Description
A 23-year-old woman with no premorbid illness presented with features of high-grade fever since 3 days. She developed progressively deteriorating sensorium, recurrent vomiting and multiple episodes of generalised tonic clonic seizures. On examination, funduscopy was normal. The patient was drowsy but arousable, disoriented to person or place. She had neck stiffness. Kernig's sign was positive. She did not localise the central (sternal) deep painful stimuli briskly with either hand although the definite paucity of any limb could not be made out. Considering the short clinical history with a triad of fever, altered sensorium and seizures and associated signs of meningeal irritation, clinical diagnosis of bacterial or viral meningoencephalitis was thought of. MRI brain showed bihemispherical multiple cortical–subcortical lacunar infarcts (figure 1). MRI contrast images did not show any significant meningeal enhancement. With the strong suspicion of meningoencephalitis, cerebrospinal fluid (CSF) analysis was done after the imaging of the brain. It showed very low sugars, normal proteins, over 300 cells with neutrophil predominance and low CSF/blood glucose index, suggestive of bacterial meningoencephalitis. The CSF culture confirmed pneumococcal growth. However, blood culture was sterile at 48 hours probably since intravenous ceftriaxone was initiated before the blood sample was collected. The patient improved with injectable vancomycin and ceftriaxone for 2 weeks, along with injectable dexamethasone which was tapered and stopped in 3 days.
Figure 1.
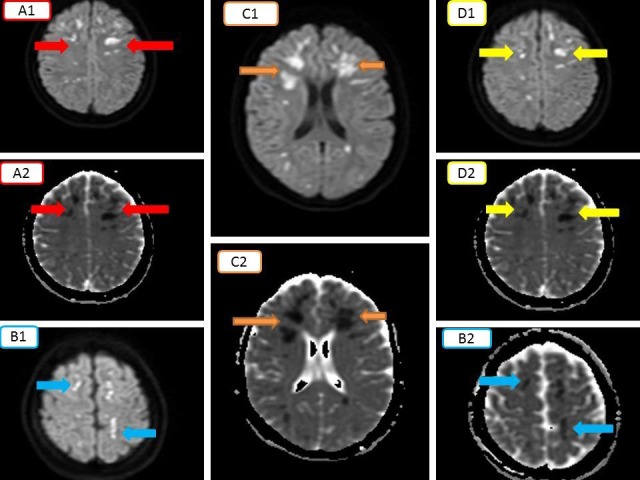
(Collage) DWI and corresponding ADC. Multiple areas of corresponding diffusion restriction suggestive of acute infarcts (A1–A2, B1–B2, C1–C2, D1–D2). ADC, apparent diffusion coefficient; DWI, diffusion-weighted images.
Pneumococcal infection is probably the most common bacterial meningitis associated with acute cerebrovascular accidents due to the inflammation induced through bacterial bloodstream invasion and activation of the complement and coagulation systems.1 Ischaemic cerebrovascular accident (CVA) is more common as compared with haemorrhagic. Elderly individuals are more commonly affected.2 It is a rarity to have a young 23-year-old woman manifest as described above. Also, other cases with cerebral vasculitis in pneumococcal meningitis have occurred late in course of admission or around discharge.3
Learning points.
Pneumococcal meningitis can often lead to vasculitis, causing cerebrovascular accidents, commonly in the form of infarcts and rarely intracerebral bleeds.
This commonly occurs in elderly population and very rarely in young adults.
Intravenous steroids in the cover of antibiotics, as per culture and sensitivity pattern are the treatment of choice.
Footnotes
Contributors: VK and SK: made substantial contributions to the conception and design of the work, acquisition, analysis and interpretation of the data. AD: involved in drafting the work and revising it critically for important intellectual content.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Mook-Kanamori BB, Geldhoff M, van der Poll T, et al. Pathogenesis and pathophysiology of pneumococcal meningitis. Clin Microbiol Rev 2011;24:557–91. 10.1128/CMR.00008-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bodilsen J, Dalager-Pedersen M, Schønheyder HC, et al. Stroke in community-acquired bacterial meningitis: a danish population-based study. Int J Infect Dis 2014;20:18–22. ISSN 1201-9712. 10.1016/j.ijid.2013.12.005 [DOI] [PubMed] [Google Scholar]
- 3. Klein M, Koedel U, Pfefferkorn T, et al. Arterial cerebrovascular complications in 94 adults with acute bacterial meningitis. Crit Care 2011;15:R281 10.1186/cc10565 [DOI] [PMC free article] [PubMed] [Google Scholar]


