Abstract
Objectives
This study aimed to (1) provide an update on the prevalence of parent-reported autism spectrum disorder (ASD) diagnosis and new information about teacher-reported ASD in two nationally representative Australian cohorts at ages 10–11 years, (2) examine differences in cohort demographic and clinical profiles and (3) compare the prevalence of teacher-reported ASD and any changes in categorisation over time across the cohorts.
Design
Secondary analyses were undertaken using data from the Longitudinal Study of Australian Children (LSAC).
Participants
Children were recruited at kindergarten age (K cohort; birth year 1999/2000) and birth (B cohort; birth year 2003/2004), with follow-up of every 2 years for six waves.
Primary outcome measures
Parent-reported and teacher-reported ASD diagnosis was ascertained at three time points (waves 4–6).
Results
At age 10–11 years, the adjusted prevalence of parent-reported ASD diagnosis was 3.9% (95% CI 3.2 to 4.5) and 2.4% (95% CI 1.6 to 2.9) in the B and K cohorts, respectively. Teacher-reported prevalence of ASD was 1.7% (95% CI 1.2 to 2.1) in the B cohort and 0.9% (95% CI 0.56 to 1.14) in the K cohort. Parents reported fewer conduct and peer problems and teachers more pro-social behaviour in B relative to K cohort ASD children. Children reported only by parents in the later-born B cohort had milder behaviour problems than parent-agreed and teacher-agreed cases. Although individual switching to ASD from other categories from 8–9 to 10–11 years was low (K cohort n=5, B cohort n=6), teachers reported more children with ASD in the B than K cohort at 10–11 years and fewer children with emotional/ behavioural problems.
Conclusions
The higher prevalence of parent-reported and teacher-reported ASD diagnosis in the later-born cohort may be partially explained by identifying children with milder behavioural problems as ASD and a change in the use of diagnostic categories in schools.
Keywords: Autism Spectrum Disorder, prevalence, epidemiology
Strengths and limitations of this study.
A strength of this study is the population representative sample, the Longitudinal Study of Australian Children.
Another strength of this study is the comparison of two birth cohorts of children born 4 years apart.
The main limitation is the use of parent-reported and teacher-reported, rather than clinician-verified, ASD diagnoses.
Autism spectrum disorder (ASD) emerges in early childhood and is characterised by atypical neurodevelopment resulting in social-communication impairment and rigid and repetitive patterns of behaviour.1 Once thought to be relatively rare, there has been a worldwide increase in the prevalence of children diagnosed with ASD with figures rising from 2 to 6/10,000 in epidemiological studies prior to the 1990s2 to current estimates of up to 260/10,000 or 2.6%.3–5
To explain the increasing prevalence of ASD, changes in risk factors or etiological causes and non-etiological factors have been explored. These include factors which may be on the causal pathway to ASD such as the effect of increasing parental age6 and other perinatal risk factors such as gestational age and birth weight.7 However, studies generally suggest minimal contribution (<1%) to increasing ASD prevalence rates.7 Non-etiological factors have explained a much higher proportion of the increase in ASD prevalence and include: changing diagnostic criteria contributing to higher functioning or milder cases being identified; diagnostic switching or substitution—favouring an ASD diagnostic label over another previously used category such as intellectual disability; and increased use of developmental surveillance or screening which may result in the identification of milder, previously unidentified and younger cases.8–11 Ascertainment methods for cases across studies have varied widely, from population representative samples to use of education, health or welfare data, resulting in further variation in prevalence estimates.8–11
The Longitudinal Study of Australian Children (LSAC) is a nationally representative study,12 13 which commenced in 2003 comprising a birth (B cohort; recruited at 0–1 years; birth year 2003/2004) and kindergarten (K cohort; recruited at 4–5 years; birth year 1999/2000) cohort. Using LSAC data, our group previously reported the prevalence of ASD diagnosis at under 7 years of age was higher in the later-born B cohort (2.5%) compared with the K cohort (1.5%).14 This finding was similar to cohort effects found in other countries where later birth years are associated with a higher prevalence of ASD.15 16 Two further time points (known as waves) of LSAC data collection have now been conducted which allow a direct comparison of the two cohorts at ages 10–11 years. Furthermore, teacher report of ASD and other related diagnostic categories are available, providing an additional informant on prevalence of children identified with additional needs in school.
We aimed to (1) compare the Australian prevalence of parent and teacher-reported ASD diagnosis over time in two cohorts of children recruited 4 years apart, (2) examine family demographic and child factors associated with prevalence differences between the two cohorts and (3) compare the prevalence of teacher-reported ASD and any changes in categorisation over time across the two cohorts.
Method
Study design
Details of the LSAC design are reported in our prior study.14 In brief, LSAC employs a cross-sequential design that follows two Australian population representative cohorts of children, initially aged 0–1 years (B cohort; n=4983) and 4–5 years (K cohort; n=5107) in 2003, assessed at two yearly waves with data used in this study collected at the age of 10–11 years (2014 for the B cohort, n=3764; 2010 for the K cohort, n=4164).
Measures
Demographic information
Demographic information was collected from the primary caregiver including neighbourhood socioeconomic disadvantage measured using the Socio-Economic Indexes for Areas Disadvantage Index (SEIFA) corresponding to the family’s postcode of residence,17 and geographic remoteness (dichotomised to very remote/remote or non-remote).18 Remote areas were classified as ‘remote’ by the ABS Australian Standard Geographic Classification (ASGC) Remoteness Classification with 12 of 311 postcodes sampled by LSAC classified as remote.
Parent-reported ASD status
The primary caregiver was asked via interview: ‘Does your child have any of these ongoing conditions?’ from which parents could select ‘Autism, Aspergers, or other autism spectrum’. Parents were also asked the child’s age at diagnosis and to rate his/her severity as mild/moderate/ severe.
Teacher-reported ASD status
Teachers were asked via questionnaire ‘Does this child receive any specialised services provided within the school because of a diagnosed disability or additional need?’ and if endorsed, ‘What is the main reason that the study child requires additional assistance or specialised services to enable them to succeed in the regular school programme?’ Response options were intellectual disability, hearing impairment, vision impairment, physical disability, speech/language impairment, emotional/behavioural problem, poor understanding of standard Australian English/ESL, ASD and learning disability/problems either with reading or mathematics.
Child factors
As described previously,14 emotional/behavioural problems were assessed using the parent-reported and teacher-reported Strengths and Difficulties Questionnaire (SDQ),19 with higher scores indicating more difficulties, except for the prosocial subscale. Quality of life was assessed using the Paediatric quality of life inventory (PedsQL) 4.0 parent proxy report20 with higher scores indicating better health-related quality of life. Language functioning was assessed using the short version of the Peabody Picture Vocabulary Test third edition (PPVT-III)21 and cognitive functioning was assessed using the Matrix Reasoning subtest from the Wechsler Intelligence Scale for Children IV (WISC-IV).22
Procedure
At each LSAC wave, trained interviewers conducted face-to-face interviews with the primary caregiver in the home, supplemented by direct assessments of children and administration of parent and teacher surveys. The LSAC study is approved by the Australian Institute of Family Studies Ethics Committee, and parents provide written informed consent. Permission was granted to use the LSAC data for addressing the current study aims.
Analyses
Aim 1: Summary statistics, including z-tests to compare adjusted proportions, were used to describe differences in parent-reported and teacher-reported ASD prevalence and characteristics for each cohort. Parent-reported ASD prevalence in the K cohort was retrospectively calculated at 6 and 8 years based on the age of diagnosis of parent report at 10/11 years. Teacher-reported ASD status was not available in the K cohort at 6 years.
Aim 2: Unadjusted and adjusted (for a priori confounding variables listed in table 1) linear regression analyses were conducted to examine the association between parent-reported ASD status and child functioning at 10–11 years in both cohorts and parent/teacher-agreed and non-agreed ASD status. Cohen’s d effect sizes are reported to indicate the strength of the differences between groups.
Table 1.
Comparison of sample characteristics for children with ASD in the birth (B) and kindergarten (K) cohorts at 10–11 years
| Measure | B (n=117–145)† |
K (n=78–92)† |
p value |
| Child age in months, mean (SD) | 130.9 (4.0) | 129.5 (3.5) | 0.010* |
| Male (%) | 81.0 | 76.7 | 0.517 |
| Number of children at home, mean (SD) | 2.5 (1.1) | 2.7 (1.3) | 0.380 |
| English main language spoken at home (%) | 94.5 | 95.1 | 0.871 |
| Indigenous (%) | 4.3 | 5.3 | 0.788 |
| Remote/very remote location (%) | 0 | 4.3 | <0.001* |
| Single parent family (%) | 33.2 | 19.0 | 0.056 |
| Maternal age at childbirth, mean (SD) | 30.2 (5.2) | 29.5 (6.6) | 0.497 |
| Paternal age at childbirth, mean (SD) | 33.0 (7.0) | 31.7 (7.0) | 0.289 |
| Primary caregiver did not complete high school (%) | 42.2 | 60.4 | 0.010* |
| Child attends special school (%; teacher report) | 6.6 | 8.6 | 0.590 |
| Neighbourhood disadvantage, mean (SD) | 991.0 (65.8) | 993.1 (58.6) | 0.814 |
AlL proportions are weighted and adjusted for LSAC sample design.
*p<0.05
†N reported as a range due to missing data across the outcomes of interest.
ASD, autism spectrum disorder.
Aim 3: Z-tests were used to compare adjusted proportions of teacher-reported diagnoses between the two cohorts over time. Summary statistics were also used to describe changes in teacher-reported categories over time.
For the above analyses, given the similarity between unadjusted and adjusted findings, we report the adjusted findings. Survey methods were also used to account for the unequal probability of participant selection into the sample, non-response and sample attrition and the multi-stage, clustered sampling design.23 Analyses were conducted in Stata V.14.0.
Results
Prevalence of parent-reported and teacher-reported ASD at 10–11 years
Prevalence of parent-reported ASD was 3.9% (95% CI 3.2 to 4.5) in the B cohort and 2.4% (95% CI 1.6 to 2.9) in the K cohort which was significantly different (p<0.001; figure 1). The mean age of parent-reported ASD diagnosis was 5.62 (SD=0.25) years in the B cohort and 5.34 (SD=0.33) years in the K cohort (p=0.85; figure 2). Parent reports indicated 57% (n=88) of ASD cases in the B and 53% (n=52) in the K cohort were mild, which was not statistically different (p=0.52). Teacher-reported prevalence of ASD was higher in the B cohort (1.7% (95% CI 1.2 to 2.1)) compared with the K cohort (0.9%(95% CI,0.6 to 1.1); p=0.002).
Figure 1.
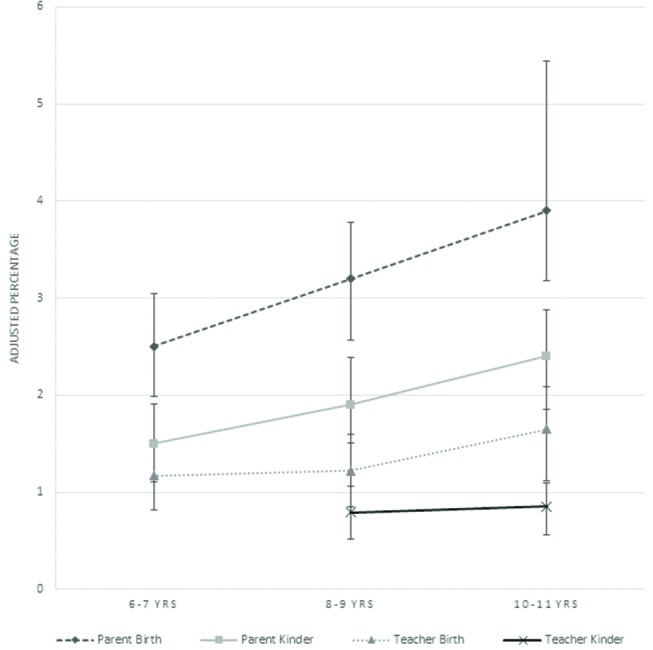
Adjusted prevalence of ASD according to teacher and parent report in the birth (B) and kindergarten (K) cohorts with 95% CI.
Figure 2.
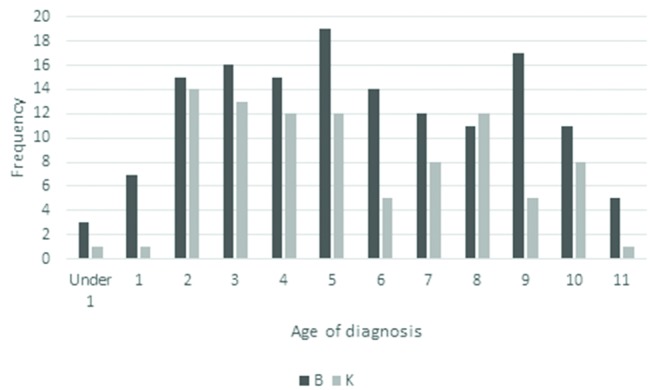
Frequency of age of diagnosis in the birth (B) and kindergarten (K) cohorts according to parent report at 10–11 years.
Figure 1 shows the prevalence of parent-reported and teacher-reported ASD over time and shows a linear increase in parent-reported diagnosis in both cohorts from 6–7 to 10–11 years. The teacher reports show an increase in the B cohort from 8–9 to 10–11 years but a stable report in the K cohort over this time. Of note the B cohort were aged 6–7 years in 2010, 8–9 years in 2012 and 10–11 years in 2014. Whereas the K cohort were 6–7 years in 2006, 8–9 years in 2008 and 10–11 years in 2010.
Differences in demographic and clinical profiles by cohort
Comparisons of demographic measures between children with and without parent-reported ASD for each cohort were repeated as per the previous study.14 Unlike our prior findings, children with ASD in both cohorts had more neighbourhood disadvantage (K cohort, p=0.04; B cohort, p=0.001) compared with children without ASD. In the B ASD group relative to the non-ASD B cohort, none were from remote locations, English was more frequently the main language spoken at home, p=0.03, and there was no difference in the mean number of children at home in those with or without ASD. Children with ASD in the B and K cohorts were directly compared on demographic variables at age 10–11 years (table 1). The children with ASD in the K cohort were younger at wave six than the B cohort and a higher proportion of primary caregivers did not complete highschool in the K cohort than in the B cohort. The difference in primary caregiver education level between the B and K cohorts with ASD is also found in the overall LSAC sample and reflects differences in the B and K cohorts rather than being specific to children with ASD diagnoses.
Children with ASD in the two cohorts were directly compared on the SDQ and PedsQL (table 2). Parents of children with ASD in the K cohort reported a higher school quality of life on the PedsQL and more conduct, peer and total difficulties on the SDQ compared with parents of children with ASD in the B cohort. Teachers’ reported lower levels of prosocial behaviour on the SDQ for children with ASD in the K compared with B ASD cohort. There were no differences between cohorts on all other variables including cognitive and language functioning.
Table 2.
Adjusted differences in functioning between children with ASD in the birth (B) and kindergarten (K) cohort at 10–11 years of age
| Measure | B ASD group M (SD) (n=62– 91)† | K ASD group M (SD) (n=120–145)† | Adjusted‡ mean difference (95% CI) | Effect size | p value |
| Quality of life (PedsQL)§ | |||||
| Physical | 66.0 (21.0) | 67.8 (19.0) | 3.9 (−2.2 to 10.0) | 0.2 | 0.204 |
| Emotional | 52.2 (19.6) | 54.6 (16.6) | 1.8 (−4.7 to 8.3) | 0.1 | 0.586 |
| Social | 55.0 (21.2) | 50.0 (22.9) | −5.3 (−12.0 to 1.4) | −0.3 | 0.123 |
| School | 53.9 (18.8) | 57.6 (15.3) | 5.8 (0.5 to 11.0) | 0.3 | 0.032* |
| Psychosocial | 53.7 (15.7) | 54.0 (14.0) | 0.8 (−4.2 to 5.7) | 0.0 | 0.752 |
| Total | 58.0 (15.8) | 58.8 (13.9) | 1.9 (−3.0 to 6.8) | 0.1 | 0.447 |
| SDQ parent | |||||
| Emotional | 4.0 (4.1) | 4.8 (2.7) | 0.6 (−0.4 to 1.6) | 0.1 | 0.220 |
| Conduct | 3.6 (3.5) | 4.2 (1.4) | 0.7 (0.1 to 1.2) | 0.1 | 0.031* |
| Hyperactivity | 5.9 (4.1) | 6.5 (2.4) | 0.8 (0 to 1.6) | 0.1 | 0.059 |
| Peer | 4.0 (3.8) | 4.9 (2.2) | 0.8 (0.1 to 1.5) | 0.1 | 0.036* |
| Prosocial§ | 6.3 (4.0) | 6.6 (2.3) | 0.1 (−0.8 to 1.0) | 0.0 | 0.820 |
| Total | 17.5 (14.2) | 20.4 (6.4) | 2.9 (0.5 to 5.3) | 0.1 | 0.020* |
| SDQ teacher | |||||
| Emotional | 3.2 (2.5) | 2.8 (2.3) | −0.6 (−1.5 to 0.2) | −0.4 | 0.122 |
| Conduct | 3.0 (1.5) | 3.0 (1.5) | 0.1 (−0.4 to 0.7) | 0.1 | 0.715 |
| Hyperactivity | 5.2 (3.1) | 5.6 (2.7) | 0.3 (−0.7 to 1.4) | 0.1 | 0.515 |
| Peer | 3.2 (2.3) | 3.7 (2.4) | 0.7 (−0.1 to 1.4) | 0.4 | 0.093 |
| Prosocial† | 5.6 (2.7) | 4.7 (2.7) | −0.9 (−1.6 to −0.1) | −0.4 | 0.022* |
| Total | 14.5 (7.1) | 15.1 (6.7) | 0.5 (−1.9 to 2.9) | 0.1 | 0.685 |
| Cognitive functioning (matrices age 10) | 9.2 (3.7) | 8.6 (3.6) | −0.4 (−1.5 to 0.6) | −0.1 | 0.409 |
| Receptive vocab (PPVT) at age 8/9 | 77.7 (5.5) | 76.2 (6.2) | −1.4 (−3.2 to 0.4) | −0.3 | 0.124 |
*p<0.05.
N reported as a range due to missing data across the outcomes of interest.
Adjusted for child age and gender, number of children in the home, language spoken at home, indigenous status, geographic location.
Lower scores indicate poorer functioning.
ASD, autism spectrum disorder; PPVT, Peabody Picture Vocabulary Test; SDQ, Strengths and Difficulties Questionnaire.
Parents of children classified as mild in the K cohort more frequently endorsed ‘Other kids not wanting to be friends’ on the PedsQL than mild ASD children in the B cohort, z=−2.27, p=0.02. Mild ASD children in the B cohort had poorer teacher-reported prosocial behaviour on the SDQ than mild ASD children in the K cohort, z=−2.80, p=0.005 (table 3).
Table 3.
Adjusted percentage (with 95% CI) of 10–11-year-old children in the clinical/below average range on outcome measures across birth (B) and kindergarten (K) cohorts.
| All ASD M (95% CI) (B n=120–145; K n=62–91)* |
Mod-severe ASD M (95% CI) (B n=47–57; K n=24–39)* | Mild ASD M (95% CI) (B n=71–88; K n=38–49)* | No ASD M (95% CI) (B n=2962–3551; K n=3286–4012)* | |
| One or more social problems | ||||
| B cohort | 81.9 (75.3 to 88.6) | 95.7 (91.1 to 100.0) | 71.2 (61 to 1.81.3) | 30.0 (27.0 to 30.9) |
| K cohort | 87.4 (80.5 to 94.4) | 95.4 (89.5 to 100.0) | 80.0 (68.3 to 91.6) | 35.4 (33.2 to 37.6) |
| PedsQL items | ||||
| Difficulty getting along with other kids† | ||||
| B cohort | 28.3 (20.2 to 36.5) | 36.7 (21.8 to 51.6) | 22.1 (12.3 to 31.9) | 8.7 (7.5 to 9.8) |
| K cohort | 33.1 (21.6 to 44.5) | 51.9 (34.7 to 69.2) | 17.1 (5.0 to 29.2) | 13.9 (12.4 to 15.4) |
| Other kids not wanting to be friends† | ||||
| B cohort | 27.3 (19.6 to 35.1) | 38.1 (22.8 to 53,4) | 19.4 (11.8 to 27.0) | 4.7 (3.8 to 5.6) |
| K cohort | 42.2 (31.8 to 52.7) | 48.8 (30.3 to 67.2) | 36.8 (22.8 to 50.8) | 4.0 (3.3 to 4.5) |
| SDQ-parent report | ||||
| Peer | ||||
| B cohort | 65.2 (57.2 to 73.3) | 87.5 (79.5 to 95.5) | 48.7 (38.7 to 58.8) | 11.4 (10.1 to 12.7) |
| K cohort | 74.8 (65.6 to 84.0) | 89.0 (79.7 to 98.3) | 62.7 (47.9 to 77.6) | 13.1 (11.7 to 14.5) |
| Prosocial‡ | ||||
| B cohort | 17.5 (11.9 to 25.1) | 25.4 (12.6 to 38.2) | 11.7 (4.1 to 19.3) | 3.6 (2.8 to 4.4) |
| K cohort | 22.0 (12.6 to 31.5) | 32.4 (14.8 to 50.0) | 13.3 (4.3 to 22.2) | 2.2 (1.7 to 2.7) |
| SDQ-teacher report | ||||
| Peer | ||||
| B cohort | 46.2 (36.3 to 56.1) | 54.8 (38.2,71.4) | 39.7 (27.6 to 51.8) | 10.8 (9.5 to 12.0) |
| K cohort | 49.1 (35.6,62.6) | 73.4 (52.2 to 94.6) | 33.0 (19.2 to 46.7) | 11.7 (10.5 to 12.8) |
| Prosocial | ||||
| B cohort | 33.6 (23.9 to 43.4) | 47.6 (30.7 to 64.4) | 23.5 (12.4 to 34.7) | 8.7 (7.5 to 9.9) |
| K cohort | 50.9 (37.7 to 64.1) | 52.4 (27.0 to 77.9) | 49.9 (33.7 to 66.0) | 8.3 (7.2 to 9.5) |
| Clinical range for cognitive functioning (matrices)‡ | ||||
| B cohort | 27.1 (18.9 to 35.4) | 41.5 (25.1 to 58.0) | 17.9 (9.0,26.8) | 17.5 (15.8,19.3) |
| K cohort | 33.9 (22.4,45.4) | 45.1 (26.7,63.6) | 24.3 (9.8,38.8) | 13.4 (11.8,15.0) |
| Clinical range in receptive vocabulary (PPVT-III) | ||||
| <16th percentile | ||||
| B cohort | 7.4 (1.7 to 13.0) | 11.7 (0.0 to 2.4) | 4.6 (0.0 to 10.0) | 2.3 (1.7 to 3.0) |
| K cohort | 10.8 (1.6 to 20.2) | 14.8 (0.0 to 29.7) | 7.4 (0.0 to 18.4) | 2.9 (2.2 to 3.6) |
| <2nd percentile | ||||
| B cohort | 2.0 (0.0 to 5.1) | 0 | 3.3 (0.0 to 8.4) | 0.4% (0.2 to 0.7) |
| K cohort | 4.0 (0.0 to 8.1) | 3.7 (0.0 to 9.6) | 4.3 (0 to 10.4) | 0.4 (0.2 to 0.6) |
N reported as a range due to missing data across the outcomes of interest.
Scores below the average range, that is, a score of 7 or below.
Social domains examined: two PedsQL items (difficulty getting along with other kids and other kids not wanting to be friends); parent-reported and teacher-reported SDQ subscales (peer problems and prosocial behaviour).
ASD, autism spectrum disorder; PPVT, Peabody Picture Vocabulary Test; PedsQL, PediatricPaediatric Quality of Life; SDQ, Strengths and Difficulties Questionnaire.
Differences in teacher reported and parent-reported ASD compared with parent-only-reported ASD
The overlap of parent and teacher ASD reports in the two cohorts at 10–11 years was examined. There was parent and teacher agreement for B n=56 (39% of parent-reported group) and K n=32 (36% of parent-reported group). Teachers reported an additional B n=8 and K n=4 cases with ASD which were not identified by parents. For the parent-reported cases where there was no agreement, 15% in both cohorts were classified by teachers under another category.
Differences in clinical functioning were compared as presented in table 4. In the B, but not the K, cohort, parent’s reported lower social QoL in the agreed teacher/parent ASD cases than in the parent-only ASD cases. Teachers reported more conduct, hyperactivity, social and peer problems, less pro-social behaviour and overall more total emotional/behavioural problems on the SDQ in the agreed teacher/parent B cohort ASD cases than the parent-only-reported cases.
Table 4.
Adjusted differences in functioning between children with parent-reported-only reported (no teacher agreement) versus parent-reported and teacher-reported ASD within the B and K cohorts at 10–11 years of age
| Measure | K ASD Teacher and parent-reported M (SD) N=30–32† | K ASD Parent-only-reported (no teacher agreement) M (SD) N=13–43† | B ASD Teacher-reportedand parent-reported M (SD) N=51–56† | B ASD Parent-only-reported (no teacher agreement) M (SD) N=40–64† |
| Quality of life (Peds QL)§ | ||||
| Physical | 66.4 (15.9) | 70.4 (18.6) | 65.2 (18.2) | 69.1 (21.3) |
| Emotional | 55.9 (13.9) | 54.9 (2.8) | 54.8 (18.4) | 49.4 (22.2) |
| Social | 47.3 (21.4) | 53.7 (23.1) | 52.2 (19.4)* | 59.5 (21.4)* |
| School | 60.0 (13.6) | 58.4 (17.1) | 53.2 (15.9) | 54.8 (21.5) |
| Psychosocial | 54.5 (13.4) | 55.7 (14.8) | 53.4 (13.8) | 54.5 (17.3) |
| Total | 58.6 (12.5) | 60.8 (2.1) | 57.5 (13.5) | 59.6 (17.1) |
| SDQ parent | ||||
| Emotional | 3.8 (2.2) | 4.8 (2.9) | 3.8 (2.6) | 4.2 (5.6) |
| Conduct | 3.9 (1.0) | 4.0 (1.4) | 3.9 (1.6) | 3.3 (4.9 |
| Hyperactivity | 6.3 (2.3) | 6.2 (2.4) | 6.7 (2.5) | 5.3 (5.5) |
| Peer | 4.8 (2.0) | 5.0 (2.3) | 4.4 (2.1) | 3.6 (5.2) |
| Prosocial§ | 6.0 (2.6) | 6.7 (2.2) | 6.6 (2.2) | 5.9 (5.6) |
| Total | 18.9 (5.1) | 20.1 (6.5) | 18.8 (6.1) | 16.4 (20.2) |
| SDQ teacher | ||||
| Emotional | 3.4 (2.5) | 2.9 (3.1) | 3.4 (2.3) | 2.6 (2.4) |
| Conduct | 3.3 (1.8) | 2.9 (1.4) | 3.6 (1.6)*** | 2.2 (1.0)*** |
| Hyperactivity | 5.5 (2.4) | 5.0 (4.0) | 6.1 (2.6)*** | 3.7 (3.3)*** |
| Peer | 4.1 (2.4) | 3.3 (2.4) | 3.9 (2.3)** | 2.4 (2.2)** |
| Prosocial§ | 4.0 (2.3) | 5.6 (2.9) | 5.0 (2.6)* | 6.8 (2.4)* |
| Total | 16.3 (7.2) | 14.2 (8.3) | 17.0 (6.6)*** | 10.9 (6.8)*** |
| Cognitive functioning (matrices age 10) | 9.3 (3.7) | 8.7 (3.5) | 9.1 (3.7) | 9.6 (3.5) |
| Receptive vocab (PPVT at age 8/9) | 76.5 (7.6) | 76.7 (5.9) | 77.3 (5.9) | 79.0 (5.1) |
*p<0.05, **p<0.01, ***p<0.001.
N reported as a range due to missing data across the outcome measures.
Lower scores indicate poorer functioning.
ASD, autism spectrum disorder; SDQ, Strengths and Difficulties Questionnaire; PPVT, Peabody Picture Vocabulary Test.
Teacher-reported special assistance categories and change over time
At age 8–9 years, there was a similar number of children categorised by teachers as having ASD in both cohorts (z=1.9, p=0.05) and emotional/behavioural problems (z=1.19, p=0.24). At 10–11 years, there were significantly more children categorised as having ASD by teachers in the B cohort compared with the K cohort (z=3.2, p=0.001) and more children categorised as having emotional/behavioural problems in the K cohort (z=2.2, p=0.03), figure 3.
Figure 3.
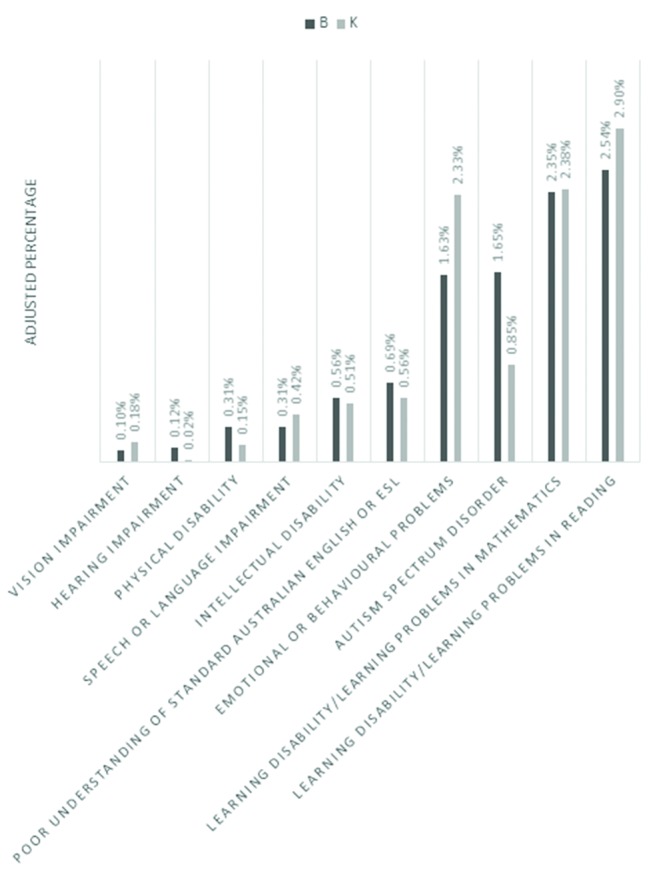
Adjusted teacher-reported percentages of students requiring special assistance in school in the birth (B) and kindergarten (K) cohorts at 10–11 years of age.
Children categorised with ASD by teachers at 10–11 years were examined over time to explore their prior categorisation at 8–9 years to understand any changes in categorisation. Of the 36 children categorised with ASD at 10–11 years in the K cohort, at age 8–9 years, 15 (42%) had not been categorised, 5 (14%) were classified under another category (one gifted, two intellectual disability and one emotional/behavioural problems) and 17 (47%) had a stable ASD categorisation. Of the 64 children categorised with ASD at 10–11 years in the B cohort, at 8–9 years, 32 (50%) had not been categorised, 6 (9%) were classified under another category (one gifted, two emotional/behavioural problems and three learning disorders) and 26 (41%) had a stable ASD categorisation.
Discussion
This study found parent-reported ASD diagnosis differed between the kindergarten (2.4%; birth years 1999/2000) and birth (3.9%; birth years 2003–2004) cohorts at 10–11 years of age. Teacher-reported ASD also differed between the two cohorts but with a lower reported percent of children requiring special assistance with ASD, with the prevalence at 10–11 years being 0.9% (K cohort) and 1.7% (B cohort).
Parent- and teacher-reported ASD
Parent-reported prevalence continued to be higher in the later-born B cohort (birth years 2003/2004) than the K cohort (birth years 1999/2000), consistent with the cohort effect of higher prevalence of ASD in later-born cohorts.15 24 However, the 3.9% reported in the B cohort by parents is higher than prior Australian and international studies. Parent-reported ASD prevalence in the K cohort was similar to a recent US study using parent report (2.2%).4 Teacher-reported prevalence in both cohorts was slightly lower than recent international estimates from educational systems, such as Northern Ireland where prevalence of ASD was 2.3%.5
There are a number of possible explanations for the higher parent and teacher prevalence in the B cohort. For example, there has been increased public awareness of ASD in Australia which may result in more children in the B cohort being diagnosed when parents were interviewed in 2014, compared with those in the K cohort who provided information in 2010.25 After the commencement of LSAC, a major Australian funding reform, called the Helping Children with Autism (HCWA) package was commenced in July 2008 including, but not limited to, financial support for diagnosis (four allied health sessions), early intervention (AU $12 000 for children diagnosed before the age of 7 years) and therapy services (20 sessions if a plan was created before the age of 13 years) for children with ASD. Whether the increase in prevalence in both cohorts over time or the differences between the B and K cohorts were influenced by changes to entitlements in Australia for ASD services could not be established from the current data. Notably, the B cohort had higher prevalence of parent reported diagnoses than the K cohort before, during and after they were eligible for the early intervention funding, based on parent-reported age of diagnosis. The peak age of diagnosis in the B cohort was at 5 years which corresponded to the commencement of the cohort’s eligibility to receive HCWA funding (2008/2009). There was also a drop in parent-reported diagnosis between the ages of 6 and 8 years, particularly in the B cohort (figure 2). This peak and then drop may be due to families seeking early diagnosis to be eligible for aged-based early intervention funding. This could also relate to school entry, which is age 5–6 years in Australia. Diagnoses are likely to be sought prior to commencement of primary school so children can receive special assistance in the education setting. In addition, an increase in new diagnoses of milder presentations of ASD in later primary years has previously been reported26 as the expectations for social communication and behaviour increase.1
Differences in cohort profiles
Previous research has suggested that increased ASD prevalence may be due to the identification of cases with milder impairment.15 In support of this, those in the B cohort with parent-reported ASD had fewer emotional/behavioural symptoms than those diagnosed in the K cohort; although there was no difference in the verbal or abstract reasoning ability using direct assessment measures. However, these tasks were brief measures of language and abstract reasoning ability and do not provide a comprehensive picture of cognition and language functioning as previously noted.14 It is also possible that the later-born B cohort received more autism early intervention than the K cohort given they had access to HCWA funding for early intervention, which may have improved their functioning levels relative to the K cohort who did not have access to this funding. The 2013 release of DSM-5 changed the categorisation of ASD. However, most children in the B cohort and all children in the K cohort were diagnosed, according to parent-reported age of diagnosis, before DSM-5 hence this is unlikely to have had an impact on the current findings.
Teacher/parent-agreed cases
Only around one-third (36% B cohort, 39% K cohort) of children with a parent-reported ASD diagnosis also had a corresponding teacher categorisation of ASD. This could relate to the differences in the way the questions were asked of teachers and parents. Teachers were asked whether the child received specialised services at school because of a diagnosed disability or additional need, which may have only captured children who have ASD and qualify for services under educational adjustment programs, which have strict eligibility criteria. Teachers and parents may also have different understandings of the symptoms of ASD.
The proportion of teacher/parent-agreed ASD cases in each cohort was similar; however, when the teacher/parent-agreed children were compared with the parent-only-reported cases, differences were present in clinical profiles in the two cohorts. In the B cohort, parent/teacher-agreed children with ASD were reported to have more severe emotional and behavioural problems than the parent-only-agreed cases. In the K cohor,t there were no differences between parent/teacher-agreed and parent-only cases. This indicates that milder cases in the B cohort had been identified by parents (but not teachers) as having ASD.
In interpreting the difference between teacher- and parent-reported prevalence of ASD, we cannot exclude the possibilities that teachers may not be aware of some ASD cases, that some children with ASD do not experience enough impairment at school to require specialised services in this setting or that some children with ASD do require specialised services at school but do not receive them. Further research is required to understand if there are children with ASD who require but do not receive additional assistance in the education setting.
Teacher-reported special assistance categories and change over time
While individual change to ASD from other categories from 8–9 to 10–11 years was low (K cohort n=5, B cohort n=6) teachers reported significantly more ASD in the B than K cohort at age 10–11, with a non-significant difference at 8–9 years. This suggests a recent preference to record children under the ASD category rather than other categories in the school setting. A prior study of US school system data found that up to 60% of the increase in ASD prevalence was due to children previously being categorised under other labels, such as intellectual disability, being reclassified as ASD.9 Changes within states of Australia over time in the definition of these disability categories may also have influenced these findings. For example, it may have become easier to meet eligibility criteria under the ASD category compared with other categories.
Strengths and limitations
The main strength of this study is the use of a nationally representative Australian sample. The key limitation is the use of parent and teacher reports of ASD status in children, rather than clinician-verified diagnoses. A difference in the questions asked of parents and teachers, as previously noted, was also a limitation preventing direct comparisons between these groups.
Implications
The increase in ASD prevalence has significant economic implications which have been highlighted by recent reports from other high income countries such as the UK27 and the USA.28 The recent UK report states that it is crucial to accurately identify children so that they can access evidence-based early interventions.27 However, there are also significant economic and social costs if children are allocated services based on a diagnosis without consideration of their severity level or specific needs.
Conclusions
These longitudinal findings point to the changing nature of ASD between the late 1990s, when the first cohort were born, and today, with changes occurring before 2013, when the fifth edition of the Diagnostic and Statistical Manual for Mental disorders was launched, including for the first time ASD as a diagnosis. This study highlights the complexities involved in understanding changes in the reported prevalence of ASD that are likely to be multifactorial. It has provided evidence in Australia of changes in diagnostic preferences and a broadening of the spectrum and that differences in service requirements can influence prevalence estimates.
bmjopen-2016-015549supp001.doc (88KB, doc)
Supplementary Material
Acknowledgments
This article uses confidential unit record files from the LSAC survey. The LSAC was initiated and funded by the Commonwealth Department of Families, Housing, Community Services and Indigenous Affairs and was managed by the Australian Institute of Family Studies. The findings and views reported in this article are those of the authors and should not be attributed to either the Commonwealth Department of Families, Housing, Community Services and Indigenous Affairs, or the Australian Institute of Family Studies. We thank all the families participating in the LSAC study. We wish to thank Melinda Randall, Elfriede Ihsen, Daryl Efron and Cheryl Dissanayake for their contribution to the prior paper reporting LSAC ASD prevalence at under 7 years.
We wish to thank the William Collie Trust, University of Melbourne, for their support of authors Dr May, Professor Williams and Ms Brignell. Dr Sciberras is funded by an NHMRC Early Career Fellowship 1037159 (2012–2015) and an NHMRC Career Development Fellowship 1110688 (2016–2019). Dr Sciberras also acknowledges the support of the NHMRC-funded Centre of Research Excellence in Child Language (1023493).
Footnotes
Contributors: The authors alone are responsible for the content and writing of the paper. TM, ES, AB and KW all made a substantial contribution to the study design and conception. TM completed the data analysis and drafted the initial version of the paper. TM, ES, AB and KW made a substantial contribution to the interpretation of findings. ES, AB and KW revised and critically reviewed the paper. TM, ES, AB and KW provided approval of the final version to be published. All authors are accountable for all aspects of the work.
Competing interests: None declared.
Ethics approval: Australian Institute of Family Studies Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: This dataset is available from Australian Institute of Family Studies.
References
- 1. Diagnostic and statistical manual of mental disorders (DSM-5). Washington DC: American Psychiatric Publications, 2013. [DOI] [PubMed] [Google Scholar]
- 2. Elsabbagh M, Divan G, Koh YJ, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res 2012;5:160–79. 10.1002/aur.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kim YS, Leventhal BL, Koh YJ, et al. Prevalence of autism spectrum disorders in a total population sample. Am J Psychiatry 2011;168:904–12. 10.1176/appi.ajp.2011.10101532 [DOI] [PubMed] [Google Scholar]
- 4. Zablotsky B, Black LI, Maenner MJ, et al. Estimated prevalence of autism and other developmental disabilities following questionnaire changes in the 2014 National Health Interview Survey. Natl Health Stat Report 2015;87:1–21. [PubMed] [Google Scholar]
- 5. Waugh I. The prevalence of autism (including Asperger Syndrome) in school age children in Northern Ireland Health do Belfast, Northen Ireland: Northern Ireland Statistics & Research Agency, 2016. [Google Scholar]
- 6. King MD, Fountain C, Dakhlallah D, et al. Estimated autism risk and older reproductive age. Am J Public Health 2009;99:1673–9. 10.2105/AJPH.2008.149021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schieve LA, Rice C, Devine O, et al. Have secular changes in perinatal risk factors contributed to the recent autism prevalence increase? Development and application of a mathematical assessment model. Ann Epidemiol 2011;21:930–45. 10.1016/j.annepidem.2011.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Coo H, Ouellette-Kuntz H, Lloyd JE, et al. Trends in autism prevalence: diagnostic substitution revisited. J Autism Dev Disord 2008;38:1036–46. 10.1007/s10803-007-0478-x [DOI] [PubMed] [Google Scholar]
- 9. Polyak A, Kubina RM, Girirajan S. Comorbidity of intellectual disability confounds ascertainment of autism: implications for genetic diagnosis. Am J Med Genet B Neuropsychiatr Genet 2015;168:600–8. 10.1002/ajmg.b.32338 [DOI] [PubMed] [Google Scholar]
- 10. King M, Bearman P. Diagnostic change and the increased prevalence of autism. Int J Epidemiol 2009;38:1224–34. 10.1093/ije/dyp261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hansen SN, Schendel DE, Parner ET. Explaining the increase in the prevalence of autism spectrum disorders: the proportion attributable to changes in reporting practices. JAMA Pediatr 2015;169:56–62. 10.1001/jamapediatrics.2014.1893 [DOI] [PubMed] [Google Scholar]
- 12. Gray M, Sanson A. Growing up in Australia: the longitudinal study of australian children. Family Matters 2005;72:4. [Google Scholar]
- 13. Sanson A, Nicholson J, Ungerer J, et al. ; Introducing the longitudinal study of australian children, 2002. [Google Scholar]
- 14. Randall M, Sciberras E, Brignell A, et al. Autism spectrum disorder: presentation and prevalence in a nationally representative australian sample. Australian and New Zealand Journal of Psychiatry 2015:0004867415595287. [DOI] [PubMed] [Google Scholar]
- 15. Keyes KM, Susser E, Cheslack-Postava K, et al. Cohort effects explain the increase in autism diagnosis among children born from 1992 to 2003 in California. Int J Epidemiol 2012;41:495–503. 10.1093/ije/dyr193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schieve LA, Rice C, Yeargin-Allsopp M, et al. Parent-reported prevalence of autism spectrum disorders in US-born children: an assessment of changes within birth cohorts from the 2003 to the 2007 National Survey of Children’s Health. Matern Child Health J 2012;16 Suppl 1:151–7. 10.1007/s10995-012-1004-0 [DOI] [PubMed] [Google Scholar]
- 17. Australian Bureau of Statistics. 2033.0. 55.001-Census of Population and Housing: socio-economic indexes for areas (SEIFA), Australia. 2011: Australian Bureau of Statistics Canberra, Australia 2013. [Google Scholar]
- 18. Deparment of Health and Aged Care. DoHaA C, Measuring remoteness: accessibility/remoteness index of Australia (ARIA. editor Canberra, ACT, Australia: Deparment of Health and Aged Care, 2001. [Google Scholar]
- 19. Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581–6. 10.1111/j.1469-7610.1997.tb01545.x [DOI] [PubMed] [Google Scholar]
- 20. Varni JW, Burwinkle TM, Seid M, et al. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr 2003;3:329–41. [DOI] [PubMed] [Google Scholar]
- 21. Dunn L, Dunn L. Peabody picture vocabulary test. 3rd edition Circle Pines, MN: American Guidance Service, 1997. [Google Scholar]
- 22. Wechsler D. Wechsler Intelligence Scale for Children–fourth edition (WISC-IV). San Antonio, TX: The Psychological Corporation, 2003. [Google Scholar]
- 23. Soloff C, Lawrence D, Misson S, et al. ; Wave 1 weighting and non-response: australian Institute of Family Studies Melbourne, 2006. [Google Scholar]
- 24. Raz R, Weisskopf MG, Davidovitch M, et al. Differences in autism spectrum disorders incidence by sub-populations in Israel 1992-2009: a total population study. J Autism Dev Disord 2015;45:1062–9. 10.1007/s10803-014-2262-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Barbaro J, Ridgway L, Dissanayake C. Developmental surveillance of infants and toddlers by maternal and child health nurses in an Australian community-based setting: promoting the early identification of autism spectrum disorders. J Pediatr Nurs 2011;26:334–47. 10.1016/j.pedn.2010.04.007 [DOI] [PubMed] [Google Scholar]
- 26. Daniels AM, Mandell DS. Explaining differences in age at autism spectrum disorder diagnosis: a critical review. Autism 2014;18:583–97. 10.1177/1362361313480277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Iemmi V, Knap M, Ragan I. The autism dividend: reaping the rewards of better investment. UK: National Autism Project, 2017. [Google Scholar]
- 28. Leigh JP, Du J. Brief report: forecasting the Economic burden of autism in 2015 and 2025 in the United States. J Autism Dev Disord 2015;45:4135–9. 10.1007/s10803-015-2521-7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-015549supp001.doc (88KB, doc)


