Abstract
Background:
No consensus is available regarding the best method for measuring tibiofemoral joint space width (JSW) on radiographs to quantify joint changes after injury. Studies that track articular cartilage thickness after injury frequently use patients’ uninjured contralateral knees as controls, although the literature supporting this comparison is limited.
Purpose:
(1) To compare JSW measurements using 2 established measurement techniques in healthy control participants and (2) to determine whether the mean JSW of the uninjured contralateral knee in a cohort with anterior cruciate ligament (ACL) reconstruction is different from that obtained from a true control population.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
Medial and lateral JSWs were measured on standardized, bilateral, semiflexed metatarsophalangeal positioning, posteroanterior radiographs of 60 healthy individuals (26 females; mean ± SD age, 25 ± 6.2 years; no history of knee injury) via 2 published techniques: a computerized surface-delineation method (surface-fit method) and a manual digitization method (midpoint method). Bland-Altman method was used to examine the agreement between JSW measurements obtained with the 2 methods and to examine the agreement between measurements obtained on left and right knees within a participant for each measurement method. Within- and between-participant variance components and intraclass correlation coefficients (ICCs) were computed for JSW measurements corresponding to each method. Two-sample t tests were used to compare the surface-fit method measurements of mean JSW of the true control group (n = 60) with the previously published mean JSW measurements from the Multicenter Orthopaedics Outcomes Network (MOON) nested cohort of 262 contralateral uninjured knees 2 to 3 years after ACL reconstruction.
Results:
For JSW in the medial compartment, the surface-fit method had lower within-participant interknee variability (σ2 within, 0.064; 95% CI, 0.04-0.09) compared with the midpoint method (σ2 within, 0.28; 95% CI, 0.20-0.43) and a higher ICC (0.93 vs 0.65; P < .001). Lateral JSW values were similar for the surface-fit method (σ2 within, 0.27; 95% CI, 0.18-0.43) and the midpoint method (σ2 within, 0.20; 95% CI, 0.14-0.31), with ICCs of 0.75 and 0.77, respectively (P = .80). With the surface-fit method, mean JSW measurements of the medial and lateral compartments of a control population were not significantly different from the contralateral uninjured knees of patients after ACL reconstruction.
Conclusion:
For measuring medial JSW, the surface-fit method was less variable across knees within a participant than the midpoint method, as evidenced by larger ICCs and lower interknee variability. For measuring lateral JSW, the 2 methods were similar. The JSW measurements of uninjured contralateral knees of patients with ACL reconstruction at 2 to 3 years postsurgery were not significantly different from those of a cohort of healthy control participants. Future work should be performed to demonstrate the validity of these methods for documenting change over time in the ACL-reconstructed knee.
Keywords: knee, osteoarthritis, joint space width, radiography, imaging
Quantitative methods are required to objectively measure structural changes in the knee due to osteoarthritis (OA) progression on radiographs. The most commonly used technique is to measure joint space narrowing by tracking changes in joint space width (JSW), which has been shown to approximate the articular cartilage thickness in the medial aspect of the joint.3
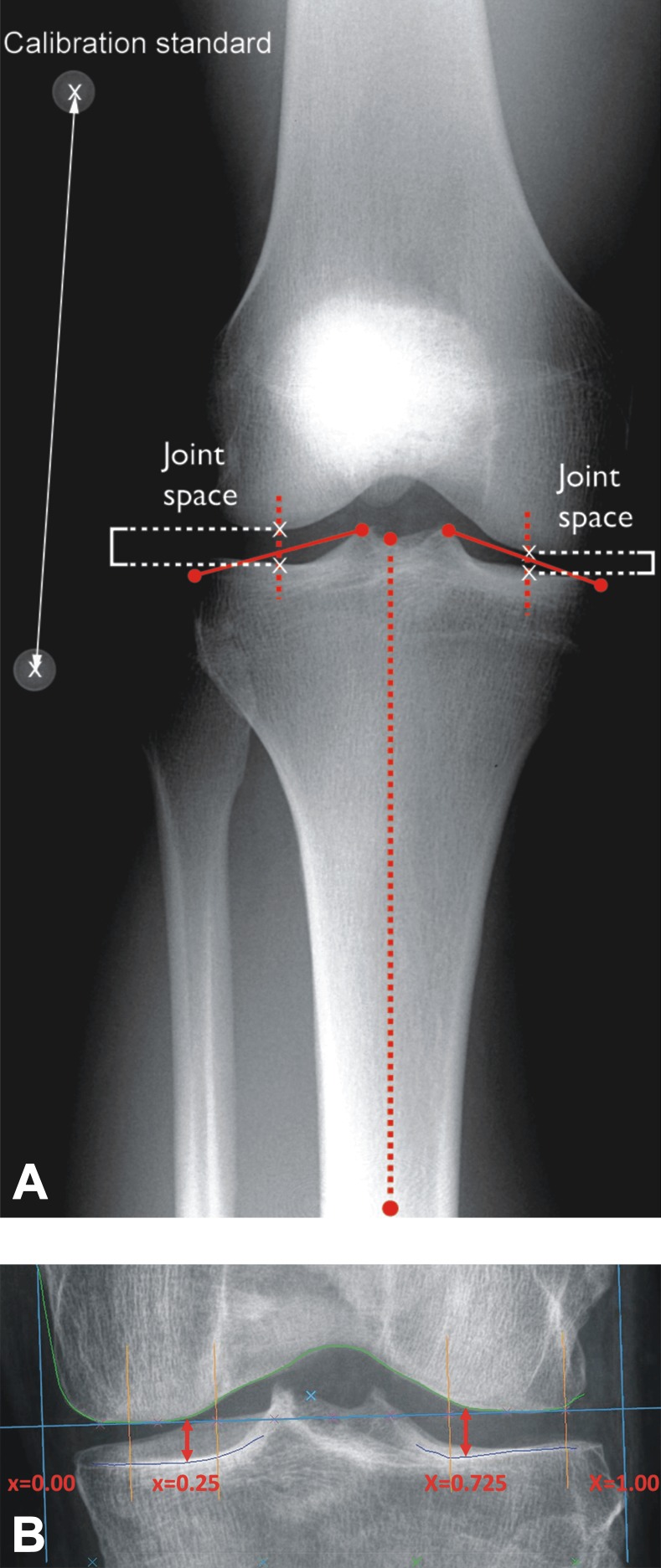
Although several methods for measuring tibiofemoral JSW on radiographs have been developed,11,13,17,26,32 the optimal method has yet to be determined.15 Two methods have been used to evaluate JSW changes in patients following anterior cruciate ligament (ACL) injury: the “midpoint” method and the “surface-fit” method.15–17,26 The midpoint method measures the medial and lateral JSW at locations on the tibia defined by the midpoint of a line connecting the tibial spine to the most medial or lateral aspect of the tibial plateau (Figure 1A).15,28 The landmarks are manually digitized by use of a computer tablet.26 The surface-fit method uses an automated surface delineation algorithm to define the tibiofemoral articular surfaces so that the JSW can be measured at specific locations within the medial and lateral compartments (Figure 1B).17 Previous studies have suggested that the locations most sensitive to change in the medial and lateral compartments are those 25% and 72.5% of the distance from the medial edge of the femoral condyle, respectively (denoted as JSW0.25 and JSW0.725).17,23,31 The agreement between these 2 methods has not been examined.
Figure 1.
(A) Midpoint method: The joint space widths (JSWs) for the medial and lateral compartments were measured between the tibial and femoral surfaces at the midpoints of the lines depicting each compartment and parallel to the long axis of the tibia. (B) Surface-fit method: The x-axis of the coordinate system was defined by a line (shown in blue) tangent to the edge of the femoral condyles in both compartments. The y-axis was defined by a line in the medial compartment perpendicular to the x-axis and tangent to the peripheral edge of the femur (shown in blue). A line defining x = 1.0 was tangent to the peripheral edge of the femur in the lateral compartment (shown in blue). The JSW in the medial compartment was measured. The surface fits for the femur and tibia are shown in green and purple. The JSW in the medial and lateral compartments was measured between these 2 surfaces along the x-axis at x = 0.25 and x = 0.725, respectively (red arrows).
Studies that track articular cartilage thickness after ACL injury frequently use the patients’ uninjured contralateral knees as controls.22 This practice is based on the assumptions that the contralateral knee is not affected after joint injury and that there are no clinically relevant side-to-side differences in JSW via magnetic resonance imaging (MRI) within younger individuals.4 However, data supporting these assumptions are limited.
The first objective of this study was to examine the agreement between measurements made with the midpoint and surface-fit methods in an active control cohort with no history of knee injuries.19 Additionally, assuming that the JSWs in the 2 knees of a healthy control participant should be nearly equivalent, the second objective was to determine which method has lower interknee (ie, within-participant) variability relative to between-participant knee variability. We hypothesized that the surface-fit method would have lower interknee variability in both the medial and lateral compartments. The final study objective was to compare the JSW of the surface-fit method from an active healthy cohort with no history of knee injuries19 with the values obtained from the uninjured contralateral control knees of ACL-reconstructed patients 2 years postoperatively from the Multicenter Orthopaedics Outcomes Network (MOON) nested cohort study.21,22 We hypothesized that there would be no difference in the mean JSW measurements between the uninjured contralateral knees of the ACL-reconstructed patients21,22 and the knees of active participants with no history of knee injury.20
Methods
Healthy Control Cohort
This study was approved by an institutional review board, and all participants granted their informed consent. The healthy control cohort19 consisted of 60 healthy volunteers (26 females; mean age, 25 ± 6.2 years) who were previously recruited into a matched control group for an ongoing clinical trial evaluating outcomes after ACL reconstruction (NCT00434837).1 Participants had no history of injury to either knee, no evidence of degenerative arthritis on radiographs, and no diseases that would predispose a patient to OA.
MOON Contralateral Cohort
The nested MOON cohort21,22 consisted of 262 individuals (148 females; mean age, 20 ± 5.0 years) who were injured in sport and underwent ACL reconstruction with autograft or allograft in a previously uninjured knee. All patients were younger than 35 years, and none had undergone ACL revision surgery or contralateral ACL reconstruction. Patients’ uninjured contralateral knees were considered as the control group for the MOON study comparison. JSW was measured by use of the surface-fit method on radiographs taken with the metatarsophalangeal (MTP) view.10,15 Medial and lateral JSWs in this cohort were measured at the same locations (JSW0.25 and JSW0.725 for the medial and lateral compartments, respectively).
Radiographs
For the healthy control cohort,19 bilateral posteroanterior radiographs of the knees were taken with semiflexed MTP positioning, as described by Buckland-Wright,10 at the participants’ baseline visit. These radiographs were used to measure medial and lateral JSWs with both the surface-fit and midpoint methods. The images of uninjured contralateral knees from the MOON cohort were obtained following the same protocol.22
Midpoint Method
JSW measurement analysis with the midpoint method was performed by a trained investigator (N.M.) on a MATLAB (The MathWorks Inc) program.15,26 The medial and lateral edges of each compartment were identified and digitized by use of a mouse. The examiner similarly digitized the midpoints of the distal tibial shaft and the proximal intercondylar midpoint. These points were connected automatically to establish the long axis of the tibial shaft. The program also constructed lines between 2 digitized points representing the left and right edges of the medial and lateral compartments. Midpoint lines that bisected each of the respective tibial compartment lines were automatically drawn parallel to the long axis of the tibia (Figure 1A).
The intersections of the femoral condyle and tibial compartments with the midpoint lines were then digitized for each compartment by the investigator. If the inter-rim distance was not equal to 0 (ie, if the anterior and posterior edges of the tibial plateau were not perfectly aligned), the program allowed the investigator to mark each rim, and it calculated the midpoint of the inter-rim distance. This point was then used as the tibial intersection for the midpoint line.
The distances between the femoral and tibial intersections with the bisecting midpoint line for each compartment were calculated as the JSW of each compartment. To control magnification error, the computer algorithm automatically determined the location of the centers of 2 spheres, which were embedded a known distance apart within the calibration standard and placed on the patient’s knee at the time of imaging, using an edge detection algorithm. The distance between the 2 centers was calculated to determine the magnification factor.
Surface-Fit Method
The fundamentals of the algorithm for the surface-fit method are as follows: A semi-automated software tool, developed by Duryea et al,16,17 was used to delineate the edges of the femoral condyles and tibial plateaus in both compartments. For the femoral condyle, this was done by creating a gradient image and ordering pixels at each horizontal location by grayscale value. The pixels with the highest grayscale were marked on the image, and isolated pixels were eliminated by use of a region-growing algorithm. Following this elimination, a partial femoral contour was delineated by connecting pixels whose grayscale value exceeded a predetermined value. The full contour was determined by applying a derivative-based edge-detection algorithm on the original grayscale image, with both ends of the partial contour used as starting points.16 The tibial plateau was determined by use of the raw grayscale image rather than the gradient image, with the largest, highest-intensity set of connected pixels chosen as the correct contour.16
Once the femoral and tibial contours were delineated, a coordinate system was defined on the radiograph (Figure 1B). The computer-delineated femoral edge was used to automatically draw a line tangent to each of the femoral condyles to define the x-axis. A trained investigator, using a semi-automated mouse-based computer tool, created 2 other lines perpendicular to the x-axis, one tangent to the medial edge of the femoral condyle (x = 0.0) and the other tangent to the lateral edge (x = 1.0). All JSW measurements were made with respect to this coordinate system. The JSW measurements with the surface-fit method were performed by the investigator who developed the algorithm (J.D.). The readings were done viewing the left and right knees for each participant simultaneously.
The coordinate system was used to make JSW measurements at fixed points along the x-axis. JSW was found by calculating the distance from the tibial plateau to the femur at specific x-values in a direction parallel to the y-axis (assumed to be the weightbearing direction). For this study, we reported the medial JSW measurements at 25% of the distance along the x-axis as defined above (JSW0.25) and the lateral JSW measurements as 72.5% of the distance along the x-axis (JSW0.725).
Statistical Analysis
The Bland-Altman method7,8 was used to examine the agreement between JSW measurements obtained using the 2 methods. Estimates of the systematic difference between methods (ie, bias) and corresponding limits of agreement were derived by use of analyses of variance (ANOVAs), accounting for the correlation between measurements from left and right knees within an individual. The corresponding limits of agreement were expected to enclose 95% of observed differences for individual measurements, assuming a normal distribution. Similarly, the agreement between measurements obtained on left and right knees within an individual was examined for each method by use of standard Bland-Altman method.2,6 All analyses were performed separately for the medial and lateral compartments. In addition to the Bland-Altman analyses, the intraclass correlation coefficient (ICC) for each method was computed as σ2 between/(σ2 between + σ2 within), where σ2 between represented the interknee variability of JSW between participants and σ2 within represented the interknee variability within participants. The higher the ICC for a particular method, the less variable the JSW measurements were between knees relative to across-participant knee variability for this population of uninjured individuals. Mixed-model ANOVA was used to estimate variance components and corresponding 95% CIs for the ICC and σ2 within, which were computed based on an SAS macro.20 ICCs were compared across methods within compartment based on the z test proposed by Donner and Zou.14 Last, 2-sample t tests were used to compare the mean JSW of the healthy control participants19 with the uninjured contralateral knees of the MOON cohort,21,22 both of which were analyzed with the surface-fit method. Student t tests were performed separately for the medial and lateral compartments.
Results
Due to poor image quality, which rendered the radiographs unable to be analyzed with one or both methods, 7 participants were excluded in the medial JSW analysis, leaving 53 sets of radiographs available for the medial compartment analyses. In the lateral JSW analysis, 8 additional participants were excluded, leaving 45 sets of radiographs for lateral compartment analyses.
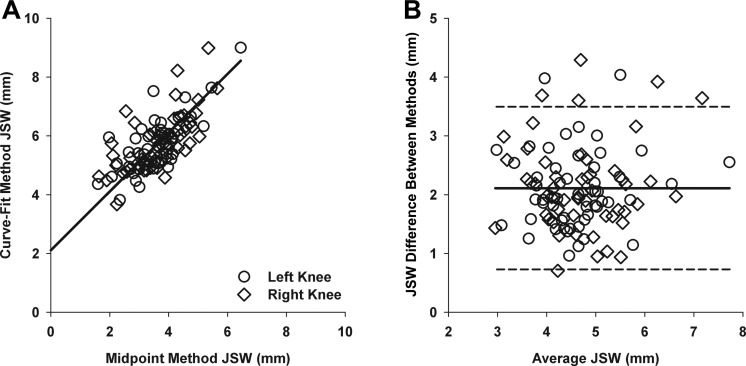
Comparison of Midpoint and Surface-Fit Methods—Medial Compartment
Figure 2 shows the comparison of medial compartment JSW measurements between the 2 methods. The 2 measurement techniques demonstrated significantly different mean medial compartment JSW, with the surface-fit method resulting in larger estimates of JSW than the midpoint method (5.71 mm vs 3.60 mm, mean difference = 2.11 mm; 95% CI, 1.95-2.28, P < .001). The estimated limits of agreement ranged from 0.72 mm to 3.50 mm.
Figure 2.
Comparison of the surface-fit and midpoint methods for measuring the joint space width (JSW) in the medial compartment. The surface-fit method JSW values for each participant and each knee (left: open circles; right: open diamonds) are plotted vs measurements obtained using the (A) midpoint method. The (B) Bland-Altman plot displays the differences between the methods (surface-fit and midpoint) vs mean JSW for the 2 methods. The solid line represents the mean difference, and the dashed lines represent the 95% limits of agreement.
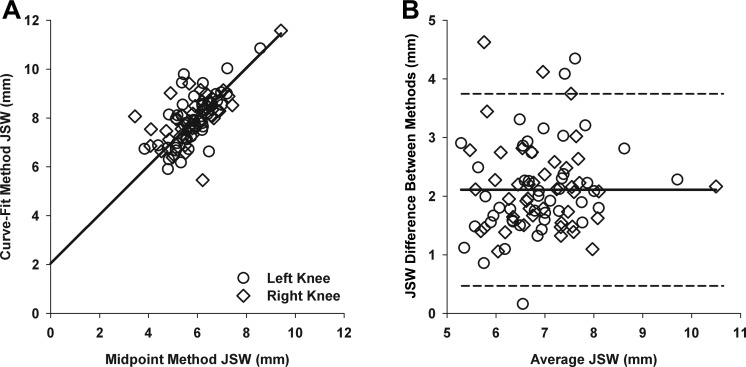
Comparison of Midpoint and Surface-Fit Methods—Lateral Compartment
Figure 3 shows the comparison of lateral compartment JSW measurements between the 2 methods. The 2 measurement techniques demonstrated significantly different mean lateral compartment JSW, with the surface-fit method resulting in larger estimates of JSW than the midpoint method (7.94 mm vs 5.84 mm, mean difference = 2.10 mm; 95% CI, 1.88-2.32, P < .001). The estimated limits of agreement ranged from 0.47 mm to 3.75 mm.
Figure 3.
Comparison of the surface-fit and midpoint methods for measuring the joint space width (JSW) in the lateral compartment. Surface-fit method JSW values for each participant and each knee (left: open circles; right: open diamonds) are plotted vs measurements obtained using the (A) midpoint method. The (B) Bland-Altman plot displays the differences between the methods (surface-fit minus midpoint) vs mean JSW for the 2 methods. The solid line represents the mean difference, and the dashed lines represent the 95% limits of agreement.
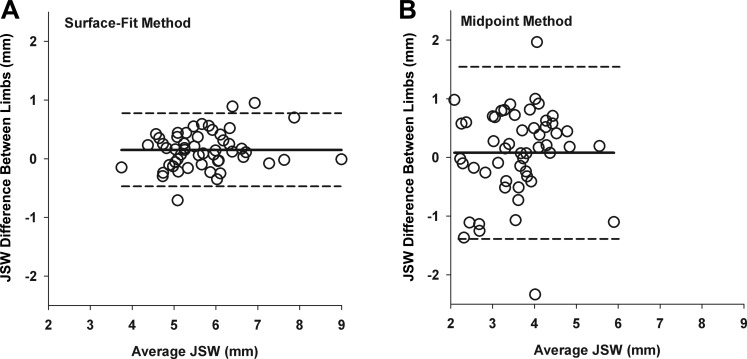
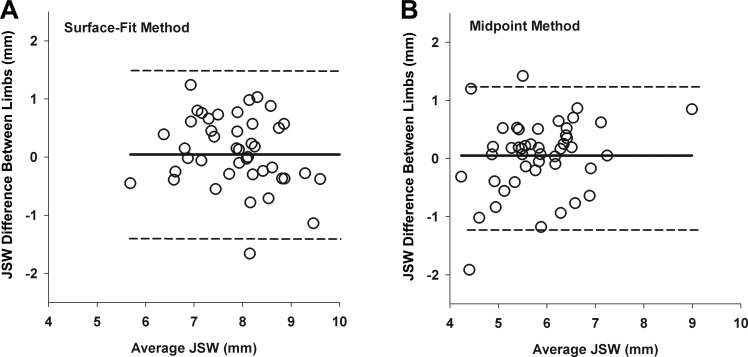
Left-Right Comparison of Both Methods—Medial Compartment
Figure 4 highlights the comparison of JSW measurements for the medial compartment from right and left knees for the surface-fit and midpoint methods. The surface-fit method resulted in a significant difference between mean JSW in right and left knees (5.78 mm vs 5.63 mm, mean difference = 0.15 mm; 95% CI, 0.06-0.24; P = .0013). For the midpoint method, there was no evidence of a systematic difference between knees, with a corresponding wider CI (3.64 mm vs 3.56 mm, mean difference = 0.08 mm; 95% CI, –0.13 to 0.29; P = .43). The estimated limits of agreement, representing the approximate range of side-to-side differences to be expected, were much narrower for the surface-fit method (0.47 to 0.77) than the midpoint method (–1.39 to 1.55).
Figure 4.
Bland-Altman plots comparing the left to right differences in joint space width (JSW) for the medial compartment for (A) the surface-fit method and (B) the midpoint method. The solid bars represent the mean differences, and the dashed lines represent the limits of agreement.
The 2 methods resulted in different estimates of variance components when measuring JSW in the medial compartment. The ICCs were 0.93 (95% CI, 0.89-0.96) for the surface-fit method and 0.65 (95% CI, 0.49-0.79) for the midpoint method (P < .001). Estimated interknee (ie, between-knee, within-participant) variability was significantly less for the surface-fit method (σ2 within = 0.06; 95% CI, 0.04-0.09) compared with the midpoint method (σ2 within = 0.28; 95% CI, 0.20-0.43)].
Left-Right Comparison of Both Methods—Lateral Compartment
Figure 5 shows the comparison of lateral compartment JSW measurements between right and left knees for the 2 measurement methods. For both the surface-fit method and the midpoint method, no significant difference was found between mean JSW in right and left knees (right knee: 7.96 mm vs 7.92 mm, mean difference = 0.04 mm, 95% CI, –0.18 to 0.26, P = .69; left knee: 5.86 mm vs 5.81 mm, mean difference = 0.05 mm; 95% CI, –0.13 to 0.24, P = .59). The estimated limits of agreement were also very similar for the 2 methods (surface-fit method: –1.41 to 1.49; midpoint method: –1.18 to 1.29).
Figure 5.
Bland-Altman plots comparing the left to right differences in joint space width (JSW) for the lateral compartment for (A) the surface-fit method and (B) the midpoint method. The solid bars represent the mean differences, and the dashed lines represent the limits of agreement.
For the lateral compartment, the ICCs were 0.75 (95% CI, 0.60-0.85) for the surface-fit method and 0.77 (95% CI, 0.63-0.87) for the midpoint method, which were not significantly different (P = .80), with similar within-participant interknee estimates of variability (surface-fit method: σ2 within = 0.27, 95% CI, 0.18-0.43; midpoint method: σ2 within = 0.20, 95% CI, 0.14-0.31).
JSW Comparison of Healthy Control Participants Versus Uninjured Knees of the MOON Cohort
The comparison of the JSW measurements between the healthy control cohort and the uninjured contralateral control knees from the MOON cohort using the surface-fit method revealed no significant differences within the medial or lateral compartments (right medial control, P = .49; left medial control, P = .07; left lateral control, P = .37; right lateral control, P = .24) (Table 1). Mean JSW measurements for the healthy cohort were within approximately 0.2 mm of the MOON cohort, representing relative differences of 5% or less.
TABLE 1.
Medial and Lateral JSWs for the Healthy Control Knees in the Present Study and the Contralateral Knees in the MOON Cohorta
| Compartment | Leg | Healthy Control Cohort19 | MOON Cohort22 | |
|---|---|---|---|---|
| Midpoint | Surface-fit | |||
| Medial | Left | 3.56 ± 0.87 | 5.63 ± 0.92 | 5.54 ± 0.86 |
| Right | 3.64 ± 0.95 | 5.78 ± 0.98 | ||
| Lateral | Left | 5.81 ± 0.85 | 7.92 ± 1.08 | 7.77 ± 1.03 |
| Right | 5.86 ± 1.01 | 7.96 ± 1.02 | ||
aValues expressed in millimeters as mean ± SD. JSW, joint space width; MOON, Multicenter Orthopaedics Outcomes Network.
Discussion
We observed significant differences between mean JSW values measured with the midpoint method and those measured with the surface-fit method. The mean JSW values for the surface-fit method were approximately 2 mm larger than those of the midpoint method on both the medial and lateral sides. This finding may be explained by how each method establishes the point of measurement on the tibia. While the surface-fit method uses the lowest point on the tibial plateau joint surface as its reference for measurement, the midpoint method uses the midpoint between the anterior and posterior rims of the tibia. Additionally, the midpoint method uses calibration beads placed at the midpoint of the knee to account for magnification error due to the x-ray projection. In our study, the surface-fit method did not include a calibration adjustment, as we assumed it would be consistent across knees within a participant. This difference could further contribute to the larger JSW values for the surface-fit method.
The surface-fit method was shown to be less variable across knees within a participant than the midpoint method for measuring medial JSW, as evidenced by larger ICCs and lower within-participant interknee variance term. For measurement of lateral JSW, the 2 methods were essentially the same.
Methodological differences may account for the greater ICCs for the surface-fit method compared with the midpoint method. The most obvious difference is that the surface-fit method uses image-processing software, making it less prone to human error. The surface-fit method uses an automatic edge-detection algorithm to delineate the tibial and femoral contours of the cartilage and uses a fixed coordinate system to measure at consistent locations across the joint (see Figure 1B). In contrast, the midpoint method measures JSW at the midpoint of the tibial spine and either the medial or lateral edge of the tibia, landmarks selected by the user (see Figure 1A). Accordingly, measurement location for the midpoint method was more variable. Although studies have shown that computer-assisted methods are more sensitive and reliable than manual methods,9,15 our findings support the need to use complete computerization and standardization of methods to eliminate user error altogether. If the midpoint method is used, this error could potentially be reduced by ensuring proper and adequate training of the investigator to increase consistency of selected points as well as choosing high-quality radiographs to make anatomic landmarks as clear as possible.
The ICC of the surface-fit method for measuring medial JSW was higher than that of the lateral compartment, while this was not the case for the midpoint method. Previous studies have shown that the lateral compartment JSW is significantly more variable than medial JSW,12,25,26 which could be due to the fact that the patient positioning protocol was originally designed to optimally align the medial compartment relative to the x-ray tube. This variability may account for the lower ICC for the surface-fit method for measuring lateral JSW compared to the medial JSW, and it indicates an area where the technique can be refined—namely, optimizing the imaging technique to allow for improved alignment and measurement of the lateral compartment.
Using the surface-fit method, which is becoming increasingly popular to measure knee JSW to document OA progression,5,18,22,24 we demonstrated that the mean JSWs of healthy control participants did not significantly differ from the contralateral JSWs of patients with unilateral ACL injury 2 to 3 years after reconstruction, in both the medial and lateral compartments. This finding supports our hypothesis and indicates that using the uninjured contralateral knee from patients with a unilateral injury as a control is a valid practice. These results support those of Tourville et al,31 who used the midpoint method to show that JSW differences in the uninjured knees of patients with ACL reconstruction did not change significantly over time. The present study is the first, however, to validate the uninjured contralateral control assumption using the surface-fit method, which we have shown to be more reliable than the midpoint method for measuring JSW in the medial compartment and hence able to detect more subtle differences.
The higher ICC and lower variance component for medial JSW measurements of the surface-fit method indicate that JSWs of an individual’s left and right knees are similar in the medial compartment, further supporting the use of the contralateral knee as a control in this compartment. Tourville et al31 reported similar findings using radiographs, and Argentieri et al4 reported no side-to-side differences in tibial cartilage thickness of 88 healthy controls in either compartment using MRI.
Uninjured contralateral controls would facilitate the study of structural differences within the joint, as both joints in an individual are subject to the same systemic risk factors, as suggested by Roemer et al.29 In this way, uninjured contralateral control knees offer ideal constraint of comorbid factors including age, body mass index, smoking, and activity level as well as other unknown potentially genetic factors. Furthermore, the use of uninjured contralateral control knees eliminates the need to recruit a separate control group for comparative studies that use JSW to investigate progression of OA after ACL injury. Using an uninjured contralateral control group will make these studies more cost-effective and easier to conduct and will increase follow-up rates and decrease patient dropout.
However, using the uninjured contralateral knee as a control entails risks, specifically in an ACL-reconstructed cohort. An analysis of the MOON cohort of 2488 primary ACL reconstructions showed that younger age and higher activity level were risk factors for contralateral ACL tear,23 findings that corroborated the results of a systematic review of risk factors of contralateral ACL injury.30 Furthermore, Paterno et al27 reported that female athletes sustain contralateral ACL injuries at a higher rate than male athletes. Thus, it is possible that the uninjured control knee could be injured in studies of ACL reconstruction outcome and thus be unable to serve as a suitable control long-term. Other factors, such as biomechanical changes in both knees subsequent to ACL injury, can also increase risk of contralateral injury30 and change a patient’s predisposition to OA. Additionally, it is possible that studies designed to use the uninjured knee as a contralateral control may have a bias toward showing less disease progression if changes are occurring in both joints.
Despite the finding that the surface-fit method had lower within-participant interknee variability in measuring medial compartment JSW than the midpoint method, the surface-fit method was sensitive enough to detect a small, statistically significant difference in medial JSW between right and left knees. This systematic right-left difference was less than 0.15 mm and therefore was not clinically relevant. The midpoint method failed to detect the systematic right-left JSW difference, most likely due to the higher within-participant interknee variability, thus limiting statistical power.
Our analysis translates the novel application of a radiographic measurement technique, which has been validated to measure the longitudinal progression of primary OA, to the earliest stages of posttraumatic OA following joint injury. The imaging technique used here, which is analogous to the fixed-flexion radiographic approach, could potentially be implemented in practice to detect posttraumatic OA in patients following joint injury. The surface-fit method software, although currently proprietary and used primarily for research purposes, has the potential to become commercially available and accessible for clinical use. Despite the finding that the surface-fit method produced larger JSW values than the midpoint method, the tool’s clinical utility would not be affected if it were used consistently across an entire population of patients.
Our study is limited in that it represents a cross section of participants and does not account for changes in JSW over time in healthy individuals. However, the cohort consisted of healthy participants without evidence of radiographic OA. Further studies should evaluate the generalizability of these results when using these methods to examine arthritic knees or those progressing to OA.
Additionally, the demographics of the healthy control cohort and the MOON cohort differed: The healthy control cohort had a mean age of 25 years and consisted of 43% females, whereas the MOON cohort had a mean age of 20 years and consisted of 56% females. Further, the healthy cohort was limited by the exclusion of radiographs (7 [12%] in the medial compartment analysis and 15 [25%] in the lateral compartment analysis) that had inadequate resolution for landmark detection by one or both techniques, even though a protocol for precise patient positioning was used. This may have been due to patient motion or other technical errors. For JSW measurements of the medial compartment, the midpoint and surface-fit methods were unable to determine JSW from 2 and 1 radiograph sets, respectively. Measurements in the lateral compartment were more difficult, as the midpoint and surface-fit methods were unable to perform measurements on 3 and 8 radiograph sets, respectively. Image acquisition and the ability to analyze images have become increasingly important in large studies, so care should be taken in such studies to improve and optimize image quality and consistency.
The ICCs of the lateral compartment measurements indicate that there is substantial room for improvement in measuring JSW in this location. One particular improvement would entail optimizing the imaging technique for the lateral compartment, making the image more compatible with analysis tools. Future studies to improve the measurements in the lateral compartment are needed.
Conclusion
The surface-fit method proved to be superior for measuring JSW in the medial compartment but was similar to the midpoint method for measurements of lateral compartment JSW. Furthermore, no differences were found between the mean JSW measurements of healthy control participants and the uninjured contralateral knees of patients 2 to 3 years after ACL reconstruction surgery, demonstrating that the uninjured contralateral knees may serve as a valid control for outcome studies of ACL reconstruction in which OA progression is being documented.
Footnotes
The article content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. One or more of the authors have declared the following potential conflict of interest or source of funding: The study was funded by the National Institutes of Health [R01-AR047910, R01-AR053684, and P20-GM104937 (Bio-engineering Core)] and the Lucy Lippitt Endowment. B.C.F. is the cofounder of Miach Orthopaedics and has received travel support from the ACL Study Group. J.D. is a consultant for Boston Imaging Core Lab LLC. M.H.J. is a consultant for Boston Imaging Core Lab LLC.
Ethical approval for this study was obtained from Lifespan Research Protection Office (IRB registration No. 00000396, 00004624, and 00000482).
References
- 1. Akelman MR, Fadale PD, Hulstyn MJ, et al. Effect of matching or overconstraining knee laxity during anterior cruciate ligament reconstruction on knee osteoarthritis and clinical outcomes: a randomized controlled trial with 84-month follow-up. Am J Sports Med. 2016;44:1660–1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Altman DG, Bland JM. Measurement in medicine: the analysis of method comparison studies. Statistician. 1983;32:307–317. [Google Scholar]
- 3. Altman R, Brandt KD, Hochberg MC, Moskowitz R. Design and conduct of clinical trials in patients with osteoarthritis. Osteoarthritis Cartilage. 1996;4:217–243. [DOI] [PubMed] [Google Scholar]
- 4. Argentieri EC, Sturnick DR, DeSarno MJ, et al. Changes to the articular cartilage thickness profile of the tibia following anterior cruciate ligament injury. Osteoarthritis Cartilage. 2014;22:1453–1460. [DOI] [PubMed] [Google Scholar]
- 5. Benichou OD, Hunter DJ, Nelson DR, et al. One-year change in radiographic joint space width in patients with unilateral joint space narrowing: data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken). 2010;62:924–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 7. Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–160. [DOI] [PubMed] [Google Scholar]
- 8. Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17:571–582. [DOI] [PubMed] [Google Scholar]
- 9. Bruyere O, Henrotin YE, Honore A, et al. Impact of the joint space width measurement method on the design of knee osteoarthritis studies. Aging Clin Exp Res. 2003;15:136–141. [DOI] [PubMed] [Google Scholar]
- 10. Buckland-Wright C. Review of the anatomical and radiological differences between fluoroscopic and non-fluoroscopic positioning of osteoarthritic knees. Osteoarthritis Cartilage. 2006;14:A19–A31. [DOI] [PubMed] [Google Scholar]
- 11. Buckland-Wright JC, Macfarlane DG, Jasani MK, Lynch JA. Quantitative microfocal radiographic assessment of osteoarthritis of the knee from weight bearing tunnel and semiflexed standing views. J Rheumatol. 1994;21:1734–1741. [PubMed] [Google Scholar]
- 12. Buckland-Wright JC, Macfarlane DG, Williams SA, Ward RJ. Accuracy and precision of joint space width measurements in standard and macroradiographs of osteoarthritic knees. Ann Rheum Dis. 1995;54:872–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dacre JE, Huskisson EC. The automatic assessment of knee radiographs in osteoarthritis using digital image analysis. Br J Rheumatol. 1989;28:506–510. [DOI] [PubMed] [Google Scholar]
- 14. Donner A, Zou G. Testing the equality of dependent intraclass correlation coefficients. J R Stat Soc Ser D. 2002;51:367–379. [Google Scholar]
- 15. Dupuis DE, Beynnon BD, Richard MJ, Novotny JE, Skelly JM, Cooper SM. Precision and accuracy of joint space width measurements of the medial compartment of the knee using standardized MTP semi-flexed radiographs. Osteoarthritis Cartilage. 2003;11:716–724. [DOI] [PubMed] [Google Scholar]
- 16. Duryea J, Li J, Peterfy CG, Gordon C, Genant HK. Trainable rule-based algorithm for the measurement of joint space width in digital radiographic images of the knee. Med Phys. 2000;27:580–591. [DOI] [PubMed] [Google Scholar]
- 17. Duryea J, Zaim S, Genant HK. New radiographic-based surrogate outcome measures for osteoarthritis of the knee. Osteoarthritis Cartilage. 2003;11:102–110. [DOI] [PubMed] [Google Scholar]
- 18. Eckstein F, Boudreau R, Wang Z, et al. Comparison of radiographic joint space width and magnetic resonance imaging for prediction of knee replacement: a longitudinal case-control study from the Osteoarthritis Initiative. Eur Radiol. 2016;26:1942–1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fleming BC, Fadale PD, Hulstyn MJ, et al. The effect of initial graft tension after anterior cruciate ligament reconstruction: a randomized clinical trial with 36-month follow-up. Am J Sports Med. 2013;41:25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hankinson SE, Manson JE, Spiegelman D, Willett WC, Longcope C, Speizer FE. Reproducibility of plasma hormone levels in postmenopausal women over a 2-3-year period. Cancer Epidemiol Biomarkers Prev. 1995;4:649–654. [PubMed] [Google Scholar]
- 21. Jones MH, Reinke E, Duryea J, et al. Predictors of lateral compartment joint space difference at a minimum of two years after ACL reconstruction: data from the MOON Onsite Cohort. Orthop J Sports Med. 2016;4:1. [Google Scholar]
- 22. Jones MH, Spindler KP, Fleming BC, et al. Meniscus treatment and age associated with narrower radiographic joint space width 2-3 years after ACL reconstruction: data from the MOON onsite cohort. Osteoarthritis Cartilage. 2015;23:581–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Consortium M, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lu B, Driban JB, Duryea J, McAlindon T, Lapane KL, Eaton CB. Milk consumption and progression of medial tibiofemoral knee osteoarthritis: data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken). 2014;66:802–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lynch JA, Buckland-Wright JC, Macfarlane DG. Precision of joint space width measurement in knee osteoarthritis from digital image analysis of high definition macroradiographs. Osteoarthritis Cartilage. 1993;1:209–218. [DOI] [PubMed] [Google Scholar]
- 26. Oksendahl HL, Gomez N, Thomas CS, et al. Digital radiographic assessment of tibiofemoral joint space width: a variance component analysis. J Knee Surg. 2009;22:205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22:116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ravaud P, Chastang C, Auleley GR, et al. Assessment of joint space width in patients with osteoarthritis of the knee: a comparison of 4 measuring instruments. J Rheumatol. 1996;23:1749–1755. [PubMed] [Google Scholar]
- 29. Roemer FW, Jarraya M, Kwoh CK, et al. Brief report: symmetricity of radiographic and MRI-detected structural joint damage in persons with knee pain—the Joints on Glucosamine (JOG) Study. Osteoarthritis Cartilage. 2015;23:1343–1347. [DOI] [PubMed] [Google Scholar]
- 30. Sward P, Kostogiannis I, Roos H. Risk factors for a contralateral anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2010;18:277–291. [DOI] [PubMed] [Google Scholar]
- 31. Tourville TW, Johnson RJ, Slauterbeck JR, Naud S, Beynnon BD. Assessment of early tibiofemoral joint space width changes after anterior cruciate ligament injury and reconstruction: a matched case-control study. Am J Sports Med. 2013;41:769–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Vignon E, Piperno M, Le Graverand MP, et al. Measurement of radiographic joint space width in the tibiofemoral compartment of the osteoarthritic knee: comparison of standing anteroposterior and Lyon schuss views. Arthritis Rheum. 2003;48:378–384. [DOI] [PubMed] [Google Scholar]