Abstract
Objectives
The aim of this study was to explore whether recording in primary care of a previously recorded hospital diagnosis was associated with increased patient utilisation of recommended medications.
Design
Registry-based prospective cohort study.
Setting and participants
19 072 patients with a hospital discharge diagnosis of transient ischaemic attack (TIA), stroke or acute coronary syndrome from hospitals in Stockholm County 2010–2013 were included in the study.
Main outcome measure
The outcome of the study was medication dispensation as a marker of adherence to recommended medications. Adherence was defined as having had at least two filled prescriptions in the third year following hospital discharge.
Results
Recording a diagnosis was associated with higher utilisation of all recommended medications with the exception of antihypertensives in patients with TIA. The differences between the groups with and without a recorded diagnosis remained after adjusting for age, sex, index year and visits to private practitioners. Dispensation of antithrombotics was high overall, 80%–90% in patients without a recorded diagnosis and 90%–94% for those with a diagnosis. Women with recorded ischaemic stroke/TIA/acute coronary syndrome were dispensed more statins (56%–71%) than those with no recorded diagnosis (46%–59%). Similarly, 68%–83% of men with a recorded diagnosis were dispensed statins (57%–77% in men with no recorded diagnosis). The rate of diagnosis recording spanned from 15% to 47% and was especially low in TIA (men 15%, women 16%).
Conclusion
Recording a diagnosis of TIA/stroke or acute coronary syndrome in primary care was found to be associated with higher dispensation of recommended secondary preventive medications. Further study is necessary in order to determine the mechanisms underlying our results and to establish the utility of our findings.
Keywords: primary care, quality in health care, preventive medicine, clinical pharmacology, myocardial infarction, stroke
Strengths and limitations of this study.
Whether or not recording a primary care diagnosis is associated with greater dispensation of recommended medication is something that, to our knowledge, has not been investigated before.
The study is based on data from a registry, which includes all residents in Stockholm County and not just a sample.
In stroke and acute coronary syndrome, the validity of discharge diagnosing in hospitals is higher than for transient ischaemic attack where there may be greater uncertainty and variation in accuracy of diagnosing due to the diagnosis defining lack of objective symptoms.
The included diagnoses were chosen in order to select patients where secondary preventive pharmacological treatment was indicated and clearly defined which limits the possibility to generalise the results to a more diverse primary care population.
Introduction
Fragmentation of healthcare and the lack of communication between different segments of the healthcare system are well-known problems affecting many countries worldwide, including Sweden.1–6 Previous studies have shown that the transfer of information between hospitals and primary care including information on discharge medication, frequently is insufficient and that this lack of communication may affect subsequent patient care.7 8 Primary care is the level of care most patients with chronic disease will depend on for their long-term care in Sweden.9 It is mandatory in Stockholm for a primary care physician to record at least one diagnosis after every consultation. To our knowledge, it has not been studied whether the choice of diagnosis influences patient-related outcomes such as medication utilisation. For several acute conditions initially treated in hospital, an important part of chronic care is patients taking secondary preventive medications. It is however well known that adherence to recommended medications declines after discharge and is often suboptimal in the long term.10–13
In this study, we explore if ‘recording a diagnosis’ has an impact on the utilisation of recommended medications. In our study, if a primary care physician ‘records a diagnosis’ it means that a patient discharged from hospital care to primary care is diagnosed with their hospital diagnosis, or a corresponding follow-up diagnosis, in primary care at some point. A diagnosis that is not being recorded in primary care could be an indication of lack of communication between the different healthcare providers, which could affect the quality of the subsequent treatment. If there is an association between recording of diagnosis and utilisation of recommended medications, then ‘recording a diagnosis’ could potentially be used as a quality indicator in primary care.
To investigate whether recording a diagnosis in primary care is associated with increased dispensation of recommended medication in the long-term care, four common groups of diagnoses with clear and evidence-based clinical guidelines,14–16 with regard to medical treatment were chosen: acute coronary syndromes, ischaemic and haemorrhagic stroke and transient ischaemic attack (TIA).
Objective
The aim of this study was to explore whether recording a diagnosis in primary care was associated with patient utilisation of recommended medications in the long term. We hypothesised that patients with a recorded diagnosis were more likely to be dispensed recommended medications.
Methods
Setting
Stockholm County Council provides healthcare to 2.2 million inhabitants at three levels: inpatient acute care at seven hospitals, outpatient secondary specialist care at hospitals or contracted specialist units and primary care in 208 centres. Approximately 90% of the population chooses to list at a primary care practice (private or public) for their basic care.17 ‘Listing’ means a patient choosing a specific centre to be their provider of primary care, with complete freedom to change provider at any point in time. The remaining part will be living in nursing homes or be unlisted. As an alternative to primary care practices, people may also visit some hundred private specialists working on the basis of the National tariff system (nationella taxan).
Study design and participants
For this registry-based prospective cohort study, data from the Stockholm County Council regional healthcare database, VAL, were used. The VAL database contains anonymised and encrypted data on the healthcare consumption, including dispensed medications, for the 2.2 million individuals residing in Stockholm County. The data include detailed information from both inpatient and outpatient care including primary care. Diagnoses from inpatient care and secondary care are registered from 1993 and diagnoses from primary care are available from 2003. More than 95% of visits to primary care physicians are coded with one or more diagnoses according to the International Classification of Diseases (ICD) system. The database also contains information on age, sex, migration and mortality for all residents.18
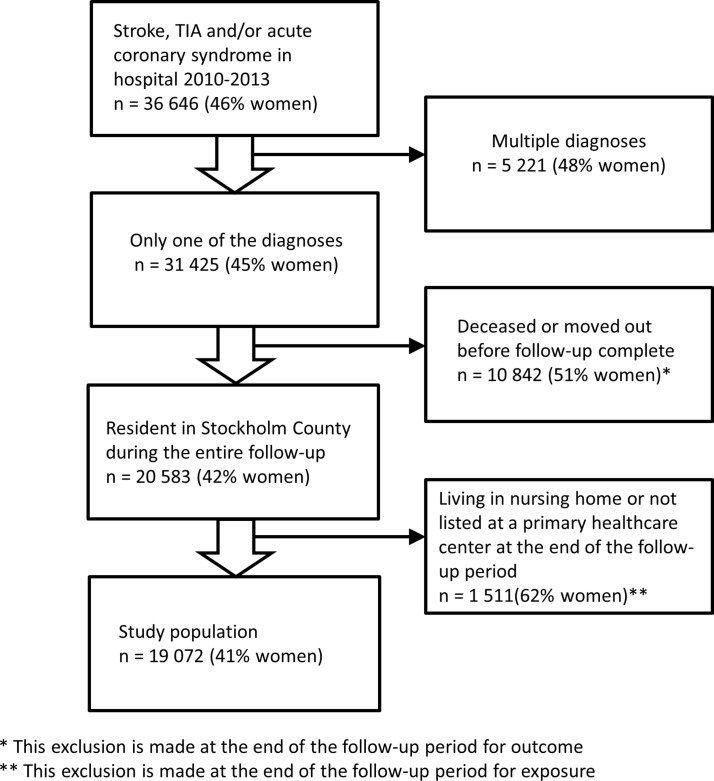
Unique patients living in Stockholm County who received a discharge diagnosis of stroke, TIA and/or acute coronary syndrome from hospitals in Stockholm County between 1 January 2010 and 31 December 2013 (see supplementary table S1 for specific ICD-10 codes) were selected using the VAL database. The year in which a patient received a diagnosis is referred to as the index year. Patients receiving different prespecified discharge diagnoses during the study period or the same discharge diagnoses during more than 1 year were excluded from the study (‘multiple diagnoses’ in figure 1). By excluding patients with more than one of the diagnoses (eg, acute coronary syndrome and haemorrhagic stroke), we were able to be more certain of which medications were recommended as secondary prevention for each patient. Patients discharged with the same diagnosis multiple times during the study period (eg, ischaemic stroke during the index year and the year after) were excluded since, in those cases, it would have been difficult to determine if a hospital or a primary care centre was in charge of the patients’ long-term care during the study. As a sensitivity analysis, we have followed the excluded patients with multiple diagnoses in the same way as the included patients. These results are presented in the supplementary figure S1 and supplementary tables S2–S4.
Figure 1.
Selection of study population.
bmjopen-2016-015723supp001.pdf (498.4KB, pdf)
We also excluded patients who died before the end of their follow-up period, patients living in nursing homes and individuals that were not listed at a primary healthcare centre.
Out of the total 36 646 patients initially selected, 19 072 were finally included in the study population. Out of these, 41% were women (see figure 1).
Recording a diagnosis in primary care
The recording of a diagnosis in primary care was the predefined exposure within the cohort. Recording a diagnosis was defined as the recording of a primary care diagnosis related to, but not necessarily identical with, the initial hospital diagnosis during the 2 years following the index year (irrespective of month). This period was defined as the recording period. Patients with a hospital diagnosis in 2010 were thus analysed with regard to recording of a diagnosis in primary care in 2011–2012 and those with hospital diagnosis 2011 were analysed 2012–2013, etc. Patients not receiving any of the prespecified diagnoses (see supplementary table S1) were defined as not recorded.
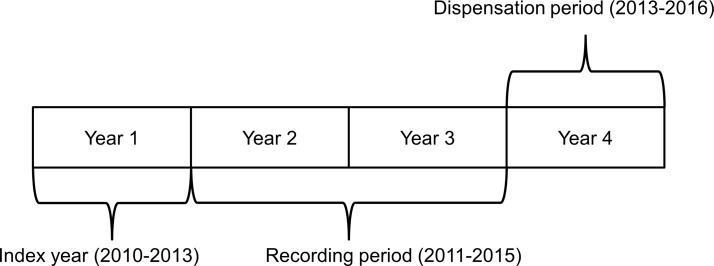
Medication adherence and dispensation
The outcome of the study was medication dispensation. Data on dispensation of medications in the entire patient cohort was extracted as a marker of adherence. Patients were considered adherent if they had at least two filled prescriptions in the third year following their index event, henceforth referred to as dispensation period (see figure 2). In Sweden, every filled prescription for chronic conditions will last for 3 months and thus two dispensations in 1 year will last for 180 days. We chose two and not one dispensation as two dispensations more strongly implies use of the medication. The third year following their index year was chosen because in many cases the hospital will be in charge of prescriptions for the first period following the index event. However, these prescriptions will last for up to a maximum of 1 year and if the prescribed therapy is to continue it is up to the primary care physician to take over prescriptions. Also, the third year was chosen to make certain that there was no overlap between the outcome and the exposure.
Figure 2.
Illustration of index year, recording period and dispensation period.
Recommended medications in ischaemic stroke and TIA include antihypertensives and statins.14 Antiplatelet agents are recommended in non-embolic stroke/TIA, while anticoagulants are recommended in embolic stroke/TIA.14 For haemorrhagic stroke, antihypertensives are recommended.16 In patients with acute coronary syndromes without persistent ST-segment elevation, guidelines recommend statins, antiplatelet agents and that patients are kept normotensive.15 Additionally, regional guidelines in Stockholm19 20 have recommended beta-blockers to all patients discharged from hospitals with acute coronary syndrome during the entire time period of our study.
Medications were divided into four groups: antithrombotics (antiplatelet agents and anticoagulants including new oral anticoagulants), antihypertensives, statins and beta-blockers. Medications studied for TIA, ischaemic stroke and acute coronary syndrome were antihypertensives, antithrombotics and statins. Additionally, in acute coronary syndrome beta-blockers were studied. For haemorrhagic stroke only data on dispensation of antihypertensives were collected. The specific ATC-codes used can be seen in the supplementary table S5. Medication dispensation was compared between recorded and not recorded patients during all recording periods (2011–2016).
Potential confounders
Sex, age, index year and visits to private specialists were identified as potential confounders. There may be differences between men and women both when it comes to the exposure, likelihood of recording a diagnosis in primary care and the outcome, likelihood of receiving certain medications.10 Age is also a factor that may be associated with both the exposure and the outcome. Elderly patients have greater comorbidity and it may be argued that this increases the number of diagnoses from which the primary care physician can choose. Also, this comorbidity implies that patients may have an indication for several different medications potentially influencing prescription behaviour. Index year may influence the results should diagnosis-recording behaviour and/or medication prescription patterns change over time.
Lastly, as private specialists linked to the National tariff system often serve as a substitute to primary care physicians, their patients are less likely to receive a primary care diagnosis. In addition, these visits affect the outcome as private specialists also prescribe medications. Supplementary table S6 shows descriptive statistics for age and for visits to private specialists.
Statistical analysis
Standard descriptive statistics were used and data are presented as proportions. Logistic regression was used in the analyses to calculate adjusted ORs with 95% CIs for drug dispensation for recorded versus not recorded patients (reference group). Adjustments were made for age (age categories <51, 51–65, 66–75, and >75 years), sex, index year and for healthcare consumption in the form of visits to private specialists that may function as a substitute to some patients’ primary care provider. The patients in our dataset are grouped within different primary healthcare centres. This implies a risk that the data are cluster-correlated and that the estimated standard errors are not independent. In order to account for this, without adjusting for the provider effect, which could be a mediator in the casual pathway, we have based standard errors on the ‘sandwich’ variance estimator. All statistical analyses were performed using SAS software, V.9.4 (SAS Institute, Cary, North Carolina, USA).
Results
Table 1 shows the absolute number and proportion of men and women with a recorded diagnosis in primary care, by diagnosis. The lowest proportion of recorded patients in primary care was found in the group of patients with TIA, whereas patients with acute coronary syndromes had the highest rate of recording. In all studied diagnoses, except for TIA, a lower percentage of women were recorded compared with men.
Table 1.
Absolute number and proportion of men and women with and without a recorded diagnosis in primary care, by diagnosis
| Recorded | Not recorded | |||
| Women | Men | Women | Men | |
| Transient ischaemic attack | 347 (16%) | 308 (15%) | 1813 (84%) | 1746 (85%) |
| Ischaemic stroke | 1189 (41%) | 1579 (46%) | 1683 (59%) | 1844 (54%) |
| Haemorrhagic stroke | 105 (35%) | 177 (43%) | 193 (65%) | 237 (57%) |
| Acute coronary syndrome | 1076 (44%) | 2580 (47%) | 1343 (56%) | 2852 (53%) |
Table 2 shows medication dispensation for recorded and not recorded patients for all diagnosis groups in both men and women. Patients with a recorded diagnosis were more likely to be dispensed two prescriptions of statins, antithrombotics and beta-blockers in the dispensation period across all studied diagnoses. The difference remained after adjusting for age, sex, index year and visits to private specialists (see table 3 and supplementary table S7 where results are stratified by sex).
Table 2.
Absolute number and proportion of men and women dispensed two prescriptions in the dispensation period, by medication class, recorded/not recorded status and diagnosis
| Statins | Antithrombotics | Antihypertensives | Beta-blockers | |||
| Transient ischaemic attack | Women | Not recorded | 827 (46%) | 1442 (80%) | 1271 (70%) | |
| Recorded | 195 (56%) | 313 (90%) | 221 (64%) | |||
| Men | Not recorded | 992 (57%) | 1451 (83%) | 1222 (70%) | ||
| Recorded | 210 (68%) | 283 (92%) | 211 (69%) | |||
| Ischaemic stroke | Women | Not recorded | 838 (50%) | 1401 (83%) | 1276 (76%) | |
| Recorded | 736 (62%) | 1074 (90%) | 893 (75%) | |||
| Men | Not recorded | 1122 (61%) | 1591 (86%) | 1373 (74%) | ||
| Recorded | 1106 (70%) | 1441 (91%) | 1212 (77%) | |||
| Haemorrhagic stroke | Women | Not recorded | 120 (62%) | |||
| Recorded | 72 (69%) | |||||
| Men | Not recorded | 147 (62%) | ||||
| Recorded | 149 (84%) | |||||
| Acute coronary syndrome | Women | Not recorded | 799 (59%) | 1136 (85%) | 1210 (90%) | 1015 (76%) |
| Recorded | 767 (71%) | 1008 (94%) | 1022 (95%) | 896 (83%) | ||
| Men | Not recorded | 2187 (77%) | 2561 (90%) | 2580 (90%) | 2208 (77%) | |
| Recorded | 2143 (83%) | 2414 (94%) | 2423 (94%) | 2149 (83%) |
Table 3.
Crude and adjusted ORs for being dispensed two prescriptions in the dispensation period according to recorded/not recorded status, by diagnosis
| Crude ORs (95% CIs) | Adjusted ORs* (95% CIs) | |
| Transient ischaemic attack | ||
| Statins | 1.55 (1.31 to 1.84) | 1.53 (1.28 to 1.82) |
| Antithrombotics | 2.33 (1.76 to 3.08) | 2.33 (1.74 to 3.11) |
| Antihypertensives | 0.83 (0.69 to 0.99) | 0.80 (0.66 to 0.96) |
| Ischaemic stroke | ||
| Statins | 1.59 (1.43 to 1.76) | 1.58 (1.42 to 1.76) |
| Antithrombotics | 1.78 (1.52 to 2.08) | 1.92 (1.63 to 2.27) |
| Antihypertensives | 1.05 (0.94 to 1.18) | 1.16 (1.03 to 1.31) |
| Haemorrhagic stroke | ||
| Antihypertensives | 2.21 (1.57 to 3.12) | 2.54 (1.72 to 3.76) |
| Acute coronary syndrome | ||
| Statins | 1.58 (1.42 to 1.75) | 1.64 (1.47 to 1.83) |
| Antithrombotics | 1.97 (1.68 to 2.32) | 2.02 (1.72 to 2.38) |
| Antihypertensives | 1.74 (1.47 to 2.07) | 1.76 (1.48 to 2.10) |
| Beta-blockers | 1.50 (1.34 to 1.68) | 1.48 (1.32 to 1.66) |
Not recorded patients are the reference group. OR >1 mean recorded patients are more likely to have two dispensations in the dispensation period.
*Adjustments made for age, sex, index year and visits to private specialists. To adjust for clustering, SEs are based on the ‘sandwich’ variance estimator.
For antihypertensives, the adjusted results show that recorded patients with stroke and acute coronary syndrome were more likely to be dispensed two prescriptions. However, recorded patients with TIA were less likely to be dispensed antihypertensives than the not recorded group.
Accounting for clustering with the ‘sandwich’ variance estimator only marginally affected the CIs, which implies that the data are not clustered to a high extent.
Discussion
Key results
Recording a diagnosis was associated with higher utilisation of recommended medications for all studied diagnosis groups, except for antihypertensives in patients with TIA. The rate of diagnosis recording spanned from 15% to 47% and was especially low in TIA (men 15%, women 16% recorded).
Potential explanations
Several factors could explain the association between recording a diagnosis and dispensation of recommended medications. Previous studies have shown that the transfer of information, when patients move between different parts of the healthcare system, frequently is insufficient and that this lack of communication may affect subsequent patient care. Discharge summaries from hospitals may be lacking or may not reach the responsible primary care physician leading to an inadequate transfer of information.7 8
There are several different electronic medical record systems used by primary care centres in Stockholm County. Some of them share systems with the hospitals enabling electronic transfer of information within the system. In these cases, the primary care physician often has electronic access to detailed information on a patient’s medical history including discharge medication. Theoretically, this access could facilitate prescription, thus influencing dispensation. Other centres need to rely on old fashion mailing of patient information and referral notes. However, even those caregivers who share the same electronic medical record system are not automatically able to read another caregiver’s information as informed consent from the patient is needed if a referral note has not been sent. Our registries do not allow us to know which centres use which electronic medical record systems. Thus, we have not been able to determine if use of certain systems increases or decreases the likelihood of recording of a diagnosis. This could be a confounding factor.
When a patient chooses to relist from one primary healthcare provider to another, there may also be a risk of patient data not being transferred which could affect knowledge of patients’ medical history and reduce the likelihood of both recording a diagnosis and prescription.
Knowledge of the condition in question including awareness of current guidelines is another factor that could influence both choice of diagnosis and dispensation. The level of knowledge may affect the likelihood of the physician focusing on the condition during visits and in continuation recording the diagnosis as well as the likelihood of prescribing medications according to guidelines and motivating the patient to continue using the preventive medications.
There may also be important differences in patient factors between the recorded and not recorded groups, which may lead to both a higher level of recorded diagnoses and increased dispensation in the recorded group. It is possible that patients who have a recorded diagnosis are more knowledgeable about their diagnoses and more assertive in their communication towards physicians, which may lead to an increased level of physician prescribing. As this is a registry study, it is difficult to ascertain whether this is the case.
In contrast to the overall pattern, patients with a recorded diagnosis of TIA were dispensed less antihypertensives than those with no recorded diagnosis. A potential explanation for the varying associations between dispensation of antihypertensive therapy and recording of the different diagnoses could stem from the fact that treatment of hypertension is well established. As many patients with stroke/TIA and/or ischaemic heart disease have established hypertension,21 22 they would be treated regardless of other diagnoses. This is not the case for antithrombotics and statins. Hypertension is also a common condition with a high prevalence of treatment and this diagnosis may be chosen instead of a diagnosis of cardiovascular/cerebrovascular disease. However, it should be noted that the proportion of patients with recorded TIA is small and the data concerning this group should be interpreted with caution.
The strikingly low rate of recording of a diagnosis in TIA may partially be explained by the lack of remaining objective symptoms. Primary care physicians caring for a patient with chronic symptoms from a stroke will be reminded of the patient’s previous disease and this may influence the likelihood of recording a stroke diagnosis. The same reminder is not provided when physicians see patients with a previous TIA in which case the diagnosis might not be recorded. However, the low rate of recording in TIA needs further research as the causes are, is in all likelihood, multifactorial. Patients with acute coronary syndrome also lack symptoms at follow-up in many cases, and still those patients are recorded to a high degree.
Policy implications
The results show that recording a diagnosis is associated with higher utilisation of recommended medications. Diagnosis recording is potentially an indicator of physician adherence to recommended treatment and a marker of an intact chain of care from hospital to primary care. What does this mean for clinical practice? Could recording of a diagnosis be used as a quality indicator? Previously published requirements for quality indicators are acceptability, feasibility, reliability, sensitivity to change and validity.23 Future research needs to confirm that these requirements are met for ‘recording a diagnosis’ before its utility as a quality indicator can be considered. Information about degree of recording of diagnosis at each primary healthcare centre could also be useful from the healthcare centre’s perspective as it provides information about their patient population, which could be used to improve the provided care.
Strengths and limitations
A strength of the study is the use of registry data, which has allowed for an unbiased inclusion of a large number of patients based on all residents in Stockholm County and not just a sample. Using hospital registries is fraught with the risk of misdiagnosing, which could lead to potential inclusion errors. However, in the case of our chosen diagnoses, there are quality registries24–27 where 84%–90% of hospital discharge diagnoses are registered. Diagnoses are generally better verified when reported to quality registries. Thus, if a high proportion of discharge diagnoses are captured by the registries, it is an indication of the high validity of the discharge diagnosing in stroke and ischaemic heart disease in hospital. For TIA, there may be greater uncertainty and variation in accuracy of diagnosing due to the diagnosis-defining lack of objective symptoms. Furthermore, we only included patients where there was an initial hospital diagnosis recorded since the focus of our study was communication between hospitals and primary care. However, it should be noted that in some cases a cardiovascular event may only be recorded in primary care and not in hospital.28 29 This means that we will not have included all patients with a stroke/TIA or acute coronary syndrome in the population during the study period.
There are different definitions of medication adherence. We have defined medication adherence as two dispensations in 1 year. However, our results may have been different if we had chosen another definition of medication adherence.
The absolute clinical benefits of our results are difficult to approximate in the present study, since we have only studied dispensation of recommended secondary preventive medication and not actual clinical outcomes. Improved adherence to recommendations may be seen as a surrogate marker for clinical benefit since the clinical benefits of good adherence to medical therapy in cardiovascular conditions has been shown in multiple studies.30–36 Further study is needed to determine if recording of diagnosis is associated with any improvements in patient outcomes such as mortality, recurrence of disease, etc.
Generalisability
The generalisability of the results depends on the definition of the study population, the included diagnoses and the organisation of the healthcare system. In the present study, the aim was to investigate the association between recording a diagnosis and recommended treatment and it was necessary to include only diagnoses with clear recommendations regarding medical treatment. The initial choice of ICD codes in the index year, where unspecific diagnoses (eg, I64.9—stroke, not specified as haemorrhage or infarction) were not included, allowed a selection of patients with diagnoses for which secondary preventive pharmacological treatment was indicated.
In order to use recording of a diagnosis in a diverse primary care population with a wide range of diagnoses, many of which are recorded in primary care only, the model used for recording of diagnosis would have to be altered and further studied. The generalisability is also limited to the record system and possible incentive structures used to stimulate recording of diagnoses as well as recall systems, the use of chronic diagnoses and such factors. Different healthcare systems are organised differently. In systems where the diagnosis dictates which medications are subsidised, recording of a diagnosis may have a different impact and would need to be interpreted in light of this. If recording of a diagnosis were to be used as a quality indicator, it would need to be used with caution and adapted to the healthcare system in question.
Conclusion
The results show that a physician recording a diagnosis in primary care seems beneficial for patient utilisation of recommended medications in TIA, stroke and acute coronary syndrome. Patients who are diagnosed with their hospital diagnosis in primary care receive recommended treatment to a higher extent than patients without such a diagnosis in primary care. Further study is necessary in order to determine if ‘recording a diagnosis’ may be used as a quality indicator.
Supplementary Material
Footnotes
Contributors: CD: contributed to the study design, researched data, contributed to analysis and interpretation of data and drafted the manuscript. LG: contributed to the study design, researched the literature, contributed to analysis and interpretation of data and drafted the manuscript. CR, KS-G and PW: contributed to the study design, contributed to analysis and interpretation of data and critically revised the manuscript. JH and MvE: came up with the original idea, contributed to the study design, contributed to analysis and interpretation of data and critically revised the manuscript. All authors approved the final manuscript.
Funding: Supported by grants provided by the Stockholm County Council (ALF project) and by the Stockholm Drug and Therapeutics Committee. Funding was provided as unrestricted grants. The funding bodies did not influence the work, the analyses or the interpretations, all which are the full responsibility of the authors.
Competing interests: None declared.
Ethics approval: The study was approved by the regional ethics review board in Stockholm, Dnr 2015/803-31/5 and Dnr 2016/1547-32.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Additional aggregate level data can be made available by emailing cecilia.dahlgren@ki.se.
References
- 1. Swedish Government Official Reports. Effective Health Care: final report (SOU 2016:2 Effektiv vård : slutbetänkande). Stockholm, Sweden: Wolters Kluwer, 2016. [Google Scholar]
- 2. Enthoven AC. Integrated delivery systems: the cure for fragmentation. Am J Manag Care 2009;15:S284–90. [PubMed] [Google Scholar]
- 3. Hofmarcher MM, Oxley H, Rusticelli E. ‘Improved Health System Performance through better Care Coordination’, OECD Health Working Papers 2007, No. 30, OECD Publishing. 10.1787/246446201766 [DOI]
- 4. Masseria CIR, Thomson S, Gemmill M, et al. . Primary care in Europe - policy brief. Secondary European commission. Primary care in Europe - policy brief. 2009. http://ec.europa.eu/social/keyDocuments.jsp?advSearchKey=primary+care+in+europe+masseria&mode=advancedSubmit&langId=en&policyArea=&type=0&country=0&year=2009
- 5. Stange KC. The problem of fragmentation and the need for integrative solutions. Ann Fam Med 2009;7:100–3. 10.1370/afm.971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vázquez ML, Vargas I, Unger JP, et al. . Evaluating the effectiveness of care integration strategies in different healthcare systems in Latin America: the EQUITY-LA II quasi-experimental study protocol. BMJ Open 2015;5:e007037 10.1136/bmjopen-2014-007037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kattel S, Manning DM, Erwin PJ, et al. . Information transfer at hospital discharge: a systematic review. J Patient Saf 2016. 10.1097/PTS.0000000000000248 [DOI] [PubMed] [Google Scholar]
- 8. Kripalani S, LeFevre F, Phillips CO, et al. . Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA 2007;297:831–41. 10.1001/jama.297.8.831 [DOI] [PubMed] [Google Scholar]
- 9. Carlsson AC, Wändell P, Ösby U, et al. . High prevalence of diagnosis of diabetes, depression, anxiety, hypertension, asthma and COPD in the total population of Stockholm, Sweden - a challenge for public health. BMC Public Health 2013;13:670 10.1186/1471-2458-13-670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Glader EL, Sjölander M, Eriksson M, et al. . Persistent use of secondary preventive drugs declines rapidly during the first 2 years after stroke. Stroke 2010;41:397–401. 10.1161/STROKEAHA.109.566950 [DOI] [PubMed] [Google Scholar]
- 11. Sjölander M, Eriksson M, Glader EL. Few sex differences in the use of drugs for secondary prevention after stroke: a nationwide observational study. Pharmacoepidemiol Drug Saf 2012;21:911–9. 10.1002/pds.2268 [DOI] [PubMed] [Google Scholar]
- 12. Chen HY, Saczynski JS, Lapane KL, et al. . Adherence to evidence-based secondary prevention pharmacotherapy in patients after an acute coronary syndrome: A systematic review. Heart Lung 2015;44:299–308. 10.1016/j.hrtlng.2015.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hirsh BJ, Smilowitz NR, Rosenson RS, et al. . Utilization of and Adherence to Guideline-Recommended Lipid-Lowering Therapy After Acute Coronary Syndrome: Opportunities for Improvement. J Am Coll Cardiol 2015;66:184–92. 10.1016/j.jacc.2015.05.030 [DOI] [PubMed] [Google Scholar]
- 14. European Stroke Organisation (ESO) Executive Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 2008;25:457–507. 10.1159/000131083 [DOI] [PubMed] [Google Scholar]
- 15. Roffi M, Patrono C, Collet JP, et al. . 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016. 37:267–315. 10.1093/eurheartj/ehv320 [DOI] [PubMed] [Google Scholar]
- 16. Steiner T, Al-Shahi Salman R, Beer R, et al. . European Stroke Organisation (ESO) guidelines for the management of spontaneous intracerebral hemorrhage. Int J Stroke 2014;9:840–55. 10.1111/ijs.12309 [DOI] [PubMed] [Google Scholar]
- 17. Dahlgren C, Brorsson H, Svereus S, et al. . Fem år med husläkarsystemet inom Vårdval Stockholm [Five years with choice in primary care in Stockholm]. Stockholm: Karolinska institutet; 2013. [Google Scholar]
- 18. Forslund T, Wettermark B, Hjemdahl P. Comparison of treatment persistence with different oral anticoagulants in patients with atrial fibrillation. Eur J Clin Pharmacol 2016;72:329–38. 10.1007/s00228-015-1983-z [DOI] [PubMed] [Google Scholar]
- 19. Gustafsson LL, Wettermark B, Godman B, et al. . The ‘wise list’- a comprehensive concept to select, communicate and achieve adherence to recommendations of essential drugs in ambulatory care in Stockholm. Basic Clin Pharmacol Toxicol 2011;108:224–33. 10.1111/j.1742-7843.2011.00682.x [DOI] [PubMed] [Google Scholar]
- 20. Acute Cardiac Care in Stockholm County (Akut Hjärtsjukvård i SLL). 2009 and 2012, ed. [Google Scholar]
- 21. O’Donnell MJ, Xavier D, Liu L, et al. . Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 2010;376:112–23. 10.1016/S0140-6736(10)60834-3 [DOI] [PubMed] [Google Scholar]
- 22. Yusuf S, Hawken S, Ôunpuu S, et al. . Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. The Lancet 2004;364:937–52. 10.1016/S0140-6736(04)17018-9 [DOI] [PubMed] [Google Scholar]
- 23. Campbell SM, Braspenning J, Hutchinson A, et al. . Research methods used in developing and applying quality indicators in primary care. BMJ 2003;326:816–9. 10.1136/bmj.326.7393.816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Asplund K, Hulter Åsberg K, Appelros P, et al. . The Riks-Stroke story: building a sustainable national register for quality assessment of stroke care. Int J Stroke 2011;6:99–108. 10.1111/j.1747-4949.2010.00557.x [DOI] [PubMed] [Google Scholar]
- 25. Riks-Stroke C. Riksstroke Annual Report (Riksstrokes årsrapport 2014). 2014.
- 26. Swedish National Board of Health and Welfare. Completeness of registries. Stockholm, Sweden, 2015(Täckningsgrader 2015: jämförelser mellan nationella kvalitetsregister och hälsodataregistren. Stockholm:Socialstyrelsen; 2015). [Google Scholar]
- 27. Jernberg T, Attebring MF, Hambraeus K, et al. . The Swedish Web-system for enhancement and development of evidence-based care in heart disease evaluated according to recommended therapies (SWEDEHEART). Heart 2010;96:1617–21. 10.1136/hrt.2010.198804 [DOI] [PubMed] [Google Scholar]
- 28. Herrett E, Shah AD, Boggon R, et al. . Completeness and diagnostic validity of recording acute myocardial infarction events in primary care, hospital care, disease registry, and national mortality records: cohort study. BMJ 2013;346:f2350 10.1136/bmj.f2350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Payne RA, Abel GA, Simpson CR. A retrospective cohort study assessing patient characteristics and the incidence of cardiovascular disease using linked routine primary and secondary care data. BMJ Open 2012;2:e000723 10.1136/bmjopen-2011-000723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Burke JP, Sander S, Shah H, et al. . Impact of persistence with antiplatelet therapy on recurrent ischemic stroke and predictors of nonpersistence among ischemic stroke survivors. Curr Med Res Opin 2010;26:1023–30. 10.1185/03007991003670563 [DOI] [PubMed] [Google Scholar]
- 31. Chen PS, Cheng CL, Kao Yang YH, et al. . Statin Adherence After Ischemic Stroke or Transient Ischemic Attack Is Associated With Clinical Outcome. Circ J 2016;80:731–7. 10.1253/circj.CJ-15-0753 [DOI] [PubMed] [Google Scholar]
- 32. Chowdhury R, Khan H, Heydon E, et al. . Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J 2013;34:2940–8. 10.1093/eurheartj/eht295 [DOI] [PubMed] [Google Scholar]
- 33. Colivicchi F, Bassi A, Santini M, et al. . Discontinuation of statin therapy and clinical outcome after ischemic stroke. Stroke 2007;38:2652–7. 10.1161/STROKEAHA.107.487017 [DOI] [PubMed] [Google Scholar]
- 34. Ho PM, Spertus JA, Masoudi FA, et al. . Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med 2006;166:1842–7. 10.1001/archinte.166.17.1842 [DOI] [PubMed] [Google Scholar]
- 35. Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA 2007;297:177–86. 10.1001/jama.297.2.177 [DOI] [PubMed] [Google Scholar]
- 36. Wei L, Wang J, Thompson P, et al. . Adherence to statin treatment and readmission of patients after myocardial infarction: a six year follow up study. Heart 2002;88:229–33. 10.1136/heart.88.3.229 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-015723supp001.pdf (498.4KB, pdf)