Background
Mexican immigrants (MAs) make up 28% of the foreign-born population of the United States (1) and Latinos represent the largest and fastest growing minority group (2). Compared to non-Hispanic whites and U.S. born Latinos, Mexican immigrants to the U.S. have diminished access to oral health care services (3) and face substantial barriers to accessing needed services. Research indicates that MAs may delay needed care, preferring to seek health services in Mexico (4, 5). Delaying care may have a number of deleterious consequences, including increased severity of oral health problems, infection, and tooth loss. Further, annual dental visits correspond to a number of positive outcomes – including decreased costs – and may be an important component of managing other health problems, including heart disease and diabetes (6).
To date, research investigating dental health services (DHS) utilization by Mexican immigrants has often drawn on Andersen’s Behavioral Model to examine the significance of individual level factors like sociodemographic status, access to services, and illness severity (7). Generally, findings indicate that diminished access to health insurance (8, 9), unfamiliarity with the U.S. health care system (10), low educational attainment, reduced oral health literacy (11), and fatalistic attitudes about oral health contribute to low rates of dental service utilization among MAs (12, 13). Language and cultural barriers (14), along with fears of deportation among undocumented immigrants, further exacerbate these trends (15).
Despite these important efforts to understand enabling factors and barriers to the use of dental health services, this body of research has important limitations. Generally, there has been a lack of attention to social and cultural factors that contribute to oral health disparities among Mexican immigrants (16, 17). Additionally, within the health service utilization literature in particular, research has tended to focus on individual decision making, which has meant considerably less attention is given to the impact of group or social influences, that may play an important role in shaping oral health and well-being among this vulnerable immigrant population. (18,19).
Conceptual Framework: The Role of Social & Cultural Influences
The research that has been conducted, including work examining the influence of fatalistic beliefs and acculturation among different ethnic groups, has produced mixed results. Generally speaking, health fatalism is the belief or set of beliefs that one’s health outcomes are predetermined and inevitable, and therefore outside individual control. Though health fatalism appears to be more prevalent among Hispanics and other ethnic minority populations compared to non-Hispanic whites, there is considerable debate about the effects of health fatalism on health outcomes (20). In oral health particularly, work by Finlayson and colleagues indicates that fatalism corresponds to less knowledge about oral health needs, driving a lower likelihood of adopting and maintaining positive oral health behaviors (21). Other work has documented similar attitudes among Mexican migrant workers to California (22) and Latino immigrants from predominantly Central America and Mexico (23), of whom 79% believed they would lose all or most of their teeth by old age.
Further, the relationship between fatalism, acculturation, and oral health status is a complicated one. Acculturation represents the process of change that occurs when an individual or group adopts or borrows traits, behaviors, or beliefs of another culture as a result of extended or repeated contact. Though fatalism appears to decrease as immigrants remain in the U.S. for longer periods, duration in the U.S. and subsequent acculturation are associated with a number of stressors that may have deleterious consequences on health – including loss of coping resources like social support and shifts in ethnic and cultural identity (20). Particularly relevant for oral health, acculturation and duration in the United States are linked to greater adoption of American dietary norms, including increased consumption of sugary foods and beverages.
More recent work has begun to call into question the purely negative effects of fatalism, suggesting that its strong correlation to religiosity and spirituality among Latino immigrants may correspond to positive effects on health (20). Though real barriers to accessing quality, affordable care remain a major problem for low-income immigrants to the United States, the high levels of religiosity among this population have been linked to better health behaviors and coping strategies (24, 25). Though this has direct implications for mental health status, it is unclear if fatalism may positively influence oral health via this pathway.
Increasingly, in an effort to address the tension in the current literature about the role of health beliefs and knowledge on health status and well-being, research attention has turned to the role of social networks in shaping patterns of response to health problems among Latino populations (26, 14, 27). Research focusing on diverse health outcomes suggests that norms, values, expectations, and beliefs shared in the context of individuals’ social networks shape the ways people manage their health (28). This may be especially true for Mexican immigrants who, while often lacking financial and material resources, have robust social networks that are essential for the process of immigration, finding employment, and adapting to life in the U.S. (29–31). Among a sample of Latina immigrants, network ties – including friends, extended family, and key health care personnel – were essential conduits of information and other resources vital for enabling access to needed medical services (26). Among Latino immigrants that experience language as a barrier to accessing services, community and other network relationships also serve as crucial resources when seeking care (15, 26, 11).
Research on help-seeking behaviors examines utilization of mental health services (26), emergency care services (33), and preventive care (34), and has revealed the significance of social networks on outcomes ranging from treatment seeking to compliance and treatment completion. Yet, research has been slow to emerge in the study of oral health. By relying on broadly conceived notions of social support and social capital, what is known provides an incomplete picture of what and how network factors contribute to seeking DHS. For instance, Nahouraii and colleagues found that among Latina immigrant mothers, receiving social support was strongly associated with their children having had a recent dental visit (35). Research among geriatric Chinese immigrants also revealed that contact frequency with friends corresponded to a greater number of dental visits (36), with another study finding similar patterns among non-immigrant elderly adults (37). The findings of these studies hint at the link between social networks and use of dental health services, but fail to reveal the structural network features and mechanisms at work.
Further, the role of social networks in shaping the health behaviors of Mexican immigrant populations cannot be assumed to follow the same trends as other groups. Past research has shown that the cultural context of Latino populations may shape both the structure and function of their network ties (38). As vulnerable and disadvantaged populations mobilize their available resources, they also face external factors that shape how they make use of these resources. For example, fear of deportation, imperfect knowledge about the medical system of the United States, and poor English proficiency may motivate Mexican immigrants to rely on lay networks rather than seeking formal health care – even in the presence of relatively severe health problems.
The promise of preliminary studies examining social relationships and dental service utilization, and the empirical work linking networks and help-seeking to other types of health services, underscore the need for further research in this area. Unanswered questions about the role of cultural factors and social relationships and their connection to oral health behaviors among Mexican immigrants also warrant further investigation. Using data from 332 Mexican immigrants living (egos) in the Midwestern United States, we attend to these gaps in the current literature. The purpose of this paper is to examine the significance of both individual and egocentric network characteristics on formal DHS utilization. Namely, two key research questions are addressed. First, what is the relationship between individuals’ sociodemographic and oral health status/attitudes and their use of formal oral health services? Second, what role do individuals’ egocentric networks play in shaping their use of formal oral health services? Specifically, in addition to individual status and health, this paper considers the role of network characteristics that may have particular relevance for oral health help-seeking – including the size of individuals’ networks, their level of dental knowledge, and the frequency with which they discuss acute dental problems with these ties.
Methods
Participants and Data Collection
Data for this research are from the Tala Survey Study, designed to capture egocentric network data on Mexican immigrants (MAs) living in the Midwestern United States. A total of 332 MAs (egos) were surveyed, gathering data on their oral health and important matters networks (alters), health behaviors, diet, and oral health attitudes. Recruitment was conducted in 2013 and 2014 at churches and other community organizations made up of primarily Hispanic populations. Volunteers were solicited by study staff, and pen and paper and in-person interviewers were conducted, lasting 20 to 45 minutes. Eligibility criteria included willingness to participate and ability to read and write in either English or Spanish. Institutional Review Board approval and a Certificate of Confidentiality were obtained.
Measures
Dependent variables
To assess use of DHS, two dependent variables are examined. First, participants who “ever had dental treatment” are coded 1 (70%), while those who had not are coded 0 (30%). Duration since respondents’ last dental visit is also calculated, and those who have seen a dentist in the past 12 months are coded 1 (41%), while all others are coded 0 (59%).
Ego sociodemographic variables
Sociodemographic variables are used as controls. Participant gender is coded 1 for female (63%) and 0 for male, age is coded in years (x̄=36.26, SD=12.20). Education is coded 1 for participants who had at least a high school degree (42%), else 0. About 63% of participants are married, while approximately 36% have dental insurance. Given the population examined, years spent in the United States (logged) is included (x̄=2.70, SD=0.57).
Ego oral health status and attitudes variables
Because health need play a role in utilization of health services, a measure of oral health status is used. Self-rated condition of teeth and gums is coded 1 from participants with good, very good, and excellent condition (35%), and 0 for poor or fair condition (64%; including <3% with no natural teeth). A measure of dental fatalism is included (33). This is determined by participants stating their level of agreement on a Likert-type scale (strongly disagree [1] to strongly agree [5]) with the statement “Most children will eventually have cavities/caries” (x̄=4.13, SD=1.24). Finally, a composite measure of oral health behaviors is used, which combines frequency of brushing, flossing, and mouthwash practices. To create the composite scores, these three items are added together, with scores ranging from 0 to 6. Based on the frequency distribution, the sample is divided into low, medium, and high groups. Those with an overall score of 0 to 2 are coded as low (35%), those scoring 3 are medium (32%; reference category), and those with scores of 4 to 6 are coded as high (33%).
Network characteristics
Using network name generators, respondents (egos) provide the names of ties (alters) with whom they discussed “matters that are important” (important matters network) and issues about dental health that they could “really count on for help when you have dental health problems” in the past 12 months (oral health matters network). After egos provide alter names, additional characteristics on these ties and their relationship to egos are collected.
Six network characteristics are examined. Network size represents the total number of ties listed as part of both the important and oral health matters name generators, ranging from 0 (<1%) to 6 (9%; x̄=3.71). Mean network closeness is used to capture the strength of the relationship to alters, on average, within participants’ network. Scores range from 1 (not very close) to 3 (very close), with an average of 2.83. The proportion of alters having seen a dentist in the past year is also used to measure the influence of network norms on dental behavior (i.e., the direction of the “push” alters may exert on egos’ DHS use). Scores range from 0 (24%) to 100 (46%; x̄=61%), and are divided by 10 to create interpretable odds ratios. Mean dental health knowledge of network alters (as subjectively appraised by egos) is included to measure the strength of the “push” alters may exert on egos in terms of oral health help-seeking (e.g., the advice of alters perceived as “more knowledgeable” may have greater influence on behavior than that of less knowledgeable alters). Egos report how much alters know about “matters of teeth, gums, and mouth”, rating alters from 1 (no knowledge; 10%) to 4 (a lot of knowledge; 13%). Based on the distribution, low (34%), medium (37%; reference category), and high (29%) network dental knowledge categories are created.
Additionally, participants report the amount they talk with alters about dental issues, ranging from 1 (none; 15%) to 4 (several times; 12%), which also represents the mechanism through which alters may influence egos (i.e., more discussion may translate to greater influence). The mean score is calculated by adding the scores for each tie and dividing by the total number of ties (x̄=2.46, SD=0.97). Finally, the mean amount alters hassle participants regarding dental issues is also used to assess the extent to which networks “push” egos to respond to dental problems. Scores for each ego range from 1 (never; 14%) to 4 (a lot; 9%) (x̄=2.41, SD=0.91).
Analysis
To examine significant differences between those who had seen a dentist in the past year and those who had not, we conduct bivariate analyses. Logistic regression for binary outcomes is used with results presented as odds ratios (OR). Regression analyses are undertaken using a stepwise approach, where groups of related variables are examined in restricted models without other covariates, with a final model that includes all variables. Multicollinearity is tested using variance inflation factors. Predicted probabilities are also used to visualize key findings. All analyses are conducted in STATA version 13.1 and ENet Software (39).
Results
Bivariate results
Table 1 shows results of bivariate statistics comparing participants who have seen a dentist in the past year and those who have not. Compared to those who have not seen a dentist in the past year, those who have are more likely to have ever had dental treatment (p<0.001). On average, those who have seen a dentist in the past year are significantly more likely to have at least a high school degree (p<0.001), dental insurance (p<0.001), and report they have good, very good, or excellent condition teeth (p<0.01). Conversely, those who have not seen a dentist in the past year, on average, tend to hold greater sentiments of dental fatalism.
Table 1.
Bivariate differences between participants who have seen a dentist/past year and those who have not
| Overall% or Mean | SD | Have Seen a Dentist/Past Year | Have Not Seen Dent. in Past Yr. | Test Statistic1 | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| N | Mean/Prop. | N | Mean/Prop. | ||||
| Ego Dental Health Service Utilizat. | |||||||
| Dental Treatment (Ever) | 70.21 % | 0.46 | 137 | 59.31 % | 94 | 40.69 % | *** |
| Ego Sociodemographics | |||||||
| Female | 62.95 % | 0.48 | 90 | 43.06 % | 119 | 56.94 % | |
| Age | 36.26 | 12.20 | 134 | 35.51 | 195 | 36.77 | |
| Education (HS Grad) | 42.17 % | 0.49 | 78 | 55.71 % | 62 | 44.29 % | *** |
| Married | 62.65 % | 0.48 | 88 | 64.23 % | 112 | 62.57 % | |
| Years in US (logged) | 2.70 | 0.57 | 136 | 2.74 | 195 | 2.67 | |
| Dental Insurance | 35.56 % | 0.48 | 77 | 65.81 % | 40 | 34.19 % | *** |
| Ego Oral Health Status/Attitudes | |||||||
| Good/V.Good/Ex. Teeth/Gums | 35.54 % | 0.48 | 63 | 53.39 % | 55 | 46.61 % | ** |
| Dental fatalism | 4.13 | 1.24 | 137 | 3.97 | 178 | 4.24 | * |
| Oral Health Behaviors: | |||||||
| Low | 35.11 % | 0.48 | 41 | 36.61 % | 71 | 63.39 % | |
| Med. | 31.97 % | 0.47 | 41 | 40.20 % | 61 | 59.80 % | |
| High | 32.92 % | 0.47 | 49 | 46.67 % | 56 | 53.33 % | |
| Network Characteristics | |||||||
| Network Size [0 – 6+] | 3.71 | 1.48 | 137 | 4.00 | 195 | 3.51 | ** |
| Mean Network Closeness [1 – 3] | 2.83 | 0.35 | 136 | 2.80 | 195 | 2.85 | |
| Prop. Dental Visit/Yr. | 61.28 % | 41.92 | 137 | 70.43 % | 195 | 54.85 % | *** |
| Dental Health Knowledge: | |||||||
| Low | 34.26 % | 0.48 | 34 | 30.63 % | 77 | 69.37 % | ** |
| Med. | 37.04 % | 0.48 | 54 | 45.00 % | 66 | 55.00 % | |
| High | 28.70 % | 0.45 | 48 | 51.61 % | 45 | 48.39 % | * |
| Mean Talk Acute Problems [1 – 4] | 2.46 | 0.97 | 134 | 2.46 | 185 | 2.46 | |
| Mean Hassles Dent. Issues [1 – 4] | 2.41 | 0.91 | 134 | 2.33 | 189 | 2.46 | |
|
| |||||||
| N (of total 332) | 316 | 137 | 43.35 | 179 | 56.65 | ||
p < 0.05;
p < 0.01;
p < 0.001
Test statistics examined include the Wicoxon-Mann-Whitney test statistic for interval or ordinal variables; Chi-square test and Fisher’s exact test are used for categorical variables.
In terms of network characteristics, respondents who have seen a dentist in the past year have larger networks than those who have not (p<0.01). Those who have gone to the dentist also have networks, on average, with a greater proportion of ties having also seen a dentist in the past year (p<0.001). In terms of dental knowledge, egos who report having not seen a dentist in the past year are more likely to have networks with low mean dental knowledge (p<0.01), while those who have seen a dentist are more likely to have networks with high mean dental knowledge (p<0.05).
Multivariate results for ego characteristics
Tables 2 and 3 present logistic regression results for four models testing key relationships of interest, including three restricted models examining ego sociodemographics, ego oral health status/attitudes, and network characteristics, and a final model including all independent variables.
Table 2.
Logistic regression of ever had dental treatment on ego and network characteristics
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Ego Sociodemographics | ||||
| Female | 0.78 (0.21) | — | — | 0.64 (0.22) |
| Age | 1.01 (0.01) | — | — | 1.02 (0.02) |
| Education (HS Grad) | 2.54 (0.75)** | — | — | 2.72 (1.01)** |
| Married | 0.91 (0.26) | — | — | 1.08 (0.36) |
| Years in US (logged) | 1.61 (0.38)* | — | — | 1.46 (0.40) |
| Dental Insurance | 4.15 (1.38)*** | — | — | 2.74 (1.05)** |
| Ego Oral Health Status/Attitudes | ||||
| Good/V.Good/Ex. Teeth/Gums | — | 2.31 (0.67)** | — | 1.53 (0.54) |
| Dental fatalism | — | 0.76 (0.09)* | — | 0.78 (0.11) |
| Oral Health Behaviors: | ||||
| Low | — | 1.00 (0.30) | — | 0.91 (0.34) |
| High | — | 1.58 (0.51) | — | 1.01 (0.40) |
| Network Characteristics | ||||
| Network Size | — | — | 1.16 (0.11) | 1.14 (0.13) |
| Mean Network Closeness | — | — | 0.33 (0.17)* | 0.41 (0.23) |
| Proportion See Dent./Past Year | — | — | 1.08 (0.04)* | 1.07 (0.04) |
| Mean Dental Knowledge: | ||||
| Low | — | — | 0.29 (0.10)*** | 0.23 (0.09)*** |
| High | — | — | 0.55 (0.20) | 0.42 (0.18)* |
| Mean Talk Acute Problems | — | — | 1.32 (0.21) | 1.45 (0.27)* |
| Mean Hassles Dent. Issues | — | — | 0.86 (0.14) | 0.77 (0.15) |
|
| ||||
| N | 322 | 315 | 309 | 281 |
| LR χ2 | 45.44*** | 19.85*** | 41.46*** | 76.20*** |
| Pseudo R2 | 0.12 | 0.05 | 0.11 | 0.22 |
Odds ratios presented, standard errors in parentheses
p < 0.05 = *; p < 0.01 = **; p < 0.001 = ***
Supplant
Table 3.
Logistic regression of past year dental visit on ego and network characteristics
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Ego Sociodemographics | ||||
| Female | 1.09 (0.28) | — | — | 1.14 (0.34) |
| Age | 1.00 (0.01) | — | — | 1.00 (0.01) |
| Education (HS Grad) | 2.16 (0.57)** | — | — | 1.53 (0.47) |
| Married | 1.25 (0.34) | — | — | 1.41 (0.44) |
| Years in US (logged) | 1.20 (0.27) | — | — | 1.13 (0.29) |
| Dental Insurance | 4.16 (1.08)*** | — | — | 2.61 (0.77)*** |
| Ego Oral Health Status/Attitudes | ||||
| Good/V.Good/Ex. Teeth/Gums | — | 2.11 (0.51)** | — | 1.87 (0.55)* |
| Dental fatalism | — | 0.89 (0.08) | — | 0.90 (0.10) |
| Oral Health Behaviors: | ||||
| Low | — | 0.87 (0.25) | — | 0.96 (0.33) |
| High | — | 1.34 (0.39) | — | 1.07 (0.36) |
| Network Characteristics | ||||
| Network Size | — | — | 1.18 (0.10)* | 1.14 (0.11) |
| Mean Network Closeness | — | — | 0.61 (0.24) | 0.65 (0.29) |
| Proportion See Dent./Past Year | — | — | 1.08 (0.03)** | 1.07 (0.04) |
| Mean Dental Knowledge: | ||||
| Low | — | — | 0.69 (0.21) | 0.75 (0.27) |
| High | — | — | 1.43 (0.42) | 1.52 (0.52) |
| Mean Talk Acute Problems | — | — | 1.09 (0.15) | 1.12 (0.18) |
| Mean Hassles Dent. Issues | — | — | 0.69 (0.10)* | 0.70 (0.12)* |
|
| ||||
| N | 325 | 318 | 311 | 283 |
| LR χ2 | 53.50*** | 14.11** | 27.21*** | 56.35*** |
| Pseudo R2 | 0.12 | 0.03 | 0.06 | 0.15 |
Odds ratios presented, standard errors in parentheses
p < 0.05 = *; p < 0.01 = **; p < 0.001 = ***
Findings indicate that MAs’ sociodemographic characteristics are significantly associated with DHS utilization. For both receipt of dental treatment and past year dental visit, those with a high school or greater education have greater odds of using of dental services, net covariates (OR=2.72, p≤0.01 and OR=2.16, p≤0.01, respectively). Further, those with dental insurance also have greater odds of using dental health services (OR=2.74, p≤0.01 and OR=2.61, p≤0.001). Results indicate that as years in the U.S. increase, odds of ever having dental treatment also increase, net covariates, though this is significant only in the restricted model (OR=1.61, p≤0.05).
Ego oral health status and attitudes are also significant predictors of help-seeking for oral health problems. Specifically, compared to those with teeth and gums in fair or poor condition, those reporting good, very good, and excellent condition have greater estimated odds of reporting dental treatment in their lifetime (OR=2.31, p≤0.01) and a past year dental visit (OR=1.87, p≤0.05), all else equal. Additionally, as dental fatalism score increases, odds of reporting ever receiving dental treatment decrease (OR=0.76, p≤0.05; only in the restricted model).
Multivariate results for network characteristics
This research also provides strong evidence that MA immigrants’ social networks are associated with DHS utilization. First, in a restricted model, as network size increases, so too do the odds of having seen a dentist in the past year (OR=1.18, p≤0.05). Similarly, in the restricted models, as the proportion of egos’ network that has seen a dentist in the past year increases, so do the odds that they have ever had dental treatment (OR=1.08, p≤0.05) or seen a dentist in the past year (OR=1.08, p≤0.05). In contrast, as mean network closeness increases, the odds of ever having had dental treatment decrease (OR=0.33, p≤0.05), though this relationship is only significant in the restricted model.
Network dental knowledge is also correlated with egos’ utilization of dental health services. Compared to egos who have networks with a medium level of dental knowledge, those with a low or high level of network dental knowledge have lower odds of ever having dental treatment, net covariates (OR=0.23, p≤0.001 and OR=0.42, p≤0.05, respectively). Increases in network discussion regarding acute dental problems correspond to greater odds of ever having dental treatment (OR=1.45, p≤0.05), while increases in network hassling regarding dental issues are associated with lower odds of having seen a dentist (OR=0.70, p≤0.05).
Predicted probability
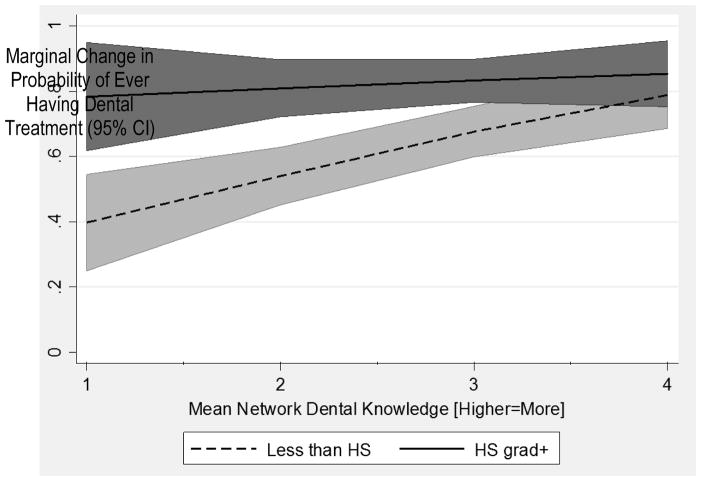
The delta method is used to illustrate the magnitude of the interaction effects of ego education by average network dental knowledge on the probability of having dental treatment (Figure 1). For both egos with less than a high school education and those with a high school education or greater, as network dental knowledge increases, so do the odds of getting treatment. However, for egos with less than a high school education, increases in alter dental knowledge have a more dramatic impact on the probability of seeking dental treatment, while this effect is more modest for those with more education. Notably, as indicated by the y-intercept, egos with a higher level of education have a greater probability of getting dental treatment in the absence of knowledgeable networks than those with lower educational attainment.
Figure 1.
Effects of ego education over mean network dental knowledge
NOTE: Shaded areas represent confidence intervals.
Discussion
The primary goal of this research is to examine use of dental health services among a Mexican immigrant population in the American Midwest, focusing on social network characteristics. Findings indicate that traditional correlates of help-seeking like health insurance and health need influence the use of DHS. As in previous studies, insurance and education correspond to greater use of health services (8, 9, 40). Better oral health is also associated with greater odds of using dental health services – an effect which may be indicative of reverse causation or may be due to a confounding factor such as concern for oral health. Importantly, this research reveals that aspects of Mexican American immigrants’ social networks are significantly linked to use of health services, in some instances promoting and in other instances deterring use of DHS. These patterns are highly unlikely to be due to reverse causation since use of DHS probably does not influence relationship formation or interpersonal processes, and other confounding factors like education are controlled.
In terms of promoting use, results indicate that network size and frequency of discussion with ties regarding acute dental problems correspond to a greater likelihood of having a dental visit in the past year and having ever had dental treatment, respectively. These findings do not hold across all models, but they are likely indicative of support and advice seeking (41) by egos while managing their health. Though past research indicates that larger networks do not always translate to greater engagement with health services (42), in the case of oral health among the MA respondents in this study, it appears that in the context of larger networks where individuals discuss their acute oral health problems with greater frequency, networks may encourage use of DHS (43). It is possible that network ties feel less able or willing to proffer advice about managing specialized health concerns like oral health – whereas they may feel more capable or confident offering advice on more general health matters – thereby, directing them to formal services instead. It may also be that individuals do not discuss oral health and oral health problems until they become relatively severe, prompting ties to encourage the use of more formal health services to manage exigent problems. Though it is possible to speculate about the mechanisms driving these findings, further research is needed to explore theorized connections.
Similarly, having a greater proportion of network ties who have seen a dentist themselves in the past year also positively corresponds to DHS utilization in the restricted models. It may be – as suggested in previous research of other types of health service utilization (44) – that in the context of networks where ties use DHS, such behavior is normalized and alters direct egos to seek services when facing health problems. Rather than normative influence, it may also be that ties who regularly use health service possess valuable information (43) about where and how to access health services, transmitting this beneficial knowledge to egos. Given the role that unfamiliarity with the U.S. health care system plays in dissuading utilization among MAs (10), alters that can lend their experience of accessing services may be an essential resource for getting those with oral health needs into care.
Findings of this study also reveal that network characteristics may, in some instances, correspond to a lower likelihood of seeking DHS. Though the measure was only significant in a single restricted model, that closer networks are linked to a lower likelihood of ever having had dental treatment may signal that particularly dense networks serve as conduits of oral health advice, in some instances supplanting dentists or other more formal sources of dental information, treatment, and care. Other research examining different types of health service utilization (e.g. use of mental health services, preventive care, etc.) among minority populations has revealed similar patterns (42, 45), suggesting that this may be a common trend in tight-knit, racial and ethnic minority communities. It may also be that closer networks are more effective at regulating individuals’ health behaviors and promoting positive behaviors (e.g. regular brushing, better dietary habits), driving lower need among those with more closely knit networks for formal health services. Finally, closeness may co-vary with other indicators that influence use of DHS, such as marital status or years in the United States, which might explain why it achieves significance only in the restricted model.
Another network resource that emerged as significant in these analyses is dental knowledge. Generally, MAs embedded in networks with low dental knowledge have lower odds of DHS utilization. As has been suggested in past research, such networks may provide little or counterproductive advice (46) regarding health behaviors (e.g., less encouragement to use dental services, even when needed) or be incapable of identifying significant problems that warrant medical intervention (32). Interestingly, egos with high dental knowledge networks, in comparison to those with a medium level, are also less likely to report having dental treatment. This may indicate, as previously suggested, that these ties are being substituted (47) in place of formal providers for advice and management of oral health. It may also be that those more inclined to use dental health services are less likely to identify network ties as highly knowledgeable.
Importantly, results also reveal that the effect of access to knowledge through networks is dependent on egos’ own level of education. That is, for MAs with greater educational attainment, alter dental knowledge has a more modest impact on the odds they will have had dental treatment. Conversely, among egos with lower educational attainment, network dental knowledge has a more pronounced positive effect on the odds they have had treatment. These trends may occur because educated egos have greater odds of using formal health services to begin with, so alter knowledge is less influential. In network terms, alters likely provide less novel information to more educated MAs, therefore the added value of their knowledge has a lesser effect on dental treatment seeking. More educated egos may also be more wary when evaluating lay knowledge, preferring to seek out formal caregivers instead. Further research is needed to determine the mechanisms underlying these relationships.
Though these novel findings represent a significant contribution to the current literature, this study is not without limitations. Because the data used are cross-sectional, causal claims cannot be made. Additional longitudinal research with MAs is needed to gain a better understanding of the potential network mechanisms driving health behaviors. That said, this study provides a preliminary basis for future research efforts in this area, suggesting that networks serve as a critical resource for immigrants: providing advice, transmitting knowledge about oral health, and shaping engagement with DHS providers. In all, this research justifies the need for systematic investigations of the roles social networks play in shaping oral health and health behaviors among vulnerable populations.
Implications and Conclusions
In all, the current study expands what is known about the relationship between social network factors and DHS utilization among Mexican immigrants to the American Midwest. It is only recently that dental health research has begun to acknowledge that social contexts play a significant role in shaping individuals’ behaviors, health status, and overall wellbeing. This study initiates an important conversation about the role of social relationships in shaping immigrants’ use of dental health services. Research drawing on social network perspectives and using network methodologies provides a more nuanced and comprehensive examination of this context, so that the pathways and mechanisms underlying these relationships can be disentangled. It is well established that immigrants use health care less frequently and receive lower quality care than individuals native to the United States (48). Identifying the pathways that prohibit and promote use of services among this population provides important clues as to how efforts to improve health promotion and link individuals to needed services may be supported. Given the especially important role that such relationships play in the lives of immigrants settling in a new environment, largely separated from the pre-immigration networks and sources of care, research of this kind may be particularly salient for this population.
There are also a number of significant policy implications of this research, especially given the key findings that more affluent, educated, and connected individuals are more likely to use oral health care. Recent changes under the Trump administration – including efforts to repeal the Affordable Care Act and increased negative attention to both documented and undocumented immigrants – imperil health insurance coverage and discourage the use of needed health services by immigrant populations. However, some states and communities are currently making efforts to provide documented and undocumented immigrants opportunities to live productive, healthful lives. Since the 1980s, loosely classified ‘sanctuary’ cities and states have adopted policies (e.g. granting government-issued identification cards, omitting questions about legal status from public forms and within public agencies) that promote greater engagement with public services and work to minimize the risks associated with seeking needed financial and health services (49). In addition to creating a more accessible pathway to oral and other types of health care, ‘sanctuary’ cities and states may also indirectly promote the kind of social network building and social integration that benefits immigrants and non-immigrants alike within these communities.
In 2016, New York State implemented the Basic Health Program (BHP) that provides low-income, legally residing populations with a low-cost health insurance option (50). So far, this program has been a success for the state: nearly 500,000 New Yorkers enrolled and the program has generated an estimated one billion dollars in state savings. A recent report generated by the Task Force on Immigrant Health Care Access under the direction of New York City mayor Bill de Blasio suggests that future savings from the BHP could be used to expand the program to provide comprehensive care to undocumented immigrants not currently eligible for BHP or other coverage (51). Programs such as these serve to minimize the barriers immigrants experience to accessing care by investing in the development of culturally and linguistically proficient providers and agencies, and by conducting outreach to educate immigrants and immigrant service organizations about these options. These types of programs appear important to support health outcomes given the findings of the present research (50, 51).
Acknowledgments
This research was funded by NIDCR grant DE022096-01A1, and by Project Development Team studies UL1TR001108 and RR025761 from the Indiana Clinical and Translational Sciences Institute. The authors declare they have no conflicts of interest.
Footnotes
Compliance with Ethical Standards
All procedures performed involving human participants were in accordance with the ethical standards of the institutional review committee and with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study. Additionally, participants in this study were protected by a Federal Certificate of Confidentiality obtained by the Principal Investigator.
Contributor Information
Erin Pullen, Indiana University, Bloomington, Indiana University Network Science Institute, 1001 E State 45/46 Bypass, Bloomington, IN 47408, Phone: (812) 855-6293, Fax: (812) 855-5090.
Brea L. Perry, Indiana University, Bloomington, Department of Sociology/Indiana University Network Science Institute, 1020 E Kirkwood Avenue, Balantine Hall 767, Bloomington IN 47405, Phone: (812) 855-5920, Fax: (812) 856-1192
Gerardo Maupome, Indiana University/Purdue University at Indianapolis, School of Dentistry/Indiana University Network Science Institute, 415 Lansing St., Indianapolis IN 46077, Phone: (317) 274-5529, Fax: (317) 278-1834.
References
- 1.Brown A, Stepler R. Statistical portrait of the foreign-born population in the United States. Pew Research Center Hispanic Trends. 2015 Sep; Available at: http://www.pewhispanic.org/files/2015/09/Statistical-Portrait-of-the-Foreign-Born-2013_09-2015.pdf\.
- 2.Krogstad JM, Lopez MH. Hispanic nativity shift: U.S. births drive population growth as immigration stalls. 2014 Apr; Available at: http://www.pewhispanic.org/2014/04/29/hispanic-nativity-shift/
- 3.Bustamante AV, et al. Variations in healthcare access and utilization among Mexican immigrants: the role of documentation status. J Immigrant Minority Health. 2012;14(1):146–155. doi: 10.1007/s10903-010-9406-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wallace SP, et al. Heading south: why Mexican immigrants in California seek health services in Mexico. Med Care. 2009;47(6):662–9. doi: 10.1097/MLR.0b013e318190cc95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bergmark R, et al. ices. J Immigr Minor Health. 2010;12(4):610–4. doi: 10.1007/s10903-008-9213-8. [DOI] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. [Google Scholar]
- 7.Andersen RM. Behavioral Model of Families’ Use of Health Services. Chicago, IL: Center for Health Administration Studies; 1968. Research Series No. 25. [Google Scholar]
- 8.Finlayson TL, et al. Dental utilization among Hispanic adults in agricultural worker families in California’s Central Valley. J Public Health Dent. 2010;70(4):292–9. doi: 10.1111/j.1752-7325.2010.00184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown A, Patten E. Statistical portrait of Hispanics in the United States, 2012. Pew Research Center Hispanic Trends. 2014 Apr; Available at: http://www.pewhispanic.org/2014/04/29/statistical-portrait-of-hispanics-in-the-united-states-2012/
- 10.Arcury TA, Quandt SA. Delivery of health services to migrant and seasonal farmworkers. Annu Rev Public Health. 2007;28:345–63. doi: 10.1146/annurev.publhealth.27.021405.102106. [DOI] [PubMed] [Google Scholar]
- 11.Butani Y, et al. Oral health-related cultural beliefs for four racial/ethnic groups: assessment of the literature. BMC Oral Health. 2008;8:26. doi: 10.1186/1472-6831-8-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramos-Gomez FJ, et al. Assessment of early childhood caries and dietary habits in a population of migrant Hispanic children in Stockton, California. ASDC J Dent for Child. 1999;66(6):395–403. [PubMed] [Google Scholar]
- 13.Documét PI, Sharma RK. Latinos’ health care access: financial and cultural barriers. J Immigr Health. 2004;6(1):5–13. doi: 10.1023/B:JOIH.0000014638.87569.2e. [DOI] [PubMed] [Google Scholar]
- 14.Patrick DL, et al. Reducing oral health disparities: a focus on social and cultural determinants. BMC Oral Health. 2006;6(S1):S4. doi: 10.1186/1472-6831-6-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perez-Escamilla R, et al. Health care access among Hispanic immigrants: ¿Alguien está escuchando? NAPA Bull. 2010;34(1):47–67. doi: 10.1111/j.1556-4797.2010.01051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castañeda H, et al. False hope: effects of social class and health policy on oral health inequalities for migrant farmworker families. Soc Sci Med. 2010;71(11):2028–37. doi: 10.1016/j.socscimed.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 17.Willems S, et al. The independent impact of household and neighborhood-based social determinants on early childhood caries: a cross-sectional study of inner-city children. Family Community Health. 2005;28:168–175. doi: 10.1097/00003727-200504000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Pescosolido B. Beyond rational choice - the social dynamics of how people seek help. Am J Sociol. 1992;97(4):1096–138. [Google Scholar]
- 19.Friedson E. Professional Dominance. Chicago, Illinois: Aldine; 1970. [Google Scholar]
- 20.Gallo LC, et al. Resiliency in the face of disadvantage: Do Hispanic cultural characteristics protect health outcomes? J Pers. 2009;77(6):1707–46. doi: 10.1111/j.1467-6494.2009.00598.x. [DOI] [PubMed] [Google Scholar]
- 21.Finlayson TL, et al. Reliability and validity of brief measures of oral health-related knowledge, fatalism, and self-efficacy in mother of African American children. Pediatr Dent. 2005;27(5):422–428. [PMC free article] [PubMed] [Google Scholar]
- 22.Woolfolk MP, et al. Self-reported health behavior and dental knowledge of a migrant worker population. Community Dent Oral Epidemiol. 1985;13(3):140–142. doi: 10.1111/j.1600-0528.1985.tb00429.x. [DOI] [PubMed] [Google Scholar]
- 23.Watson MR, et al. Caries conditions among 2–5-year old immigrant Latino children related to parents’ oral health knowledge, opinions and practices. Community Dent Oral Epidemiol. 1999;27(1):8–15. doi: 10.1111/j.1600-0528.1999.tb01986.x. [DOI] [PubMed] [Google Scholar]
- 24.Arredondo EM, et al. Is church attendance associated with Latinas’ health practices and self-reported health? Am J Health Behavior. 29:502–511. doi: 10.5555/ajhb.2005.29.6.502. [DOI] [PubMed] [Google Scholar]
- 25.Otero-Sabogal R, et al. Access and attitudinal factors related to breast and cervical cancer screening: Why are Latinas still underscreened? Health Educ and Behav. 30:337–359. doi: 10.1177/1090198103030003008. [DOI] [PubMed] [Google Scholar]
- 26.Derose KP. Networks of care: how Latina immigrants find their way to and through a county hospital. J Immigr Health. 2000;2(2):79–87. doi: 10.1023/A:1009533901752. [DOI] [PubMed] [Google Scholar]
- 27.Batra M, et al. Social capital and oral health. J Clin Diagn Res. 2014;8(9):ZE10–ZE11. doi: 10.7860/JCDR/2014/9330.4900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Olafsdottir S, Pescosolido BA. Drawing the line: the cultural cartography of utilization recommendation for mental health problem. J Health Soc Behav. 2009 Jun;50(2):228–44. doi: 10.1177/002214650905000208. [DOI] [PubMed] [Google Scholar]
- 29.Hagan JM. Social networks, gender, and immigrant incorporation: resources and constraints. Am Sociol Review. 1998;63(1):55–67. [Google Scholar]
- 30.Andersson F, et al. Discussion Paper Series: Institute for the Study of Labor (IZA) 4423. Bonn, Germany: 2009. Do as the neighbors do: the impact of social networks on immigrant employment. [Google Scholar]
- 31.Poros M. Migrant social networks: vehicles for migration, integration, and development. Migration Information Source: The Online Journal of the Migration Policy Institute. 2011 Mar; Available at: http://www.migrationpolicy.org/article/migrant-social-networks-vehicles-migration-integration-and-development.
- 32.Pescosolido BA, et al. Social networks and patterns of use among the poor with mental health problems in Puerto Rico. Med Care. 1998;36(7):1057–72. doi: 10.1097/00005650-199807000-00012. [DOI] [PubMed] [Google Scholar]
- 33.Kangovi S, et al. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Health Aff. 2013;32(7):1196–203. doi: 10.1377/hlthaff.2012.0825. [DOI] [PubMed] [Google Scholar]
- 34.Suarez L, et al. Social networks and cancer screening in four U.S. Hispanic groups. Am J Prev Med. 2000;19(1):47–52. doi: 10.1016/s0749-3797(00)00155-0. [DOI] [PubMed] [Google Scholar]
- 35.Nahouraii H, et al. Social support and dental utilization among children of Latina immigrants. J Health Care Poor Underserved. 2008;19(2):428–41. doi: 10.1353/hpu.0.0017. [DOI] [PubMed] [Google Scholar]
- 36.Wu B, et al. Comparison of utilization of dental care services among Chinese- and Russian-speaking immigrant elders. J Public Health Dent. 2005;65(2):97–103. doi: 10.1111/j.1752-7325.2005.tb02793.x. [DOI] [PubMed] [Google Scholar]
- 37.Burr JA, Lee HJ. Social relationships and dental care service utilization among older adults. J Aging Health. 2013;25(2):191–220. doi: 10.1177/0898264312464497. [DOI] [PubMed] [Google Scholar]
- 38.Pescosolido BA, et al. Social networks and patterns of use among poor with mental health problems in Puerto Rico. Med Care. 36(7):1057–72. doi: 10.1097/00005650-199807000-00012. [DOI] [PubMed] [Google Scholar]
- 39.Borgatti SP. E-network software for ego-network analysis. Lexington: Analytic Technologies; 2006. [Google Scholar]
- 40.Finlayson TL, et al. Dental utilization by children in Hispanic agricultural worker families in California. 2014;2(1–2):15–24. [PMC free article] [PubMed] [Google Scholar]
- 41.Perry BL, Pescosolido BA. Social network activation: the role of health discussion partners in recovery from mental illness. Soc Sci Med. 2015;125:116–28. doi: 10.1016/j.socscimed.2013.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pescosolido BA, et al. Social networks and patterns of use among the poor with mental health problems in Puerto Rico. Med Care. 1998;36(7):1057–72. doi: 10.1097/00005650-199807000-00012. [DOI] [PubMed] [Google Scholar]
- 43.Devillanova C. Social networks, information and health care utilization: Evidence from undocumented immigrants in Milan. J Health Econ. 2008;27(2):265–86. doi: 10.1016/j.jhealeco.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 44.Vogel DL, et al. Seeking help from a mental health professional: The influence of one’s social network. J Clin Psychol. 2007;63(3):233–45. doi: 10.1002/jclp.20345. [DOI] [PubMed] [Google Scholar]
- 45.Pullen E, et al. African American women’s preventative care usage: The role of social support and racial experiences and attitudes. Sociol Health Illn. 2014;36(7):1037–53. doi: 10.1111/1467-9566.12141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thoits P. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. 2011;52(2):145–61. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- 47.Thoits P. Perceived social support and the voluntary, mixed, and pressured use of mental health services. Soc Ment Health. 2011;1(1):4–19. [Google Scholar]
- 48.Derose KP, et al. Immigrants and health care: Sources of vulnerability. Health Affairs. 2007;26(2):1258–68. doi: 10.1377/hlthaff.26.5.1258. [DOI] [PubMed] [Google Scholar]
- 49.Villazor RC. What is a sanctuary. SMU Law Review. 2008;61:133–156. [Google Scholar]
- 50.Barrios-Paoli L. Improving immigrant access to health care in New York City: A report from the mayor’s task force on immigrant health care access. 2016 Available at: http://www1.nyc.gov/assets/home/downloads/pdf/reports/2015/immigrant-health-task-force-report.pdf.
- 51.New York State Department of Health (NYS DOH) Basic health contingency plan. 2016 Available at: https://www.health.ny.gov/health_care/managed_care/essential/2016_contingency_plan.htm.