Abstract
Background:
Evidence supporting the effectiveness of aerobic training, specific for fatigue, in severely fatigued patients with multiple sclerosis (MS) is lacking.
Objective:
To estimate the effectiveness of aerobic training on MS-related fatigue and societal participation in ambulant patients with severe MS-related fatigue.
Methods:
Patients (N = 90) with severe MS-related fatigue were allocated to 16-week aerobic training or control intervention. Primary outcomes were perceived fatigue (Checklist Individual Strength (CIS20r) fatigue subscale) and societal participation. An improvement of ⩾8 points on the CIS20r fatigue subscale was considered clinically relevant. Outcomes were assessed by a blinded observer at baseline, 2, 4, 6 and 12 months.
Results:
Of the 89 patients that started treatment (median Expanded Disability Status Scale (interquartile range), 3.0 (2.0–3.6); mean CIS20r fatigue subscale (standard deviation (SD)), 42.6 (8.0)), 43 received aerobic training and 46 received the control intervention. A significant post-intervention between-group mean difference (MD) on the CIS20r fatigue subscale of 4.708 (95% confidence interval (CI) = 1.003–8.412; p = 0.014) points was found in favour of aerobic training that, however, was not sustained during follow-up. No effect was found on societal participation.
Conclusion:
Aerobic training in MS patients with severe fatigue does not lead to a clinically meaningful reduction in fatigue or societal participation when compared to a low-intensity control intervention.
Keywords: Multiple sclerosis, rehabilitation, exercise therapy, fatigue, randomized controlled trial
Introduction
Multiple sclerosis (MS) is considered an immune-mediated chronic disorder of the central nervous system and is the most common neurological disease causing disability in young and middle-aged people.1 MS-related fatigue is one of the most often reported symptoms that leads to restrictions in societal participation and performance in daily life at home, at work and in leisure activities.2,3 MS-related fatigue can be defined as ‘a subjective lack of mental or physical energy as perceived by the individual (or caregiver) to interfere with usual and desired activities’.4 It can be of central or peripheral origin and may affect physical, cognitive or psychosocial functions.5
Exercise therapy may positively affect MS-related fatigue, and a variety of mechanisms have been proposed to explain possible beneficial effects including a neuroprotective effect,6 normalization of hypothalamic–pituitary–adrenal axis imbalances5 or an anti-inflammatory effect.7,8 In addition, aerobic training or exercise in general may reduce the imminent effects of reduced physical activity and the vicious cycle of deconditioning leading to a reduced physical fitness, reduced general health and a higher incidence of comorbidity.9,10 A meta-analysis evaluating current evidence on the effectiveness of exercise therapy on fatigue in patients with MS found a significant heterogeneous moderate effect in favour of exercise therapy (standardized mean difference (SMD): −0.53, 95% confidence interval (CI) = −0.73 to −0.33).11 However, the effectiveness of exercise therapy was not investigated in patients specifically selected for severe levels of fatigue and were insufficiently powered to study MS-related fatigue.11
The objective of the ‘Treating Fatigue in Multiple Sclerosis–Aerobic training’ (TREFAMS-AT) trial was to estimate the immediate and 1-year follow-up effect of 16-week aerobic training, in comparison with a control intervention, on MS-related fatigue and societal participation in ambulant patients with severe MS-related fatigue.
Methods
TREFAMS-AT was a multicentre, single-blinded, randomized controlled trial with five repeated measurements over the course of 12 months. The TREFAMS-AT trial was part of a multi-trial programme (TREFAMS-ACE) designed to study the effects of aerobic training, cognitive behavioural therapy and energy conservation management on MS-related fatigue in ambulant persons with severe MS-related fatigue (eSupplement 1).12
Study participants
Recruitment took place between October 2011 and October 2014 through two hospital-based outpatient MS centres: St Antonius Hospital, Nieuwegein, The Netherlands and Jeroen Bosch Hospital, Den Bosch, The Netherlands. The recruiting rehabilitation physician or neurologist informed potential participants about the TREFAMS-AT trial. Subsequently, potential participants were evaluated against the inclusion and exclusion criteria and enrolled if eligible. In short, inclusion criteria included patients with definite MS, age ⩾18 and ⩽70 years, ambulant (Expanded Disability Status Scale (EDSS) ⩽6.0), severe fatigue (Checklist Individual Strength (CIS20r) fatigue subscale ⩾35) and no signs of an MS exacerbation or corticosteroid treatment <3 months. Patients were excluded if having severe mood disorders (Hospital Anxiety and Depression Scale (HADS) – depression subscale >11), severe co-morbidity (Cumulative Illness Rating Scale item scores ⩾3), current pregnancy or given birth <3 months, newly initiated pharmacological (e.g. amantadine) or non-pharmacological treatment for fatigue (e.g. structured aerobic training) <3 months. This study was approved by the medical ethical board of the VU University Medical Center, Amsterdam and registered under number ISRCTN69520623 (Controlled-trials.com). All participants provided oral and written informed consent in compliance with the declaration of Helsinki and good clinical practice.
Randomization and therapy allocation
Randomization was performed by an independent researcher, using an online concealed computer-generated randomization scheme with random variable block sizes (Julius Center, University Medical Center Utrecht, Utrecht, The Netherlands).
Procedures
For a comprehensive overview, according to the TiDiER guidelines,13 of the aerobic training intervention, see eSupplement 2. In short, the aerobic training programme consisted of aerobic interval training, three times a week, for the duration of 16 weeks. In total 12 sessions were given in an outpatient clinic and supervised by an experienced physiotherapist whereas the remaining 36 sessions were home-based using identical equipment as provided by the study team for the duration of the intervention. The frequency of supervised sessions declined gradually during the intervention phase. Each training session consisted of 30 minutes of aerobic interval training on an electro-magnetic cycle ergometer. Each training session entailed six interval cycles consisting of 3 minutes at 40%, 1 minute at 60% and 1 minute at 80% of peak power. Peak power was determined at the start of training and re-evaluated after 8 weeks by means of a cardiopulmonary exercise test (CPET) until voluntary exhaustion. Participants logged the date and time of training, the number of minutes completed, the perceived exertion at the end of their training session and any comments or reasons for not completing the training session.
Participants allocated to the control condition received three 45-minute consultations with an MS nurse over the 16-week period (see eSupplement 3). The content of the consultations led by the MS nurse covered two important aspects in relation to the experimental intervention: (1) reliable information on MS-related fatigue and (2) guidance from the experienced MS nurse that aimed to reassure the patient that his or her concerns or questions were being taken seriously. The MS nurse was not allowed to refer the patient to any other outpatient or inpatient facilities for the treatment of fatigue.
Outcome measures
All outcomes were assessed serially at baseline, 2, 4 (i.e. post-intervention), 6 and 12 months of follow-up. Face-to-face measurements were performed by a trained single-blinded assessor (M.H.) and performed at the hospital-based outpatient clinic through which the patient was recruited on separate days from those in which the experimental and control condition were provided to maintain blinding. The primary outcomes of the TREFAMS-AT trial were MS-related fatigue measured with the Checklist Individual Strength (CIS20r) fatigue subscale, and societal participation measured with the Impact on Participation and Autonomy (IPA) questionnaire.14,15
The CIS20r fatigue subscale entails eight items on a 7-point Likert scale leading to a sum score between 8 and 56 points and details perceived fatigue (e.g. ‘I feel tired’) over the previous 2 weeks.14 A change of eight points was considered to be a clinically relevant difference.12 The IPA is a generic questionnaire that addresses perceived problems of participation and autonomy, reflected in 32 items assigned to five domains including autonomy indoors, autonomy outdoors, family role, social relations, work and education.15 A score of 0–4 is calculated for each domain, and a higher score indicates greater perceived restrictions in that respective domain. A responsiveness study in a heterogeneous outpatient rehabilitation setting showed that the IPA questionnaire has a moderate ability to detect within-patient changes over time.15
Safety was assessed in terms of the number of self-reported as well as (steroid) treated MS relapses during each visit window and defined as new or a worsening of reoccurring symptoms for a duration longer than 24 hours, in the absence of fever or secondary inflammation (e.g. infection).
The secondary outcome measures were related to the primary working mechanism (i.e. physical fitness) as well as complementary fatigue measures. Participants performed a CPET including gas exchange measurement on an electromagnetically braked cycle ergometer to determine peak exercise capacity at each measurement visit. Following a 3-minute rest phase, participants cycled at 25+10 W/min (women) or 15 W/min (men) until voluntary exhaustion. The following CPET parameters were used in this study: peak oxygen consumption (VO2peak, VO2peak corrected for body weight and %predicted-VO2peak16), peak power output (W) and the anaerobic threshold (%predicted-VO2peak).
In addition to the CIS20r fatigue subscale, we also included the CIS20r subscales for concentration, motivation and activity, the Modified Fatigue Impact Scale (MFIS)17 which entails a physical, cognitive and psychosocial subscale and the Fatigue Severity Scale (FSS) which assesses the impact of fatigue.18
Therapy adherence
Therapy adherence was assessed by (1) the number of therapy sessions adhered to and (2) the percentage work performed within the aerobic training group relative to the work prescribed. Next to the aerobic training or MS nurse consultation, the number of additional medical and allied healthcare consultations was documented at each visit.
Statistical analysis
The sample size calculation was based on the CIS20r fatigue subscale. A total of 45 patients per arm, and 90 patients in total, were needed to detect a clinically relevant difference of eight points on the CIS20r fatigue subscale in an MS population with a standard deviation (SD) of 12.7, with a power of 80%, an alpha of 0.05 and a drop-out rate of 20%.19,20 Successful blinding of the assessor (M.H.) for treatment allocation was tested by comparing the assessors’ guesses with actual treatment allocation using a Cohen’s Kappa statistic following completion of the data collection and analysis (i.e. successful blinding when Kappa statistic <0.20).21 An independent two-sample t-test or chi-square test was used to compare differences between the two groups at baseline.
Longitudinal mixed-model analyses were performed on an intention-to-treat basis. The primary analysis was the change in the CIS20r fatigue subscale score in the aerobic training group compared with the control intervention. Study centre, baseline value of the dependent variable, time, study group and time-by-study group were included as independent variables. In addition, adjusted analyses were performed by adding gender and EDSS at baseline as fixed covariates on the basis of their association with aerobic capacity.22 These analyses were repeated for the IPA subdomains and secondary outcomes related to physical fitness and MS-related fatigue. We calculated (adjusted for disease severity) both the odds of reporting an MS relapse and having received steroid treatment under the hypothesis that the latter would be indicative of a significant relapse requiring treatment as confirmed by a neurologist. The proportion of patients that showed a clinically meaningful difference (⩾8 points) in the aerobic training group against those in the control intervention was calculated. Based on the absolute risk reduction (ARR) between the intervention and control condition, the number needed to treat (NNT) was estimated. All analyses were performed two-tailed, with a critical value of 0.05 using SPSS, version 22.
Results
Study population
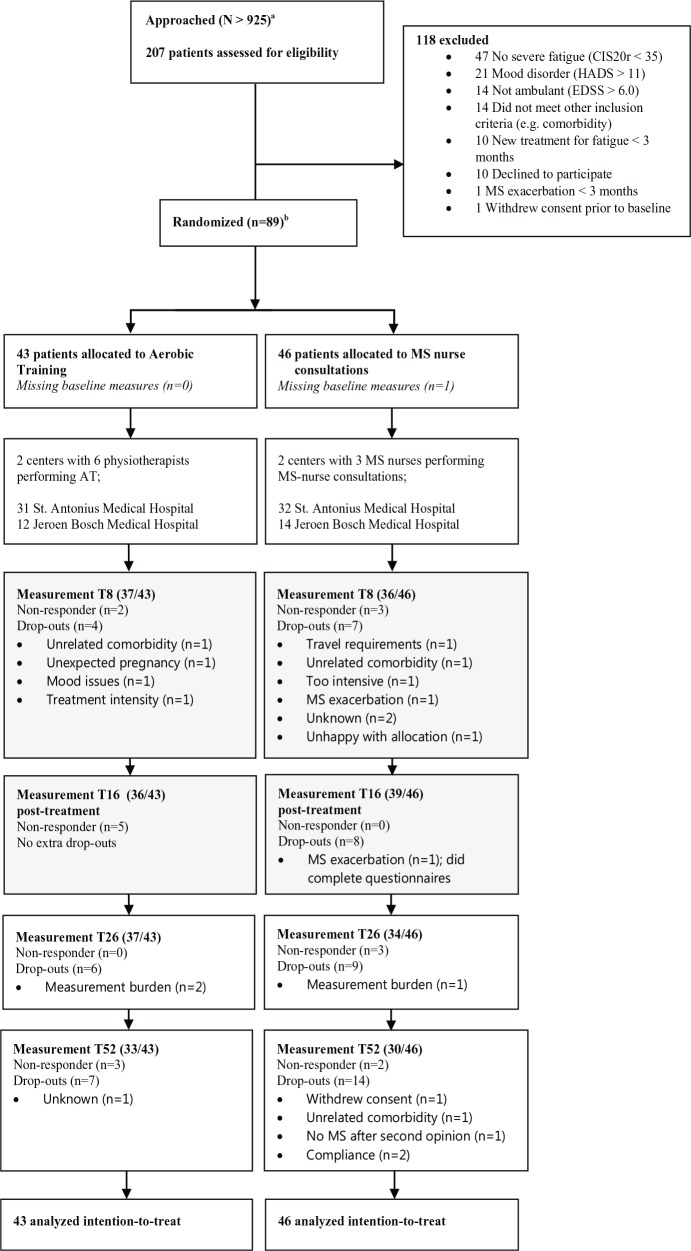
Figure 1 shows the trial profile. Of the 925 MS patients approached between 1st October 2011 and 1st October 2014, 207 were assessed for eligibility and 90 were included. Primary reasons for not participating were the lack of severe fatigue (CIS20r fatigue subscale < 35; 44%) or suspected mood disorders (HADS subscale depression > 11; 20%). Table 1 shows the baseline characteristics of the study sample. Despite the random allocation, the aerobic training group had a lower EDSS score (MD (standard error (SE)),−0.6 (0.3), p = 0.038), shorter time since diagnosis (−3.7 (1.5), p = 0.016), lower mean age (−5.1 (2.0), p = 0.014) and less perceived restrictions in the work/education domain of the IPA (−0.4 (0.2), p = 0.020). The drop-out rate post-intervention was 15.7% whereas the overall drop-out rate at 1-year follow-up was 29.2%. Reasons for drop-out are listed in Figure 1.
Figure 1.
CONSORT diagram for TREFAMS-AT trial. The light grey area marks the treatment phase.
aDue to use of a website and local advertisement, the exact number of potential participants reached cannot be determined.
b90 patients with MS were included; one withdrew prior to randomization due to transport issues.
Table 1.
Demographics and baseline characteristics.
| Total (N = 89) | AT (n = 43) | MS nurse (n = 46) | |
|---|---|---|---|
| Characteristics | |||
| Gender (%F) | 73.3 | 74.4 | 71.7 |
| Age (years) | 45.8 ± 9.7 | 43.1 ± 9.8 | 48.2 ± 9.2* |
| BMI (kg/m2) | 25.5 ± 4.8 | 25.6 ± 5.4 | 25.4 ± 4.3 |
| EDSSa | 3.0 (2.0–3.6) | 2.5 (2.0–3.5) | 3.0 (2.0–4.0)* |
| Disease duration (years)a | 8.0 (2.0–15.3) | 7.0 (2.0–10.0) | 12.0 (2.0–19.0)* |
| Type of MS (n) | |||
| RRMS | 65 | 31 | 34 |
| SPMS | 8 | 3 | 5 |
| PPMS | 16 | 9 | 7 |
| Use of MS medication (n) | |||
| Interferon | 21 | 9 | 12 |
| Glatiramer | 11 | 5 | 6 |
| Natalizumab | 7 | 3 | 4 |
| Fingolimod | 4 | 3 | 1 |
| Tecfidera | 1 | – | 1 |
| Laquinimod | 1 | – | 1 |
| 4-aminopyridine | 2 | 1 | 1 |
| CIRSa | 1.6 (1.5) | 1.5 (1.5) | 1.7 (1.5) |
| MMSE (0–30) | 28.7 (1.5) | 28.8 (1.4) | 28.5 (1.6) |
| Primary outcomes | |||
| CIS20r fatigue (8–56)a | 42.6 (8.0) | 42.6 (7.4) | 42.4 (8.5) |
| IPA autonomy indoors (0–4)a | 0.7 (0.6) | 0.7 (0.6) | 0.7 (0.6) |
| IPA family role (0–4)a | 1.5 (0.7) | 1.4 (0.7) | 1.6 (0.7) |
| IPA autonomy outdoors (0–4)a | 1.6 (0.8) | 1.5 (0.7) | 1.6 (0.8) |
| IPA social relations (0–4)a | 0.9 (0.5) | 0.9 (0.5) | 0.9 (0.5) |
| IPA work/education (0–4)a | 1.9 (0.9) | 1.7 (0.9) | 2.1 (0.8)* |
| Secondary fatigue outcomes | |||
| FSS (1–7)a | 5.3 (0.9) | 5.2 (1.0) | 5.3 (0.9) |
| MFIS total score(0–84)a | 41.2 (12.1) | 40.8 (12.1) | 41.5 (12.3) |
| MFIS physical (0–36)a | 20.2 (5.6) | 19.7 (4.9) | 20.6 (6.2) |
| MFIS cognitive (0–40)a | 17.4 (7.7) | 17.7 (7.1) | 16.8 (8.1) |
| MFIS psychosocial (0–8)a | 3.7 (1.8) | 3.5 (1.7) | 3.9 (1.8) |
| CIS20r concentration (5–35)a | 19.8 (7.5) | 20.9 (6.6) | 18.7 (8.2) |
| CIS20r motivation (4–28)a | 14.9 (5.3) | 15.1 (5.2) | 14.7 (5.5) |
| CIS20r physical activity (3–21)a | 12.4 (4.8) | 12.1 (4.6) | 12.8 (4.9) |
| Fitness parameters | |||
| VO2peak (L/min) | 1.64 (0.54) | 1.75 (0.57) | 1.53 (0.50) |
| VO2peak (mL/kg/min) | 21.6 (5.9) | 22.6 (6.2) | 20.8 (5.6) |
| VO2peak (%predicted) | 64.4 (17.6) | 65.0 (17.3) | 63.7 (18.3) |
| Anaerobic threshold (%VO2peak)b | 43.9 (14.0) | 45.0 (16.5) | 42.9 (11.4) |
| Peak power (W) | 151 (51) | 161 (52) | 142 (49) |
AT: aerobic training; MS: multiple sclerosis; BMI: body mass index; EDSS: Expanded Disability Status Scale; RRMS: relapsing-remitting multiple sclerosis; SPMS: secondary-progressive multiple sclerosis; PPMS: primary-progressive multiple sclerosis; CIRS: Cumulative Illness Rating Scale; MMSE: mini-mental state exam; CIS20r: Checklist Individual Strength; IPA: Impact on Participation and Autonomy questionnaire; FSS: Fatigue Severity Scale; MFIS: Modified Fatigue Impact Scale; VO2peak: peak oxygen uptake; SD: standard deviation.
All values are mean ± SD except for the EDSS and disease duration which are median (interquartile range).
Lower score represents a better outcome.
The anaerobic threshold is presented relative to the predicted peak oxygen uptake.
Significant (p < 0.05) between-group difference at baseline.
Therapy content
The average (±SD) adherence in the experimental group was 74 ± 25% completed sessions and 71 ± 25% of prescribed workload at an average intensity of 14.0 ± 2.1 on the 6–20 Borg scale of perceived exertion. Adherence was significantly (p < 0.05) lower in the second 8-week period (66 ± 30% completed session; 62 ± 31% of prescribed workload) of treatment in comparison to the first 8-week period (86 ± 14% completed session; 79 ± 25% of prescribed workload). In addition, perceived exertion (6–20 Borg scale of perceived exertion) following each training session was significantly higher (13.5 ± 2.0 vs 14.8 ± 2.4; p < 0.05) during the second 8 weeks of training. A total of 87% of the participants allocated to the control condition completed all three consultations with the MS nurse. The self-reported supplemental medical or allied healthcare consultations were not significantly different between the two study groups.
Outcome measures
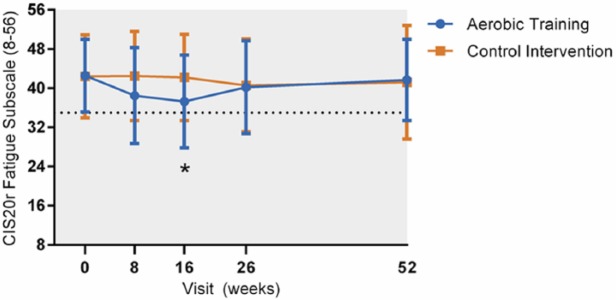
Cohen’s Kappa between assessor’s guess and actual allocation was 0.057 (p = 0.593), indicating successful blinding of the assessor. The mean CIS20r subscale fatigue score significantly improved from baseline to 4 months by 4.708 (95% CI = 1.003–8.412; p = 0.014; Table 2) points in favour of aerobic training. This effect was not sustained during the follow-up assessment at months 6 and 12 (Table 2; Figure 2). No significant improvements were found on the various domains of societal participation. The effect on the CIS20r fatigue subscale was preceded by an increase in peak power output between baseline and 2 months (MD = 11.701, 95% CI = 0.200–23.202; p = 0.048) in favour of the aerobic training group. However, no significant improvements were found with regard to VO2peak and/or anaerobic threshold.
Table 2.
The effect of aerobic training versus control on the primary outcome measures, secondary fatigue measures, and fitness parameters.
| T8 |
T16 |
T26 |
T52 |
MD (SE), p
Between-group effect |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AT | C | AT | C | AT | C | AT | C | T8 | T16 | T26 | T52 | |
| Primary outcomes | ||||||||||||
| n valid | 43 | 37 | 34 | 39 | 37 | 34 | 33 | 30 | ||||
| CIS20r fatigue (8–56)a | 38.5 (9.8) | 42.5 (9.1) | 37.3 (9.5) | 42.2 (8.8) | 40.2 (9.5) | 40.6 (9.5) | 41.7 (8.3) | 41.2 (11.6) | −3.308 (1.877), p = 0.080 | −4.708 (1.890), p = 0.014* | −0.402 (1.908), p = 0.834 | 1.145 (1.971), p = 0.562 |
| IPA autonomy indoors (0–4)a | 0.7 (0.6) | 0.7 (0.5) | 0.5 (0.6) | 0.7 (0.6) | 0.7 (0.7) | 0.6 (0.6) | 0.8 (0.7) | 0.8 (0.6) | −0.027 (0.087), p = 0.756 | −0.112 (0.088), p = 0.203 | 0.084 (0.091), p = 0.358 | −0.007 (0.093), p = 0.944 |
| IPA family role (0–4)a | 1.4 (0.7) | 1.5 (0.7) | 1.2 (0.8) | 1.4 (0.7) | 1.4 (0.7) | 1.4 (0.7) | 1.3 (0.9) | 1.4 (0.6) | −0.031 (0.121), p = 0.801 | −0.082 (0.122), p = 0.502 | 0.107 (0.125), p = 0.394 | −0.005 (0.127), p = 0.996 |
| IPA autonomy outdoors (0–4)a | 1.4 (0.8) | 1.6 (0.6) | 1.4 (0.8) | 1.6 (0.8) | 1.4 (0.9) | 1.5 (0.7) | 1.5 (0.8) | 1.5 (0.6) | −0.078 (0.125), p = 0.531 | −0.097 (0.125), p = 0.438 | 0.059 (0.128), p = 0.646 | 0.096 (0.129), p = 0.459 |
| IPA social relations (0–4)a | 1.0 (0.6) | 0.9 (0.5) | 0.9 (0.5) | 1.0 (0.6) | 0.9 (0.5) | 0.9 (0.6) | 1.0 (0.5) | 1.0 (0.5) | 0.033 (0.092), p = 0.718 | −0.138 (0.092), p = 0.135 | 0.039 (0.095), p = 0.680 | 0.070 (0.096), p = 0.469 |
| IPA work/education (0–4)a | 1.7 (0.9) | 2.0 (1.0) | 1.7 (0.9) | 1.8 (0.7) | 1.7 (0.9) | 1.9 (0.7) | 1.8 (1.0) | 2.0 (0.9) | 0.005 (0.166), p = 0.974 | 0.225 (0.167), p = 0.181 | 0.133 (0.172), p = 0.441 | 0.168 (0.174), p = 0.337 |
| Secondary outcomes | ||||||||||||
| Fatigue | ||||||||||||
| nvalid | 43 | 37 | 34 | 39 | 37 | 34 | 33 | 30 | ||||
| FSS (1–7)a | 5.1 (1.1) | 5.3 (1.0) | 5.1 (0.9) | 5.2 (1.0) | 5.2 (0.9) | 5.1 (1.1) | 5.2 (1.1) | 5.1 (1.1) | −0.042 (0.170), p = 0.808 | −0.011 (0.173), p = 0.949 | 0.095 (0.176), p = 0.589 | 0.317 (0.180), p = 0.079 |
| MFIS total score(0–84)a | 37.3 (12.7) | 43.8 (12.2) | 38.6 (12.0) | 41.5 (11.9) | 38.3 (13.7) | 34.7 (11.8) | 39.0 (13.4) | 39.9 (11.9) | −3.861 (2.296), p = 0.094 | −1.775 (2.320), p = 0.445 | 3.312 (2.344), p = 0.159 | 0.952 (2.407), p = 0.693 |
| MFIS physical subscale(0–36)a | 18.0 (6.2) | 21.8 (5.7) | 19.0 (5.4) | 20.4 (5.3) | 18.1 (6.2) | 17.8 (6.7) | 18.5 (6.1) | 20.1 (4.8) | −2.038 (1.168), p = 0.083 | −0.711 (1.173), p = 0.545 | 0.586 (1.191), p = 0.623 | −0.760 (1.224), p = 0.535 |
| MFIS cognitive subscale (0–40)a | 16.0 (6.8) | 17.6 (8.9) | 15.9 (7.6) | 17.1 (8.8) | 16.4 (7.8) | 13.8 (7.2) | 17.2 (6.8) | 16.1 (9.1) | −1.330 (1.156). p = 0.252 | −1.164 (1.170), p = 0.321 | 2.056 (1.183), p = 0.084 | 1.391 (1.207), p = 0.251 |
| MFIS psychosocial subscale (0–8)a | 3.4 (1.8) | 4.4 (1.6) | 3.6 (1.4) | 4.1 (1.5) | 3.8 (1.7) | 3.2 (1.8) | 3.4 (1.7) | 3.8 (1.6) | −0.771 (0.325), p = 0.019 | −0.188 (0.329), p = 0.567 | 0.547 (0.335), p = 0.104 | −0.191 (0.342), p = 0.576 |
| CIS20r concentration (5–35)a | 19.2 (6.5) | 20.0 (7.8) | 18.3 (6.8) | 20.3(7.1) | 19.7 (7.3) | 18.8 (7.0) | 20.7 (6.8) | 19.5 (7.7) | −1.301 (1.260), p = 0.303 | −2.458 (1.268), p = 0.054 | −0.314 (1.282), p = 0.807 | 1.037 (1.326), p = 0.435 |
| CIS20r motivation (4–28)a | 13.6 (5.0) | 14.6 (5.7) | 14.6 (4.9) | 15.2 (4.9) | 15.3 (5.9) | 14.7 (6.0) | 14.7 (4.8) | 13.8 (5.7) | −1.231 (0.957), p = 0.200 | −0.583 (0.964), p = 0.546 | −0.204 (0.975), p = 0.834 | 0.345 (1.013), p = 0.734 |
| CIS20r physical activity (3–21)a | 11.6 (5.3) | 14.1 (3.9) | 11.7 (4.9) | 13.2 (4.3) | 12.4 (4.9) | 13.1 (4.2) | 12.0 (3.7) | 13.1 (4.4) | −2.181 (0.854), p = 0.011* | −1.398 (0.859), p = 0.106 | −0.849 (0.868), p = 0.329 | −0.414 (0.901), p = 0.647 |
| Fitness parameters | ||||||||||||
| n valid | 35 | 31 | 27 | 31 | 24 | 33 | 27 | 30 | ||||
| VO2peak (L/min) | 1.78 (0.55) | 1.52 (0.55) | 1.74 (0.59) | 1.58 (0.55) | 1.75 (0.51) | 1.53 (0.59) | 1.68 (0.49) | 1.61 (0.59) | 0.082 (0.080), p = 0.305 | 0.048 (0.082), p = 0.561 | 0.023 (0.082), p = 0.779 | −0.046 (0.082), p = 0.579 |
| VO2peak (mL/kg/min) | 23.5 (6.4) | 20.2 (6.2) | 23.5 (7.4) | 21.4 (6.4) | 22.9 (6.0) | 20.8 (7.0) | 22.3 (5.6) | 21.9 (7.0) | 1.628 (1.046), p = 0.122 | 0.979 (1.075), p = 0.364 | 0.313 (1.083), p = 0.773 | −0.710 (1.085), p = 0.514 |
| VO2peak (%predicted) | 68.2 (17.7) | 63.4 (17.6) | 68.8 (21.9) | 65.7 (18.7) | 67.8 (19.8) | 64.2 (21.8) | 65.5 (16.9) | 66.1 (20.0) | 3.827 (3.038), p = 0.210 | 3.491 (3.135), p = 0.267 | 1.667 (3.163), p = 0.599 | −1.146 (3.165), p = 0.718 |
| Anaerobic threshold (%VO2peak)b | 47.8 (19.2) | 46.5 (14.8) | 45.1 (9.6) | 47.3 (17.4) | 47.1 (14.8) | 46.7 (18.6) | 44.5 (11.4) | 47.2 (13.4) | −0.801 (3.114), p = 0.797 | 0.799 (3.222), p = 0.804 | −3.500 (3.260), p = 0.285 | −5.137 (3.264), p = 0.118 |
| Peak power (W) | 180 (58) | 149 (51) | 180 (61) | 151 (51) | 171 (58) | 150 (53) | 173 (54) | 151 (58) | 11.701 (5.868), p = 0.048* | 8.971 (6.038), p = 0.140 | −1.326 (6.095), p = 0.828 | 1.708 (6.189), p = 0.783 |
AT: aerobic training; C: control condition; MD: mean difference – reflects the between-group difference at that time point; SE: standard error; CIS20r: Checklist Individual Strength; IPA: Impact on Participation and Autonomy questionnaire; FSS: Fatigue Severity Scale; MFIS: Modified Fatigue Impact Scale; VO2peak: peak oxygen uptake.
Lower score represents better outcome; T8–T52 represent the time (T) in weeks post-baseline at which the outcome was assessed.
The anaerobic threshold is presented relative to the predicted peak oxygen uptake.
Significant (p < 0.05) between-group difference at that given visit corrected for baseline and study centre (highlighted in bold).
Figure 2.
Change in perceived fatigue according to the CIS20r fatigue subscale in the aerobic training group (blue line) and control group (orange line). The horizontal reference line at 35 points indicates the value above which participants had to score in order to be included (i.e. severe fatigue). Asterisk (*) indicates a significant (p = 0.014) mean difference of 4.7 points between the aerobic training group and control group based on the mixed-model analysis.
With respect to the secondary fatigue measures, from baseline to 2 months, a significant effect was found on the MFIS psychosocial subscale (MD = −0.771, 95% CI = −1.388 to −0.154; p = 0.019) and on the CIS20r physical activity subscale (MD = −2.181, 95% CI = −3.855 to −0.507; p = 0.011), in favour of aerobic training. No such effect was found from baseline to 4 months or during the follow-up phase.
In total, 11 of the 34 participants (32.4%) in the exercise group, who completed the post-intervention assessment, and 8 out of 38 participants (21.1%) allocated to the control condition showed a clinically meaningful reduction of eight points or larger on the CIS20r fatigue subscale leading to an ARR of 0.113 (95% CI = 0.091–0.317) and a NNT of 8.9 (95% CI = 3.2 to infinite; p > 0.05). Despite imbalances in disease severity at baseline, the adjusted analyses including gender and EDSS did not lead to different results.
Safety
The odds of (self)reporting an MS relapse in patients with relapsing–remitting MS (N = 65), corrected for disease severity, was 0.277 (95% CI = 0.097–0.787; p = 0.016) in favour of aerobic training. The odds of undergoing steroid treatment related to an MS relapse in patients with relapsing–remitting MS, corrected for disease severity, was 0.946 (95% CI = 0.241–3.711; p = 0.937).
Discussion
To the best of our knowledge, this study is the largest, single-blind randomized controlled trial specifically designed and powered to assess the effectiveness of aerobic training on MS-related fatigue and societal participation in severely fatigued patients with MS. We found a small significant post-intervention effect in favour of aerobic training on our primary outcome, MS-related fatigue. The odds of reporting an MS relapse or receiving steroid treatment indicated that aerobic training is not associated with a higher risk for MS exacerbations. The limited magnitude (i.e. 4.7 points; range = 8–56) of change on the CIS20r fatigue subscale was below the predefined cut-off of eight points for a clinically relevant difference, did not result in corresponding changes on the secondary fatigue measures, and was not sustained during follow-up. The NNT was estimated at 9.
Research into MS-related fatigue is hampered by the lack of understanding and consensus regarding the construct and assessment of MS-related fatigue. This is, for instance, illustrated by the finding that the decline in MS-related fatigue was only captured within the CIS20r fatigue subscale and may suggest some regression to the mean or placebo effect. However, also according to the cut-off for severe fatigue on the FSS (>5.0), most patients were severely fatigued at baseline according to the FSS as well.23 If we argue that the CIS20r fatigue subscale measures the severity of fatigue, and the FSS measures the impact of fatigue (e.g. ‘fatigue interferes with my physical functioning’), this would confirm our conclusion that the small decline in fatigue severity does not reduce the impact of fatigue and may therefore explain the absence of improvements in societal participation. Surprisingly, despite low levels of physical fitness at baseline, markers of physical fitness showed limited response to the provided training stimulus; a significant effect on peak power at 8 weeks and a marginal non-significant trend towards an increase in peak oxygen uptake and greater aerobic capacity. These results may have been hampered by selective loss of treatment adherence during the second phase of the training intervention. However, the magnitude of change in VO2peak was not out of scope with the previous literature indicating heterogeneous and small effects on VO2peak in patients with MS.9 This may question the trainability of patients with MS or potential subgroups of patients. Future research should be conducted to identify predictors of treatment response with respect to aerobic training or exercise therapy in general and the interaction of these predictors with the dose of therapy provided. However, even if we are able to pre-select patients that are likely to benefit from aerobic training, it is important to recall that the small reduction on the CIS20r fatigue subscale in this study was not sustained during follow-up. It has been suggested that incorporating behavioural change techniques into exercise-based interventions may improve the long-term effectiveness of exercise interventions.24,25 However, a recent review showed that behavioural physical activity interventions also fail to sustain long-term effects.26
A Cochrane systematic review (search date 24 October 2014) on the effects of exercise therapy on fatigue in patients with MS identified 45 studies, of which 35 trials were included in a pooled meta-analysis.11 The overall SMD of exercise therapy was −0.53 (95% CI = −0.73 to −0.33) in favour of exercise therapy. For aerobic training in particular, the SMD was −0.43 (95% CI = −0.69 to −0.17) suggesting that the outcome on the primary outcome fatigue (SMD = −0.53 (95% CI = −1.0 to −0.06)) was within the pooled 95% limits of this Cochrane review. However, in contrast to our study, the trials included in the Cochrane review suffer from two major limitations. First, none of the included trials did use fatigue as a primary outcome measure, and, second, none of these trials did include specifically participants with a predefined severe level of fatigue.
Despite the robust study design, this study shows some limitations. First, it took 1 year longer than expected to recruit the required 90 patients with MS with severe fatigue. Fatigue has been previously identified as one of the key barriers to engaging in physical activity for patients with MS.27 This may have delayed the inclusion and raised concerns regarding the implementation of (high-intensity) exercise as a means to improve fatigue in patients with pre-existing severe levels of fatigue. However, being an important barrier to engage in physical activity, this also reduces the likelihood of an increase in physical activity in patients allocated to the control condition. Second, the actual training response in terms of physical fitness was marginal yet in line with previous work.9 Future research should elucidate the fundamental question as to the trainability of persons with multiple sclerosis as well as whether the magnitude of change in physical fitness mediates the change in MS-related fatigue.
On the basis of this study and previous research, we conclude that despite the small significant positive post-intervention effect and the absence of associated harm, aerobic training does not lead to clinically relevant improvements in MS-related fatigue and societal participation. This conclusion does not imply that aerobic training should not be used in clinical practice. Exercise therapy, and aerobic training in particular, has proven efficacy in the treatment and prevention of physical deconditioning, mobility problems, secondary health risks and potentially in disease progression.6,9,10
Supplementary Material
Acknowledgments
This study has been performed on behalf of the Treating Fatigue in Multiple Sclerosis: Aerobic Training, Cognitive Behavioural Therapy, Energy Conservation management (TREFAMS-ACE) Study Group: V de Groot and H Beckerman (programme coordination), A Malekzadeh, LE van den Akker, M Looijmans (until September 2013), SA Sanches (until February 2012), J Dekker, EH Collette, BW van Oosten, CE Teunissen, MA Blankenstein, ICJM Eijssen, M Rietberg (VU University Medical Center, Amsterdam); M Heine, O Verschuren, G Kwakkel, JMA Visser-Meily, IGL van de Port (until February 2012), E Lindeman (until September 2012) (Center of Excellence for Rehabilitation Medicine, University Medical Centre Utrecht and Rehabilitation Centre, De Hoogstraat, Utrecht); LJM Blikman, J van Meeteren, JBJ Bussmann, HJ Stam, RQ Hintzen (Erasmus MC, University Medical Center, Rotterdam); HGA Hacking, EL Hoogervorst, STFM Frequin (St Antonius Hospital, Nieuwegein); H Knoop, BA de Jong (until January 2014), G Bleijenberg (until April 2012) (University Medical Center St Radboud, Nijmegen); FAJ de Laat (Libra Rehabilitation Medicine & Audiology – location Leijpark, Tilburg); MC Verhulsdonck (Rehabilitation Center, Sint Maartenskliniek, Nijmegen); EThL van Munster (Jeroen Bosch Hospital, Den Bosch); CJ Oosterwijk, GJ Aarts (until March 2013) (Dutch patient organization, Multiple Sclerosis Vereniging Nederland (MSVN), The Hague).
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The TREFAMS-ACE study was funded by the Fonds NutsOhra (ZonMw 89000005). The funding organization had no role in the design and conduct of the study; collection, management, analysis and interpretation of data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Contributor Information
Martin Heine, VUmc MS Center Amsterdam and Department of Rehabilitation Medicine, VU University Medical Center, Amsterdam, The Netherlands/Brain Center Rudolf Magnus and Center of Excellence for Rehabilitation Medicine, University Medical Center Utrecht and Rehabilitation Center De Hoogstraat, Utrecht, The Netherlands.
Olaf Verschuren, Brain Center Rudolf Magnus and Center of Excellence for Rehabilitation Medicine, University Medical Center Utrecht and Rehabilitation Center De Hoogstraat, Utrecht, The Netherlands.
Erwin LJ Hoogervorst, Multiple Sclerosis Center, St Antonius Hospital, Nieuwegein, The Netherlands.
Erik van Munster, Department of Neurology, Jeroen Bosch Ziekenhuis, Den Bosch, The Netherlands.
Hub GA Hacking, Multiple Sclerosis Center, St Antonius Hospital, Nieuwegein, The Netherlands.
Anne Visser-Meily, Brain Center Rudolf Magnus and Center of Excellence for Rehabilitation Medicine, University Medical Center Utrecht and Rehabilitation Center De Hoogstraat, Utrecht, The Netherlands.
Jos WR Twisk, Department of Epidemiology and Biostatistics, VU University Medical Center, Amsterdam, The Netherlands/EMGO+ Institute for Health and Care Research, VU University Medical Center, Amsterdam, The Netherlands.
Heleen Beckerman, VUmc MS Center Amsterdam and Department of Rehabilitation Medicine, VU University Medical Center, Amsterdam, The Netherlands; EMGO+ Institute for Health and Care Research, VU University Medical Center, Amsterdam, The Netherlands.
Vincent de Groot, VUmc MS Center Amsterdam and Department of Rehabilitation Medicine, VU University Medical Center, Amsterdam, The Netherlands; EMGO+ Institute for Health and Care Research, VU University Medical Center, Amsterdam, The Netherlands.
Gert Kwakkel, VUmc MS Center Amsterdam and Department of Rehabilitation Medicine, VU University Medical Center, Amsterdam, The Netherlands/Department of Neurorehabilitation, Reade Center of Rehabilitation and Rheumatology, Amsterdam, The Netherlands/Department of Physical Therapy and Human Movement Sciences, Northwestern University, Chicago, IL, USA.
References
- 1. Compston A, Coles A. Multiple sclerosis. Lancet 2008; 372: 1502–1517. [DOI] [PubMed] [Google Scholar]
- 2. Browne P, Chandraratna D, Angood C, et al. Atlas of multiple sclerosis 2013: A growing global problem with widespread inequity. Neurology 2014; 83: 1022–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. De Groot V, Beckerman H, Twisk JW, et al. Vitality, perceived social support and disease activity determine the performance of social roles in recently diagnosed multiple sclerosis: A longitudinal analysis. J Rehabil Med 2008; 40: 151–157. [DOI] [PubMed] [Google Scholar]
- 4. Multiple Sclerosis Council for Clinical Practice Guidelines. Fatigue and multiple sclerosis: Evidence-based management strategies for fatigue in multiple sclerosis. Washington, DC: Paralyzed Veterans of America, 1998, http://www.pva.org/atf/cf/{CA2A0FFB-6859–4BC1BC96–6B57F57F0391}/fatigue1b772.pdf [Google Scholar]
- 5. Chaudhuri A, Behan PO. Fatigue in neurological disorders. Lancet 2004; 363: 978–988. [DOI] [PubMed] [Google Scholar]
- 6. Dalgas U, Stenager E. Exercise and disease progression in multiple sclerosis: Can exercise slow down the progression of multiple sclerosis? Ther Adv Neurol Disord 2012; 5: 81–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. White LJ, Castellano V. Exercise and brain health–implications for multiple sclerosis: Part II – immune factors and stress hormones. Sports Med 2008; 38: 179–186. [DOI] [PubMed] [Google Scholar]
- 8. White LJ, Castellano V. Exercise and brain health–implications for multiple sclerosis: Part 1 – neuronal growth factors. Sports Med 2008; 38: 91–100. [DOI] [PubMed] [Google Scholar]
- 9. Langeskov-Christensen M, Heine M, Kwakkel G, et al. Aerobic capacity in persons with multiple sclerosis: A systematic review and meta-analysis. Sports Med 2015; 45: 905–923. [DOI] [PubMed] [Google Scholar]
- 10. Marrie RA, Horwitz RI. Emerging effects of comorbidities on multiple sclerosis. Lancet Neurol 2010; 9: 820–828. [DOI] [PubMed] [Google Scholar]
- 11. Heine M, van de Port I, Rietberg MB, et al. Exercise therapy for fatigue in multiple sclerosis. Cochrane Database Syst Rev 2015; 9: CD009956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Beckerman H, Blikman LJ, Heine M, et al. The effectiveness of aerobic training, cognitive behavioural therapy, and energy conservation management in treating MS-related fatigue: The design of the TREFAMS-ACE programme. Trials 2013; 14: 250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014; 348: g1687. [DOI] [PubMed] [Google Scholar]
- 14. Beurskens AJ, Bultmann U, Kant I, et al. Fatigue among working people: Validity of a questionnaire measure. Occup Environ Med 2000; 57: 353–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cardol M, Beelen A, van den Bos GA, et al. Responsiveness of the Impact on Participation and Autonomy questionnaire. Arch Phys Med Rehabil 2002; 83: 1524–1529. [DOI] [PubMed] [Google Scholar]
- 16. Wasserman K, Hansen JE, Sue DY, et al. Principles of exercise testing and interpretation: Including pathophysiology and clinical applications. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2012. [Google Scholar]
- 17. Fisk JD, Ritvo PG, Ross L, et al. Measuring the functional impact of fatigue: Initial validation of the fatigue impact scale. Clin Infect Dis 1994; 18(Suppl. 1): S79–S83. [DOI] [PubMed] [Google Scholar]
- 18. Krupp LB, LaRocca NG, Muir-Nash J, et al. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 1989; 46: 1121–1123. [DOI] [PubMed] [Google Scholar]
- 19. Gielissen MF, Verhagen S, Witjes F, et al. Effects of cognitive behavior therapy in severely fatigued disease-free cancer patients compared with patients waiting for cognitive behavior therapy: A randomized controlled trial. J Clin Oncol 2006; 24: 4882–4887. [DOI] [PubMed] [Google Scholar]
- 20. Van der Werf SP, Jongen PJ, Lycklama à, Nijeholt GJ, et al. Fatigue in multiple sclerosis: Interrelations between fatigue complaints, cerebral MRI abnormalities and neurological disability. J Neurol Sci 1998; 160: 164–170. [DOI] [PubMed] [Google Scholar]
- 21. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310. [PubMed] [Google Scholar]
- 22. Heine M, Wens I, Langeskov-Christensen M, et al. Cardiopulmonary fitness is related to disease severity in multiple sclerosis. Mult Scler 2016; 22: 231–238. [DOI] [PubMed] [Google Scholar]
- 23. Tellez N, Rio J, Tintore M, et al. Does the Modified Fatigue Impact Scale offer a more comprehensive assessment of fatigue in MS? Mult Scler 2005; 11: 198–202. [DOI] [PubMed] [Google Scholar]
- 24. Geidl W, Semrau J, Pfeifer K. Health behaviour change theories: Contributions to an ICF-based behavioural exercise therapy for individuals with chronic diseases. Disabil Rehabil 2014; 36: 2091–2100. [DOI] [PubMed] [Google Scholar]
- 25. Motl RW. Lifestyle physical activity in persons with multiple sclerosis: The new kid on the MS block. Mult Scler 2014; 20: 1025–1029. [DOI] [PubMed] [Google Scholar]
- 26. Sangelaji B, Smith CM, Paul L, et al. The effectiveness of behaviour change interventions to increase physical activity participation in people with multiple sclerosis: A systematic review and meta-analysis. Clin Rehabil 2016; 30: 559–576. [DOI] [PubMed] [Google Scholar]
- 27. Asano M, Duquette P, Andersen R, et al. Exercise barriers and preferences among women and men with multiple sclerosis. Disabil Rehabil 2013; 35: 353–361. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.