Abstract
Background:
Self-care is assumed to benefit health outcomes in patients with chronic heart failure (HF), but the evidence is conflicting for health-related quality of life (HRQOL). The aim of this study was to examine the association of (changes in) self-care with HRQOL while adjusting for psychological distress.
Methods:
In total, 459 patients (mean age = 66.1 ± 10.5 years, 73% male) with chronic HF completed questionnaires at baseline and at 6, 12 and 18 months of follow-up. Self-care and HF-specific HRQOL were quantified with the European Heart Failure Self-care Behaviour scale and the Minnesota Living with Heart Failure Questionnaire.
Results:
Using general linear models, multivariable between-subject (estimate = –0.14, p = 0.005) and no within-subject effects of self-care were found for better HRQOL over time. Associations between self-care and HRQOL were fully explained by depression (estimate = 1.77, p < 0.001). Anxiety (estimate = 4.49, p < 0.001) and Type D personality (estimate = 13.3, p < 0.001) were associated with poor HRQOL, but only partially accounted for the relationship between self-care and emotional HRQOL.
Conclusions:
Self-care was prospectively associated with better disease-specific HRQOL in patients with HF, which was fully accounted for by depression, and partially accounted for by anxiety and Type D personality. Changes in self-care within a person did not affect HRQOL. Psychological distress should be considered in future efforts to address self-care and HRQOL.
Keywords: Anxiety, depression, heart failure, quality of life, self-care, stress, psychological, Type D personality
Introduction
Chronic heart failure (HF) is a clinical syndrome affecting 2–3% of the global population.1,2 It is associated with frequent hospital admissions, imposing a vast burden on industrialised countries.3,4 Standard treatment of HF is aimed at prolonging life by maintaining physiological stability.1 It usually involves a complex regimen of daily self-care behaviours, including pharmacological therapy, symptom monitoring and lifestyle modifications.
Health-related quality of life (HRQOL) is profoundly impaired in patients with HF.5 Many patients suffer from other conditions, including diabetes, anaemia and renal disease,6 but also from psychological distress.7,8 Patients with HF are prone to experiencing disabling psychosocial consequences of their burdening condition, such as social isolation and fear.9 Several demographic and clinical factors are known to impact HRQOL, such as younger age, increased disease severity and poor functional capacity.10
It seems likely that self-care would benefit HRQOL, as it is targeted at reducing HF symptoms in order to improve the patient’s physical condition. However, findings from previous, primarily cross-sectional and small studies have yielded inconsistent results,11–14 also when examining the effects of self-care interventions on HRQOL.15 We therefore investigated the longitudinal association of HF self-care and HRQOL in a large cohort of patients with chronic HF. We extend previous work by examining whether differences in self-care within and between patients were related to HRQOL over time. Furthermore, as psychological distress adversely relates to HRQOL,7,11 we explored whether depression, anxiety and Type D personality explained potential relationships between self-care and HRQOL.
Methods
Patients and procedure
This study is part of the Elisabeth-TweeSteden Heart Failure Cohort Study. Consecutive patients attending the outpatient HF clinic of the Elisabeth-TweeSteden teaching hospital (Tilburg, The Netherlands) were approached for participation in a longitudinal study with five measurement occasions over a total follow-up period of 18 months.16,17 Exclusion criteria comprised: diastolic HF; age ⩾80 years; a myocardial infarction or hospitalisation in the month prior to inclusion; a life-threatening disease with a life expectancy <1 year; serious psychiatric illness except for mood disorders; or insufficient understanding of and fluency in the Dutch language. Patients were informed about the study and recruited by their cardiologist or specialised HF nurse. If patients agreed to participate, they were called in the same week to arrange a baseline appointment. At baseline, patients completed a psychological survey at home, which was returned in a self-addressed envelope. At 6, 12 and 18 months of follow-up, patients were contacted to complete the psychological survey again. In case of missing items, patients were contacted by phone or email in an attempt to obtain the missing answers. If the questionnaire was not returned within 2 weeks, patients received a reminder telephone call or letter. Of 570 eligible patients, 465 agreed to participate (81%) and 459 patients returned the baseline questionnaire. Written informed consent was obtained from all patients. The study protocol was approved by the institutional medical ethics review boards of all participating hospitals.
Measures
Self-care
The nine-item European Heart Failure Self-care Behaviour scale (EHFScB-9)18 was administered in order to assess self-care at baseline and 6, 12 and 18 months of follow-up. Items were rated on a five-point Likert scale from 1 (‘I completely agree’) to 5 (‘I completely disagree’). To calculate sum scores, item scores were reversed, with a possible range of 9–45. Raw sum scores were transformed into standardised scores from 0 to 100, with higher scores reflecting better self-care.19 This includes a four-item ‘consulting behaviour’ subscale that measures whether patients contact their physician in case of a sudden increase of the following symptoms: shortness of breath, ankle swelling, weight gain or fatigue. The remaining items assess how patients judge their adherence to the most commonly recommended self-care behaviours: daily weight monitoring, limiting fluids, low-sodium diet, regular exercise and medication adherence. The internal consistency of the total self-care and its consultation scale were acceptable (Cronbach’s α = 0.79) and good (Cronbach’s α = 0.87) at baseline, respectively. For descriptive statistical purposes, we split the person-mean of self-care (i.e. an individual’s self-care scores averaged over all time points) at the median in order to denote low and high self-care, as there are no well-validated cut-off values published in the literature.
Health-related quality of life
The Minnesota Living with Heart Failure (MLWHF) questionnaire was administered in order to assess HF-specific HRQOL at all time points.20,21 The MLWHF is designed to assess the effects of HF symptoms, functional limitations and psychological distress on the patient’s quality of life. Twenty-one items are answered on a six-point Likert scale ranging from 0 to 5. Higher scores indicate worse HF-specific HRQOL, with a difference of five denoting a clinically relevant change.22 This provides a total score that includes additional social, HF-specific and healthcare-related items, as well as a physical and emotional dimensional subscale score.
Depression
The 21-item Beck Depression Inventory (BDI)23 was used in order to assess depressive symptomatology. This is a well-validated self-report measure and has been found to be reliable for measuring depressive symptomatology in patients with chronic HF.24 Each item is rated on a 0–3 scale. A total score is obtained by the sum of all items. We performed three assessments of depressive symptoms at baseline and at the 12- and 18-month follow-up visits. Internal consistency was good at all three measurement occasions, with Cronbach’s α being 0.86, 0.83 and 0.82, respectively.
Anxiety
Symptoms of anxiety were assessed with the two anxiety items (i.e. tension and restlessness) of the Symptoms of Anxiety–Depression index (SAD4), which has been shown to detect an increased risk of anxiety disorder in cardiac patients.25 Items are answered on a five-point Likert scale with a range from 0 (‘not at all’) to 4 (‘very much’). The internal consistency was high in this study (Cronbach’s α range = 0.87–0.92).
Type D personality
The 14-item Type D Scale (DS14) was used in order to assess Type D personality,26 which is defined as the combination of the negative affectivity (NA) and social inhibition (SI) personality traits. Individuals with a Type D personality tend to experience negative emotions across time and situations, and have the tendency of not expressing themselves in social interactions because of fear of rejection or disapproval by others. Type D personality has been shown to independently predict HRQOL27 and self-care28 in patients with HF. Items are answered on a five-point Likert scale, ranging from 0 (‘false’) to 4 (‘true’). The DS14 consists of two seven-item subscales – NA and SI – which are time-stable and internally consistent (Cronbach’s α = 0.88/0.86).26,29 In the current study, Cronbach’s α was .87 for NA and .84 for SI. The standardised cut-off score of ⩾10 on both subscales was used in order to classify individuals with a Type D personality.26
Sociodemographic and clinical covariates
We included demographics (i.e. age, gender, educational level and living alone), cardiac history and comorbidities. We dichotomised education into two groups (i.e. 8 years or less vs. more than 8 years) for presentation purposes. We did not include New York Heart Association (NYHA) functional class, as its criteria largely overlap with the items of the MLWHF questionnaire. Left ventricular ejection fraction (LVEF) was also not included as a covariate because the majority of studies have found no association between (LVEF) and HRQOL.10,11
Statistical analysis
We examined the course of total, physical and emotional HRQOL over all measurement occasions using pairwise comparisons. We stratified the course of HRQOL for above- and below-median levels of total self-care. In order to analyse the effects of the level (between subjects) and change (within subjects) of self-care over time on the course of HRQOL, we conducted linear mixed modelling analyses (using maximum likelihood [ML] estimation and an unstructured covariance matrix). To this end, we calculated the person-mean of self-care over the measurement occasions in order to address a between-subjects effect. Then, we calculated the deviations from this person-mean at each time point in order to obtain information on the person-specific change in self-care so as to address within-subjects effects. These two variables constituted our independent variables.
Three separate analyses were performed for total, physical and emotional HRQOL as outcome measures. Separate analyses were performed for total self-care and for the consultation behaviour subscale.13 In step 1, the self-care variables (person-mean and deviation) were entered (unadjusted model). In step 2, we adjusted the models for demographic and clinical covariates. In a final step, we separately added depression, anxiety and Type D personality. All illness-related and psychological covariates were time-varying, except for demographic variables and Type D personality. Estimates were reported, which represent the non-standardised regression coefficients of the dependent variable when the independent variable increases by one unit. Analyses were performed with SPSS 20.0 for Windows (IBM SPSS Statistics for Windows, version 20.0; Armonk, NY: IBM Corp. USA). Tests were two-tailed with a p-value < 0.05 indicating statistical significance.
Results
Sample characteristics
Baseline characteristics are presented in Table 1. Patients with below-median scores of total self-care received less education. They demonstrated less favourable health behaviours (reduced physical activity and higher body mass index). The below-median self-care patients more often had a cardiac history. Angiotensin-related medication and loop diuretics were less likely to be prescribed to the below-median self-care group. Those who were low in self-care reported increased symptoms of depression and anxiety. There were some trend associations as well, suggesting that the below-median self-care patients lived alone a bit more often. They also tended to have larger comorbidity burdens, as well as fewer implanted cardioverter defibrillators or pacemakers. Type D personality tended to be more prevalent in the low self-care group, although this was not a significant difference (p = 0.08).
Table 1.
Baseline patient characteristics (in percentages, unless stated otherwise).
| Characteristic | Total (n = 459) | Low self-care (n = 231) | High self-care (n = 228) | Test statistic | p-value |
|---|---|---|---|---|---|
| Demographics | |||||
| Female gender | 27% (124) | 27% (63) | 27% (61) | 0.02 | 0.90 |
| Age in years, mean (SD) | 66.1 (10.5) | 66.4 (10.8) | 65.9 (10.3) | 0.29 | 0.59 |
| Low education | 34% (157) | 42% (97) | 26% (60) | 13.04 | <0.001 |
| Living with partner | 72% (330) | 69% (157) | 76% (173) | 3.05 | 0.08 |
| Clinical characteristics | |||||
| NYHA class III/IV | 39% (179) | 39% (90) | 39% (89) | 0.00 | 0.98 |
| LVEF, mean % (SD) | 31.0 (6.9) | 30.9 (6.8) | 31.1 (7.0) | 0.12 | 0.73 |
| Ischaemic aetiology | 55% (251) | 59% (136) | 50% (115) | 4.48 | 0.34 |
| Cardiac history | 58% (266) | 63% (145) | 53% (121) | 4.43 | 0.04 |
| Implanted ICD | 6% (28) | 4% (9) | 8% (19) | 3.94 | 0.05 |
| Implanted pacemaker | 12% (53) | 9% (21) | 14% (32) | 2.81 | 0.09 |
| CCI score, mean (SD) | 2.9 (1.6) | 3.0 (1.7) | 2.7 (1.5) | 3.32 | 0.07 |
| Cardiac rehabilitation | 9% (43) | 9% (20) | 10% (23) | 0.25 | 0.62 |
| Health behaviour characteristics | |||||
| BMI, mean (SD) | 28.0 (5.5) | 28.6 (6.0) | 27.4 (4.8) | 5.56 | 0.02 |
| Physically active | 56% (255) | 45% (102) | 67% (153) | 23.14 | <0.001 |
| Smoking | 24% (110) | 27% (62) | 21% (48) | 2.27 | 0.13 |
| Medication | |||||
| Aspirin | 40% (185) | 43% (100) | 37% (85) | 1.72 | 0.19 |
| β-blocker | 69% (318) | 66% (152) | 73% (166) | 2.44 | 0.12 |
| ACEi/ARB | 85% (390) | 81% (186) | 90% (204) | 7.20 | 0.007 |
| Diuretics | |||||
| Loop diuretic | 70% (323) | 65% (150) | 76% (173) | 6.59 | 0.01 |
| Thiazide | 5% (23) | 5% (12) | 5% (11) | 0.03 | 0.86 |
| Aldosterone receptor antagonist | 22% (102) | 23% (53) | 22% (49) | 0.12 | 0.73 |
| Other potassium saving | 5% (21) | 3% (7) | 6% (14) | 2.54 | 0.11 |
| Psychological characteristics | |||||
| Depression, mean (SD) | 9.0 (6.8) | 10.1 (7.3) | 7.9 (6.1) | 12.8 | <0.001 |
| Anxiety, mean (SD) | 1.4 (1.8) | 1.7 (1.0) | 1.2 (1.6) | 8.27 | 0.004 |
| Type D personality | 20% (89) | 23% (52) | 16% (37) | 3.06 | 0.08 |
| Psychosocial counselling | 7% (33) | 8% (19) | 6% (14) | 0.79 | 0.37 |
| Psychotropic medication | 13% (61) | 13% (30) | 14% (31) | 0.04 | 0.85 |
Bold: significant at p < 0.05.
ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; BMI: body mass index; CCI: Charlson Comorbidity Index; ICD: implanted cardioverter defibrillator; LVEF: left ventricular ejection fraction; NYHA: New York Heart Association.
Attrition
In total, 56 patients (13%; of whom 22 were deceased) dropped out at the 12-month measurement occasion, while another 20 patients (4%; of whom seven were deceased) dropped out at the 18-month measurement occasion. Patients who dropped out were more likely to have a worse illness severity (NYHA class III, χ2 = 12.1, p < 0.001) and to have a lower educational level (χ2 = 5.7, p = 0.02). Patients who dropped out at 18 months were more likely to have an elevated Charlson Comorbidity Index (CCI) score at 12 months (F = 8.47, p = 0.004; no differences at earlier measurement occasions). There were no differences in self-care between completers and dropouts. Patients who dropped out did have significantly worse HRQOL during the measurement occasions before their dropping out (inclusion: F = 5.20, p = 0.02; 6-month follow-up: F = 7.50, p = 0.006) and had increased levels of depression (F = 4.45, p = 0.04) and anxiety (F = 5.06, p = 0.03) at baseline, but not at intermediate follow-up occasions.
HRQOL over time
HRQOL differed over time (F = 3.96, p = 0.01), with pairwise comparisons showing that HRQOL was, on average, better at all follow-up occasions than at baseline (p < 0.04; Figure 1). At 1 year, HRQOL tended to be better than at 6 months (p = 0.05), while at 18 months, HRQOL was not significantly different from HRQOL at the 12-month follow-up. Average differences were smaller than five points (between 1.6 and 3.0). Physical and emotional subscale scores showed a main effect of time (F = 2.84, p = 0.04; F = 9.51, p < 0.001, respectively), although the pattern of differences was different. Physical HRQOL had a wave form, with patients doing better at 1 year of follow-up and moving back towards baseline levels at 18 months of follow-up. Emotional HRQOL was worse at baseline compared to at all three other follow-up occasions.
Figure 1.
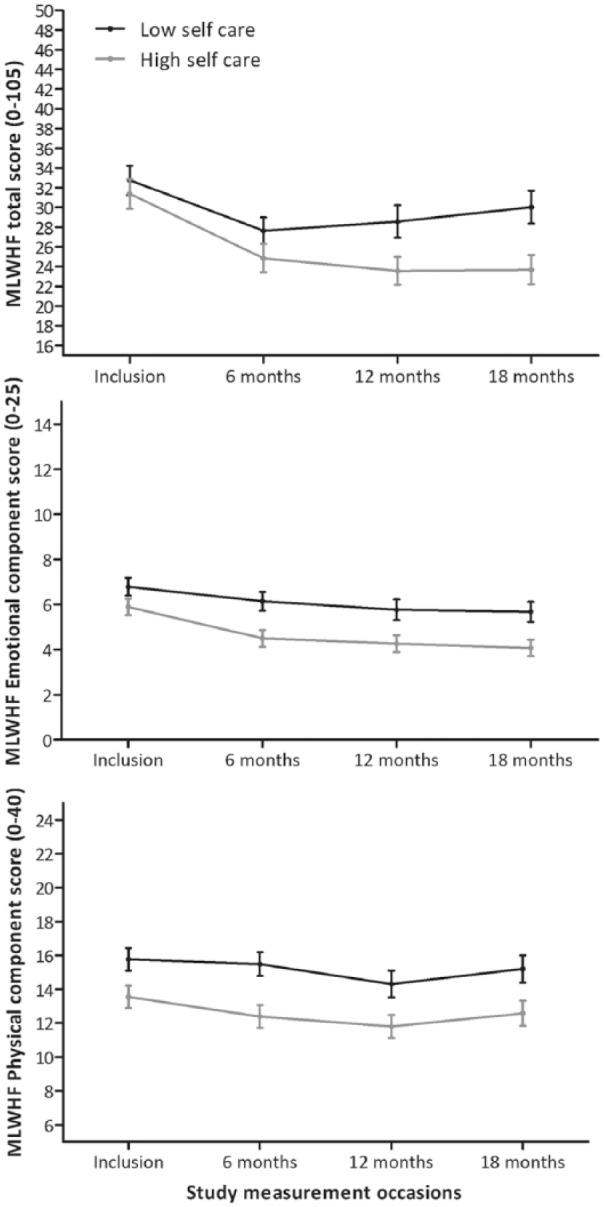
Health-related quality of life total, emotional and physical component scores over time and stratified by self-care categories.
Higher MLWHF scores denote worse health-related quality of life. Self-care groups were based on the median split of the longitudinal person-mean.
MLWHF: Minnesota Living with Heart Failure.
More patients in the above-median self-care group (42%) showed a clinically relevant improvement in HRQOL of five points or more over the first 6 months compared to the below-median self-care group (32%), which included a larger number of patients who significantly deteriorated (37% vs. 29%). At 12 months, there were more deteriorating patients in the low self-care group (31% vs. 22%). The percentage of improving patients was equal for low and high self-care groups. At 18 months, the differences between low and high self-care groups altered, with a similar percentage of clinically relevant deterioration as compared to baseline in HRQOL (32 vs. 27%) and more divergent percentages of patients who were clinically improving (32% vs. 42%).
Self-care and HRQOL
As a first step, we entered the person mean of self-care and the deviation from this person-mean over time in order to assess between-subjects and within-subjects effects of self-care on HRQOL total and component scores. The results showed a significant between-subjects effect of self-care (F = 12.61, p < 0.001), but no significant within-subjects effect (F = 0.32, p = 0.57). Table 2 shows the estimates of the individual parameters, representing non-standardised regression coefficients of the dependent variable when the independent variable increases by one unit. Better mean self-care was associated with better HRQOL over time, while within-person variation in self-care across time was unrelated to the level of HRQOL across time. After adjusting for established covariates (step 2), the relationship between self-care and HRQOL remained similar. Low education level was a significant predictor of worse HRQOL. In the third and final step, we included psychological distress in three different sub-models for depression, anxiety and Type D personality. All three psychological distress variables were strongly related to total HRQOL. Examining the difference in self-care estimates between models 2 and 3 would give an indication of how much of the effect of self-care on HRQOL could be explained by psychological stress. Depression shared almost all variance with self-care, as the estimate for the grand mean of self-care (between subjects) was reduced to nearly zero. Anxiety overlapped partly with self-care in explaining variance in HRQOL over time, indicating that self-care affected HRQOL independently of anxiety. Type D personality overlapped the least with self-care in explaining variance in HRQOL over time, with the estimate of self-care largely remaining similar to the estimate in the prior step.
Table 2.
Results from multivariable linear mixed models for self-care total score.
| HRQOL – total |
HRQOL – physical |
HRQOL – emotional |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | t-value | p-value | Estimate | t-value | p-value | Estimate | t-value | p-value | ||
| Time (6-month steps) | −1.12 | −3.22 | 0.001 | −0.25 | −1.36 | 0.18 | −0.45 | −3.90 | <0.001 | |
| Step 1: unadjusted model | ||||||||||
| Time (6-month steps) | −1.10 | −3.16 | 0.002 | −0.34 | −2.11 | 0.04 | −0.46 | −4.61 | <0.001 | |
| Self-care between | −0.17 | −3.37 | 0.001 | −0.09 | −3.66 | <0.001 | −0.03 | −2.29 | 0.02 | |
| Self-care within | −0.04 | −1.01 | 0.31 | −0.02 | −1.33 | 0.18 | 0.002 | 0.18 | 0.85 | |
| Step 2: covariate adjusted model | ||||||||||
| Time (6-month steps) | −1.19 | −3.41 | 0.001 | −0.40 | −2.46 | 0.01 | −0.47 | −4.61 | <0.001 | |
| Self-care between | −0.14 | −2.81 | 0.005 | −0.07 | −2.98 | 0.003 | −0.03 | −1.95 | 0.052 | |
| Self-care within | −0.04 | −1.01 | 0.31 | −0.02 | 1.37 | 0.17 | 0.002 | 0.20 | 0.84 | |
| Low education | 4.22 | 2.18 | 0.03 | 2.55 | 2.78 | 0.006 | 0.67 | 1.30 | 0.19 | |
| Living alone | 0.30 | 0.17 | 0.87 | 0.81 | 0.95 | 0.35 | 0.02 | 0.04 | 0.97 | |
| Cardiac history | −1.19 | −0.67 | 0.50 | −0.08 | −0.09 | 0.93 | −0.34 | −0.70 | 0.48 | |
| Comorbidity burden | 0.67 | 1.51 | 0.13 | 0.55 | 2.65 | 0.008 | −0.02 | −0.17 | 0.87 | |
| Step 3: complete model (covariate adjusted + psychological variable) | ||||||||||
| A | Self-care between | −0.03 | −0.87 | 0.38 | −0.03 | −1.5 | 0.13 | 0.004 | 0.40 | 0.78 |
| Depression | 1.77 | 18.96 | <0.001 | 0.71 | 15.3 | <0.001 | 0.53 | 22.46 | <0.001 | |
| B | Self-care between | −0.09 | −2.09 | 0.04 | −0.05 | −2.36 | 0.02 | −0.008 | −0.04 | 0.97 |
| Anxiety | 4.49 | 12.87 | <0.001 | 1.76 | 10.55 | <0.001 | 1.59 | 17.52 | <0.001 | |
| C | Self-care between | −0.12 | −2.38 | 0.02 | −0.06 | −2.64 | 0.009 | −0.02 | −1.4 | 0.16 |
| Type D | 13.3 | 6.20 | <0.001 | 4.68 | 4.53 | <0.001 | 4.40 | 8.08 | <0.001 | |
This table shows three prediction models of HRQOL total, physical and emotional scores in an unadjusted model, a covariate-adjusted model and the full model, including psychological predictors. Because of the high correlation between psychological variables, we calculated the third model three times separately for each psychological predictor. Estimates denote the change in the outcome value when the predictor changes by one unit/point.
Bold: significant at p < 0.05 level; italic: p < 0.10.
HRQOL: health-related quality of life.
The physical and emotional subcomponents were less strongly related to self-care than the total score (Table 2). In unadjusted analyses, between-subject differences in self-care were significantly related to difference in physical and emotional HRQOL over time. This effect disappeared for emotional HRQOL in adjusted analyses. Low education level and a larger comorbidity burden were both related to poorer physical but not emotional HRQOL. It was shown that psychological distress was strongly related to poorer physical and emotional HRQOL. Higher self-care remained a predictor for better physical HRQOL when anxiety and Type D personality were included. Self-care no longer predicted emotional HRQOL when psychological distress variables were included.
Consultation behaviour and HRQOL
Results were similar for consultation behaviour. We found a main effect of between-subject differences (F = 16.74, p < 0.001), but no within-subject effects on consultation behaviour (F = 1.25, p = 0.26). These main effects were similar for the physical (F = 17.55, p < 0.001; F = 1.56, p = 0.21) and emotional HRQOL (F = 8.95, p = 0.003; F = 0.001, p = 0.97) subcomponents. Table 3 shows the estimates of the individual parameters, representing non-standardised regression coefficients of the dependent variable when the independent variable increases by one unit. Between-subject differences in consultation behaviour affected levels of HRQOL in unadjusted analyses; poorer consultation behaviour was associated with worse HRQOL, and this remained significant and of similar size when adjusting for demographic and clinical covariates. Within-subject variation of reported consultation behaviour over time was unrelated to HRQOL. When considering psychological distress, poorer consultation behaviour remained a predictor for poorer HRQOL when anxiety and Type D personality were included. Depression reduced the effect of consultation behaviour to a non-significant level. With respect to the physical and emotional subcomponents, similar patterns appeared as were observed for total self-care.
Table 3.
Results from multivariable linear mixed models for the consultation behaviour subscale score.
|
HRQOL – total
|
HRQOL – physical
|
HRQOL – emotional
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | t-value | p-value | Estimate | t-value | p-value | Estimate | t-value | p-value | ||
| Time (6-month steps) | −1.12 | −3.22 | 0.001 | −0.25 | −1.36 | 0.18 | −0.45 | −3.90 | <0.001 | |
| Step 1: unadjusted model | ||||||||||
| Time (6-month steps) | −1.10 | −3.17 | 0.002 | −0.34 | −2.12 | 0.04 | −0.46 | −4.63 | <0.001 | |
| Consultation between | −0.14 | −4.03 | <0.001 | −0.07 | −4.16 | <0.001 | −0.02 | −2.81 | 0.005 | |
| Consultation within | −0.01 | −0.58 | 0.56 | −0.01 | −0.93 | 0.35 | 0.008 | 1.16 | 0.25 | |
| Step 2: covariate adjusted model | ||||||||||
| Time (6-month steps) | −1.20 | −3.42 | 0.001 | −0.40 | −2.67 | 0.01 | −0.47 | −4.63 | <0.001 | |
| Consultation between | −0.12 | −3.56 | <0.001 | −0.06 | −3.58 | <0.001 | −0.02 | −2.53 | 0.01 | |
| Consultation within | −0.01 | −0.56 | 0.58 | −0.01 | −0.92 | 0.36 | 0.008 | 1.16 | 0.25 | |
| Low education | 4.12 | 2.14 | 0.033 | 2.52 | 2.77 | 0.006 | 0.64 | 1.27 | 0.21 | |
| Living alone | 0.17 | 0.10 | 0.93 | 0.76 | 0.89 | 0.38 | −0.01 | −0.03 | 0.98 | |
| Cardiac history | −1.26 | −0.72 | 0.48 | −0.13 | −0.15 | 0.88 | −0.34 | −0.70 | 0.47 | |
| Comorbidity burden | 0.67 | 1.51 | 0.13 | 0.55 | 2.63 | 0.009 | −0.02 | −0.14 | 0.88 | |
| Step 3: complete model (covariate adjusted + psychological variable) | ||||||||||
| A | Consultation between | −0.05 | −1.93 | 0.054 | −0.03 | −2.30 | 0.02 | −0.003 | −0.48 | 0.63 |
| Depression | 1.75 | 18.89 | <0.001 | 0.70 | 15.28 | <0.001 | 0.53 | 22.37 | <0.001 | |
| B | Consultation between | −0.08 | −2.84 | 0.005 | −0.04 | −2.95 | 0.003 | −0.009 | −1.24 | 0.22 |
| Anxiety | 4.47 | 12.82 | <0.001 | 1.76 | 10.51 | <0.001 | 1.58 | 17.40 | <0.001 | |
| C | Consultation between | −0.10 | −3.12 | 0.002 | −0.05 | −3.24 | 0.001 | −0.02 | −1.96 | 0.050 |
| Type D | 13.1 | 6.14 | <0.001 | 4.62 | 4.48 | <0.001 | 4.35 | 7.99 | <0.001 | |
This table shows three prediction models of HRQOL total, physical and emotional scores in an unadjusted model, a covariate-adjusted model and the full model, including psychological predictors. Because of the high correlation between psychological variables, we calculated the third model three times separately for each psychological predictor. Estimates denote the change in the outcome value when the predictor changes by one unit/point.
Bold: significant at p < 0.05 level; italic: p < 0.10.
HRQOL: health-related quality of life.
Discussion
The current study examined the longitudinal association of self-care and HRQOL over a follow-up period of 18 months in a cohort of 459 patients with chronic HF. The results led to two primary conclusions. First, between-subject differences in self-care, but not within-subject changes in self-care, were associated with HRQOL over time. Lower self-care was associated with poorer overall HRQOL, as well as its physical and emotional subcomponents. Associations were robust since they were hardly affected by established covariates, and were similar for total self-care and the consulting for HF symptoms subscale. Against the background of the inconsistent results published so far, the current study supports the notion that HF self-care is prospectively associated with HRQOL.11–14 Self-care was most relevant in terms of total HRQOL, which involved additional social, HF-specific and healthcare-related items in comparison to the physical and emotional HRQOL subcomponents. This study extends previous work on the impact of psychological factors on cardiac disease30 by showing that psychological distress affected the relationship between HF self-care and HRQOL negatively; either a substantial part or the entire relationship was explained by psychological distress levels. Depression fully explained the relationship between self-care and all HRQOL domains. While anxiety and Type D personality were related to poor HRQOL, they only explained the relationship between self-care and emotional HRQOL. In line with the majority of studies, patients who were low in self-care reported higher levels of psychological distress.31
Depression, anxiety and Type D personality should be considered in future attempts to address self-care and HRQOL. Why depression was more relevant with respect to self-care and physical HRQOL may be explained by its somatic–affective component greatly impacting physical function through direct and indirect effects. Research increasingly shows that somatic rather than cognitive depressive symptoms are related to poorer cardiovascular health (e.g. reduced heart rate variability32), as well as increased mortality risk in HF.16 We hypothesise that somatic–affective symptoms may be of indirect influence on physical HRQOL, preventing patients from performing daily self-care behaviours. Another reason may be negative cognitive bias, which is often present in people with depressive symptoms, leading to poor perceptions of both self-care and HRQOL.33
HRQOL improved over time, but this was not clinically significant (<5 points). Clinically significant deteriorations in HRQOL were observed more often in patients who were low in self-care, especially within the first year of follow-up. Against expectations,13 within-person variations in self-care did not relate to changes in HRQOL. Changes in self-care within a person may perhaps be necessary in order to maintain stable physical and emotional homeostasis, which may therefore not be reflected in significant changes in HRQOL. Further studies are necessary in order to replicate these results and examine such a mechanism. Predictors of poor HRQOL other than self-care were low education level and increasing CCI, which reflects the burden of comorbid conditions and ageing.
Further studies should examine which components of psychological distress serve as potential mediators of the relationship between self-care and HRQOL. Accumulating studies suggest that specific psychological characteristics or dimensions (e.g. anhedonia or somatic symptoms) of depression are more important with respect to specific facets of self-care31 and HRQOL.34 Given the lack of effectiveness of self-care interventions on quality of life,15 interventions that are designed to improve self-care may have to incorporate the role of psychological distress in order to impact HRQOL. This is supported by a meta-analysis showing that face-to-face psychosocial interventions are beneficial to improving quality of life in chronic HF patients.35
There are several limitations of this study. Self-care was assessed by means of self-report, which is subject to systematic biases and may not reflect actual behaviour.36 It would also have been preferable to use a more extensive anxiety measure or interview. The follow-up period of 18 months might have been too short to detect relevant changes in self-care and/or HRQOL. Our findings suggest that psychological distress mediates associations between self-care and HRQOL. This was not addressed with statistical methods, as it diverted from the main aim of the study. We had a small percentage of missing data. As mixed linear effects modelling makes use of ML estimation, imputation of the missing values was not necessary. Finally, given the observational nature of the study design, no conclusions can be drawn regarding the causality of these relationships. The strengths of this study were its large sample size, its longitudinal design with self-care and HRQOL as time-varying variables and its inclusion of psychological distress. In addition, this is the first study to examine whether changes in self-care within a person were associated with changes in HRQOL.
Advances in cardiovascular treatment have led to better survival rates. Consequently, the chronicity of HF continues to increase and the risk for hospitalisation remains high. Clinicians are challenged to minimise the devastating effects of HF on HRQOL, possibly through effective self-care. This study confirmed that self-care was associated with HRQOL, but this relationship was greatly affected by psychological distress, primarily depression. Changes in self-care within a person over time did not contribute to HRQOL. From a clinical perspective, our results emphasise the notion that psychological distress is essential to and underlies the relationship between self-care and HRQOL. Further research will enable us to gain a better understanding of the potential psychological and behavioural factors that contribute to overall HRQOL in patients with chronic HF.
Footnotes
Conflict of interest: The authors declare that there is no conflict of interest.
Funding: Part of this work was supported with a VICI grant (453-04-004) from the Dutch Organization for Scientific Research (NWO) awarded to Prof Dr Johan Denollet.
Implications for practice
- Self-care, but not changes in self-care, is associated with heart failure-related quality of life over time.
- Depressive symptoms are most relevant in determining worse heart failure-related quality of life.
- Minimising psychological distress may benefit both self-care and health-related quality of life.
References
- 1. Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 2008; 29(19): 2388–2442. [DOI] [PubMed] [Google Scholar]
- 2. Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart 2007; 93(9): 1137–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cook C, Cole G, Asaria P, et al. The annual global economic burden of heart failure. Int J Cardiol 2014; 171(3): 368–376. [DOI] [PubMed] [Google Scholar]
- 4. Guha K, McDonagh T. Heart failure epidemiology: European perspective. Curr Cardiol Revi 2013; 9(2): 123–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lesman-Leegte I, Jaarsma T, Coyne JC, et al. Quality of life and depressive symptoms in the elderly: A comparison between patients with heart failure and age- and gender-matched community controls. J Card Fail 2009; 15(1): 17–23. [DOI] [PubMed] [Google Scholar]
- 6. Mentz RJ, Kelly JP, von Lueder TG, et al. Noncardiac comorbidities in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol 2014; 64(21): 2281–2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jaarsma T, Johansson P, Agren S, et al. Quality of life and symptoms of depression in advanced heart failure patients and their partners. Curr Opin Support Palliat Care 2010; 4(4): 233–237. [DOI] [PubMed] [Google Scholar]
- 8. Triposkiadis FK, Skoularigis J. Prevalence and importance of comorbidities in patients with heart failure. Curr Heart Fail Rep 2012; 9(4): 354–362. [DOI] [PubMed] [Google Scholar]
- 9. Jeon YH, Kraus SG, Jowsey T, et al. The experience of living with chronic heart failure: A narrative review of qualitative studies. BMC Health Serv Res 2010; 10: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Juenger J, Schellberg D, Kraemer S, et al. Health related quality of life in patients with congestive heart failure: Comparison with other chronic diseases and relation to functional variables. Heart 2002; 87(3): 235–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nesbitt T, Doctorvaladan S, Southard JA, et al. Correlates of quality of life in rural patients with heart failure. Circ Heart Fail 2014; 7(6): 882–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Seto E, Leonard KJ, Cafazzo JA, et al. Self-care and quality of life of heart failure patients at a multidisciplinary heart function clinic. J Cardiovasc Nurs 2011; 26(5): 377–385. [DOI] [PubMed] [Google Scholar]
- 13. Lee CS, Mudd JO, Hiatt SO, et al. Trajectories of heart failure self-care management and changes in quality of life. Eur J Cardiovasc Nurs 2015; 14(6): 486–494. [DOI] [PubMed] [Google Scholar]
- 14. Buck HG, Dickson VV, Fida R, et al. Predictors of hospitalization and quality of life in heart failure: A model of comorbidity, self-efficacy and self-care. Int J Nurs Stud 2015; 51(11): 1714–1722. [DOI] [PubMed] [Google Scholar]
- 15. Ditewig JB, Blok H, Havers J, et al. Effectiveness of self-management interventions on mortality, hospital readmissions, chronic heart failure hospitalization rate and quality of life in patients with chronic heart failure: A systematic review. Patient Educ Couns 2010; 78(3): 297–315. [DOI] [PubMed] [Google Scholar]
- 16. Schiffer AA, Pelle AJ, Smith OR, et al. Somatic versus cognitive symptoms of depression as predictors of all-cause mortality and health status in chronic heart failure. J Clin Psychiatry 2009; 70(12): 1667–1673. [DOI] [PubMed] [Google Scholar]
- 17. Smith OR, Kupper N, Schiffer AA, et al. Somatic depression predicts mortality in chronic heart failure: Can this be explained by covarying symptoms of fatigue? Psychosom Med 2012; 74(5): 459–463. [DOI] [PubMed] [Google Scholar]
- 18. Jaarsma T, Arestedt KF, Martensson J, et al. The European Heart Failure Self-care Behaviour scale revised into a nine-item scale (EHFScB-9): A reliable and valid international instrument. Eur J Heart Fail 2009; 11(1): 99–105. [DOI] [PubMed] [Google Scholar]
- 19. Vellone E, Jaarsma T, Stromberg A, et al. The European Heart Failure Self-care Behaviour Scale: New insights into factorial structure, reliability, precision and scoring procedure. Patient Educ Couns 2014; 94(1): 97–102. [DOI] [PubMed] [Google Scholar]
- 20. Rector TS, Kubo SH, Cohn JN. Patients’ self-assessment of their congestive heart failure: Content, reliability and validity of a new measure, the Minnesota Living with Heart Failure questionnaire. Heart Fail 1987; 3: 198–209. [Google Scholar]
- 21. Middel B, Bouma J, de Jongste M, et al. Psychometric properties of the Minnesota Living with Heart Failure Questionnaire (MLHF-Q). Clin Rehabil 2001; 15(5): 489–500. [DOI] [PubMed] [Google Scholar]
- 22. Rector TS, Tschumperlin LK, Kubo SH, et al. Use of the Living with Heart Failure questionnaire to ascertain patients’ perspectives on improvement in quality of life versus risk of drug-induced death. J Card Fail 1995; 1(3): 201–206. [DOI] [PubMed] [Google Scholar]
- 23. Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev 1988; 8(1): 77–100. [Google Scholar]
- 24. Lahlou-Laforet K, Ledru F, Niarra R, et al. Validity of Beck Depression Inventory for the assessment of depressive mood in chronic heart failure patients. J Affect Disord 2015; 184: 256–260. [DOI] [PubMed] [Google Scholar]
- 25. Denollet J, Strik JJ, Lousberg R, et al. Recognizing increased risk of depressive comorbidity after myocardial infarction: Looking for 4 symptoms of anxiety-depression. Psychother Psychosom 2006; 75(6): 346–352. [DOI] [PubMed] [Google Scholar]
- 26. Denollet J. DS14: Standard assessment of negative affectivity, social inhibition, and type D personality. Psychosom Med 2005; 67(1): 89–97. [DOI] [PubMed] [Google Scholar]
- 27. Widdershoven J, Kessing D, Schiffer A, et al. How are depression and type D personality associated with outcomes in chronic heart failure patients? Curr Heart Fail Rep 2013; 10(3): 244–253. [DOI] [PubMed] [Google Scholar]
- 28. Pelle AJ, Schiffer AA, Smith OR, et al. Inadequate consultation behavior modulates the relationship between type D personality and impaired health status in chronic heart failure. Int J Cardiol 2010; 142(1): 65–71. [DOI] [PubMed] [Google Scholar]
- 29. Kupper N, Boomsma DI, de Geus EJ, et al. Nine-year stability of type D personality: Contributions of genes and environment. Psychosom Med 2011; 73(1): 75–82. [DOI] [PubMed] [Google Scholar]
- 30. Sowden GL, Huffman JC. The impact of mental illness on cardiac outcomes: A review for the cardiologist. Int J Cardiol 2009; 132(1): 30–37. [DOI] [PubMed] [Google Scholar]
- 31. Kessing D, Denollet J, Widdershoven J, et al. Psychological determinants of heart failure self-care: Systematic review and meta-analysis. Psychosom Med. 2016; 78(4): 412–331. [DOI] [PubMed] [Google Scholar]
- 32. Messerotti Benvenuti S, Buodo G, Mennella R, et al. Somatic, but not cognitive–affective, symptoms are associated with reduced heart rate variability in individuals with dysphoria. Front Psychol 2015; 6: 599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Everaert J, Koster EH, Derakshan N. The combined cognitive bias hypothesis in depression. Clin Psychol Rev 2012; 32(5): 413–324. [DOI] [PubMed] [Google Scholar]
- 34. Rumsfeld JS, Havranek E, Masoudi FA, et al. Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J Am Coll Cardiol 2003; 42(10): 1811–1817. [DOI] [PubMed] [Google Scholar]
- 35. Samartzis L, Dimopoulos S, Tziongourou M, et al. Effect of psychosocial interventions on quality of life in patients with chronic heart failure: A meta-analysis of randomized controlled trials. J Card Fail 2013; 19(2): 125–134. [DOI] [PubMed] [Google Scholar]
- 36. Garber MC, Nau DP, Erickson SR, et al. The concordance of self-report with other measures of medication adherence: A summary of the literature. Med Care 2004; 42(7): 649–652. [DOI] [PubMed] [Google Scholar]


