Abstract
Multiple myeloma has been reported to be associated with rheumatoid arthritis (RA). POEMS syndrome is a rare variant of multiple myeloma and is characterised by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin changes. We report the case of a 67-year-old patient with RA who developed numbness and tingling in both legs due to polyneuropathy. CT showed a massive right pleural effusion and a sclerotic lesion in the right ninth rib. Histopathological examination of the rib revealed IgA lambda-type plasmacytoma. Serum vascular endothelial growth factor was extremely high at 5530 pg/mL. We made a diagnosis of POEMS syndrome. A literature search of the PubMed database identified only two documented cases of POEMS syndrome in patients with RA. Neuropathies are reportedly more frequent in patients with RA than in the general population. Rheumatologists should consider POEMS syndrome in patients with RA and neurological symptoms.
Keywords: rheumatoid arthritis, haematology (incl blood transfusion), peripheral nerve disease
Background
The risk of lymphoproliferative disorders, such as lymphoma, leukaemia or multiple myeloma, has been reported to be moderately increased by the presence of rheumatoid arthritis (RA). For example, the relative risk of lymphoma is two to six times higher in patients with RA than in the general population,1 and there have been a number of reports of multiple myeloma in elderly patients with RA.2–4 POEMS syndrome (also known as Crow-Fukase syndrome) is a rare variant of multiple myeloma characterised by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin changes. Here, we describe an interesting case of POEMS syndrome in a patient with RA.
Case presentation
A 67-year-old Japanese man with RA was referred to our clinic with right pleural effusion and a 4-month history of progressive difficulty in walking. He complained of numbness, tingling, decreased sensation and muscle weakness in both legs. The patient had a 3-year history of RA and was being treated with tacrolimus. On examination, his temperature was 37.1°C, blood pressure 123/74 mm Hg and pulse 80 bpm. On auscultation, breath sounds were decreased on the right. Neurological examination revealed the cranial nerves were normal. Sensory modalities and muscle strength were decreased symmetrically in the distal part of the legs. Skin examination revealed hyperpigmentation of the limbs and face, hypertrichosis of the limbs and haemangiomata distributed predominantly on the trunk. The patient had pedal oedema and a swollen right knee. No other swollen or tender joints were evident, and he was evaluated as having low clinical RA disease activity. He also had significant right cervical and axillary lymphadenopathy.
Investigations
Laboratory investigations revealed C reactive protein of 6.2 mg/L, haemoglobin of 13.5 g/dL, white blood cell count of 11.8×109/L (neutrophil count 9.3×109/L) and platelet count of 505×109/L. Serum albumin and lactate dehydrogenase were normal at 3.4 g/dL and 112 U/L, respectively. Serum total IgG, IgA and IgM were not elevated (1528 mg/dL, 294 mg/dL and 113 mg/dL, respectively). No M-protein was detected by immunoelectrophoresis. Rheumatoid factor and anticyclic citrullinated peptide antibody were both positive at 48 IU/mL (normal <20) and 5.7 U/mL (normal <5), respectively.
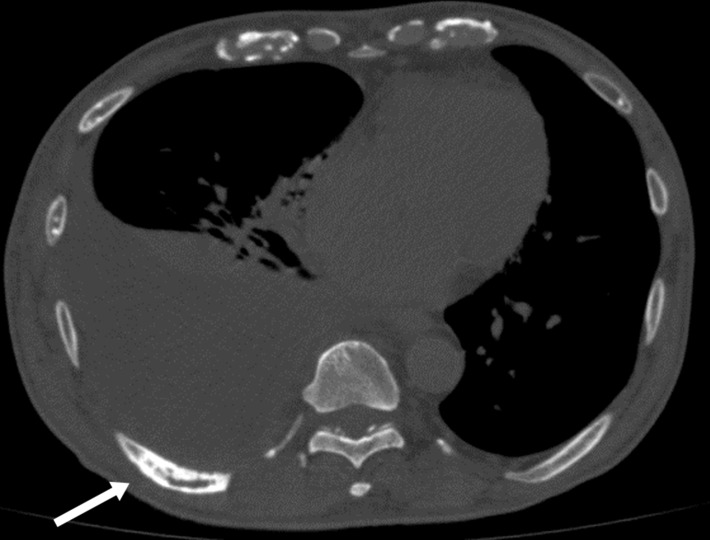
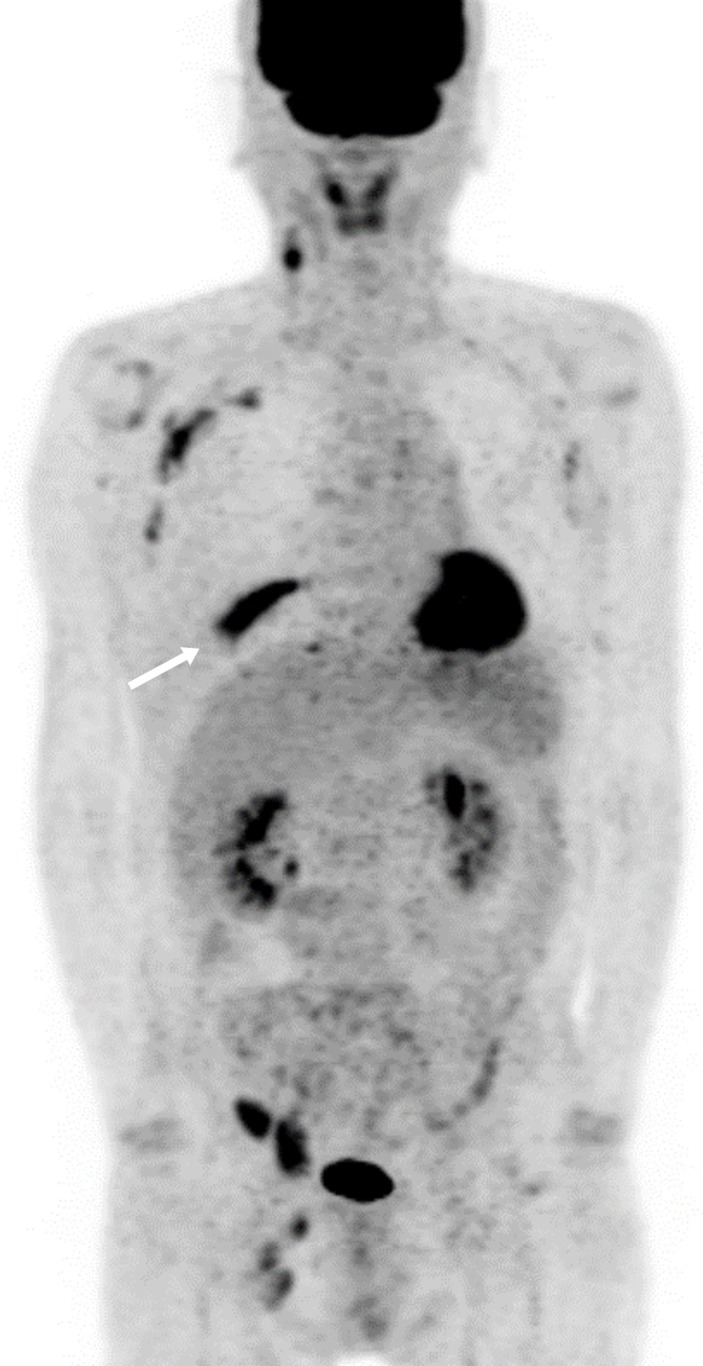
Nerve conduction study revealed marked symmetric reduction in median, ulnar, peroneal and tibial nerve velocities. Amplitude was also decreased, but not as much as velocity. These findings were suggestive of demyelinating polyneuropathy. CT of the chest showed a massive right pleural effusion and a sclerotic lesion in the right ninth rib (figure 1). 18F-fluoro-2-deoxyglucose-positron emission tomography-CT showed high accumulation in the right ninth rib and the cervical, axillary, iliac and inguinal lymph nodes (figure 2). The pleural effusion was transudative, and no malignant cells were seen on cytopathology. Right cervical lymph node biopsy revealed many lymphoid follicles with mantle zones and blood vessels penetrating into germinal centres, suggestive of Castleman disease. We performed partial resection of the right ninth rib, and histopathology revealed IgA lambda-type plasmacytoma. Preoperative serum vascular endothelial growth factor (VEGF) was extremely high at 5530 pg/mL (normal <707).
Figure 1.
CT showing a massive right pleural effusion and a sclerotic lesion in the right ninth rib (arrow).
Figure 2.
Positron emission tomography-CT showing increased tracer uptake in the right ninth rib (arrow) and in the cervical, axillary, iliac and inguinal lymph nodes.
Treatment
We made a diagnosis of POEMS syndrome and referred the patient to the haematology department for chemotherapy. He was started on lenalidomide 25 mg per day for 21 days of a 28-day cycle with dexamethasone 20 mg once weekly. At the time of writing, he had received 9 cycles of treatment over a period of 9 months.
Outcome and follow-up
After starting chemotherapy, the patient's neurological and muscle symptoms improved gradually but significantly. Six months later, serum VEGF had decreased to 786 pg/mL.
Discussion
POEMS syndrome is a rare lymphoproliferative disorder that causes multiorgan damage. The International Myeloma Working Group has defined specific diagnostic criteria for POEMS syndrome and, according to this definition, both monoclonal gammopathy and polyneuropathy are required for the diagnosis.5 Our patient had an osteosclerotic plasmacytoma in the rib and peripheral demyelinating polyneuropathy, and thus met the diagnostic criteria. The association between POEMS syndrome and Castleman disease is well known.5 Our patient also had POEMS-associated multicentric Castleman disease.6 Most patients with POEMS syndrome have skin manifestations. Our patient had hyperpigmentation, hypertrichosis and glomeruloid haemangiomata and reported that these symptoms had developed suddenly in the preceding months. Careful physical examination is required for accurate diagnosis of this syndrome.
A literature search of the PubMed database identified only two documented cases of POEMS syndrome in association with RA.7 8 The time interval between diagnosis of RA and onset of POEMS syndrome was 2 years in the first case and 18 years in the second case. These two patients presented with typical manifestations of POEMS syndrome, including polyneuropathy, monoclonal gammopathy, extravascular volume overload and cutaneous symptoms. In the second case, serum VEGF was elevated.
The mechanism underlying the multisystem organ manifestations of monoclonal gammopathy is not clear. Increased levels of inflammatory cytokines, including interleukin 6 and tumour necrosis factor alpha, have been reported, and cytokines are believed to play an important role in the pathogenesis of monoclonal gammopathy. Elevated serum VEGF is another characteristic feature of POEMS syndrome. VEGF is a potent inducer of vascular permeability and is produced by platelets and plasma cells.9 Serum VEGF levels are reportedly more than 5 to 10-fold higher in patients with POEMS syndrome compared with healthy controls.10 In our patient, serum VEGF was extremely high at 5530 pg/mL on admission and had decreased to 786 pg/mL 6 months after starting chemotherapy. This suggests that VEGF was either secreted by the plasmacytoma or that unknown factors produced by this tumour-induced platelet-derived production of VEGF.
POEMS syndrome runs a chronic clinical course and the long-term survival outcome is generally regarded as good.11 A study at the Mayo Clinic reported that younger age, albumin >3.2 g/dL and a complete haematological response were associated with superior overall survival.11 In our patient, serum albumin at the time of diagnosis was 3.4 g/dL (>3.2 g/dL). The haematological response to treatment was not evaluated since M-protein was not detected at diagnosis.
Neuropathies are reported to be more frequent in patients with RA than in the general population.12 Neurological symptoms are not severe in most cases, but combined sensorimotor neuropathy can occur in seropositive RA, particularly in male patients.13 The most common peripheral nerve involvement in RA is multiple mononeuritis.14 The typical initial presentation of POEMS syndrome is symmetric distal sensory loss or weakness, indicating polyneuropathy. The course of neuropathy is progressive, and some patients may become confined to a wheelchair. The findings in our patient emphasise the importance of early recognition of this syndrome by rheumatologists.
Learning points.
Several reports have demonstrated an association between rheumatoid arthritis (RA) and multiple myeloma.
POEMS syndrome (polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin changes), a variant of multiple myeloma, is considered rare but may in reality be underdiagnosed.
Rheumatologists should be aware of POEMS syndrome as a possible diagnosis in patients with RA and polyneuropathy.
Serum vascular endothelial growth factor levels should be measured in suspected cases of POEMS syndrome.
Footnotes
Contributors: TA and YM involved in conception or design of the work. TA and SK are responsible for acquisition of data. TA, SK, TM and YM are responsible for analysis and interpretation of data. TA, TM and YM drafted the manuscript or revised.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Zintzaras E, Voulgarelis M, Moutsopoulos HM. The risk of lymphoma development in autoimmune diseases: a meta-analysis. Arch Intern Med 2005;165:2337–44. 10.1001/archinte.165.20.2337 [DOI] [PubMed] [Google Scholar]
- 2.Dreyer L, Mellemkjær L, Andersen AR, et al. . Incidences of overall and site specific cancers in TNFα inhibitor treated patients with rheumatoid arthritis and other arthritides - a follow-up study from the DANBIO registry. Ann Rheum Dis 2013;72:79–82. 10.1136/annrheumdis-2012-201969 [DOI] [PubMed] [Google Scholar]
- 3.Landgren O, Zhang Y, Zahm SH, et al. . Risk of multiple myeloma following medication use and medical conditions: a case-control study in Connecticut women. Cancer Epidemiol Biomarkers Prev 2006;15:2342–7. 10.1158/1055-9965.EPI-06-0097 [DOI] [PubMed] [Google Scholar]
- 4.Setoguchi S, Solomon DH, Weinblatt ME, et al. . Tumor necrosis factor alpha antagonist use and cancer in patients with rheumatoid arthritis. Arthritis Rheum 2006;54:2757–64. 10.1002/art.22056 [DOI] [PubMed] [Google Scholar]
- 5.Rajkumar SV, Dimopoulos MA, Palumbo A, et al. . International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 2014;15:e538–48. 10.1016/S1470-2045(14)70442-5 [DOI] [PubMed] [Google Scholar]
- 6.Fajgenbaum DC, Uldrick TS, Bagg A, et al. . International, evidence-based consensus diagnostic criteria for HHV-8-negative/idiopathic multicentric Castleman disease. Blood 2017;129:1646–57. 10.1182/blood-2016-10-746933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Albitar S, Bourgeon B, Genin R, et al. . POEMS syndrome, steroid-dependent diabetes mellitus, erythema elevatum diutinum, and rheumatoid arthritis as extramedullary manifestations of plasma cell dyscrasia. Am J Kidney Dis 1998;31:e3.1–e3.4. 10.1053/ajkd.1998.v31.pm10074579 [DOI] [PubMed] [Google Scholar]
- 8.Bandyopadhyay D, Kochhar GS, Hanouneh I, et al. . Ascites in a 42-year-old woman. Cleve Clin J Med 2013;80:771–6. 10.3949/ccjm.80a.12118 [DOI] [PubMed] [Google Scholar]
- 9.D'Souza A, Hayman SR, Buadi F, et al. . The utility of plasma vascular endothelial growth factor levels in the diagnosis and follow-up of patients with POEMS syndrome. Blood 2011;118:4663–5. 10.1182/blood-2011-06-362392 [DOI] [PubMed] [Google Scholar]
- 10.Kanai K, Sawai S, Sogawa K, et al. . Markedly upregulated serum interleukin-12 as a novel biomarker in POEMS syndrome. Neurology 2012;79:575–82. 10.1212/WNL.0b013e318263c42b [DOI] [PubMed] [Google Scholar]
- 11.Kourelis TV, Buadi FK, Kumar SK, et al. . Long-term outcome of patients with POEMS syndrome: an update of the Mayo Clinic experience. Am J Hematol 2016;91:585–9. 10.1002/ajh.24356 [DOI] [PubMed] [Google Scholar]
- 12.Bekkelund SI, Torbergsen T, Husby G, et al. . Myopathy and neuropathy in rheumatoid arthritis. A quantitative controlled electromyographic study. J Rheumatol 1999;26:2348–51. [PubMed] [Google Scholar]
- 13.Chamberlain MA, Bruckner FE. Rheumatoid neuropathy. Clinical and electrophysiological features. Ann Rheum Dis 1970;29:609–16. 10.1136/ard.29.6.609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lanzillo B, Pappone N, Crisci C, et al. . Subclinical peripheral nerve involvement in patients with rheumatoid arthritis. Arthritis Rheum 1998;41:1196–202. [DOI] [PubMed] [Google Scholar]