Abstract
Purpose:
The aim of this study was to evaluate the relationship between initial probing depth (IPD) and changes in clinical parameters following non-surgical periodontal treatment (NPT) in chronic periodontitis patients.
Subjects and Methods:
A total of 1672 periodontal pockets having 3mm≤IPD≤9mm of depth in 15 chronic periodontitis patients were included. NPT consisting of oral hygiene instructions, scaling and root planing was applied in two sessions. Probing depth (PD), clinical attachment level, gingival recessions (GR) were measured before and eight weeks after treatment. Pocket sites were grouped according to their IPD and root number as single- or multi-rooted teeth.
Results:
Other than the sites having 3 mm IPD, PD reduction and GR increase were significant in all groups (p<0.001). Attachment gains (AG) were significant in all single-rooted teeth (p<0.001) again except those having IPD=3mm. However, AG was significant in multi-rooted teeth having only 7mm≤IPD≤9mm (p<0.05). Positive correlations were observed between IPD and PD reduction, GR increase and AG in single-rooted teeth (p<0.001). Furthermore, positive correlations were found between IPD and PD reduction and GR increase in multi-rooted teeth (p<0.001), but there was no correlation between IPD and AG.
Conclusion:
NPT may lead to positive association between IPD and PD reduction as well as GR increase, which is independent from tooth root anatomy.
Keywords: Chronic periodontitis, dental scaling, periodontal pocket, root planning, periodontology
Introduction
Periodontal diseases are bacterial related chronic inflammations which may lead to the destruction of tooth-supporting tissues and ultimately tooth loss (1). Periodontal breakdown occurs due to an association between colonized periodontal pathogens in microbial dental plaque and host response developed against to these microorganisms (2, 3). Chronic periodontitis (CP) is a periodontal disease that is seen in early adulthood and it is characterized by spontaneous or provoked gingival bleeding, oral malodor, migration and mobility of teeth, loss of attachment and alveolar bone (4). Changes in color, consistency and volume of gingivae, bleeding on probing, periodontal pocket formation, furcation involvement and tooth loss are some of the clinical features of chronic periodontitis. Alveolar bone loss can be observed in horizontal and vertical directions or in combination of these vectors.
The aim of non-surgical periodontal treatment (NPT) is the elimination of bacterial deposits adhered to tooth surfaces, primarily by means of dental plaque control performed by the patient, in addition to dental scaling and root surface debridement performed by the dentist (5, 6, 7). Additionally, occlusal adjustment and elimination of plaque retentive areas such as dental caries are important components of this treatment approach that aims to control the periodontal inflammation. Early stages of CP cases can be treated successfully by maintaining optimum oral hygiene and NPT (8). However, in moderate to advanced stages of CP cases, NPT provides firm gingival structure by the elimination of gingival inflammation, which is a prerequisite for surgical periodontal treatment (9). Reevaluation of periodontal tissue healing after NPT is crucial to predict the prognosis and to plan ahead for further periodontal treatment. However, conflicting arguments exist regarding the optimal time point to assess the healing of periodontal tissues following NPT (10, 11). This period should neither be too short to permit overtreatment of the patient nor be too long to cause a shift in the subgingival microbial flora incompatible with periodontal health status (12). The subgingival microbial flora gains pathogenic features within 4-8 weeks following NPT in cases with inadequate plaque control (13). Factors that influence healing following NPT are categorized as tooth/site, patient and dentist-related factors (14). While patient-related factors can be exampled as oral hygiene status, smoking habit, systemic diseases/conditions, host response, socioeconomic level of patient, dentist-related factors include knowledge and clinical experience, elimination of bacterial deposits sufficiently and existence of necessary instruments to perform NPT. Initial probing depths (IPD), periodontal inflammatory status of the sites and anatomical characteristics of tooth such as furcations, grooves, and root number are considered as tooth/site-related factors.
Systematic reviews and meta-analysis support the effect of NPT for controlling periodontal disease by reducing inflammation (15, 16). Probing depth (PD) is an important clinical parameter that influences healing after NPT. Furthermore, it is considered for the assessment of the clinical status of the periodontal tissues (17).IPD is a predictable prognostic factor for the clinicians to anticipate the results of NPT. A number of studies showed that NPT reduces PD about 1-2 mm and increases the clinical attachment levels (CAL) about 0.5-2 mm in moderate and deep periodontal pockets (15, 16, 18, 19, 20). On the other hand, NPT may also cause attachment loss in shallow pockets. To avoid this, clinicians should be cautious not to perform over-instrumentation (21). The aim of this study was therefore to evaluate the relationship between IPD and changes in clinical parameters of CP patients following NPT. The null hypothesis of this research is that the NPT does not have any effect on the relationship between IPD and changes in selected clinical parameters used for the evaluation of CP treatment.
Subjects and Methods
The protocol of this single-centered, prospective study was approved by The Clinical Research Ethics Committee of Yeditepe University in Istanbul, Turkey (2012/255). Research was conducted according to the principles outlined in the Declaration of Helsinki on experimentation involving human subjects. The duration of the study was 10 weeks. This clinical trial was approved by ClinicalTrials.gov with the registration number NCT02861326.
Study participants
The sample of this study consisted of 1672 periodontal pockets of 15 chronic periodontitis patients having 3 mm≤IPD≤9 mm, who had been treated in the clinics of Periodontology Department, Marmara University Faculty of Dentistry, Istanbul, Turkey. To be included in this study, participants had to be systemically healthy, non-smoker, between 35 to 65 years of age, had not been received any periodontal treatment within the last 3 months, have horizontal bone loss in radiograps, have at least 20 teeth except third molars in the oral cavity and consent to participate in the study. CP was diagnosed according to Armitage (4). The exclusion criteria were as follows: any systemic alteration that might interfere with the prognosis of periodontal diseases (i.e,. diabetes mellitus, HIV infection), smoking, usage of antibiotics and anti-inflammatory drugs or any other medication taken within the previous 6 months that might affect the outcome of the study, any physical limitations or restrictions that might impede normal oral hygiene procedures. Written informed consent was obtained from all subjects.
Clinical protocol
In the first session, previous medical histories of all subjects were recorded and they went through detailed radiographic and periodontal examinations. Clinical periodontal parameters were recorded and NPT consisting of oral hygiene instructions, scaling and tooth surface debridement with ultrasonic (Cavitron, BOBCAT Pro Dentsply International, York, PA, USA) and hand (Gracey, SG 5/6, 7/8, 11/12, 13/14, Hu-Friedy Mfg. Co., LLC, Chicago, IL, USA) instruments were performed in two separate sessions with one week interval. Measurements of clinical periodontal parameters were repeated in all subjects 8 weeks after completion of NPT.
Periodontal examination
All clinical examinations were carried out by a single examiner (SEM). Intra-examiner calibration was done with five subjects whose data were not used in the study. The examiner measured their PD twice within three days. The intra-class correlation was calculated as 93.9%.
Clinical periodontal parameters included plaque index (PI)(22), gingival index (GI)(23), PD, clinical attachment level (CAL) and gingival recession (GR).The distance from the free gingival margin to the bottom of the periodontal pocket was defined as PD. CAL was defined as the distance from the cementoenamel junction to the bottom of the periodontal pocket. GR was defined as the distance from the cementoenamel junction to free gingival margin and, positive value was given if free gingival margin was located apically, and negative value if it was located coronally from the cementoenamel junction. Clinical parameters were recorded using a periodontal probe of University of North Carolina (PCPUNC15, Hu-Friedy Mfg. Co., LLC, Chicago, IL, USA).
PD values of the pockets measured at the first appointment were considered as the IPD values of these sites. Hence, all periodontal pockets were grouped according to their IPD with a range 3 to 9 mm for both single- and multi-rooted teeth, separately.
Statistical analysis
Statistical Package for Social Sciences (SPSS) software (IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY, USA) was used for statistical analysis. The Kolmogorov-Smirnov test was used to check the data for normal distribution. Repeated measurements of clinical periodontal parameters were analyzed with Paired Samples T-test. The relationship between IPD and changes in clinical periodontal parameters was analyzed with Pearson correlation coefficient. Confidence interval was set to 95% and p values less that 0.05 were considered as statistically significant.
Results
Mean age and age range of the study participants were; 45.06±3.79 years and 36 to 52 years, respectively. 1672 (N=1672) periodontal pockets were divided into 7 groups according to their IPD in both single- (number of periodontal pockets=1148) and multi-rooted teeth (number of periodontal pockets=524). As shown in Figure 1 and Figure 2, the sites having 4 mm IPD had the highest, and those having 9 mm IPD had the lowest frequency in both single- and multi-rooted teeth groups.
Figure 1.
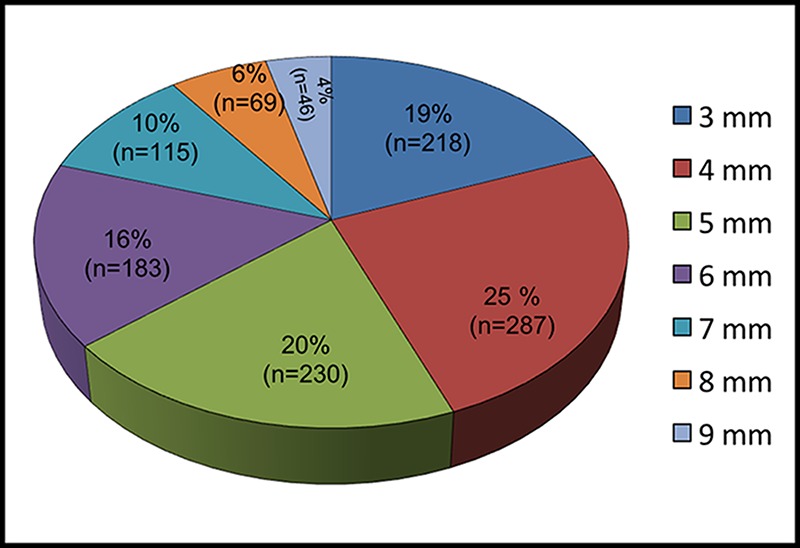
Number and frequencies of periodontal pockets in single-rooted teeth according to initial probing depth measurements.
Figure 2.
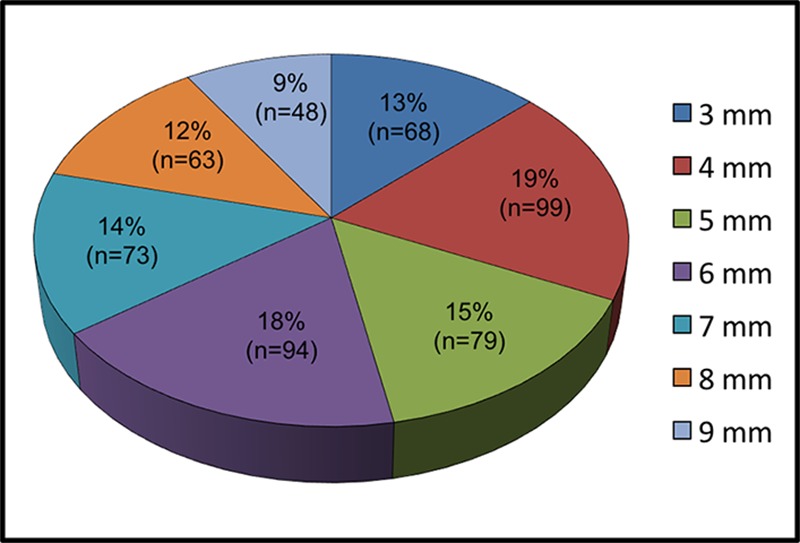
Number and frequencies of periodontal pockets in multi-rooted teeth according to initial probing depth measurements.
PD reduction (Figure 3) and Figure 4) and GR increase (Figure 5 and Figure 6) were significant in all groups (p<0.001) except for the sites having 3 mm IPD. Highest reduction in PD was observed at the sites with 9 mm IPD among groups in both single-rooted teeth (3.97±0. 97 mm) and multi-rooted teeth (2.39±1.67 mm).
Figure 3.
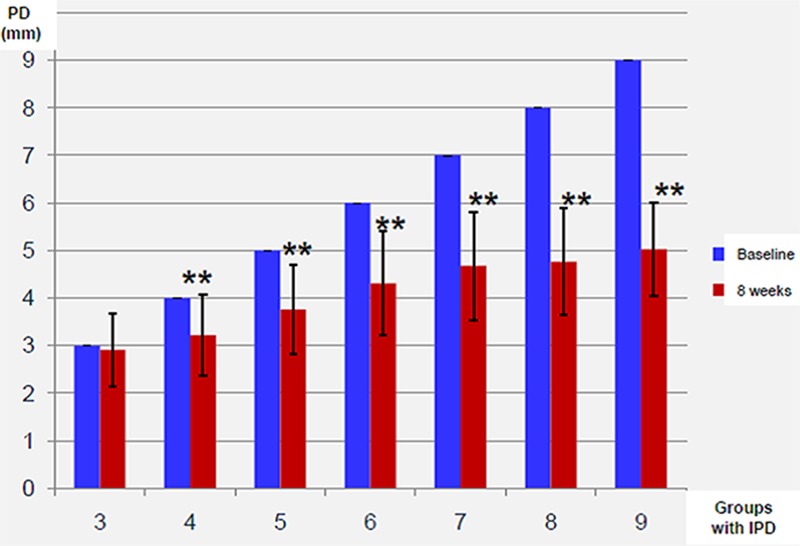
Mean probing depths on baseline and 8 weeks after treatment in single-rooted teeth groups (PD: probing depth, IPD: initial probing depth, ** indicates significant difference).
Figure 4.
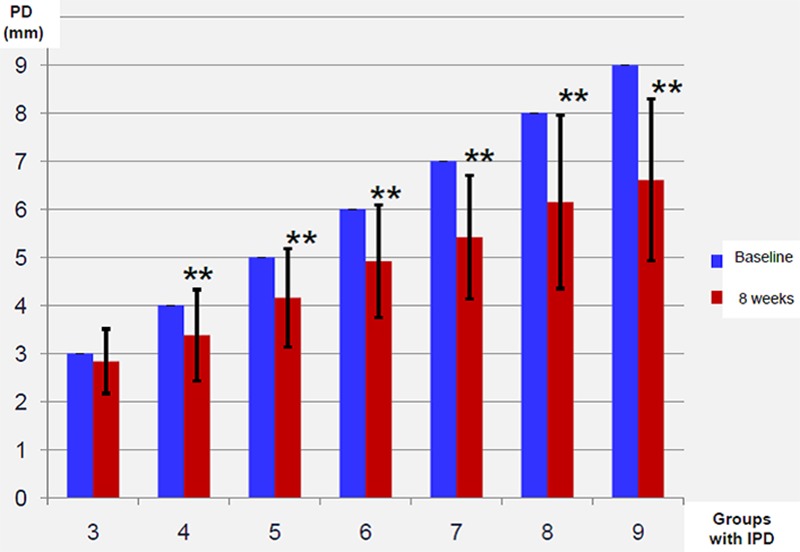
Mean probing depths on baseline and 8 weeks after treatment in multi-rooted teeth groups (PD: probing depth, IPD: initial probing depth, ** indicates significant difference).
Figure 5.
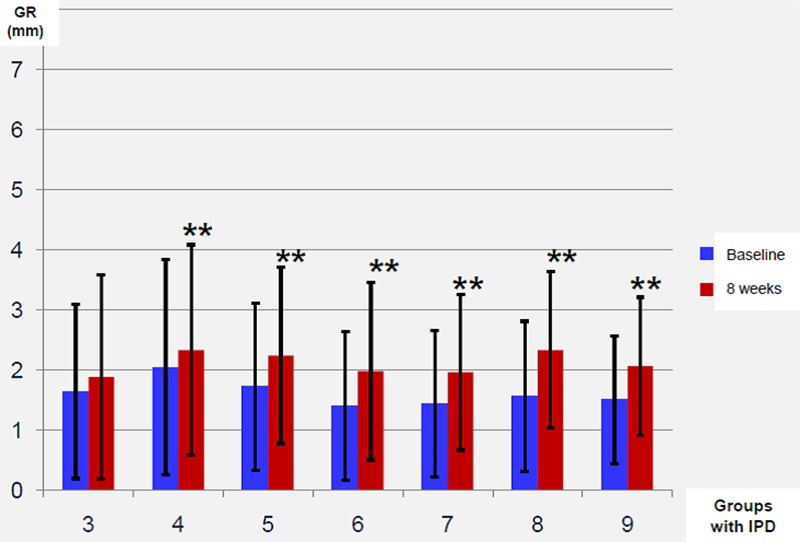
Mean gingival recessions on baseline and 8 weeks after treatment in single-rooted teeth groups (GR: gingival recession, IPD: initial probing depth, ** indicates significant difference).
Figure 6.
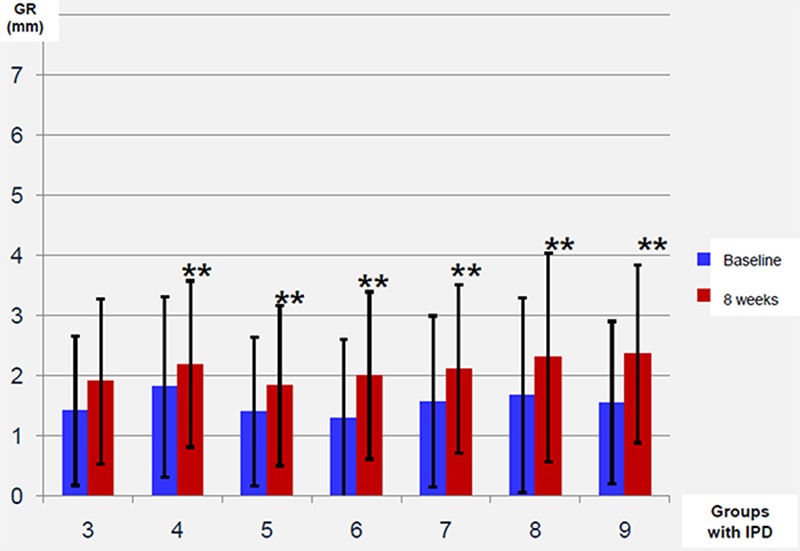
Mean gingival recessions on baseline and 8 weeks after treatment in multi-rooted teeth groups (GR: gingival recession, IPD: initial probing depth, ** indicates significant difference)
While significant attachment gains (AG) were obtained in all single-rooted teeth (p<0.001), except the sites with IPD=3 mm (Figure 7), multi-rooted teeth with only 7 mm≤IPD≤9 mm demonstrated significant AG (p<0.05) (Figure 8). On the other hand, the sites with IPD=3 mm demonstrated attachment loss rather than gain following NPT.
Figure 7.
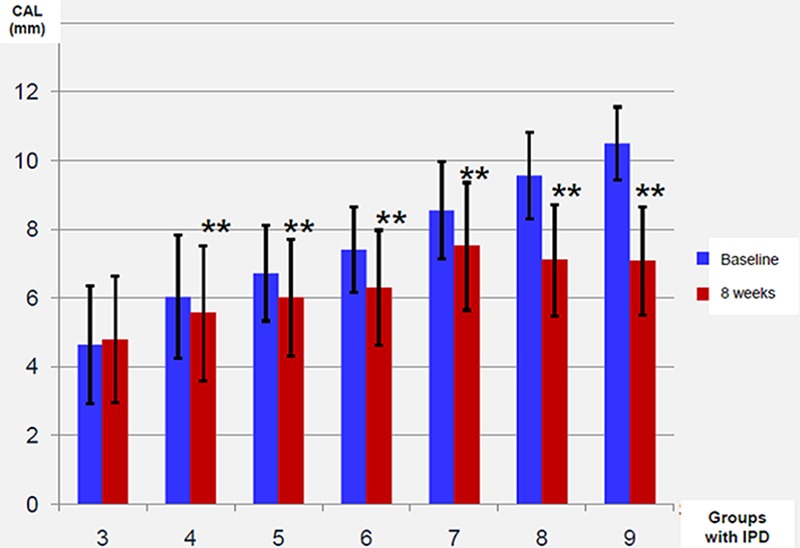
Mean clinical attachment levels on baseline and 8 weeks after treatment in single-rooted teeth groups (CAL: clinical attachment level, IPD: initial probing depth, **indicates significant difference).
Figure 8.
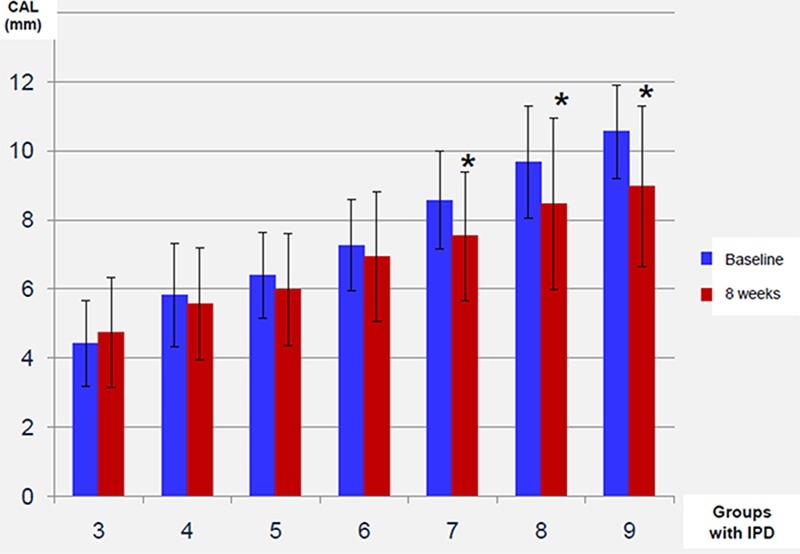
Mean clinical attachment levels on baseline and 8 weeks after treatment in multi-rooted teeth groups (CAL: clinical attachment level, IPD: initial probing depth, **indicates significant difference).
Positive correlations were detected between IPD and PD reduction, GR increase, AG on single-rooted teeth (p<0.001) (Table 1). Moreover, positive correlations (p<0.001) were found between IPD and PD reduction, GR increase in multi-rooted teeth, but there was no correlation between IPD and AG (Table 1).
Table 1.
Correlations between IPD and PD reduction, GR increase, attachment gain of periodontal pockets in single- and multi-rooted teeth ( IPD:initial probing depth, PD:probing depth, GR: gingival recession, AG: attachment gain, *p<0.05 and **p<0.001 in Pearson correlation analysis).
| IPD | PD Reduction | GR Increase | AG |
|---|---|---|---|
| Single-rooted teeth | 0.69** | 0.14** | 0.55** |
| Multi-rooted teeth | 0.44** | 0.11* | 0.26 |
Discussion
Chronic periodontitis is the most frequently observed periodontal disease worldwide and it is still one of the two foremost causes of tooth loss (24, 25). It is an infectious and inflammatory disease that needs to be treated for maintain both periodontal and systemic health (26, 27).
NPT is the first step for treatment of chronic periodontitis and it was accepted as the gold standard (28, 29). NPT ensures the mechanical elimination of periodontal pathogens and their by-products. Oral hygiene instructions, scaling and root surface debridement, are the basic steps of NPT to achieve resolution of gingival inflammation. These steps provide clean and smooth root surfaces that are biologically acceptable for the attachment of gingival epithelial and connective tissue cells, shrinkage of gingiva as well as PD reduction and AG(30, 31). The success of mechanical instrumentation is affected by the IPD, tooth root anatomy and surface structure, and clinician’s experience (32). Deep periodontal pockets are the most challenging sites to remove all calculus and biofilm. Badersten et al. (32) showed that up to 44% of calculus remain residual in the pockets having IPD>6 mm.
Following NPT, all recorded clinical parameters improved significantly in both single- and multi-rooted teeth. In addition, our results indicate that the PD reduction of pockets in single-rooted teeth is higher than that of multi-rooted teeth having the same IPD, which support the findings of previous reports (33). Moreover, positive correlations were observed between IPD and PD reduction, GR increase and AG on single-rooted teeth, which are consistent with the results of previous studies (17,28) evaluating effects of NPT on clinical periodontal parameters.
Cobb (28) reported 1.29 mm mean PD reduction in non-molar sites having 4 mm<IPD<6 mm. Our results showed that mean PD reduction of the sites in single-rooted teeth with 4 mm<IPD<6 mm was 1.23 mm. On the other hand, while the mean PD reduction of the sites with IPD>6 mm on single-rooted teeth was 3.17 mm in our study, Cobb (28) reported this value as 2.16 mm. In a recent study, Miremadi et al. (34) showed that the sites with IPD>6 mm represented 3.0 mm PD reduction, which is similar to our findings. PD reduction occurs either by GR increase, AG or by combination of these factors (5). GR results from the shrinkage of marginal gingival tissue in the apical direction(35). Transformation of the ulcerated pocket epithelium into the long junctional epithelium (36), and the enhancement of collagen fibers in the connective tissue content after NPT may result in AG, which leads to increased resistance of the tissue to the penetration of periodontal probe (37).
The sites with initially deep PDs demonstrated high levels of AG, while shallow sites showed loss of CAL following NPT, due to over-instrumentation that generates mechanical trauma (28). Cobb (28) reported 0.55 mm AG in the sites of non-molar teeth having 4 mm<IPD<6 mm and 1.19 mm of the sites with IPD>6mm. Similar to these findings, we found that respective AG values were 0.77 mm and 2.31 mm. On the other hand, in the study of Miremadi et al.(34), the mean CALs of shallow sites before and after NPT were 4.0±0.8 mm and 3.9±0.8 mm and the AG was statistically significant.
Conclusion
Within the limitations of this study, our findings demonstrated no correlation between IPD and AG in multi-rooted teeth, but support the positive association between IPD and PD reduction as well as GR increase following NPT, which is independent from tooth root anatomy. Moreover, our results emphasized that the sites with IPD=3 mm show attachment loss rather than gain following NPT.
Footnotes
Source of funding: None declared.
Conflict of interest: None declared.
References
- 1.Kinane DF, Attstrom R. Advances in the pathogenesis of periodontitis. Group b consensus report of the fifth european workshop in periodontology. J Clin Periodontol. 2005;32 Suppl 6:130–131. doi: 10.1111/j.1600-051X.2005.00823.x. [DOI] [PubMed] [Google Scholar]
- 2.Darveau RP, Tanner A, Page RC. The microbial challenge in periodontitis. Periodontol 2000. 1997;14:12–32. doi: 10.1111/j.1600-0757.1997.tb00190.x. [DOI] [PubMed] [Google Scholar]
- 3.Dentino A, Lee S, Mailhot J, Hefti AF. Principles of periodontology. Periodontol 2000. 2013;61(1):16–53. doi: 10.1111/j.1600-0757.2011.00397.x. [DOI] [PubMed] [Google Scholar]
- 4.Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4(1):1–6. doi: 10.1902/annals.1999.4.1.. [DOI] [PubMed] [Google Scholar]
- 5.Claffey N, Polyzois I, Ziaka P. An overview of nonsurgical and surgical therapy. Periodontol 2000. 2004;36:35–44. doi: 10.1111/j.1600-0757.2004.00073.x. [DOI] [PubMed] [Google Scholar]
- 6.Ishikawa I, Baehni P. Nonsurgical periodontal therapy--where do we stand now. Periodontol 2000. 2004;36:9–13. doi: 10.1111/j.1600-0757.2004.03670.x. [DOI] [PubMed] [Google Scholar]
- 7.Yilmaz S, Efeoglu E, Noyan U, Kuru B, Kilic AR, Kuru L. The evolution of clinical periodontal therapy. J Marmara Univ Dent Fac. 1994;2(1):414–423. [PubMed] [Google Scholar]
- 8.Badersten A, Nilveus R, Egelberg J. Effect of nonsurgical periodontal therapy. I. Moderately advanced periodontitis. J Clin Periodontol. 1981;8(1):57–72. doi: 10.1111/j.1600-051X.1981.tb02024.x. [DOI] [PubMed] [Google Scholar]
- 9.Aljateeli M, Koticha T, Bashutski J, Sugai JV, Braun TM, Giannobile WV, Wang HL. Surgical periodontal therapy with and without initial scaling and root planing in the management of chronic periodontitis: A randomized clinical trial. J Clin Periodontol. 2014;41(7):693–700. doi: 10.1111/jcpe.12259. [DOI] [PubMed] [Google Scholar]
- 10.Magnusson I, Lindhe J, Yoneyama T, Liljenberg B. Recolonization of a subgingival microbiota following scaling in deep pockets. J Clin Periodontol. 1984;11(3):193–207. doi: 10.1111/j.1600-051X.1984.tb01323.x. [DOI] [PubMed] [Google Scholar]
- 11.Mousques T, Listgarten MA, Phillips RW. Effect of scaling and root planing on the composition of the human subgingival microbial flora. J Periodontal Res. 1980;15(2):144–151. doi: 10.1111/j.1600-0765.1980.tb00268.x. [DOI] [PubMed] [Google Scholar]
- 12.Segelnick SL, Weinberg MA. Reevaluation of initial therapy: When is the appropriate time. J Periodontol. 2006;77(9):1598–1601. doi: 10.1902/jop.2006.050358. [DOI] [PubMed] [Google Scholar]
- 13.Mousques T, Listgarten MA, Stoller NH. Effect of sampling on the composition of the human subgingival microbial flora. J Periodontal Res. 1980;15(2):137–143. doi: 10.1111/j.1600-0765.1980.tb00267.x. [DOI] [PubMed] [Google Scholar]
- 14.Drisko CH. Nonsurgical periodontal therapy. Periodontol 2000. 2001;25:77–88. doi: 10.1034/j.1600-0757.2001.22250106.x. [DOI] [PubMed] [Google Scholar]
- 15.Suvan JE. Effectiveness of mechanical nonsurgical pocket therapy. Periodontol 2000. 2005;37:48–71. doi: 10.1111/j.1600-0757.2004.03794.x. [DOI] [PubMed] [Google Scholar]
- 16.Van der Weijden GA, Timmerman MF. A systematic review on the clinical efficacy of subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol. 2002;29 Suppl 3:55–71. doi: 10.1034/j.1600-051X.29.s3.3.x. [DOI] [PubMed] [Google Scholar]
- 17.Claffey N, Loos B, Gantes B, Martin M, Egelberg J. Probing depth at re-evaluation following initial periodontal therapy to indicate the initial response to treatment. J Clin Periodontol. 1989;16(4):229–233. doi: 10.1111/j.1600-051X.1989.tb01646.x. [DOI] [PubMed] [Google Scholar]
- 18.Cobb CM. Clinical significance of non-surgical periodontal therapy: An evidence-based perspective of scaling and root planing. J Clin Periodontol. 2002;29 Suppl 2:6–16. doi: 10.1034/j.1600-051X.29.s2.2.x. [DOI] [PubMed] [Google Scholar]
- 19.Sanz I, Alonso B, Carasol M, Herrera D, Sanz M. Nonsurgical treatment of periodontitis. J Evid Based Dent Pract. 2012;12(3 Suppl):76–86. doi: 10.1016/S1532-3382(12)70019-2. [DOI] [PubMed] [Google Scholar]
- 20.Tunkel J, Heinecke A, Flemmig TF. A systematic review of efficacy of machine-driven and manual subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol. 2002;29 Suppl 3:72–81. doi: 10.1034/j.1600-051X.29.s3.4.x. [DOI] [PubMed] [Google Scholar]
- 21.Drisko CL. Scaling and root planing without overinstrumentation: Hand versus power-driven scalers. Curr Opin Periodontol. 1993:78–88. [PubMed] [Google Scholar]
- 22.Silness J, Loe H. Periodontal disease in pregnancy. Ii. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–135. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 23.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–551. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 24.Albandar JM, Rams TE. Global epidemiology of periodontal diseases: An overview. Periodontol 2000. 2002;29:7–10. doi: 10.1034/j.1600-0757.2002.290101.x. [DOI] [PubMed] [Google Scholar]
- 25.Oliver RC, Brown LJ, Loe H. Periodontal treatment needs. Periodontol 2000. 1993;2:150–160. doi: 10.1111/j.1600-0757.1993.tb00227.x. [DOI] [PubMed] [Google Scholar]
- 26.Caula AL, Lira-Junior R, Tinoco EM, Fischer RG. The effect of periodontal therapy on cardiovascular risk markers: A 6-month randomized clinical trial. J Clin Periodontol. 2014;41(9):875–882. doi: 10.1111/jcpe.12290. [DOI] [PubMed] [Google Scholar]
- 27.Jeffcoat MK, Jeffcoat RL, Gladowski PA, Bramson JB, Blum JJ. Impact of periodontal therapy on general health: Evidence from insurance data for five systemic conditions. Am J Prev Med. 2014;47(2):166–174. doi: 10.1016/j.amepre.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 28.Cobb CM. Non-surgical pocket therapy: Mechanical. Ann Periodontol. 1996;1(1):443–490. doi: 10.1902/annals.1996.1.1.443. [DOI] [PubMed] [Google Scholar]
- 29.Drisko CL. Periodontal debridement: Still the treatment of choice. J Evid Based Dent Pract. 2014;14 Suppl:33–41. doi: 10.1016/j.jebdp.2014.02.007. e31. [DOI] [PubMed] [Google Scholar]
- 30.Haffajee AD, Cugini MA, Dibart S, Smith C, Kent RL. Socransky SS. The effect of srp on the clinical and microbiological parameters of periodontal diseases. J Clin Periodontol. 1997;24(5):324–334. doi: 10.1111/j.1600-051X.1997.tb00765.x. [DOI] [PubMed] [Google Scholar]
- 31.Lavanchy DL, Bickel M, Baehni PC. The effect of plaque control after scaling and root planing on the subgingival microflora in human periodontitis. J Clin Periodontol. 1987;14(5):295–299. doi: 10.1111/j.1600-051X.1987.tb01536.x. [DOI] [PubMed] [Google Scholar]
- 32.Badersten A, Nilveus R, Egelberg J. Effect of nonsurgical periodontal therapy (viii). Probing attachment changes related to clinical characteristics. J Clin Periodontol. 1987;14(7):425–432. doi: 10.1111/j.1600-051X.1987.tb01548.x. [DOI] [PubMed] [Google Scholar]
- 33.Loos B, Nylund K, Claffey N, Egelberg J. Clinical effects of root debridement in molar and non-molar teeth. A 2-year follow-up. J Clin Periodontol. 1989;16(8):498–504. doi: 10.1111/j.1600-051X.1989.tb02326.x. [DOI] [PubMed] [Google Scholar]
- 34.Miremadi SR, de Hugo B, Steyaert H, Princen K, Cosyn J. A randomized controlled trial comparing surgical dna non-surgical periodontal therapy: A 3-year clinical and cost-effectiveness analysis. J Clin Periodontol. 2015;42(8):748–755. doi: 10.1111/jcpe.12434. [DOI] [PubMed] [Google Scholar]
- 35.Adriaens PA, Adriaens LM. Effects of nonsurgical periodontal therapy on hard and soft tissues. Periodontol 2000. 2004;36:121–145. doi: 10.1111/j.1600-0757.2004.03676.x. [DOI] [PubMed] [Google Scholar]
- 36.Caton JG, Zander HA. The attachment between tooth and gingival tissues after periodic root planing and soft tissue curettage. J Periodontol. 1979;50(9):462–466. doi: 10.1902/jop.1979.50.9.462. [DOI] [PubMed] [Google Scholar]
- 37.Caton J, Nyman S, Zander H. Histometric evaluation of periodontal surgery. Ii. Connective tissue attachment levels after four regenerative procedures. J Clin Periodontol. 1980;7(3):224–231. doi: 10.1111/j.1600-051X.1980.tb01965.x. [DOI] [PubMed] [Google Scholar]


