Abstract
Background
Medical screening and load monitoring procedures are commonly used in professional football to assess factors perceived to be associated with injury.
Objectives
To identify prognostic factors (PFs) and models for lower extremity and spinal musculoskeletal injuries in professional/elite football players from medical screening and training load monitoring processes.
Methods
The MEDLINE, AMED, EMBASE, CINAHL Plus, SPORTDiscus and PubMed electronic bibliographic databases were searched (from inception to January 2017). Prospective and retrospective cohort studies of lower extremity and spinal musculoskeletal injury incidence in professional/elite football players aged between 16 and 40 years were included. The Quality in Prognostic Studies appraisal tool and the modified Grading of Recommendations Assessment, Development and Evaluation synthesis approach was used to assess the quality of the evidence.
Results
Fourteen studies were included. 16 specific lower extremity injury outcomes were identified. No spinal injury outcomes were identified. Meta-analysis was not possible due to heterogeneity and study quality. All evidence related to PFs and specific lower extremity injury outcomes was of very low to low quality. On the few occasions where multiple studies could be used to compare PFs and outcomes, only two factors demonstrated consensus. A history of previous hamstring injuries (HSI) and increasing age may be prognostic for future HSI in male players.
Conclusions
The assumed ability of medical screening tests to predict specific musculoskeletal injuries is not supported by the current evidence. Screening procedures should currently be considered as benchmarks of function or performance only. The prognostic value of load monitoring modalities is unknown.
Keywords: prediction, lower extremity injuries, injury profiling, risk factors, prediction models
Introduction
The incidence of musculoskeletal injuries reported in European professional football (soccer) players is high. On average, players sustain two injuries and miss 37 days of training and match play per season,1 with most injuries occurring to the lower extremities.2 Team performance is negatively affected by increased injury incidence and severity3 and the subsequent financial implications are considerable.4 Therefore, injury prevention strategies are potentially of great benefit to professional clubs.3
In professional sport, general medical examination5 and physical performance tests (PPTs)6 7 are commonly used to screen for factors perceived to indicate enhanced injury risk.8 9 A survey of elite European professional football teams has identified that 94% routinely use injury risk screening and monitoring with the most common methods including muscle flexibility, strength and imbalance assessment and joint mobility examination.10
Evaluation of training and match load through technological modalities such as Global Positioning Systems (GPS) and heart rate monitoring are also commonly employed for this purpose in football,10 11 alongside subjective indicators such as perceived exertion ratings and wellness evaluation.10
Factors associated with injury and assessed through screening and load monitoring have been given many different names in the literature, such as risk factors, predictive factors and predictors. However, The PROGnosis RESearch Strategy Partnership, an international, interdisciplinary collaboration which aims to enhance the impact of prognosis research, terms such factors as prognostic factors (PFs). PFs are defined as variables associated with or predictive of clinical events (such as injury) in populations with a defined baseline state.12 13 Importantly, PFs may or may not offer insights into injury causality, but by being associated with or predictive of the outcome of interest, they are potentially useful for developing multivariable prognostic models. These models aim to make meaningful individual risk predictions and inform stratified management approaches designed to reduce risk.14 Hence, medical screening and training load monitoring processes are concerned with prognosis. Consequently within this review only the term PF will be used for measures derived from such practices. PFs are intrinsic (person specific) or extrinsic (environment specific)15 and deemed modifiable or non-modifiable.16 For intrinsic factors, an example of a non-modifiable factor is age, whereas a modifiable factor could be strength. For extrinsic factors, a non-modifiable factor example is weather, while modifiable factors include training load.
Previous systematic reviews have investigated PFs for injuries in sport6 7 17–22 and football in general.23 These findings have limited clinical relevance as analyses were not stratified by sport, skill level or both. PFs should be considered specific to sport and populations of amateur or professional athletes, as there are fundamental differences in metabolic, biomechanical and loading exposure characteristics that may also predispose to particular injuries. Specifically, in professional football, a previous systematic review found that history of a previous hamstring injury (HSI) may be associated with future HSIs, although the evidence relating to the prognostic value of isokinetic strength testing, functional movement screen, muscle imbalance assessment, use of psychological questionnaires and fatigue monitoring was either inconclusive or insufficient.24 However, the analysis only included these commonly perceived PFs identified by an international survey of medical practice in professional clubs25 and did not examine other potentially relevant factors. The only review of training load monitoring found that high intensity football training may be associated with increased injury propensity,11 although these findings were limited to generalised injury categories rather than specific outcomes. There are no exhaustive systematic reviews that have investigated PFs identified through medical screening and training load monitoring procedures for specific injuries in professional football.
Therefore, the aims of this systematic review are to: i) identify PFs for specific lower extremity and spinal musculoskeletal injuries in adult professional/elite football players, from medical screening and training load monitoring processes and ii) identify any current prognostic models that are able to predict specific lower extremity and spinal injuries in adult professional/elite football players.
Methods
The methodology was specified a priori through protocol registration with the International Prospective Register of Systematic Reviews.26 This review has conformed to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines (online supplementary file 6).27
Eligibility criteria
Types of studies
Prospective and retrospective cohort studies were included as these are best suited for prognosis research.28 Studies of any other design were excluded.
Types of participants
Studies were included if participants were defined as professional/elite football players, aged between 16 and 40 years. Studies were excluded if they contained participants from non-football or mixed sports, or amateur/recreational football players of any age.
Types of outcome measures
Outcomes were any lower extremity or spinal musculoskeletal injury categories, defined by specific diagnosis and/or anatomical location. Outcomes that were not defined with specific diagnosis and/or location, or used generalised injury categories (eg, defined as injuries, match injuries, training injuries, overuse injuries, general muscle or ligament injuries) were excluded. Studies were included if the magnitude of association between PFs and outcomes were reported with appropriate summary effect measures, that is, odds ratios (OR), risk ratios (RR), incidence rate ratios (IRR) or hazard ratios (HR) alongside corresponding p values and confidence intervals (CI). Studies were excluded if measures of association were not reported, that is, only significance testing was reported.
Types of prognostic factors
Studies were included if any of the following were investigated: 1) general medical examination/questionnaire (including anthropometric information), 2) any clinical musculoskeletal examination/assessment methods (including flexibility, mobility and strength measurement) or PPT (including measures of core stability, functional movement control, strength and proprioception), 3) medical imaging, 4) training load measurement (time unit documentation, technology such as GPS and physiological parameters, eg, heart rate measures). Studies were excluded if PFs or models were not investigated or if treatment interventions were performed.
Data sources and search strategy
The MEDLINE, AMED, EMBASE, CINAHL Plus, SPORTDiscus electronic bibliographic databases were searched from inception to 24 July 2016, and repeated on 12 December 2016 to identify new literature. The strategy is presented in the online supplementary file 1; terms were adapted to the requirements of each specific database. To ensure that all relevant studies were captured, a secondary search of the PubMed database was conducted on 2 January 2017 using a broad non-specific strategy of football OR soccer AND injuries. Where the full text was obtained, reference lists were searched. Searches were limited to original research articles, published in English through peer-reviewed journals. Systematic and narrative reviews, clinical commentaries, editorials, conference abstracts, grey literature or studies from non-peer-reviewed journals were excluded.
bmjsem-2017-000263supp001.pdf (79.9KB, pdf)
Study selection
Titles and abstracts of retrieved studies were independently screened by the lead reviewer (TH). The second reviewer (MJC) verified the results and relevant full-text articles were obtained. All were screened for eligibility in a standardised, unblinded manner jointly by both reviewers. Data were extracted by one reviewer (TH) using a standardised form (see online supplementary file 2) and verified by the second reviewer (MJC).
bmjsem-2017-000263supp002.pdf (82.4KB, pdf)
Risk of bias in individual studies
Risk of bias was assessed using The Quality in Prognostic Studies (QUIPS) tool,29 which is advocated by the Cochrane Prognosis Methods Group and has moderate to near perfect inter-rater reliability.29 QUIPS evaluates validity and bias through participation, attrition, PF, confounding variable and statistical reporting domains. Domains contained several items where extracted information was entered and this guided judgement of potential for bias. After consideration, each domain was rated as low, moderate or high risk of bias and the corresponding risk level for each domain was colour coded as green, amber or red, respectively.
Both reviewers assessed the evidence independently, but were not blinded to authors, title or journal. Disagreements were resolved through discussion. If consensus could not be reached, the third reviewer (JCS) was consulted.
Data analysis and synthesis
Extracted data and QUIPS appraisal summaries were tabulated to assess heterogeneity of study characteristics and quality (table 1). Subgroup analysis of male and female participants was planned a priori. The quantity, quality and heterogeneity of the literature prevented formal statistical evaluation, so a narrative synthesis was performed. All results were extracted for each study (see online supplementary file 3).
Table 1.
Characteristics, prognostic factors, outcomes and QUIPS assessments for included studies
| Prognostic factors stated in text | QUIPS score per domain | |||||||||||||
| Study | Specific outcomes | N | Follow-up | Demographics/anthropometrics | Neuromuscular | Anatomical | Physiological | Training load/recovery | Participation | Attrition | Prognostic factors | Outcome measurement | Confounding measurement | Statistical reporting |
| Arnason et al30 | Hamstring strains, groin strains, ankle sprains, knee sprains | 306 males |
1 season | Age, height, weight, BMI, body comp, PMH | Maximal average squat power, standing jump, CMJ | Flexibility | – | Match exposure, training: match ratio. | ||||||
| Bengtsson et al31 | Hamstring injuries, quadriceps injuries, adductor injuries and calf injuries | Unknown | 1–11 seasons | – | – | – | – | Recovery time between matches | ||||||
| Carling et al32 | Hamstring strains, quadriceps strains, groin strains, calf strains, ankle sprains, knee sprains | 35 males | 6 seasons | – | – | – | – | No. of matches in 3/4 day cycle | ||||||
| Faude et al33 | Ankle sprains, knee sprains, ACL tears | 143 females |
1 season | Age, height, weight BMI, limb dominance, playing position, PMH |
– | – | – | Training time, match time | ||||||
| Fousekis et al34 | Hamstring injuries, quadriceps injuries | 100 males |
10 months | Age, height, weight, PMH | Ankle isokinetic strength, knee isokinetic strength, functional knee strength ratio, stabilometry | Mid thigh girth, lower limb length, knee joint stability, ankle flexibility, hamstring and quadriceps flexibility | – | – | ||||||
| Fousekis et al35 | Ankle sprains | 100 males | 10 months | Age, height, weight, PMH, limb dominance | Ankle isokinetic strength, stabilometry | Tibia length, lower limb length, ankle joint stability, ankle flexibility |
– | – | ||||||
| Hagglund et al36 | Ankle sprains, groin injuries, knee joint trauma | 197 males | 2 seasons | Age, height, weight, BMI, PMH | – | – | – | – | ||||||
| Hagglund et al37 | Hamstring injuries, quadriceps injuries, adductor injuries, calf injuries | 1401 males | 9 seasons | Age, height, weight, PMH, limb dominance, playing position | – | – | – | Training/match exposure, Match venue/type, Period in season, Climate |
||||||
| Hagglund et al38 | Patella tendinopathy | 2379 males | 4.3 seasons | Age, height, weight, playing position | – | – | – | Total exposure, Training/match exposure, Period in season, Team home playing surface |
||||||
| Henderson et al39 | Hamstring injuries | 36 males | 1 season | Age, height, weight, lean mass | Knee isokinetic strength, NCMJ jump, CMJ |
Active hip flexion ROM (dominant side) | Yo-yo endurance test | – | ||||||
| Nilstad et al40 | Thigh injuries, knee injuries, ankle injuries, lower leg and foot injuries | 173 females | 1 season | Age, height, weight, BMI, PMH, seasons at elite level | Knee isokinetic strength, leg press, hip abductor strength, knee valgus during drop jump landing, SEBT | Knee joint stability, hypermobility, foot pronation | – | Training/match exposure | ||||||
| Timmins et al43 | Hamstring injuries | 152 males | 1 season | Age, height, weight, PMH | Eccentric hamstring strength/imbalance, MVIC strength/MVIC imbalance | US passive fascicle length, passive fascicle length relative to BFlh length, 25% MVIC length, passive fascicle length imbalance, 25% MVIC fascicle length imbalance, passive muscle thickness, 25% MVIC muscle thickness | – | – | ||||||
| Waldén et al41 | Knee injuries, traumatic knee injuries, overuse knee injuries | 310 males | 1 season | Age, height, weight, PMH, limb dominance, playing position | – | – | – | Training/match exposure | ||||||
| Van Dyk et al42 | Hamstring injuries | 614 males | 4 seasons | – | Knee isokinetic strength, mixed hamstring/quadriceps ratios | – | – | – | ||||||
BMI, body mass index; PMH, previous medical history; CMJ, countermovement jump; NCMJ, non-countermovement jump; QUIPS, Quality in Prognostic Studies; SEBT, Star Excursion Balance Test; MVIC, maximum voluntary isometric contraction; US, ultrasound;BFlh, biceps femoris long head.
▪ Low risk of bias; ▪ moderate risk of bias; ▪ high risk of bias.
bmjsem-2017-000263supp003.pdf (404.5KB, pdf)
This synthesis process was based on the modified Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework.28 All significant PFs for a specific injury outcome were tabulated and grouped (table 2). Any PFs investigated by multiple studies for the same outcome, while using the same effect measures, were tabulated and presented graphically (figures 2–4). These data and QUIPS appraisals were used to make key judgements for each PF in the following domains: 1) study limitations, 2) consistency of results, 3) effect sizes, 4) precision of results, 5) publication bias, 6) overall quality (see online supplementary file 4 for detailed explanation of how judgements for each domain were made).
Table 2.
Summary of synthesis of prognostic factors for all injury outcomes with associated GRADE evaluation
| Adapted GRADE criteria | |||||||||||||
| Injury type | Specific Outcomes | Potential prognostic factors | Number of studies | Authors | Effect measure | Univariate Effect size (95% CI) | Multivariate effect size (95% CI) | Study limitations | Consistency of results | Effect size | Precision of results | Publication bias | Overall quality |
| Muscle injuries | Hamstring injuries | Increasing age | 2 | Hagglund et al 36 37 | HR | Figure 2 | 1.1 (1 to 1.2) | Many | No | Small | Imprecise | Likely | Low |
| Increasing age | 2 | Arnason et al,30 Henderson et al 39 | OR | – | Figure 3 | Many | Yes | Small | Precise | Likely | Low | ||
| Previous hamstring injury | 2 | Hagglund et al 36 37 | HR | Figure 2 | Figure 2 | Many | Yes | Moderate | Imprecise | Likely | Low | ||
| Previous hamstring injury | 2 | Arnason et al,30 Fousekis et al 34 | OR | 7.42 (2.9 to 19) | Figure 3 | Very many | No | Variable | Imprecise | Likely | Very low | ||
| Stature (above mean) | 1 | Hagglund et al 37 | HR | 0.82 (0.68 to 1.0) | – | Many | N/A | Small | Imprecise | Likely | Very low | ||
| Previous quadriceps injury | 1 | Hagglund et al 37 | HR | 1.44 (1.08 to 1.93) | – | Very many | N/A | Small | Imprecise | Likely | Very low | ||
| Eccentric hamstring strength asymmetries | 1 | Fousekis et al 34 | OR | – | 3.88 (1.13 to 13.23) | Very many | N/A | Moderate | Imprecise | Likely | Low | ||
| BW adjusted eccentric hamstring strength (60 deg/s) | 1 | Van Dyk et al 42 | OR | – | 1.37 (1.01 to 1.85) | Many | N/A | Small | Imprecise | Likely | Very low | ||
| BW adjusted concentric quadriceps strength (60 degree/s) | 1 | Van Dyk et al 42 | OR | – | 1.41 (1.03 to 1.92) | Many | N/A | Small | Imprecise | Likely | Very low | ||
| Active hip flexion ROM (dominant leg) | 1 | Henderson et al 39 | OR | – | 0.77 (0.62 to 0.97) | Many | N/A | Small | Imprecise | Likely | Low | ||
| Increased NCMJ height | 1 | Henderson et al 39 | OR | – | 1.47 (1.02 to 2.12) | Many | N/A | Small | Imprecise | Likely | Low | ||
| Functional leg length asymmetry | 1 | Fousekis et al 34 | OR | – | 3.8 (1.08 to 13.33) | Very many | N/A | Large | Imprecise | Likely | Low | ||
| Position: goalkeeper | 1 | Hagglund et al 37 | HR | 0.11 (0.06 to 0.23) | 0.11 (0.06 to 0.24) | Very many | N/A | Large | Imprecise | Likely | Very low | ||
| Time of season: | |||||||||||||
| September-November | 1 | Hagglund et al 37 | OR | 2.24 (1.34 to 3.74) | 2.16 (1.29 to 3.60) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| December–February | 1 | Hagglund et al 37 | OR | 2.56 (1.54 to 4.26) | 2.55 (1.53 to 4.24) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| March–May | 1 | Hagglund et al 37 | OR | 2.56 (1.54 to 4.28) | 2.49 (1.49 to 4.17) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Playing league matches with ≤4 days recovery | 1 | Bengtsson et al 31 | RR | – | 1.28 (1.06 to 1.56) | Many | N/A | Small | Imprecise | Likely | Very low | ||
| Venue: away match | 1 | Hagglund et al 37 | OR | 0.75 (0.62 to 0.91) | 0.76 (0.63 to 0.92) | Very many | N/A | Small | Imprecise | Likely | Very low | ||
| Quadriceps injuries | Previous adductor injury | 1 | Hagglund et al 37 | HR | 1.88 (1.31 to 2.69) | 1.68 (1.16 to 2.41) | Very many | N/A | Small | Imprecise | Likely | Very Low | |
| Previous quadriceps injury | 1 | Hagglund et al 37 | HR | 3.47 (2.49 to 4.84) | 3.1 (2.21 to 4.36) | Very many | N/A | Large | Imprecise | Likely | Very low | ||
| Previous calf injury | 1 | Hagglund et al 37 | HR | 2.08 (1.37 to 3.17) | 1.91 (1.24 to 2.93) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Position: goalkeeper | 1 | Hagglund et al 37 | HR | 0.46 (0.23 to 0.9) | 0.41 (0.2 to 0.82) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Playing league matches with ≤4 days recovery | 1 | Bengtsson et al 31 | RR | – | 1.8 (1.19 to 2.72) | Many | N/A | Small | Imprecise | Likely | Very Low | ||
| Match type: UEFA CL | 1 | Hagglund et al 37 | OR | 0.51 (0.25 to 1.01) | 0.48 (0.24 to 0.97) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Adductor injuries | Previous adductor injury | 1 | Hagglund et al 37 | HR | 1.48 (1.06 to 2.06) | 1.40 (1 to 1.96) | Very many | N/A | Small | Imprecise | Likely | Very low | |
| Position: goalkeeper | 1 | Hagglund et al 37 | HR | 0.58 (0.33 to 0.99) | 0.51 (0.29 to 0.91) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Venue: away match | 1 | Hagglund et al 37 | OR | 0.56 (0.43 to 0.73) | 0.56 (0.43 to 0.73) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Match type: other cup | 1 | Hagglund et al 37 | OR | 0.60 (0.37 to 0.97) | – | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Groin strain injuries | Previous groin strain | 1 | Arnason et al 30 | OR | 5.71 (2 to 15.9) | 7.3 (2.3 to 23.2) | Many | N/A | Large | Imprecise | Likely | Low | |
| Reduced ROM hip abduction | 1 | Arnason et al 30 | OR | – | 0.9 (0.8 to 1) | Many | N/A | Small | Imprecise | Likely | Very Low | ||
| Calf muscle injuries | Previous calf muscle injury | 1 | Hagglund et al 37 | HR | 2.83 (1.86 to 4.31) | 2.33 (1.52 to 3.57) | Very many | N/A | Moderate | Imprecise | Likely | Very low | |
| Increasing age | 1 | Hagglund et al 37 | HR | 2.02 (1.45 to 2.82) | 1.93 (1.38 to 2.71) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Previous adductor injury | 1 | Hagglund et al 37 | HR | 1.87 (1.26 to 2.77) | 1.71 (1.15 to 2.55) | Very many | N/A | Small | Imprecise | Likely | Very low | ||
| Previous hamstring injury | 1 | Hagglund et al 37 | HR | 2.1 (1.51 to 2.54) | 1.74 (1.24 to 2.44) | Very many | N/A | Small | Imprecise | Likely | Very low | ||
| Match type: UEFA CL | 1 | Hagglund et al 37 | OR | 2.43 (1.61 to 3.67) | 2.72 (1.78 to 4.14) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Position: goalkeeper | 1 | Hagglund et al 37 | HR | 0.43 (0.2 to 0.96) | 0.36 (0.16 to 0.82) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Ligament injuries | Ankle sprain | Previous ankle sprain* | 2 | Arnason et al, 30 Faude et al 33 | OR | Figure 4 | Figure 4 | Many | No | Large | Imprecise | Likely | Very low |
| Weight above median | 1 | Fousekis et al 35 | OR | – | 5.72 (1.37 to 23.95) | Many | N/A | Large | Imprecise | Likely | Very low | ||
| BMI > median | 1 | Fousekis et al 35 | OR | – | 8.16 (1.42 to 46.63) | Many | N/A | Large | Imprecise | Likely | Very low | ||
| Eccentric ankle strength asymmetry >15% | 1 | Fousekis et al 35 | OR | – | 8.88 (1.95 to 40.36) | Many | N/A | Large | Imprecise | Likely | Very low | ||
| Playing three matches within4 days | 1 | Carling et al 32 | IRR | 10.4 (1.9 to 57.9) | – | Many | N/A | Large | Imprecise | Likely | Very low | ||
| Knee sprain | Previous knee sprain* | 2 | Arnason et al 30 Faude et al 33 | OR | Figure 4 | Figure 4 | Many | No | Moderate | Imprecise | Likely | Very low | |
| ACL tear | Previous ACL tear† | 1 | Faude et al 33 | OR | – | 5.24 (1.42 to 19.59) | Many | N/A | Large | Imprecise | Likely | Very low | |
| Tendinopathy | Patellar tendinopathy | Age | 1 | Hagglund et al 38 | OR | – | 0.97 (0.93 to 1.01) | Very many | N/A | Small | Imprecise | Likely | Very low |
| Increased body weight (per 5 kg) | 1 | Hagglund et al 38 | OR | – | 1.15 (1 to 1.33) | Very many | N/A | Small | Imprecise | Likely | Very low | ||
| Total football exposure hours (per 10 hours increase) | 1 | Hagglund et al 38 | OR | No data | 1.02 (1 to 1.04) | Very many | N/A | Small | Imprecise | Likely | Very low | ||
| Injuries defined by anatomical location | Traumatic knee injuries | Previous ACL injury‡ | 1 | Waldén et al 41 | Rel. R | – | 2.6 (1.1 to 6.7) | Very many | N/A | Moderate | Imprecise | Likely | Very low |
| Previous ACL injury§ | 1 | Waldén et al 41 | Rel. R | – | 2.7 (1.3 to 5.8) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Previous knee injury | 1 | Hagglund et al 36 | HR | – | 3.10 (1.3 to 7.6) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Overuse knee injuries | Previous ACL injury ‡ | 1 | Waldén et al 41 | Rel. R | – | 7.9 (3.4 to 18.5) | Very many | N/A | Large | Imprecise | Likely | Very low | |
| Previous ACL injury§ | 1 | Waldén et al 41 | Rel. R | – | 4.8 (2.0 to 11.2) | Very many | N/A | Large | Imprecise | Likely | Very low | ||
| Thigh injuries | Increased BMI | 1 | Nilstad et al 40 | OR | 1.37 (0.95 to 1.98) | 1.51 (1.08 to 2.11) | Few | N/A | Small | Imprecise | Likely | Very low | |
| Knee injuries | Previous ACL injury ‡ | 1 | Waldén et al 41 | Rel. R | – | 4.5 (2.3 to 8.8) | Very many | N/A | Large | Imprecise | Likely | Very low | |
| Previous ACL injury§ | 1 | Waldén et al 41 | Rel. R | – | 3.4 (1.8 to 6.3) | Very many | N/A | Moderate | Imprecise | Likely | Very low | ||
| Ankle injuries | Age | 1 | Nilstad et al 40 | OR | 0.64 (0.44 to 0.95) | 0.65 (0.4 to 1.05) | Few | N/A | Small | Imprecise | Likely | Very low | |
| Increased 1 RM leg press | 1 | Nilstad et al 40 | OR | 1.47 (1.05 to 2.05) | 1.41 (0.97 to 2.06) | Few | N/A | Small | Imprecise | Likely | Very low | ||
| Foot pronation | 1 | Nilstad et al 40 | OR | 1.56 (1.13 to 2.15) | 1.55 (0.99 to 2.41) | Few | N/A | Small | Imprecise | Likely | Very low | ||
| Reduced knee valgus angle | 1 | Nilstad et al 40 | OR | 1.14 (0.49 to 2.66) | 0.64 (0.41 to 1) | Few | N/A | Moderate | Imprecise | Likely | Very low | ||
| Lower leg/foot injuries | Previous knee injury | 1 | Nilstad et al 40 | OR | 3.73 (1.47 to 9.46) | 3.57 (1.27 to 9.99) | Few | N/A | Large | Imprecise | Likely | Low | |
| Increased BMI | 1 | Nilstad et al 40 | OR | 1.44 (0.84 to 2.49) | 1.4 (0.90 to 2.17) | Few | N/A | Small | Imprecise | Likely | Very low | ||
| Increased age | 1 | Nilstad et al 40 | OR | 1.48 (1 to 2.21) | 1.47 (0.98 to 2.2) | Few | N/A | Small | Imprecise | Likely | Very low | ||
| Groin injuries | Previous groin injury | 1 | Hagglund et al 36 | HR | 2.40 (1.2 to 4.6) | – | Very many | N/A | Small | Imprecise | Likely | Very low | |
RR, rate ratio; Rel. R, relative risk; IRR, incidence rate ratio; BMI, body mass index; ACL, anterior cruciate ligament; BW, body weight; N/A, not available; GRADE, Grading of Recommendations Assessment, Development and Evaluation; NCMJ, non-countermovement jump; RM, repetition maximum; UEFA CL, UEFA Champions League match;
Effect size and CIs in bold indicate significant value. Effect sizes and CIs in normal font indicate non-significant result. Effect sizes classed as small if measures between 0.66–1 and 1 – 2.4, moderate 0.33–0.66 and 2.5 – 4.4, large 0–0.33 and ≥4.5.
*Arnason et al 30 investigated male subjects, whereas Faude et al 33 investigated female subjects—see figure 4 for details.
† Faude et al 33 have investigated female participants only.
‡Denotes where knee used as unit of analysis,
§ Denotes where player used as unit of analysis.
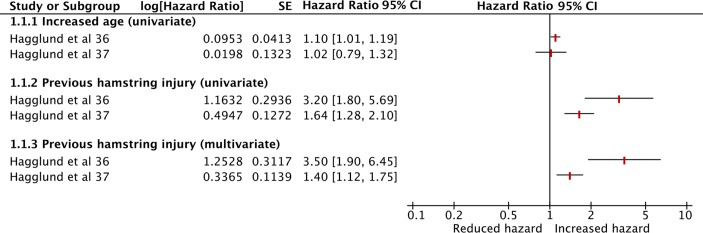
Figure 2.
Graph presenting hamstring injury prognostic factors in male participants, investigated by multiple studies—HR analyses.
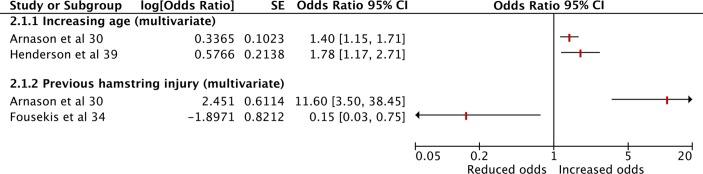
Figure 3.
Graph presenting hamstring injury prognostic factors in male participants, investigated by multiple studies—OR analyses.
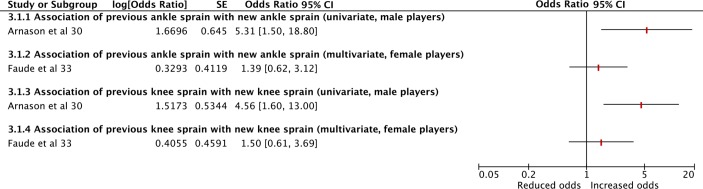
Figure 4.
Graph presenting prognostic factors for ankle sprain and knee sprain injuries, investigated by two or more studies—OR analyses.
bmjsem-2017-000263supp004.pdf (63.5KB, pdf)
Results
Study selection
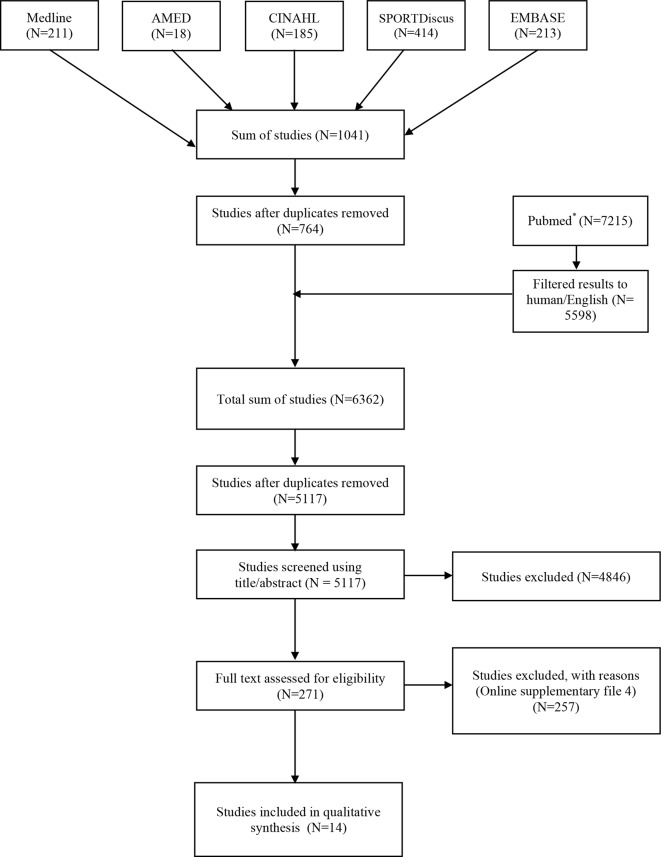
From the searches, 6362 total results were returned with 1245 duplicates, leaving 5117 studies (figure 1). After screening titles and abstracts 4846 studies were excluded. The full texts of the remaining 271 studies were obtained; 257 studies were not eligible at this stage. All excluded studies are listed (with exclusion reasons) in online supplementary file 5. A final total of 14 studies were included.
Figure 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses flow chart, highlighting the study selection process. *Search results from non-specific search strategy of football OR soccer AND injuries.
bmjsem-2017-000263supp005.pdf (279.7KB, pdf)
Characteristics and quality of included studies
For all included studies, the characteristics, PFs and outcomes investigated along with QUIPS risk of bias assessments are presented in table 1. A narrative summary across studies is provided in the sections below.
General
Studies predominantly originated from Europe30–41 with one each from the Middle East42 and Australia.43Follow-up ranged from 1 to 11 football seasons.30–33 36–43 Two studies34 35 stated a 10-month follow-up, equating to one season.
Participants
Participant numbers were provided in 13 studies30 32–43 and totalled 5946 professional/elite players but as one study31 did not report the number of included participants the true total is unknown. Two studies33 40 exclusively investigated female players (n=316). All other studies used male participants only (n=5630).
Outcomes
All outcomes were defined as time loss injuries, that is, injuries that resulted in a player being unable to fully participate in training or match play. Nine outcomes were categorised by diagnosis and anatomical region, whereas seven were categorised by anatomical region only without diagnosis (table 2). No spinal outcomes were investigated.
Prognostic factors
Demographic/anthropometric factors frequently included age, height, weight, body mass index and past medical history.30 33–41 43 Neuromuscular factors included strength, power, jumping, knee control and proprioceptive tests,30 34 35 39 40 42 43 although there was a variety of testing procedures.
Five studies34 35 39 40 42 investigated isokinetic strength tests. For ankle plantarflexor and dorsiflexor muscle groups, only two studies by the same group34 35 used a comparable concentric-eccentric strength testing protocol. For quadriceps and hamstring isokinetic strength testing, four studies34 39 40 42 investigated peak torque, although different protocols and measurements were used.
Anatomical factors included lower limb muscle flexibility, hypermobility, ankle range of motion, ankle stability and foot pronation assessments,30 34 35 39 40 although considerable variation in methods existed. One study43 investigated biceps femoris architecture through ultrasound examination. Two studies investigated anterior knee laxity using a KT 1000 arthrometer,34 40 although it was unclear if identical protocols were followed.
Training and match exposure in hours was reported in six studies,30 33 37 38 40 41 although only one evaluated this as a PF (for patellar tendinopathy).38 Technological evaluation of training load variables were not investigated as PFs for specific injuries in any study. One study investigated match fixture congestion32 and another studied recovery time31 between games.
Eight studies performed univariate PF analyses.30–32 36–38 40 43 Thirteen studies used multivariable statistical models to assess the independent value of PFs.30 31 33–43 However, there was no evidence of an attempt to develop a prognostic model for making individual predictions or validation of a model’s prospective performance.
Effect summary measures
Considerable heterogeneity was evident for reported effect estimates which prohibited meta-analysis. Effect measures included ORs,30 33–35 37–40 HRs,36 37 rate ratios31 32 and relative risk.41 43
Risk of bias within and across studies
The quality of reporting was generally of a poor to moderate standard. Overall, out of 84 domains, 19 (23%) were classed as low risk, 26 (31%) were classed as moderate risk and 39 (46%) were classed as high risk of bias.
Study participation
Three studies were classed as high risk,31 34 35 eight studies were of moderate risk,30 32 37–39 41–43 while three33 36 40 were considered low risk of bias in terms of participation reporting. Ten studies did not report eligibility criteria,30 31 33 36–41 43 whereas four reported this but in insufficient detail.32 34 35 42 Papers considered low risk33 36 40 had good descriptions of recruitment period, location, source and sample population characteristics. In studies considered high or moderate risk,30–32 34 35 37–39 41–43 these factors were either not reported or reported inadequately.
Study attrition
Eight studies30–32 34 36–38 42 were considered high risk as attrition rate, characteristics and reasons for participants lost to follow-up were either not reported or inadequately described. Two studies40 41 were of moderate risk as reasons for attrition were reported but no participant characteristics were reported. Four studies33 35 39 43 were of low risk of bias as response rate was 100% so attrition was not applicable.
Prognostic factor measurement
Across 12 studies,30 31 33–39 41–43 PF measurement reporting was of moderate to high risk of bias. Validity of PF measurement was reported adequately in only one study.43 Frequently, reliability of measurement was not reported33 34 36–39 41 42 or inadequately described.30 35 39 Two studies reported reliability appropriately40 43 and were considered low risk. There were no missing data for PF measurements in seven studies,30 33–35 40–42 although this was either not reported or inadequately described in the other studies.31 32 36–39 43
Outcome measurement
Eleven papers30–38 41 43 were considered high risk of bias because specific clinical or imaging diagnostic criteria for injury outcomes were not stated or inadequately described. Reliable or validated methods for diagnosis confirmation were also not reported in any of these studies and may be a source of misclassification bias. In studies considered moderate risk, one43 stated clinical criteria for HSIs with diagnosis confirmed with MRI, although this was not standardised. One study39 did not state specific clinical criteria, although reported HSI was confirmed through MRI; it was unclear whether only structural HSIs were included for analysis. Only one study40 was considered low risk. Instead of documenting injury type, outcomes were reported per body location. By using non-diagnostic anatomical outcome measures, the implications of misclassification bias were less in this study.
Study confounding
Ten studies30 32–38 40 41 were considered high risk for confounding reporting. Definitions of confounding factors were either not reported or unclear. Three studies36 37 40 stated that adjustments were made for one factor in the statistical analysis. It was assumed that these were considered as confounding factors, although not explicitly defined as such.
Four studies31 39 42 43 were considered as moderate risk. Confounding factors were clearly defined and appropriately adjusted for in the analyses by one study.42 Three studies31 39 43 stated that analyses were adjusted for covariates. In these papers it was assumed that these were confounders, although were not specifically defined as such. Dataset completeness for defined confounding variables and methods of missing data management were also not reported in any study.
Statistical analysis
Statistical analysis reporting was of low risk of bias in nine studies;30 31 34–37 40 42 43data were presented in sufficient detail, with the justification for statistical modelling outlined and no evidence of selective reporting. Two studies32 39 were considered as moderate risk because of selective reporting of significant findings. Three studies33 38 41 were considered high risk. One33 did not use any form of statistical modelling and selective reporting was evident. Another41 described the effect measure as relative risk, which was either inappropriate for the Cox proportional hazard model used or due to reporting inaccuracy. One study38 reported only significant PFs, using a high significance level of 0.20, and referred the reader to online appendices for all results, which were unavailable for download.
Data synthesis
Results of studies
All PFs with associated effect measures, CIs and p values for all included studies are presented in online supplementary file 3. Significant PFs, or factors investigated by multiple studies, per outcome are summarised in table 2. To aid understanding of this table, PFs have been grouped according to specific injury outcomes that were defined within the included literature. For factors presented in the table, the evaluation of the related evidence according to modified GRADE assessment domains is also presented.
All evidence was low or very low quality (table 2). Significant methodological limitations were evident and as significant PFs were derived predominantly from single studies, examination of consistency was limited. Effect measures were variable across factors, but imprecision of effect was common and a sample size calculation was reported by only two studies.34 43 Due to the paucity of literature, publication bias was likely.
Muscle injuries
Muscle injury outcomes were investigated in male participants only. Six significant PFs were identified for quadriceps and calf injuries and four for adductor injuries (table 2), derived from one study.37 Two significant factors for groin strain were found in one study30 (table 2).
It was unclear whether adductor and groin strain injuries were comparable due to lack of diagnostic criteria presented and have been treated as separate entities.
Nineteen significant factors associated with HSIs were identified, with 14 via single studies (table 2). Two studies36 37 investigated increased age and history of previous HSI using HRs, as summarised in figure 2.
Increased age was investigated through univariate analysis only. Hagglund et al36 reported that for every 1 year increase in age, there was an associated small increase in hazard, with a narrow CI lying on the border of significance. However, their later study37 demonstrated no significant association. In both studies, previous HSI was significantly associated with increased hazard for further HSI, in both univariate and multivariate analyses. Hagglund et al36 reported a greater estimated association with larger CIs, possibly due in part to the much smaller sample size. Using ORs, two studies investigated increased age30 39 and two studies investigated previous HSIs30 34 as PFs for new HSIs using multivariate analyses (figure 3).
Similar to the HR analysis, there was consensus that for every 1 year increase in age, odds of developing a HSI were significantly increased,30 39 although effect sizes were small (range 1.40–1.78). In contrast, there was no agreement regarding the effect of previous HSI on the odds of sustaining a new HSI; point estimates lay either side of the line of no effect with very wide CIs, suggesting a considerable lack of precision and may be related to methodological or sample size differences.
Ligament injuries and tendinopathies
Outcomes related to ligament injuries and tendinopathies relied on a smaller evidence base, also of low to very low quality (table 2) and included ankle and knee sprain, ACL tear and patellar tendinopathy. Two studies30 33 investigated the association of a previous ankle sprain with new ankle sprain and a previous knee sprain with new knee sprain, using ORs in male and female participants, respectively. This permitted a limited subgroup analysis (figure 4).
Significant positive associations for both outcomes were found in the male-only study,30 while non-significant positive associations were reported in the female-only study.33 It was difficult to ascertain whether these inconsistencies were due to gender, methodological quality or statistical power. Differences in statistical methods may also have been influential. In terms of ankle sprain outcomes, all other PFs of weight, body mass index and eccentric ankle strength asymmetry related to male players only and were reported by one study (table 2).35 One study reported that a previous anterior cruciate ligament (ACL) injury was significantly associated with a new ACL injury in females,33 while another study reported that previous ACL injury was significantly associated with both traumatic and overuse knee injuries in males41 (table 2). Three significant factors associated with patellar tendinopathy were observed by one study of male participants.38
Injuries defined by anatomical location
PFs for outcomes defined per anatomical location rather than by diagnosis are summarised in table 2. Predominantly these were obtained from a single study40 of female players, although groin and knee injuries in males were investigated by one study per respective outcome.36 41 None of these outcomes could therefore be compared in multiple studies.
Discussion
This review has evaluated the evidence related to PFs or prognostic models for specific lower extremity and spinal musculoskeletal injuries identified through medical screening and training load monitoring processes in professional football. Overall, the paucity, heterogeneity and methodological limitations of the literature meant that the current evidence was of very low or low quality. Within our review, the between-study heterogeneity which limited comparisons between PFs and outcomes may be partly explained by differences in individual clubs’ screening and monitoring practices, confirmed previously through international questionnaires.10 25 The overall limitations in quantity of evidence may be explained in part by a possible reluctance of individual clubs to share data within the research community for fear of losing a competitive advantage. This highlights the potential value of conducting large multi-team cohort studies of professional players such as those identified within this review. 30 31 33–38 40–43 On the few occasions where multiple studies could be used to compare PFs and outcomes, only two factors demonstrated consensus. That is, in terms of prognostic value for future HSIs in male professional football players, a history of previous HSI appears to increase hazard ratio,36 37 while increasing age appears to elevate the odds of a new HSI occurring.30 39 No studies were found to have examined spinal injury outcomes.
Although most studies used multivariable models to examine PF interactions, none had set out to develop a prognostic model or validated injury prediction performance of a model prospectively. Therefore, the current evidence base is relevant only to the initial stages of prognostic model development, which is identifying potential candidate PFs to consider including in models.14 44
While PFs from traditional medical screening methods were assessed,30 33–42 surprisingly only one study examined an imaging modality43 and no studies investigated training load monitoring derived from technology such as GPS or heart rate measures. Although five studies30 33 37 40 41 recorded training and match exposure in terms of time units, only one study analysed this as a PF, for patellar tendinopathy. The results of this study suggested that for every 10 hours increase in total football exposure, the odds of developing patellar tendinopathy in male professional players increased by a factor of 1.02 (95% CI 1.0 to1.04).38 No other studies were available to assess the consistency of these findings and with the insufficient volume of evidence it could be argued that the prognostic value of training load monitoring for specific lower extremity or spinal injuries is unknown at present.
After identifying high-quality cohort studies of professional footballers, an earlier review found that a history of previous injury was a significant PF for future injuries of the same type and other locations. This included that a history of HSI was strongly associated with new HSI.24 McCall et al24 also found that there was insufficient evidence to evaluate the effect of fatigue, muscle imbalance, FMS and isokinetic testing as PFs for injuries. Although McCall et al24 did not locate studies relating to fatigue, our review identified two studies31 32 which investigated recovery time between games or match fixture congestion. These factors could be indirectly related to fatigue. We found that in agreement with McCall et al,24 there was insufficient evidence to establish the prognostic value of isokinetic muscle testing and FMS. Our review demonstrates consensus with this prior review that a previous HSI increases risk of a future HSI. However, we have also identified that increasing age may also be influential on HSI, which has not been reported previously. Despite this agreement there was a discrepancy noted in the quality of included studies in our review and the findings of McCall et al.24 Our review found that all evidence related to previous injury was potentially subject to major biases and consistency of results could not be examined for most factors, other than the effects of increasing age and previous HSI on future HSIs. 24
The differences in reported evidence quality between reviews may be due to different appraisal systems. McCall et al24 used the Scottish Intercollegiate Guidelines Network (SIGN) tool for appraisal, whereas we used the QUIPS tool and modified GRADE framework which are specific to prognostic research and arguably more suitable for the study designs reviewed. Considerable differences in inclusion and exclusion criteria existed and also, our study chose to investigate specific musculoskeletal outcomes of the the lower extremities and spine only rather than musculoskeletal injuries affecting all body areas. Additionally, McCall et al24 investigated only a limited selection of PFs and screening tests identified through a survey, whereas this review attempted to provide an exhaustive examination of all PFs related to screening and training load monitoring in professional football.
In terms of reporting quality, all studies within our review consistently performed poorly in the domains of PF measurement and study confounding. Outcome measurement was a very serious limitation and subject to risk of major misclassification bias due to the lack of specific diagnostic criteria or utilisation of gold standard diagnostic measures. This diagnostic imprecision means that it is questionable if these outcomes can actually be attributed to specific pathologies. It is clear that research quality in football prognostic studies needs to improve through transparent reporting of reliability and validity measurements, explicit identification of confounding factors and the use of clinical diagnostic criteria and/or confirmatory diagnostic modalities to accurately establish the presence of an injury outcome. Until such time, associations between potential PFs and specific injuries should be considered non-robust. A greater and improved evidence base is also necessary to assist future development of prognostic models in an attempt to predict individual injury outcomes. Many of the issues highlighted in this review relate to the reporting rather than necessarily the conduct of the studies included. It is hoped that recommendations aiming to improve the transparency of prognosis research46 will improve the quality of evidence available in the future.
What does this mean to clinicians?
Our results suggest that the ability of medical screening tests to predict specific musculoskeletal injury risk is not supported by the current evidence. Extrinsic non-modifiable factors of age and previous injury may be the only PFs associated with further HSIs, although this is supported by low-quality evidence. At present, screening tests should only be considered as markers of individual musculoskeletal function or performance and therefore primarily useful as benchmarks following injury or in the evaluation of training effects. Presently, when considering specific lower extremity or spinal injuries the prognostic value of load measures is unknown.
Limitations
Despite a thorough literature search using MeSH terms and keywords, certain relevant studies may have been missed. As the search was limited to articles published in academic journals only, this may have introduced some publication bias. Also, both reviewers were not blinded to the authors of the papers included for appraisal. Also, although the QUIPS appraisal tool has been stated to have moderate to near perfect reliability,29 inter-rater reliability was not formally evaluated in our review. Nevertheless, this is the only known systematic review that has evaluated PF for lower extremity and spinal injuries in professional football (soccer) players, using specific prognostic research appraisal and synthesis tools.
Conclusion
The current evidence suggests that a previous HSI and increasing age may be associated with development of future HSIs in male professional football players. This must be interpreted with caution, as significant issues and complexities within the literature have been highlighted. This limits current understanding of PF accuracy through medical screening and training load monitoring. Further research is essential to help further the knowledge base of this important area of football and sports medicine.
Summary box.
What is already known?
In professional football, the risk of sustaining a lower extremity musculoskeletal injury is considerable.
Medical screening and training load monitoring processes are commonly used to identify prognostic factors for injury and develop preventative strategies to reduce risk.
Several previous systematic reviews have investigated prognostic factors for injury identified through screening tests generally in sport.
One previous review has investigated a limited number of prognostic factors through screening tests in professional football.
What are the new findings?
The evidence is of low to very low quality.
Previous hamstring injury and increasing age may increase the risk of a future hamstring injury in male professional players. The limitations of the evidence mean that the contribution of other prognostic factors cannot be fully excluded and currently the ability of medical screening procedures to predict specific injury risk is unsubstantiated.
The prognostic value of training load monitoring is unknown.
Future studies are needed to improve understanding of the prognostic value of medical screening and training load monitoring in professional football.
bmjsem-2017-000263supp006.doc (63KB, doc)
Acknowledgments
The authors would like to thank Professor David Felson, Professor Ian Bruce and Mary Ingram at the University of Manchester. The authors would also like to thank all staff within the medical department at Manchester United (especially Dr. Steve McNally, Neil Hough, John Davin, Richard Merron, Jonathan Picot and Russ Hayes) for their help and support with this review. This report includes independent research supported by the National Institute for Health Research Biomedical Research Unit Funding Scheme. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health. The authors also thank Arthritis Research UK for their support: Arthritis Research UK grant number 20380.
Footnotes
Contributors: Literature searching (TH, MP), data extraction (TH, MJC), data appraisal (TH, JCS, MJC), data synthesis (TH), data interpretation (TH, JCS, MJC) manuscript writing (TH, JCS, MJC), manuscript review (TH, JCS, MP, MJC).
Funding: The lead reviewer (TH) is currently receiving sponsorship by Manchester United Football Club Limited to complete a PhD study programme.
Competing interests: None declared.
Patient consent: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ekstrand J, Hägglund M, Waldén M, et al. . Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med 2011;45:553–8. 10.1136/bjsm.2009.060582 [DOI] [PubMed] [Google Scholar]
- 2.Hägglund M, Waldén M, Ekstrand J, et al. . Injuries among male and female elite football players. Scand J Med Sci Sports 2009;19:819–27. 10.1111/j.1600-0838.2008.00861.x [DOI] [PubMed] [Google Scholar]
- 3.Hägglund M, Waldén M, Magnusson H, et al. . Injuries affect team performance negatively in professional football: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med 2013;47:738–42. 10.1136/bjsports-2013-092215 [DOI] [PubMed] [Google Scholar]
- 4.Woods C, Hawkins R, Hulse M, et al. . The Football Association Medical Research Programme: an audit of injuries in professional football-analysis of preseason injuries. Br J Sports Med 2002;36:436–41. 10.1136/bjsm.36.6.436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cook G, Burton L, Hoogenboom B et al. . Pre-participation screening: the use of fundamental movements as an assessment of function - part 1. N Am J Sports Phys Ther 2006;1:62–72. [PMC free article] [PubMed] [Google Scholar]
- 6.Hegedus EJ, McDonough S, Bleakley C, et al. . Clinician-friendly lower extremity physical performance measures in Athletes: a systematic review of measurement properties and correlation with injury, part 1. the tests for knee function including the hop tests. Br J Sports Med 2015;49:642–8. 10.1136/bjsports-2014-094094 [DOI] [PubMed] [Google Scholar]
- 7.Hegedus EJ, McDonough SM, Bleakley C, et al. . Clinician-friendly lower extremity physical performance tests in athletes: a systematic review of measurement properties and correlation with injury. Part 2--the tests for the hip, thigh, foot and ankle including the star excursion balance test. Br J Sports Med 2015;49:649–56. 10.1136/bjsports-2014-094341 [DOI] [PubMed] [Google Scholar]
- 8.Bahr R. Why screening tests to predict injury do not work-and probably never will…: a critical review. Br J Sports Med 2016;50:776–80. 10.1136/bjsports-2016-096256 [DOI] [PubMed] [Google Scholar]
- 9.Gabbe B, Bennell KL, Wajswelner H, et al. . Reliability of common lower extremity musculoskeletal screening tests. Physical Therapy in Sport 2004;5:90–7. 10.1016/S1466-853X(04)00022-7 [DOI] [Google Scholar]
- 10.McCall A, Dupont G, Ekstrand J. Injury prevention strategies, coach compliance and player adherence of 33 of the UEFA Elite Club Injury Study teams: a survey of teams’ head medical officers. Br J Sports Med 2016;50:725–30. 10.1136/bjsports-2015-095259 [DOI] [PubMed] [Google Scholar]
- 11.Jaspers A, Brink MS, Probst SG, et al. . Relationships between training load Indicators and training outcomes in professional soccer. Sports Med 2017;47:533–44. 10.1007/s40279-016-0591-0 [DOI] [PubMed] [Google Scholar]
- 12.Hemingway H, Croft P, Perel P, et al. . Prognosis research strategy (PROGRESS) 1: a framework for researching clinical outcomes. BMJ 2013;346:e5595 10.1136/bmj.e5595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bouwmeester W, Zuithoff NPA, Mallett S, et al. . Reporting and methods in clinical prediction research: a systematic review. PLoS Med 2012;9:e1001221–12. 10.1371/journal.pmed.1001221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steyerberg EW, Moons KG, van der Windt DA, et al. . Prognosis Research Strategy (PROGRESS) 3: prognostic model research. PLoS Med 2013;10:e1001381 10.1371/journal.pmed.1001381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bahr R, Krosshaug T. Understanding injury mechanisms: a key component of preventing injuries in sport. Br J Sports Med 2005;39:324–9. 10.1136/bjsm.2005.018341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meeuwisse WH. Predictability of Sports Injuries. Sports Medicine 1991;12:8–15. 10.2165/00007256-199112010-00002 [DOI] [PubMed] [Google Scholar]
- 17.Dallinga JM, Benjaminse A, Lemmink KA. Which screening tools can predict injury to the lower extremities in team sports?: a systematic review. Sports Med 2012;42:791–815. 10.1007/BF03262295 [DOI] [PubMed] [Google Scholar]
- 18.Maffey L, Emery C. What are the risk factors for groin strain injury in sport? A systematic review of the literature. Sports Med 2007;37:881–94. [DOI] [PubMed] [Google Scholar]
- 19.Ryan J, DeBurca N, Mc Creesh K. Risk factors for groin/hip injuries in field-based sports: a systematic review. Br J Sports Med 2014;48:1089–96. 10.1136/bjsports-2013-092263 [DOI] [PubMed] [Google Scholar]
- 20.Freckleton G, Pizzari T. Risk factors for hamstring muscle strain injury in sport: a systematic review and meta-analysis. Br J Sports Med 2013;47:351–8. 10.1136/bjsports-2011-090664 [DOI] [PubMed] [Google Scholar]
- 21.Drew MK, Finch CF. The relationship between training load and Injury, illness and soreness: a systematic and Literature Review. Sports Med 2016;46:861–83. 10.1007/s40279-015-0459-8 [DOI] [PubMed] [Google Scholar]
- 22.Gabbett TJ, Whyte DG, Hartwig TB, et al. . The relationship between workloads, physical performance, injury and illness in adolescent male football players. Sports Med 2014;44:989–1003. 10.1007/s40279-014-0179-5 [DOI] [PubMed] [Google Scholar]
- 23.van Beijsterveldt AM, van de Port IG, Vereijken AJ, et al. . Risk factors for hamstring injuries in male soccer players: a systematic review of prospective studies. Scand J Med Sci Sports 2013;23:253–62. 10.1111/j.1600-0838.2012.01487.x [DOI] [PubMed] [Google Scholar]
- 24.McCall A, Carling C, Davison M, et al. . Injury risk factors, screening tests and preventative strategies: a systematic review of the evidence that underpins the perceptions and practices of 44 football (soccer) teams from various premier leagues. Br J Sports Med 2015;49:583–9. 10.1136/bjsports-2014-094104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCall A, Carling C, Nedelec M, et al. . Risk factors, testing and preventative strategies for non-contact injuries in professional football: current perceptions and practices of 44 teams from various premier leagues. Br J Sports Med 2014;48:1352–7. 10.1136/bjsports-2014-093439 [DOI] [PubMed] [Google Scholar]
- 26.Hughes T, Callaghan MJ, Sergeant J. Prognostic factors for musculoskeletal injury identified through medical profiling/screening and training load monitoring in professional football - A systematic review. PROSPERO 2016. http://www.crd.york.ac.uk/PROSPERO_REBRANDING/display_record.asp?ID=CRD42016038204. [DOI] [PubMed] [Google Scholar]
- 27.Liberati A, Altman DG, Tetzlaff J, et al. . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009;62:e1–e34. 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 28.Huguet A, Hayden JA, Stinson J, et al. . Judging the quality of evidence in reviews of prognostic factor research: adapting the GRADE framework. Syst Rev 2013;2:71 10.1186/2046-4053-2-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hayden JA, van der Windt DA, Cartwright JL, et al. . Assessing bias in studies of prognostic factors. Ann Intern Med 2013;158:280–8. 10.7326/0003-4819-158-4-201302190-00009 [DOI] [PubMed] [Google Scholar]
- 30.Arnason A, Sigurdsson SB, Gudmundsson A, et al. . Risk factors for injuries in football. Am J Sports Med 2004;32:5S–16. 10.1177/0363546503258912 [DOI] [PubMed] [Google Scholar]
- 31.Bengtsson H, Ekstrand J, Hägglund M. Muscle injury rates in professional football increase with fixture congestion: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med 2013;47:743–7. 10.1136/bjsports-2013-092383 [DOI] [PubMed] [Google Scholar]
- 32.Carling C, McCall A, Le Gall F, et al. . The impact of short periods of match congestion on injury risk and patterns in an elite football club. Br J Sports Med 2016;50:764–8. 10.1136/bjsports-2015-095501 [DOI] [PubMed] [Google Scholar]
- 33.Faude O, Junge A, Kindermann W, et al. . Risk factors for injuries in elite female soccer players. Br J Sports Med 2006;40:785–90. 10.1136/bjsm.2006.027540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fousekis K, Tsepis E, Poulmedis P, et al. . Intrinsic risk factors of non-contact quadriceps and hamstring strains in soccer: a prospective study of 100 professional players. Br J Sports Med 2011;45:709–14. 10.1136/bjsm.2010.077560 [DOI] [PubMed] [Google Scholar]
- 35.Fousekis K, Tsepis E, Vagenas G. Intrinsic risk factors of noncontact ankle sprains in soccer: a prospective study on 100 professional players. Am J Sports Med 2012;40:1842–50. 10.1177/0363546512449602 [DOI] [PubMed] [Google Scholar]
- 36.Hägglund M, Waldén M, Ekstrand J, et al. . Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med 2006;40:767–72. 10.1136/bjsm.2006.026609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hägglund M, Waldén M, Ekstrand J, et al. . Risk factors for lower extremity muscle injury in professional soccer: the UEFA Injury Study. Am J Sports Med 2013;41:327–35. 10.1177/0363546512470634 [DOI] [PubMed] [Google Scholar]
- 38.Hägglund M, Zwerver J, Ekstrand J, et al. . Epidemiology of patellar tendinopathy in elite male soccer players. Am J Sports Med 2011;39:1906–11. 10.1177/0363546511408877 [DOI] [PubMed] [Google Scholar]
- 39.Henderson G, Barnes CA, Portas MD, et al. . Factors associated with increased propensity for hamstring injury in English Premier League soccer players. J Sci Med Sport 2010;13:397–402. 10.1016/j.jsams.2009.08.003 [DOI] [PubMed] [Google Scholar]
- 40.Nilstad A, Andersen TE, Bahr R, et al. . Risk factors for lower extremity injuries in elite female soccer players. Am J Sports Med 2014;42:940–8. 10.1177/0363546513518741 [DOI] [PubMed] [Google Scholar]
- 41.Waldén M, Hägglund M, Ekstrand J, et al. . High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury. Br J Sports Med 2006;40:158–62. discussion 58-62 10.1136/bjsm.2005.021055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van Dyk N, Bahr R, Whiteley R, et al. . Hamstring and quadriceps isokinetic strength deficits are weak risk factors for hamstring Strain Injuries: a 4-Year Cohort Study. Am J Sports Med 2016;44:1789–95. 10.1177/0363546516632526 [DOI] [PubMed] [Google Scholar]
- 43.Timmins RG, Bourne MN, Shield AJ, et al. . Short biceps femoris fascicles and eccentric knee flexor weakness increase the risk of hamstring injury in elite football (soccer): a prospective cohort study. Br J Sports Med 2016;50:1524–35. 10.1136/bjsports-2015-095362 [DOI] [PubMed] [Google Scholar]
- 44.Riley RD, Hayden JA, Steyerberg EW, et al. . Prognosis Research Strategy (PROGRESS) 2: prognostic factor research. PLoS Med 2013;10:e1001380 10.1371/journal.pmed.1001380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vandenbroucke JP, von Elm E, Altman DG, et al. . Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med 2007;4:e297–54. 10.1371/journal.pmed.0040297 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2017-000263supp001.pdf (79.9KB, pdf)
bmjsem-2017-000263supp002.pdf (82.4KB, pdf)
bmjsem-2017-000263supp003.pdf (404.5KB, pdf)
bmjsem-2017-000263supp004.pdf (63.5KB, pdf)
bmjsem-2017-000263supp005.pdf (279.7KB, pdf)
bmjsem-2017-000263supp006.doc (63KB, doc)