Abstract
Background
Especially in the first 6 months of life, skull deformities manifesting as a uni- or bilateral flattening of the occiput often give rise to questions of differential diagnosis and potential treatment. In this review, the authors summarize the current understanding of risk factors for this condition, and the current state of the relevant diagnostic assessment and options for treatment.
Methods
The recommendations given in this selective review of the literature are based on current studies and on existing guidelines on the prevention of sudden infant death, the recommendations of the German Society for Pediatric Neurology (Deutsche Gesellschaft für Neuropädiatrie), and the American guidelines on the treatment of positional plagiocephaly in infancy.
Results
Pre-, peri-, and postnatal risk factors can contribute to the development of positional skull deformities. These deformities can be diagnosed and classified on the basis of their clinical features, supplemented in unclear cases by ultrasonography of the cranial sutures. The putative relationship between positional skull deformities and developmental delay is currently debated. The main preventive and therapeutic measure is parent education to foster correct positioning habits (turning of the infant to the less favored side; prone positioning on occasion when awake) and beneficial stimulation of the infant (to promote lying on the less favored side). If the range of motion of the head is limited, physiotherapy is an effective additional measure. In severe or refractory cases, a skull orthosis (splint) may be useful.
Conclusion
The parents of children with positional skull deformities should be comprehensively informed about the necessary preventive and therapeutic measures. Treatment should be initiated early and provided in graded fashion, according to the degree of severity of the problem. Parental concern about the deformity should not be allowed to lead to a rejection of the reasonable recommendation for a supine sleeping position.
Since the 1992 publication of the recommendation to put infants to sleep on their backs, rates of sudden infant death have fallen significantly (1, 2). For this reason, this sensible recommendation should be adhered to (3). Simultaneously, reports of mostly mild skull deformities in children of merely a few weeks in age increased over this period (4– 6), presenting clinically as a unilateral or bilateral flattening of the occiput. Although causality has, strictly speaking, not been proved, an association with the recommendation for putting babies to sleep in the supine position seems plausible. The rate of skull deformities decreases as children get older. In a cohort study, 16% of children aged 6 weeks had skull deformities whereas the rate fell to 3.3% at age 2 years (7). A prospective epidemiological study from the Netherlands found moderate to severe skull deformities in 1% of investigated children aged 5.5 years (8). In routine clinical practice, skull deformities—especially within the first 6 months of life—often give rise to questions about differential diagnoses and options for intervention (4, 5, 7, 9– 12, e1, e2).
Methods
This selective literature review provides an overview of the pathogenesis, possible risk factors, symptoms, and diagnosis of positional skull deformities, as well as therapeutic options. We took into account the fact that some existing studies have substantial limitations: small numbers of investigated patients, lacking control groups, and pre-selection in the severity grade under investigation with resultant biases (6). Furthermore, the number of prospective studies is small.
The recommendations mentioned follow the US and German guidelines for the prevention of sudden infant death, the recommendations of the German Neuropediatric Society, and the guideline issued at the end of 2016 by the US Congress of Neurological Surgeons (CNS) and the Section of Pediatric Neurosurgery for the treatment of pediatric positional plagiocephaly (2– 5). An evidence-based German guideline is lacking to date.
Pathogenesis
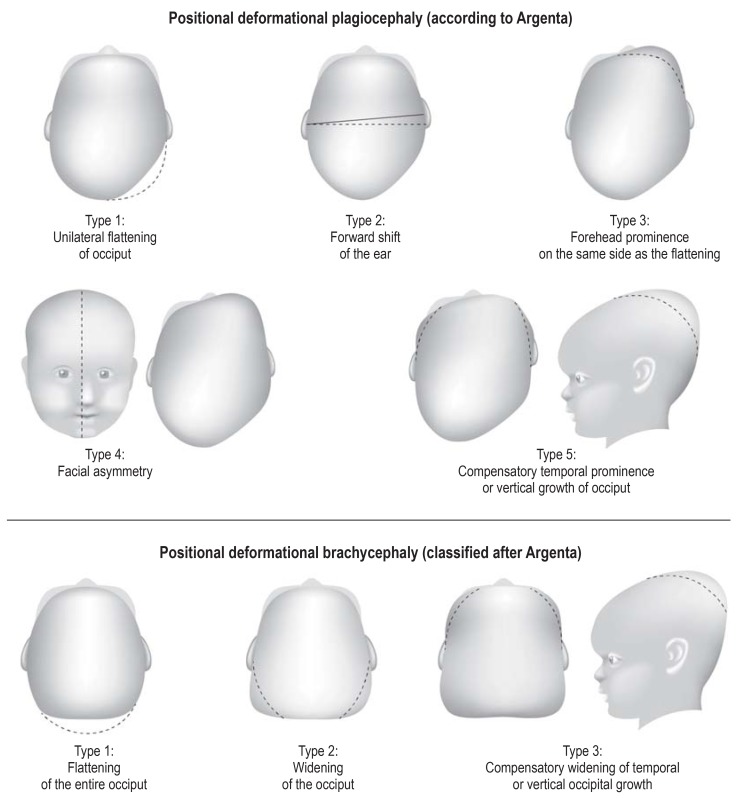
At birth, the cranial sutures have not yet fused, so that the cranial bones can move when passing through the birth canal and the skull may rapidly increase in size post partum. The crucial force in this setting is the increase in the size of the cerebrum, whose volume doubles within the first 6–7 months of life. The skull is easily moldable in the first months of life, and application of external force/pressure can lead to deformity of the cerebral cranium as well as of the viscerocranium. Placing a baby on its back can therefore lead to unilateral flattening of the occiput (positional/deformational plagiocephaly, DP) or symmetrical flattering of the entire occiput (positional/deformational brachycephaly, DB) (figure 1).
Figure 1.
Classification of positional plagiocephaly and brachycephaly according to Argenta (20)
Positional skull deformities have to be distinguished from intrauterine or peripartum deformities, which usually reduce spontaneously and quickly. For this reason, the terms DP or DB should be used only from the 6th week of life; perinatal skull deformities can turn into positional symmetries.
Risk factors
In the pathogenesis of positional skull deformities, prepartum, peripartum, and postpartum risk factors play a role (table 1).
Table 1. Predisposing (risk) factors.
| Factors | Mentioned in the literature (%) |
| Prenatal factors | |
| Male sex | 72 |
| Primiparous mother | 45 |
| Young parents | 32 |
| Low educational status | 27 |
| Forced abnormal intrauterine positioning | 18 |
| Perinatal factors | |
| Obstetric interventions (ventouse, forceps) | 45 |
| High birth weight | 37 |
| Prematurity | 32 |
| Large head circumference | 23 |
| Postnatal factors | |
| Supine position | 63 |
| Restricted head movement, torticollis | 45 |
| Preference for one side | 37 |
| Bottle feeding without changing position | 27 |
| Little “tummy time“ | 27 |
| Developmental delay, little activity | 23 |
Limited intrauterine space or forced abnormal intrauterine positioning have been discussed as predisposing factors (9, 10). This could explain why the incidence doubles in boys (9– 13), who as a rule are bigger than girls. Multiple births are also associated with a higher risk (14).
Mobility restrictions of the cervical spine—for example owing to torticollis or a bleed into the sternocleidomastoid muscle as a result of birth trauma—are additional risk factors for developing DP (15). Torticollis is present in 20% of children with DP but in only 0.1–2% of children with a symmetrical skull shape (14). Skull deformities are more common in primiparous women and after ventouse or forceps deliveries (11). Preterm birth or developmental delays—possibly associated with a prolonged stay in an intensive care ward—are further risk factors.
A preference for one side can develop as a result of unilateral stimuli—for example, if the baby‘s feeding position is never changed (16). Our own studies have shown that 8% of children younger than 16 weeks had a favorite side; in about half of cases the result was unilateral flattening of the occiput. By contrast, breast feeding has a protective effect because it means changing position during feeding (16). As has been described previously, consistently putting infants to sleep in the supine position is also a risk factor (11, 12, 17). Ultimately, the pathogenesis and the underlying mechanisms of positional skull deformities have not been fully explained (9).
Diagnostic evaluation
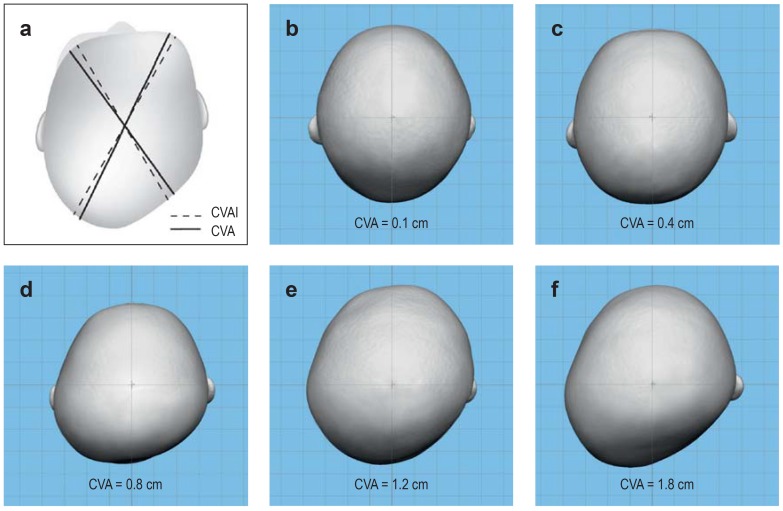
Usually the diagnosis of positional skull asymmetry is possible only by means of a clinical medical examination (4, 5, 18, 19). The clinical presentation of DP differs from that of DB (5). Argenta et al. undertook a classification based on the clinical characteristics (figure 1) (5, 20, e3). The drawbacks of this classification are that the severity of the individual abnormalities is not reflected. This makes it difficult to assess their course, among others. In addition to the clinical description, the diagonal diameters, the position, the width, and the circumference of the head are captured by applying standard cephalometric measurements using a tape measure and pelvimeter (5, 21). Such measurements undertaken on the head directly, of anthropometrically defined landmarks, are reliable, but may be riddled with errors in the case of restless infants (22, e4). Moss and Mortenson et al. (e5, e6) define the cranial vault asymmetry (CVA) (Figure 2, eFigure 1) as the difference between the largest and smallest diagonal diameter of the skull. A CVA <3 mm is regarded as physiological, a deviation between = 3 mm and = 12 mm is regarded as a mild to moderate asymmetry, and a deviation of >12 mm counts as a moderate to severe asymmetry (5) (figure 2). Whereas the CVA is measured without defined angles, Loveday et al. (e7) defined the so-called cranial vault asymmetry index (CVAI). To this end, two diagonals are used, which are angled bilaterally by 30° to the median sagittal plane. The CVAI results from the difference in length of these two diagonals, which is divided by the longer diagonal. Values below 3.5% are regarded as physiological (5).
Figure 2.
a) Schematic depiction of cephalometric measurements (see also eFigure 1). The solid line shows the measurement of the cranial vault asymmetry (CVA) according to Moss and Mortenson et al. (e5, e6), based on the difference between the largest and smallest diagonal diameter. The dotted line shows the measurement of the cranial vault asymmetry index (CVAI) according to Loveday et al. (e7), based on two diagonals that are both angled at 30° to the mid-sagittal plane. b–f) Stereophotogrammetric images (top view) with differing cranial vault asymmetry (CVA). Even though the image cannot visualize all clinical signs, compensatory prominence of the forehead and compensatory widening of the skull with increasing degrees of severity are clearly recognizable.
eFigure 1.
Cephalometric measurement of the diagonal diameter by means of pelvimetry
In order to capture the skull‘s three-dimensionality, radiation-free surface scanning procedures can be used, among which 3-D stereophotogrammetry has been found to be a fast, reproducible, and precise method (4, 23). Synchronized photographic cameras with an exposure time of below 1.5 ms generate a 3-D image of the head that is free from radiation and artefacts. These data sets are used for extended diagnostic evaluation, follow-up, and also as a matrix for creating individually made cranial orthoses (23). Plaster impressions of babies‘ heads are regarded as obsolete in this day and age.
If uncertainty prevails even after careful clinical examination, ultrasonography can be undertaken in order to establish the diagnosis (4, 5, 18, 19). Within the first 13 months of life, open skull sutures can be distinguished from fused sutures with a high degree of reliability (e8). The next step, which is required in rare cases of doubt only, consists of a two-plane skull x-ray. In the diagnostic evaluation of positional skull asymmetry, no justifiable indication exists for computed tomography scanning, which incurs a substantial radiation burden (4, 5, 18, 24).
Differential diagnostic evaluation
For the purposes of differential diagnostic evaluation, positional skull deformities have to be distinguished from premature fusion of the skull sutures (craniosynostosis) (15).
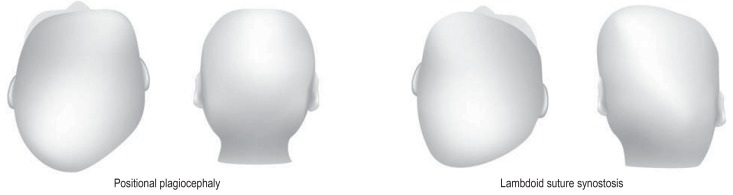
In this setting, the premature unilateral fusion of the lambdoid suture, accompanied by unilateral flattening of the occiput, can be mistaken for DP (efigure 2). If looking at a unilateral lambdoid suture synostosis from above, the head has a trapezoid shape. In DP, however, the shape resembles a parallelogram, resulting from a possible protrusion of the forehead (frontal bossing) of the side of the flattened occiput. The occipital aspect in synostosis of the lambdoid suture shows a parallelogram-like shift, caused by the contralateral protrusion [bossing] of the parietal region and the inferior displacement of the petrous bone, with the ipsilateral ear shifted downwards (15, 23). In DB, the occipital aspect will usually show a normal shape of the head.
eFigure 2.
Clinical distinction between right-sided positional deformational plagiocephaly (DP) and right-sided unilateral lambdoid suture synostosis (LS)
Left: DP – top view shows parallelogram-like shift; back view shows normal shaped head
Right: LS – top view shows trapezoid shaped head; back view shows parallelogram shaped head
In rare cases, unilateral synostosis of the coronal suture can be mistaken for DP. In unilateral coronal synostosis, a top view shows ipsilateral reduction of the sagittal skull length. Contralaterally, frontolateral bossing of the forehead is seen. Furthermore, ipsilateral convex facial scoliosis is seen, with the face deviating to the opposite side of the affected suture and the characteristic ipsilateral orbital deformation. These signs are usually of differential diagnostic value (19).
Pathogenesis and spontaneous course
An association between positional skull deformities and developmental delays has been the subject of controversial discussion (15, e9, e10). Motor developmental delays have been reported most often (25, 26). A fundamental problem of all studies of this topic is the question of whether a developmental delay is the cause or the consequence of a skull deformity (25). Robust data are thus far lacking. Numerous studies have methodological problems (non-homogenous groups of patients, no control groups) and different influencing variables (socioeconomic status, parents‘ IQ, individual support, among others) (15). These criticisms were considered by Weissler et al. (26). They regard a developmental delay only as a risk factor, not as a consequence of a positional skull deformity. An association with raised intracranial pressure has not been described.
The extent to which positional asymmetries affect the development of mandible/maxilla, teeth, and possible malocclusions has not been studied to a satisfactory degree. An association between DP and lateral crossbite is possible, but has not been confirmed (21).
The observed rise in incidence lasts up to the 4th month of life; over the following period, up to the 24th month of life, the incidence decreases (7, 8). According to some reports, the incidence falls to 3.3% at age 2 years (7, 13). A recent prospective epidemiologic study from the Netherlands found mild asymmetries in 5.5% of children aged 5.5 years; the proportion of moderate to severe skull deformities was 1% (8). A study including 14–17 year olds who had been born after the recommendation for putting babies to sleep on their backs had been published found a prevalence of 2.1% (27). Unfortunately the study had not collected data on the possible burden caused by the existing asymmetry. It therefore remains unknown which criteria contribute to a favorable or unfavorable spontaneous course.
The largest fluctuations in existing studies on incidence and spontaneous disease course can be explained by different ages or different methods (clinically descriptive or cephalometric) at the time of data collection, as well as differently composed patient populations (26).
Few studies assume that the existing asymmetries will improve or normalize completely without treatment, most of the studies recommend therapy according to stage (4, 26, 27, e11, e12).
Prevention
Providing parents with relevant information/education and preventive measures are simple, economical, and effective options for preventing positional skull deformities (4, 5, 28).
The consultation with the parents should also promote understanding of the possible development of a positional skull disorder, and thus its prevention. Even though in positional skull deformities, psychosocial considerations are key, no conclusion is possible about any further reaching consequences (26).
Making physical contact from varying angles has a preventive effect—such as when holding the child or by changing the orientation of the bed vis-à-vis window or door. In addition to such changes when making physical contact, the less favored side can be intentionally supported as a corrective and thus therapeutic measure (4, 5, 28). The child may develop a favorite position if the parents prefer a particular side. This might explain the fact that the right side is more often affected, as most parents are right-handed.
Placing awake infants on their tummies for 3–30 minutes every day („tummy time“) while keeping them under observation also reduces the risk of developing positional skull deformity (15, 29, 30).
Therapy
The therapeutic spectrum includes different approaches, which build on each other provided the therapy starts early (table 2) (4, 5, 31). On the background of different wishes and ideas or parents‘ expectations of a beautifully shaped head, medical and cosmetic aspects will have to be balanced carefully.
Table 2. Diagnostic evaluation, prevention, and treatment of positional skull deformities.
| Diagnostic evaluation | ||
| Clinical examination |
|
|
| Ultrasound exam of the skull sutures |
|
|
| Two-place skull x-ray |
|
|
| Prevention*1 | ||
| Informing/educating and instructing the parents |
|
|
| Therapy*2 | Optimal timing | |
| Positioning therapy |
|
|
| Physiotherapy |
|
|
| Cranial remolding orthosis (baby helmet therapy) |
|
|
*1 Prevention should be undertaken early in all children.
*2 Treatments should be initiated in a timely manner and build on one another, in the best case scenario..
Positioning
The simplest therapeutic approach is positioning treatment, delivered by the parents. Useful in this setting, before the 4th month of life, is actively positioning the baby, while lying on its back, from side to side or placing it towards the side of its head that is not affected. In moderate DP, this might be sufficient for the shape of the head to normalize (4, 32).
Positioning aids, such as cushions, have been described in some studies as useful therapy, comparable or even superior to physiotherapy (33, e13). However, the valid guidelines for preventing sudden infant death make explicit mention of the fact that infants‘ beds should be free of any pillows, cushions, and the like (2– 4). Positioning treatment is unequivocally recommended, whereas the advice is against using positioning aids (4, 5).
Physiotherapy
Movement restrictions of the head are often the cause of DP, and for this reason they should be treated early on (34). Even though the literature does not provide an optimal start date for therapy, the CNS guidelines recommend the early uptake of additional physiotherapy or manual therapy to reduce the incidence and prevalence of DP (32, 33, 35). Appropriate forms of physiotherapy include passive stretching or therapeutic approaches following Bobath or Vojta (36). The relevant guidelines contain detailed explanations of the physiotherapeutic approaches. Physiotherapy administered in addition to positioning therapy or use of a cranial orthosis shortens the duration of therapy and improves the results in severe cases (4, 35). Infants younger than 6 months with a CVA <10 mm should initially be treated only by using positional therapy and physiotherapy (31). In a study including 4378 children, 77.1% of existing asymmetries normalized as a result (31).
Cranial orthoses (cranial molding therapy or helmet therapy)
An individually made cranial orthosis that fits without exerting pressure remolds physiological growth by permitting growth in areas that are deficient and inhibits it in areas where it is too prominent (figure 3). This enables passive harmonization of the head. The orthosis is worn 23 hours a day (26). Possible risks of cranial orthosis treatment include skin irritations and pressure sores (37). Problems caused by the orthosis‘s own weight (ca. 150–180 g) are not to be expected (37). We are not aware of any studies of possible psychosocial impairments of children owing to a cranial orthosis. The costs for cranial remolding orthosis therapy are about € 2000 (6).
Figure 3.
Child wearing cranial remolding orthosis, Arrows show space for growth
Compared with positioning therapy and physiotherapy, cranial orthoses reduce existing deformities more efficiently and quickly (4, 31). The only randomized study on that topic does, however, not show any benefit for baby helmet therapy compared with positional or physical therapy (38). However, the study excluded more severe skull deformities, which reduces its validity (4, 26, 38). The largest—but retrospective—study shows that orthosis therapy is superior (95% normalization of asymmetries) to positioning therapy and physiotherapy (77.1%) (31). If the diagnosis is made early, positioning therapy and physiotherapy may be sufficient. In such cases, baby helmet therapy should be started only if the asymmetry parameters have not improved after 4 months (31). Further prospective randomized studies are needed.
Although the treatment of DP notably improves the CVA, the ear axis is mostly corrected to a rather lesser degree (23). For the duration of baby helmet therapy, continuing physiotherapeutic measures, especially if movement impairments persist, make sense. In principle, therapy using cranial orthoses is recommended in pronounced skull deformities around the 6th month of life (4, 5, 23, 39). Recent studies have found, however, that in severe forms, an earlier start is associated with better results (4). Therapy can be started up to the end of the 1st year of life, although such a late start of treatment may hamper the therapeutic success (4, 5, 31, 39). While bearing in mind growth dynamics, hitherto untreated infants beyond the 7th month of life with a CVA >12 mm or a clearly visible deformity should be treated immediately with an orthosis (4, 31).
Surgery for positional skull asymmetries is not justifiable, except for extremely rare indications stemming from cosmetic-social considerations (5, 26).
Conclusion
When treating positional skull deformities, the earliest possible and stage-appropriate intervention is of essence.
In addition to initially explaining the problem to the parents, targeted positional measures and physiotherapeutic interventions can be effective therapies. Treatment using remolding cranial orthoses is very effective but should be reserved for therapy-resistant and severe forms.
Parents‘ worry about positional skull deformities should never lead to disregarding the sensible advice for putting babies to sleep on their backs (4, 40).
Key Messages.
Among the risk factors for positional skull deformities that are most frequently mentioned in the literature are male sex, baby placed on its back for sleep, primiparous mother, obstetric measures (ventouse, forceps), restricted head movement (torticollis), preference for one side, and high birth weight
Mostly, clinical examination is sufficient for making a diagnosis. In less clear-cut cases, additional cranial ultrasonography can be undertaken to check the degree of fusion of the skull sutures. Two-place radiography is required in only very rare cases of doubt. Because of the radiation load, computed tomography scanning is not justifiable
After a diagnosis has been made, early and stage/grade-appropriate therapy should be initiated.
Positioning therapy and physiotherapy can be used for all grades of severity of positional skull deformity, whereas treatment using a cranial remolding orthosis should be undertaken only in severe cases or those that were diagnosed late.
Even though placing an infant on its back favors the development of positional skull deformities, the recommendation stands that babies should be placed in a supine position in order to avoid sudden infant death.
Acknowledgments
Translated from the original German by Birte Twisselmann, PhD.
Footnotes
Conflict of interests statement
The authors declare that no conflict of interest exists.
References
- 1.American Academy of Pediatrics. AAP Task Force on Infant Positioning and SIDS: positioning and SIDS. Pediatrics. 1992;89:1120–1126. [PubMed] [Google Scholar]
- 2.Arbeitsgemeinschaft der Wissenschaftlichen. Medizinischen Fachgesellschaften, Leitlinie der Deutschen Gesellschaft für Schlafmedizin Nr. 063/002, S1-Leitlinie. Plötzlicher Säuglingstod. 01/2012. [Google Scholar]
- 3.AAP Task Force on sudden infant death syndrome. SIDS and other sleep-related infant deaths: updated 2016 recommendations for a safe infant sleeping environment. Pediatrics. 2016;138 doi: 10.1542/peds.2016-2938. e20162938. [DOI] [PubMed] [Google Scholar]
- 4.Flannery AM, Tamber MS, Mazzola C, et al. Congress of neurological surgeons systematic review and evidence-based guidelines for the management of patients with positional plagiocephaly: executive summary. Neurosurgery. 2016;79:623–624. doi: 10.1227/NEU.0000000000001426. [DOI] [PubMed] [Google Scholar]
- 5.Rosenbaum T, Borusiak P, Schweitzer T, et al. Dynamische Kopforthesen („Helmtherapie“) Stellungnahme der gemeinsamen Therapiekommission der Gesellschaft für Neuropädiatrie und der Deutschen Gesellschaft für Sozialpädiatrie und Jugendmedizin 2012. Neuropädiatrie in Klinik und Praxis. 2014;1:4–9. [Google Scholar]
- 6.Goh JL, Bauer DF, Durham SR, Stotland MA. Orthotic (helmet) therapy in the treatment of plagiocephaly. Neurosurg Focus. 2013;35 doi: 10.3171/2013.7.FOCUS13260. [DOI] [PubMed] [Google Scholar]
- 7.Hutchison BL, Hutchison LAD, Thompson JMD, Mitchell EA. Plagiocephaly and brachycephaly in the first two years of life: a prospective cohort study. Pediatrics. 2004;114:970–980. doi: 10.1542/peds.2003-0668-F. [DOI] [PubMed] [Google Scholar]
- 8.van Vlimmeren LA, Engelbert RH, Pelsma M, Groenewoud HM, Boere-Boonekamp MM, der Sanden MW. The course of skull deformation from birth to 5 years of age: a prospective cohort study. Eur J Pediatr. 2017;176:11–21. doi: 10.1007/s00431-016-2800-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Bock F, Braun V, Renz-Polster H. Deformational plagiocephaly in normal infants: a systematic review of causes and hypotheses. Arch Dis Child. 2017;102:535–542. doi: 10.1136/archdischild-2016-312018. [DOI] [PubMed] [Google Scholar]
- 10.Joganic JL, Lynch JM, Littlefield TR, Verrelli BC. Risk factors associated with deformational plagiocephaly. Pediatrics. 2009;124:e1126–e1133. doi: 10.1542/peds.2008-2969. [DOI] [PubMed] [Google Scholar]
- 11.Mawji A, Vollman AR, Fung T, Hatfield J, McNeil DA, Sauve R. Risk factors for positional plagiocephaly and appropriate time frames for prevention messaging. Paediatr Child Health. 2014;19:423–427. doi: 10.1093/pch/19.8.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peitsch WK, Keefer CH, LaBrie RA, Mulliken JB. Incidence of cranial asymmetry in healthy newborns. Pediatrics. 2002;110 doi: 10.1542/peds.110.6.e72. [DOI] [PubMed] [Google Scholar]
- 13.Bialocerkowski AE, Vladusic SL, Wei Ng C. Prevalence, risk factors, and natural history of positional plagiocephaly: a systematic review. Dev Med Child Neurol. 2008;50:577–586. doi: 10.1111/j.1469-8749.2008.03029.x. [DOI] [PubMed] [Google Scholar]
- 14.Losee JE, Mason AC, Dudas J, Hua LB, Mooney MP. Nonsynostotic occipital plagiocephaly: factors impacting onset, treatment, and outcomes. Plast Reconstr Surg. 2007;119:1866–1873. doi: 10.1097/01.prs.0000259190.56177.ca. [DOI] [PubMed] [Google Scholar]
- 15.Shweikeh F, Nuno M, Danielpour M, Krieger MD, Drazin D. Positional plagiocephaly: an analysis of the literature on the effectiveness of current guidelines. Neurosurg Focus. 2013;35 doi: 10.3171/2013.8.FOCUS13261. [DOI] [PubMed] [Google Scholar]
- 16.Boere-Boonekamp MM, van der Linden-Kuiper LL. Positional preference: prevalence in infants and follow-up after two years. Pediatrics. 2001;107:339–343. doi: 10.1542/peds.107.2.339. [DOI] [PubMed] [Google Scholar]
- 17.Branch LG, Kesty K, Krebs E, Wright L, Leger S, David LR. Deformational plagiocephaly and craniosynostosis: trends in diagnosis and treatment after the „back to sleep“ campaign. J Craniofac Surg. 2015;26:147–150. doi: 10.1097/SCS.0000000000001401. [DOI] [PubMed] [Google Scholar]
- 18.Linz C, Collmann H, Meyer-Marcotty P, et al. Occipital plagiocephaly: unilateral lambdoid synostosis versus positional plagiocephaly. Arch Dis Child. 2015;100:152–157. doi: 10.1136/archdischild-2014-305944. [DOI] [PubMed] [Google Scholar]
- 19.Schweitzer T, Bohm H, Meyer-Marcotty P, Collmann H, Ernestus RI, Krauss J. Avoiding CT scans in children with single-suture craniosynostosis. Childs Nerv Syst. 2012;28:1077–1082. doi: 10.1007/s00381-012-1721-0. [DOI] [PubMed] [Google Scholar]
- 20.Argenta L, David L, Thompson J. Clinical classification of positional plagiocephaly. J Craniofac Surg. 2004;15:368–372. doi: 10.1097/00001665-200405000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Kluba S, Rosskopf F, Kraut W, et al. Malocclusion in the primary dentition in children with and without deformational plagiocephaly. Clin Oral Investig. 2016;20:2395–2401. doi: 10.1007/s00784-016-1716-4. [DOI] [PubMed] [Google Scholar]
- 22.Mortenson PA, Steinbok P. Quantifying positional plagiocephaly: reliability and validity of anthropometric measurements. J Craniofac Surg. 2006;17:413–419. doi: 10.1097/00001665-200605000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Meyer-Marcotty P, Bohm H, Linz C, et al. Head orthesis therapy in infants with unilateral positional plagiocephaly: an interdisciplinary approach to broadening the range of orthodontic treatment. J Orofac Orthop. 2012;73:151–165. doi: 10.1007/s00056-011-0070-z. [DOI] [PubMed] [Google Scholar]
- 24.Pokora R, Krille L, Dreger S, et al. Computed tomography in Germany. Results and insights from a cohort study and health insurance data (AOK). Dtsch Arztebl Int. 2016;113:721–728. doi: 10.3238/arztebl.2016.0721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hutchison BL, Stewart AW, Mitchell EA. Deformational plagiocephaly: a follow-up of head shape, parental concern and neurodevelopment at ages 3 and 4 years. Arch Dis Child. 2011;96:85–90. doi: 10.1136/adc.2010.190934. [DOI] [PubMed] [Google Scholar]
- 26.Weissler EH, Sherif RD, Taub PJ. An evidence-based approach to nonsynostotic plagiocephaly. Plast Reconstr Surg. 2016;138:682e–689e. doi: 10.1097/PRS.0000000000002543. [DOI] [PubMed] [Google Scholar]
- 27.Roby BB, Finkelstein M, Tibesar RJ, Sidman JD. Prevalence of positional plagiocephaly in teens born after the „Back to Sleep“ campaign. Otolaryngol Head Neck Surg. 2012;146:823–828. doi: 10.1177/0194599811434261. [DOI] [PubMed] [Google Scholar]
- 28.Aarnivala H, Vuollo V, Harila V, Heikkinen T, Pirttiniemi P, Valkama AM. Preventing deformational plagiocephaly through parent guidance: a randomized, controlled trial. Eur J Pediatr. 2015;174:1197–1208. doi: 10.1007/s00431-015-2520-x. [DOI] [PubMed] [Google Scholar]
- 29.Persing J, James H, Swanson J, et al. Prevention and management of positional skull deformities in infants American Academy of Pediatrics Committee on Practice and Ambulatory Medicine, Section on Plastic Surgery and Section on Neurological Surgery. Pediatrics. 2003;112:199–202. doi: 10.1542/peds.112.1.199. [DOI] [PubMed] [Google Scholar]
- 30.Laughlin J, Luerssen TG, Dias MS, Surgery CoPAMSoN. Prevention and management of positional skull deformities in infants. Pediatrics. 2011;128:1236–1241. doi: 10.1542/peds.2011-2220. [DOI] [PubMed] [Google Scholar]
- 31.Steinberg JP, Rawlani R, Humphries LS, Rawlani V, Vicari FA. Effectiveness of conservative therapy and helmet therapy for positional cranial deformation. Plast Reconstr Surg. 2015;135:833–842. doi: 10.1097/PRS.0000000000000955. [DOI] [PubMed] [Google Scholar]
- 32.van Vlimmeren LA, van der Graaf Y, Boere-Boonekamp MM, L‘Hoir MP, Helders PJ, Engelbert RH. Effect of pediatric physical therapy on deformational plagiocephaly in children with positional preference: a randomized controlled trial. Arch Pediatr Adolesc Med. 2008;162:712–728. doi: 10.1001/archpedi.162.8.712. [DOI] [PubMed] [Google Scholar]
- 33.Wilbrand JF, Seidl M, Wilbrand M, et al. A prospective randomized trial on preventative methods for positional head deformity: physiotherapy versus a positioning pillow. J Pediatr. 2013;162:1216–1221. doi: 10.1016/j.jpeds.2012.11.076. [DOI] [PubMed] [Google Scholar]
- 34.Kaplan SL, Coulter C, Fetters L. Physical therapy management of congenital muscular torticollis: an evidence-based clinical practice guideline: from the Section on Pediatrics of the American Physical Therapy Association. Pediatr Phys Ther. 2013;25:348–394. doi: 10.1097/PEP.0b013e3182a778d2. [DOI] [PubMed] [Google Scholar]
- 35.Cabrera-Martos I, Valenza MC, Valenza-Demet G, Benitez-Feliponi A, Robles-Vizcaino C, Ruiz-Extremera A. Effects of manual therapy on treatment duration and motor development in infants with severe nonsynostotic plagiocephaly: a randomised controlled pilot study. Childs Nerv Syst. 2016;32:2211–2217. doi: 10.1007/s00381-016-3200-5. [DOI] [PubMed] [Google Scholar]
- 36.Jung MW, Landenberger M, Jung T, Lindenthal T, Philippi H. Vojta therapy and neurodevelopmental treatment in children with infantile postural asymmetry: a randomised controlled trial. J Phys Ther Sci. 2017;29:301–306. doi: 10.1589/jpts.29.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Freudlsperger C, Bodem JP, Kargus S, Castrillon-Oberndorfer G, Hoffman J, Engel M. The incidence of complications associated with molding helmet therapy: an avoidable risk in the treatment of positional head deformities? J Craniofac Surg. 2015;26:e299–e302. doi: 10.1097/SCS.0000000000001649. [DOI] [PubMed] [Google Scholar]
- 38.van Wijk RM, van Vlimmeren LA, Groothuis-Oudshoorn CG, van der Ploeg CP, Ijzerman MJ, Boere-Boonekamp MM. Helmet therapy in infants with positional skull deformation: randomised controlled trial. BMJ. 2014;348 doi: 10.1136/bmj.g2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Freudlsperger C, Steinmacher S, Saure D, et al. Impact of severity and therapy onset on helmet therapy in positional plagiocephaly. J Craniomaxillofac Surg. 2016;44:110–115. doi: 10.1016/j.jcms.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 40.Martiniuk A, Jacob J, Faruqui N, Yu W. Positional plagiocephaly reduces parental adherence to SIDS guidelines and inundates the health system. Child Care Health Dev. 2016;42:941–950. doi: 10.1111/cch.12386. [DOI] [PubMed] [Google Scholar]
- E1.van Vlimmeren LA, van der Graaf Y, Boere-Boonekamp MM, L‘Hoir MP, Helders PJ, Engelbert RH. Risk factors for deformational plagiocephaly at birth and at 7 weeks of age: a prospective cohort study. Pediatrics. 2007;119:e408–e418. doi: 10.1542/peds.2006-2012. [DOI] [PubMed] [Google Scholar]
- E2.Bialocerkowski AE, Vladusic SL, Wei Ng C. Prevalence, risk factors, and natural history of positional plagiocephaly: a systematic review. Dev Med Child Neurol. 2008;50:577–586. doi: 10.1111/j.1469-8749.2008.03029.x. [DOI] [PubMed] [Google Scholar]
- E3.Spermon J, Spermon-Marijnen R, Scholten-Peeters W. Clinical classification of deformational plagiocephaly according to Argenta: a reliability study. J Craniofac Surg. 2008;19:664–668. doi: 10.1097/SCS.0b013e31816ae3ec. [DOI] [PubMed] [Google Scholar]
- E4.Farkas LG. Accuracy of anthropometric measurements: past, present, and future. Cleft Palate Craniofac J. 1996;33:10–18. doi: 10.1597/1545-1569_1996_033_0010_aoampp_2.3.co_2. discussion 9-22. [DOI] [PubMed] [Google Scholar]
- E5.Moss SD. Nonsurgical, nonorthotic treatment of occipital plagiocephaly: what is the natural history of the misshapen neonatal head? J Neurosurg. 1997;87:667–670. doi: 10.3171/jns.1997.87.5.0667. [DOI] [PubMed] [Google Scholar]
- E6.Mortenson PA, Steinbok P. Quantifying positional plagiocephaly: reliability and validity of anthropometric measurements. J Craniofac Surg. 2006;17:413–419. doi: 10.1097/00001665-200605000-00005. [DOI] [PubMed] [Google Scholar]
- E7.Loveday BP, de Chalain TB. Active counterpositioning or orthotic device to treat positional plagiocephaly? J Craniofac Surg. 2001;12:308–313. doi: 10.1097/00001665-200107000-00003. [DOI] [PubMed] [Google Scholar]
- E8.Regelsberger J, Delling G, Tsokos M, et al. High-frequency ultrasound confirmation of positional plagiocephaly. J Neurosurg. 2006;105:413–417. doi: 10.3171/ped.2006.105.5.413. [DOI] [PubMed] [Google Scholar]
- E9.Kordestani RK, Patel S, Bard DE, Gurwitch R, Panchal J. Neurodevelopmental delays in children with deformational plagiocephaly. Plast Reconstr Surg. 2006;117:207–218. doi: 10.1097/01.prs.0000185604.15606.e5. [DOI] [PubMed] [Google Scholar]
- E10.Speltz ML, Collett BR, Stott-Miller M, et al. Case-control study of neurodevelopment in deformational plagiocephaly. Pediatrics. 2010;125:e537–e542. doi: 10.1542/peds.2009-0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E11.Feijen M, Franssen B, Vincken N, van der Hulst RR. Prevalence and consequences of positional plagiocephaly and brachycephaly. J Craniofac Surg. 2015;26:e770–e773. doi: 10.1097/SCS.0000000000002222. [DOI] [PubMed] [Google Scholar]
- E12.Wilbrand JF, Lautenbacher N, Pons-Kuhnemann J, et al. Treated versus untreated positional head deformity. J Craniofac Surg. 2016;27:13–18. doi: 10.1097/SCS.0000000000002167. [DOI] [PubMed] [Google Scholar]
- E13.Hutchison BL, Stewart AW, de Chalain TB, Mitchell EA. A randomized controlled trial of positioning treatments in infants with positional head shape deformities. Acta Paediatr. 2010;99:1556–1560. doi: 10.1111/j.1651-2227.2010.01872.x. [DOI] [PubMed] [Google Scholar]