has been documented that patients with mental health disorders and/or substance abuse disorders are more likely to have multiple ED visits within a year (Coffey et al., 2010). On the contrary, not all patients are asked about marijuana use, or receive urine drug screens for marijuana during hospitalizations and ED visits, leading to asymmetric surveillance between those with mental health diagnoses and those without mental health diagnoses. We also did not conduct any analyses of changes in codes, or prevalence of diagnosis such as mental illness over time.
Reporting and coding practices may be a source of variation. The differences in provider and coder use of codes for nondependent cannabis abuse (305.20–305.23) and cannabis dependence (304.30–304.33) in practice are unclear. Conversations with hospital coders indicate that these codes may not be applied consistently from hospital to hospital across Colorado. Therefore, hospitalizations and ED visits with marijuana-related billing codes were determined by the presence of any of the four marijuana-related billing codes within the first three listed diagnosis codes for examining rates and in any of the listed diagnosis codes for examining primary diagnosis categories. It is not clear if the rank of the order of the marijuana-related codes is important in capturing healthcare encounters related to marijuana and examining marijuana-related codes within the first three listed diagnosis codes could be an underestimation (Drosler et al., 2014; Slavova et al., 2014).
Finally, RPC cases rely on self-reporting by either the patient or healthcare provider. Calls may have reporting bias as exposure calls may have more severe effects. Thus, RPC data could be an underestimation of true marijuana exposures. Although variables are standardized in data collection at the RPC, documentation may not be consistent and some variables may be missing. Confirmatory testing was not performed on all exposures, so it is possible that some cases may not have been true exposures.
These limitations demonstrate the complexity in evaluating the impact marijuana legalization has on emergency care and other aspects of public health. Improved surveillance methods, consistent data collection, and increased granularity are needed to more accurately describe and better determine causality to specific medical and behavioral health conditions. As more states legalize medical and recreational marijuana, their respective public health agencies and state governments should implement well designed surveillance programs to add to this body of research. Collaboration between states is also essential.
5. Conclusion
Legalization of medical and recreational marijuana in Colorado has been associated with an increase in hospitalizations, ED visits, and poison center calls linked with marijuana exposure. Analyses of these administrative datasets are important to monitor the public health impact of marijuana and provide data for rapid policy interventions. More detailed research including full review of medical records is necessary to ascertain severity and causality in these acute healthcare encounters. Overrepresentation of marijuana-related billing codes for ED visits and hospitalizations with mental illness primary diagnoses suggests an important priority research area to determine the role of marijuana.
Acknowledgments
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflicts of interest
Dr. Wang has a Colorado Department of Public Health and Environment (CDPHE) Grant evaluating cannabidiol in pediatric epilepsy patients. He also receives royalties from UpToDate on related subject matter. Dr. Monte receives support from NIH 1 K23 GM110516 and NIH CTSI UL1 TR001082. Dr. Monte is partially funded by a grant through the CDPHE to study the public health effects of cannabis edible products in Colorado. Dr. Monte has a patent pending for a synthetic cannabinoid clinical assay and has been award funding through the Department of Defense for examination of patterns of use of synthetic cannabinoids and assay development. All authors participate on the CDPHE Retail Marijuana Public Health Advisory Committee.
References
- Aspis I, Feingold D, Weiser M, et al. Cannabis use and mental health-related quality of life among individuals with depressive disorders. Psychiatry Res. 2015;230:341–349. doi: 10.1016/j.psychres.2015.09.014. http://dx.doi.org/10.1016/j.psychres.2015.09.014. [DOI] [PubMed] [Google Scholar]
- Bachhuber MA, Saloner B, Cunningham CO, et al. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Intern Med. 2014;174(10):1668–1673. doi: 10.1001/jamainternmed.2014.4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell C, Slim J, Flaten HK, et al. Butane hash oil burns associated with marijuana liberalization in Colorado. J Med Toxicol. 2015 Dec;11(4):422–425. doi: 10.1007/s13181-015-0501-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. 2015 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2016. [Google Scholar]
- Cerda M, Wall M, Feng T, et al. Association of state recreational marijuana laws with adolescent marijuana use. JAMA Pediatr. 2017;171(2):142–149. doi: 10.1001/jamapediatrics.2016.3624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CHA Databank. [Accessed December 13, 2016];2015 Sep 2; http://www.cha.com/Member-Services/CHA-DATABANK.aspx.
- CO Const Amend 20 Art XVIII §14. 2016 http://www.lexisnexis.com/hottopics/colorado/?app=00075&view=full&interface=1&docinfo=off&searchtype=lt&search=Colo.+Const.+Art.+XVIII%252C+Section+14.
- CO Const Amend 64 Art XVIII §16. 2012 http://www.colorado.gov/cs/Satellite?blobcol=urldata&blobheader=application/pdf&blobkey=id&blobtable=MungoBlobs&blobwhere=1251834064719&ssbinary=true.
- Coffey RM, Houchens R, Chu BC, et al. Emergency Department Use for Mental and Substance Use Disorders. Agency for Healthcare Research and Quality (AHRQ); U.S: 2010. Available. http://www.hcup-us.ahrq.gov/reports.jsp (Online August 23) [Google Scholar]
- Crary D. Marijuana Legalization Pulls big Victories on Election Night 2016. Assoc Press; 2016. Nov, [Accessed December 27, 2016]. http://www.thecannabist.co/2016/11/09/marijuana-legalization-win-polls-election-2016/67176/ [Google Scholar]
- Di Forti M, Marconi A, Carra E, et al. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. Lancet Psychiatry. 2015;2(3):233–238. doi: 10.1016/S2215-0366(14)00117-5. [DOI] [PubMed] [Google Scholar]
- Drosler SE, Romano PS, Sundararajan V, et al. How many diagnosis fields are needed to capture safety events in administrative data? Findings and recommendations from the WHO ICD-11 Topic Advisory Group on Quality and Safety. Int J Qual Health Care. 2014;26(1):16–25. doi: 10.1093/intqhc/mzt090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Saha TD, Ruan WJ, et al. Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions–III. JAMA Psychiatry. 2016;73(1):39–47. doi: 10.1001/jamapsychiatry.2015.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hancock-Allen JB, Barker L, Van Dyke M, et al. Death following ingestion of an edible marijuana product-Colorado, March 2014. MMWR. 2015;64(28):771–772. doi: 10.15585/mmwr.mm6428a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna RC, Perez JM, Ghose S. Cannabis and development of dual diagnoses: a literature review. Am J Drug Alcohol Abuse. 2016;(September):1–14. doi: 10.1080/00952990.2016.1213273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthcare Cost and Utilization Project. Clinical Classifications Software (CCS) for ICD-9-CM. 2015 Jul 06; https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- Huestis MA. Pharmacokinetics and metabolism of the plant cannabinoids, delta9-tetrahydrocannabinol, cannabidiol and cannabinol. [Accessed December 28, 2016];Handb Exp Pharmacol. 2005 168:657–690. doi: 10.1007/3-540-26573-2_23. http://www.ncbi.nlm.nih.gov/pubmed/16596792. [DOI] [PubMed] [Google Scholar]
- Kim HS, Anderson JD, Saghafi O, et al. Cyclic vomiting presentations following marijuana liberalization in Colorado. Acad Emerg Med. 2015 Jun;22(6):694–699. doi: 10.1111/acem.12655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HS, Hall KE, Genco EK, et al. Marijuana tourism and emergency department visits in Colorado. N Engl J Med. 2016;374(8):797–798. doi: 10.1056/NEJMc1515009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamy FR, Daniulaityte R, Sheth A, et al. “Those edibles hit hard”: Exploration of Twitter data on cannabis edibles in the U.S. Drug Alcohol Depend. 2016;164:64–70. doi: 10.1016/j.drugalcdep.2016.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Light M, Orens A, Rowberry J, Saloga CW. The Economic Impact of Marijuana Legalization in Colorado. [Accessed December 1, 2016];Marijuana Policy Gr. 2016 Oct; http://www.mjpolicygroup.com/pubs/MPGImpactofMarijuanaonColorado-Final.pdf.
- Mark T, Vandivort-Warren R, Stocks C, Levit K, et al. Treatment for Substance Use Disorders in Community Hospitals. Agency for Healthcare Research and Quality (AHRQ); U.S: 2010. Available:. http://www.hcup-us.ahrq.gov/reports.jsp (Online August 31) [Google Scholar]
- Odgen DW. [Accessed December 27, 2016];Memorandum from Deputy Attorney General David W Ogden to all United States attorneys regarding investigations and prosecutions in states authorizing the medical use of marijuana. 2009 Oct 19; https://www.justice.gov/opa/blog/memorandum-selected-united-state-attorneys-investigations-and-prosecutions-states.
- Practice Management Information Corporation [PMIC] International Classification of Diseases 9th Revision Clinical Modification. 6. 1, 2, & 3. Los Angeles, California: 2015a. p. 827. [Google Scholar]
- Practice Management Information Corporation [PMIC] International Classification of Diseases 9th Revision Clinical Modification. 6. 1, 2, & 3. Los Angeles, California: 2015b. p. 725. [Google Scholar]
- Practice Management Information Corporation [PMIC] International Classification of Diseases 9th Revision Clinical Modification. 6. 1, 2, & 3. Los Angeles, California: 2015c. p. 314. [Google Scholar]
- Practice Management Information Corporation [PMIC] International Classification of Diseases 9th Revision Clinical Modificaiton. 6. 1, 2, & 3. Los Angeles, California: 2015d. pp. 313–314. [Google Scholar]
- Shi Y. Medical marijuana policies and hospitalizations related to marijuana and opioid pain reliever. Drug Alcohol Depend. 2017;173:144–150. doi: 10.1016/j.drugalcdep.2017.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S, Bunn TL, Talbert J. Drug overdose surveillance using hospital discharge data. Public Health Rep. 2014;129(5):437–445. doi: 10.1177/003335491412900507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings. Office of Applied Studies; Rockville, MD: 2010. NSDUH Series H-38A, HHS Publication No. SMA 10-4586 Findings. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Drug Abuse Warning Network, 2011: national estimates of drug-related emergency department visits. 2013 https://www.samhsa.gov/data/sites/default/files/DAWN-SR154-SuicideAttempts2014/DAWN-SR154-SuicideAttempts2014.pdf. [PubMed]
- Wallace A. Colorado pot shops post record-breaking sales figures topping $122 million in July 2016. The Cannabist; 2016. Sep, [Accessed December 27, 2016]. http://www.thecannabist.co/2016/09/12/colorado-marijuana-sales-july-revenue-pot-tax/63054/ [Google Scholar]
- Wang GS, Narang SK, Wells K, et al. A case series of marijuana exposures in pediatric patients less than 5 years of age. Child Abuse Negl. 2011;35(7):563–565. doi: 10.1016/j.chiabu.2011.03.012. [DOI] [PubMed] [Google Scholar]
- Wang GS, Roosevelt G, Le Lait MC, et al. Association of unintentional pediatric exposures with decriminalization of marijuana in the United States. Ann Emerg Med. 2014;63(6):684–689. doi: 10.1016/j.annemergmed.2014.01.017. [DOI] [PubMed] [Google Scholar]
- Wang GS, Le Lait MC, Deakyne S, et al. Unintentional pediatric exposures to marijuana in Colorado, 2009–2015. JAMA Pediatr. 2016;170(9):e160971. doi: 10.1001/jamapediatrics.2016.0971. [DOI] [PubMed] [Google Scholar]