Abstract
We report a case of a tubo-ovarian abscess infected with Salmonella enterica serotype typhi. A 19-year-old Nepalese woman presented to a hospital in Kathmandu with lower abdominal pain, constipation, fever and a non-healing, suppurative surgical wound from an emergency caesarian section performed 2 months previously at 37 weeks of pregnancy. She also had an exploratory laparotomy for an appendix perforation with peritonitis at 25 weeks of gestation. Her wound infection did not respond to cloxacillin and she had an exploratory laparotomy, and a tubo-ovarian abscess was found from which S. typhi was isolated. She had a bilateral salpingo-oophorectomy and responded to 14 days of chloramphenicol. A tubo-ovarian abscess is a rare complication of enteric fever.
Keywords: tropical medicine (infectious disease), obstetrics, gynaecology and fertility, infectious diseases
Background
Salmonella enterica serovar typhi (S. typhi) is a leading cause of illness in Nepal.1 A tubo-ovarian abscess caused by S. typhi is a rare complication with only two patients reported in the literature.2 3 Here we describe a case of tubo-ovarian abscess caused by S. typhi in Nepal.
Case presentation
A 19-year-old woman presented in January 2017 to Patan Hospital in Kathmandu, Nepal, with abdominal pain localised around the site of a recent incision for a caesarian section. She had a prior history of an exploratory laparotomy for perforated appendicitis and peritonitis at 25 weeks of pregnancy. At operation, 100 mL of pus was aspirated from the bilateral paracolic gutters. At 37 weeks of pregnancy, an emergency caesarean section was performed because of meconium-stained liquor. The baby was born healthy. She was discharged on the fourth day postcaesarean. Suture removal was performed a week later when cloxacillin was prescribed for 7 days because of serous discharge from the wound. A wound culture showed no bacterial growth. She was then well until 2 months later when she presented with abdominal pain.
On examination, her temperature was 100oF, pulse 98 bpm and blood pressure 90/60 mm Hg. Her surgical incision site was red, indurated, with fluctuating tenderness. Ten millilitres of pus was aspirated but had no bacterial growth after 48 hours. Ultrasonography revealed cystic collection posterior to the uterus. Cloxacillin was started at 500 mg four times daily. Further wound debridement with culdocentesis was performed on day 20 of admission and 150 mL of pus was drained. S. typhi was cultured from this pus but, because she showed no signs of fever, the cloxacillin was continued for 2 weeks and she was discharged.
She returned to hospital 6 days later having become unwell with fever, pain in the right lower quadrant, nausea, vomiting and constipation. She appeared toxic, with a temperature of 101.2oF, with a 5 cm gap in the abdominal wound, associated with minimal discharge and tenderness. Per-vaginal examination revealed a bulky tender uterus with decreased mobility.
Investigations
An ultrasonography showed a 10×10 cm2 mass in the Pouch of Douglas (figure 1).
Figure 1.

Ultrasound sonography test abdomen pelvis showing cystic area in Pouch of Douglas.
An exploratory laparotomy was performed which revealed dense adhesions in the rectus sheath, subcutaneous tissue, muscle, omentum and uterus. The left ovary was adherent to the Pouch of Douglas and rectum posteriorly with additional inflammation of the right tube and ovary. Approximately 40 mL of pus was drained from a left ovarian abscess and bilateral salpingo-oophorectomy was carried out (figure 2).
Figure 2.
Histopathology sample of left tubo-ovarian mass excised.
S.%20typhi was cultured from the pus (figure 3). By disc sensitivity testing, the isolate was susceptible to chloramphenicol, amoxicillin, trimethoprim-sulfamethoxazole, ceftriaxone and azithromycin but resistant to ciprofloxacin and gatifloxacin.
Figure 3.

Salmonella typhi growth on MacConkey sheep blood agar.
Treatment
The patient had already been on antibiotics for a long period of time. Keeping in mind the uprising resistance to ceftriaxone, chloramphenicol at 500 mg four times a day was started.
Outcome and follow-up
The fever subsided within 48 hours and the chloramphenicol was continued for 14 days (figure 4). She was reviewed at 1-month follow-up when she was improving and her child was healthy.
Figure 4.
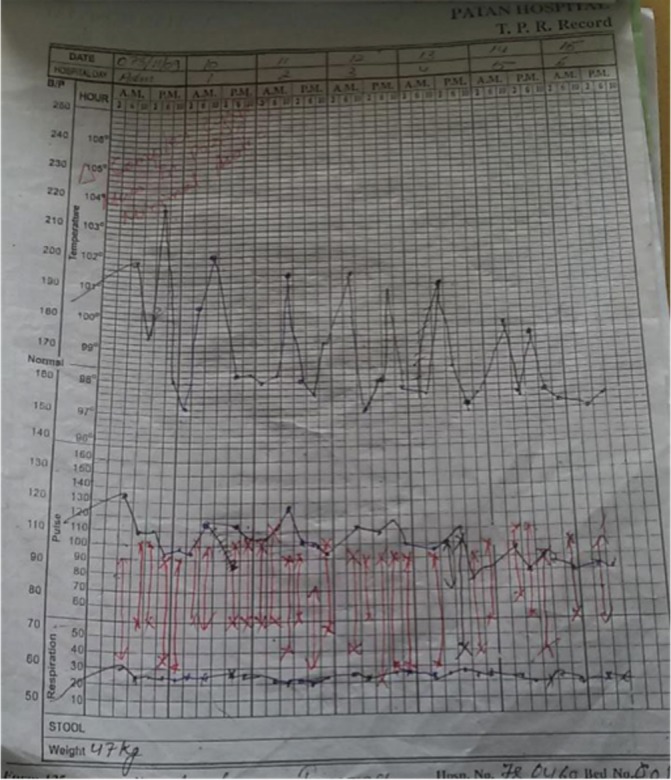
Fever charting showing decline in fever after chloramphenicol administration.
Discussion
A tubo-ovarian abscess is an inflammatory mass that presents as a late complication of pelvic inflammatory disease, infected intrauterine devices, acute appendicitis, diverticulitis or any abdominal surgery. Predisposing factors include diabetes mellitus, immunodeficiency and pregnancy. The route of transmission is commonly through an ascending infection from the cervix or haematogenous/lymphatic spread. Isolation of S. typhi from tubo-ovarian abscess has been rarely reported.
The route of infection for this S. typhi tubo-ovarian abscess is unclear. It is possible that she was a chronic carrier of typhoid and this colonisation led to the complication. Alternatively, she might have had a recent exposure to typhoid.
The isolation of S. typhi from the abdominal wound pus was unexpected and because of the lack of fever the significance was uncertain. The surgical wound infection initially responded to cloxacillin and the typhi was not specifically treated. However, she might have been in an incubation period when she did not have fever. In fact, the isolation of S. typhi should never be considered as non-pathogenic and she would have benefited with chloramphenicol treatment at that time.
In recent years, there has been an increase in resistance in S. typhi in Nepal to the fluoroquinolones,4 which have been considered the first-line antimicrobial choice. This has been accompanied by higher levels of susceptibility to chloramphenicol, amoxicillin, cotrimoxazole and azithromycin.5 Ceftriaxone is also effective, especially when parenteral treatment needs to be given.
S. typhi isolated from a tubo-ovarian abscess has only been reported previously in Malta and India.3 4 6 Non-typhoidal salmonellae (NTS) have been isolated from a tubo-ovarian abscess in Japan (2013) with Salmonella O77; in Turkey (2013) in a patient with systemic lupus erythematosus complicated with NTS8; in Slovenia (2010) with S. stanleyville9; in Malaysia (2007) with S. enteritidis10; and in Spain (2007) with S. manhattan.11
Typhoidal Salmonella has been occasionally isolated from other unusual sites12 such as a pleural empyema and chest wall cavity,13 14 a lung hydatid cyst,15 a Brodie's ulna abscess,16 splenic abscess,17–19 parotid abscess,20 21 testicular abscess,22 breast abscess,23 24 spondylodiscitis25 and even the myocardium.6 26 The development of such extraintestinal infections probably depends on the ingested inoculum size, the virulence of the strain, the host’s immune response and previous exposure, and local protective factors.27
Learning points.
Salmonella typhi infection should be considered in the differential diagnosis in patients who develop deep abscesses in a typhoid fever endemic region.
Pelvic mass may present as infected abscess in tubo-ovarian region in postsurgical patients.
Exploratory laparotomy is a treatment to be considered for patients with ovarian mass complicated with non-healing surgical wound.
Footnotes
Contributors: All the authors have contributed to the making of this case report. PS, BB and AB conceptualised the report. AB and RT collected informed consent and detailed information from the patient and the related medical staff. BB, AB, RT and PS edited the report into the final presentable manuscript. All the authors were involved in patient care, helped write the manuscript and approved the final version.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Karkey A, Aryjal A, Basnyat B, et al. Kathmandu, Nepal: still an enteric fever capital of the world. J Infect Dev Ctries 2008;2:461–5. [DOI] [PubMed] [Google Scholar]
- 2.Selvam EM, Sridevi TA, Menon M, et al. A case of salmonella enterica serovar typhi tubo ovarian abscess. J Obstet Gynaecol India 2015;65:278–80. 10.1007/s13224-014-0566-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vasallo L, Attard R. Tuboovarian abscess as a complication of typhoid fever, 1968. [Google Scholar]
- 4.Thompson CN, Karkey A, Dongol S, et al. Treatment response in enteric fever in an era of increasing antimicrobial resistance: an individual patient data analysis of 2092 participants enrolled into 4 randomised controlled trials in Nepal. Clinical Infect Dis 2017;64:1522–31. 10.1093/cid/cix185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta V, Kaur J, Kaistha N. Re-emerging chloramphenicol sensitivity and emerging low level ciprofloxacin resistance among Salmonella enterica serotype typhi isolates in North India. Trop Doct 2009;39:28–30. 10.1258/td.2008.070452 [DOI] [PubMed] [Google Scholar]
- 6.Childs L, Gupta S. Salmonella enteritidis induced myocarditis in a 16-year-old girl. BMJ Case Rep [Internet] 2012. http://casereports.bmj.com/content/2012/bcr-2012-007628.full.pdf+html?sid=f888be2e-4850-408f-8111-9511338378a3%5Cnhttp://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed10b&AN=2013028990%5Cnhttp://wa4py6yj8t.search.serialssolutions.com/?url_ve [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tohya T, Yoshimura T, Onoda C. Unilateral ovarian abscess caused by salmonella. Infect Dis Obstet Gynecol 2003;11:217–9. 10.1080/10647440300025524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guler S, Oksuz H, Cetin GY, et al. Bilateral tubo ovarian abscess and sepsis caused by Salmonella in patients with SLE. BMJ Case Rep 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gorisek NM, Oresković S, But I. Salmonella ovarian abscess in young girl presented as acute abdomen--case report. Coll Antropol 2011;35:223–5. [PubMed] [Google Scholar]
- 10.Thaneemalai J, Asma H, Savithri DP. Salmonella tuboovarian abscess. Med J Malaysia 2007;62:422–3. [PubMed] [Google Scholar]
- 11.Alonso D, Muñoz J, Ruiz J, et al. Salmonella ovarian abscess following travel diarrhoea episode. Arch Gynecol Obstet 2007;276:551–3. 10.1007/s00404-007-0380-y [DOI] [PubMed] [Google Scholar]
- 12.Sudhaharan S, Padmaja K, Solanki R. Extra-intestinal salmonellosis in a tertiary care center in South India. J Infect Dev Ctries 2014;8:831–7. [DOI] [PubMed] [Google Scholar]
- 13.Afridi FI, Farooqi BJ, Hussain A. Pleural Empyema Due to Salmonella typhi. Physicians and Surgeons Pakistan 2012;22:803–80. [PubMed] [Google Scholar]
- 14.Tonziello G, Valentinotti R, Arbore E, et al. Salmonella typhimurium abscess of the chest wall. Am J Case Rep 2013;14:502–6. 10.12659/AJCR.889546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aslam F, Bhaila I, Nadeem N, et al. Salmonella typhi-infected lung hydatid cyst. Pediatr Infect Dis J 2005;24:270–2. 10.1097/01.inf.0000154331.67419.78 [DOI] [PubMed] [Google Scholar]
- 16.Kc I, Lam YL, Chang RY. Brodie's abscess of the ulna caused by salmonella typhi. 2008;14:154–6. [PubMed] [Google Scholar]
- 17.Rodan BA, Max RJ, Breiman RS, et al. Splenic abscess due to salmonella typhimurium bacteremia. South Med J 1981;74:382–3. 10.1097/00007611-198103000-00043 [DOI] [PubMed] [Google Scholar]
- 18.Cabadak H, Erbay A, Karaman K, et al. Splenic abscess due to Salmonella enteritidis. Infect Dis Rep 2012;4:4–10. 10.4081/idr.2012.e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Comarmond C, Jauréguiberry S, Vaillant JC, et al. Giant splenic abscess due to Salmonella enteritidis in a returning traveler. J Travel Med 2010;17:271–3. 10.1111/j.1708-8305.2010.00407.x [DOI] [PubMed] [Google Scholar]
- 20.Moraitou E, Karydis I, Nikita D, et al. Case report: parotid abscess due to Salmonella enterica serovar enteritidis in an immuno competent adult. Int J Med Microbiol 2007;297:123–6. 10.1016/j.ijmm.2006.11.005 [DOI] [PubMed] [Google Scholar]
- 21.Shen CH, Lin YS, Chang FY. Gas-forming parotid abscess in a diabetic patient: an unusual complication of Salmonella enteritidis bacteremia. Am J Med Sci 2008;336:504–7. 10.1097/MAJ.0b013e3181626545 [DOI] [PubMed] [Google Scholar]
- 22.Al-Obeid K, Al Khalifan NN, Jamal W, et al. Epididymo-orchitis and testicular abscess caused by Salmonella enteritidis in immunocompromised patients in Kuwait. Med Princ Pract 2006;15:305–8. 10.1159/000092996 [DOI] [PubMed] [Google Scholar]
- 23.Sood S. Breast abscess by Salmonella paratyphi a: case report and literature review. J Clin Diagn Res 2015;9:DD03–DD04. 10.7860/JCDR/2015/15083.6539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Delori M, Abgueguen P, Chennebault J-M, et al. [Breast abscess with Salmonella typhi and review of the literature]. J Gynecol Obstet Biol Reprod (Paris) [Internet] 2007;36:709–12. [DOI] [PubMed] [Google Scholar]
- 25.Zebouh M, Loïez C, Marceau L, et al. [Spondylodiscitis due to Salmonella enteritica serotype Typhi]. Ann Biol Clin 2005;63:517–8. [PubMed] [Google Scholar]
- 26.Chakraborty PP, Bhattacharjee R, Bandyopadhyay D, et al. Diagnosis and treatment of scrub typhus--the Indian scenario. J Assoc Physicians India 2010;58:186–7. [PubMed] [Google Scholar]
- 27.Huang DB, DuPont HL. Problem pathogens: extra-intestinal complications of Salmonella enterica serotype Typhi infection. Lancet Infect Dis 2005;5:341–8. 10.1016/S1473-3099(05)70138-9 [DOI] [PubMed] [Google Scholar]



