Abstract
Study Design:
Retrospective cohort study.
Objective:
The S2-alar-iliac (S2AI) technique has been described as an alternative method for pelvic fixation in place of iliac screws (ISs) in spinal deformity surgery. The objective of this study was to analyze the impact of S2AI screws on radiographical outcomes, including spinopelvic parameters.
Methods:
A retrospective review of 17 patients receiving ISs and 46 patients receiving S2AI screws for correction of adult spinal deformity between 2010 and 2015 with minimum 1-year follow-up was conducted. Patient data on postoperative complications, including reoperation rates and proximal junctional kyphosis (PJK), and radiographical parameters was collected and statistically analyzed.
Results:
With mean follow-up of 21.1 months, the overall reoperation rate was significantly lower in the S2AI group than in the IS group (21.7% vs 58.8%, P = .01), but the incidence of PJK was similar (32.6% vs 35.3%, P > .99). Moreover, the time to reoperation in the IS group was significantly shorter than in the S2AI group (P = .001), and the S2AI group trended toward a longer time to reoperation due to PJK (P = .08). There was a significantly higher change in pelvic incidence (PI) in the S2AI group (−6.0°) compared with the IS group (P = .001).
Conclusions:
Compared with the IS technique, the S2AI technique demonstrated a lower rate of overall reoperation, a similar rate of PJK, longer time to reoperation, and possible reduction in PI. Future studies may be warranted to clarify the mechanism of these results and how they can be translated into improved patient care.
Keywords: lumbar lordosis, lumbosacropelvic fixation, iliac screw, pelvic incidence, proximal junctional kyphosis, proximal junctional failure, S2-alar-iliac screw
Introduction
Surgical management of adult spinal deformities involving long posterior fusion remains a substantial challenge due to the high incidence of proximal junctional kyphosis (PJK)1,2 and pseudarthrosis,3,4 particularly at the L5-S1 junction. To prevent these clinically relevant complications, several efforts have been made. First, risk factors for PJK have been extensively discussed in the literature, such as overcorrection of kyphotic deformities5,6 or lumbar lordosis (LL),7 combined anterior and posterior spinal fusion,8 fusion to the sacrum,9 selection of the uppermost instrumented vertebra (UIV),2 and disruption of posterior proximal intervertebral elements.10,11 In light of these risk factors, a wide variety of treatment strategies have been explored, such as vertebral cement augmentation,12-15 dynamic spine stabilization,16 and minimally invasive instrumentation placement.17 To prevent pseudarthrosis, use of iliac screws (IS) for long-segment fusion ending at the sacrum or other pelvic fixation techniques such as the Galveston technique,18 use of bone morphogenetic protein–2 (BMP-2),19 and simultaneous or subsequent L5-S1 interbody fusion20 have been reported in the literature.
Meanwhile, the S2-alar-iliac (S2AI) technique, originally described in 2007 by Sponseller21 and Kebaish,22 has been investigated as an alternative pelvic fixation method.23-29 This technique has several theoretical advantages over the IS technique in that its insertion point is deeper than the IS technique and offset use is not usually required, as the entry point of an S2AI screw is usually in line with the S1 pedicle screws.30 According to prior retrospective, comparative studies, these theoretical merits have proven to be valid in actual clinical practice. For instance, Shabtai et al31 reported that the S2AI group had a lower rate of implant failure and less surgical revisions due to screw prominence, and Mazur et al27 and Elder et al32 found that use of the S2AI technique over the IS technique was independently protective of reoperation.
However, in spite of emerging clinical evidence demonstrating the advantages of S2AI screws, little is known about their influence on spinopelvic parameters and their effect on the proximal junction of the construct. To the best of our knowledge, only one prior study by Sponseller et al29 compared the S2AI technique with the IS technique, finding that the S2AI technique produced significantly better correction of pelvic obliquity but not improved coronal Cobb angle correction. Therefore, the objective of this study was to compare the S2AI technique with the IS technique in adult spinal deformity patients in terms of clinical and radiographical outcomes, focusing on postoperative changes in spinopelvic parameters and trends in PJK.
Materials and Methods
Patient Population
This study was conducted under an institutional review board–approved protocol (NA_00038491). From October, 2010, to February, 2015, 113 patients with the diagnosis of adult spinal deformity underwent deformity correction surgery involving sacropelvic instrumentation with ISs or S2AI screws, either as primary surgery or revision surgery, at a single institution. Patients were followed for more than 1 year with pre- and postoperative standing scoliosis radiographs depicting coronal plane alignment, and sagittal plane alignment. Spinopelvic parameters were measured pre- and postoperatively. Patients who had undergone resection of tumors of the spinal column as well as sacropelvic reconstruction with pelvic screw insertion and then subsequently developed spinal deformities were excluded as the difference in biomechanical strength could have affected clinical outcomes. Following application of these inclusion and exclusion criteria, a total of 63 patients, with 17 in the IS group and 46 in the S2AI group, were included in this study. From October 2010 to December 2013, S2AI screws and ISs were equally selected based on surgeons’ preference, but from January 2014 to February 2015, S2AIs were preferentially utilized unless there were any contraindications, such as prior history of high sacrectomy or sacral trauma, since we were aware of the improved clinical outcomes via the S2AI technique.
Surgical Procedure
All procedures were performed via an open posterior approach, and the joint capsule at the UIV was left intact. The S2AI technique was well established in our department approximately in 2012. Therefore, ISs were preferentially selected over the periods from 2010 to 2012 and S2AI instrumentation was favored from 2012 to 2015. The detailed procedures for the IS technique and the S2AI screw technique have been described previously.30,33,34 Patients required deformity correction via Smith-Peterson osteotomies or pedicle subtraction osteotomies. Anterior lumbar interbody fusion (ALIF), posterior lumbar interbody fusion (PLIF), or transforaminal lumbar interbody fusion (TLIF) were supplementally performed in some patients,19,37,38 depending on prior history of abdominal surgeries and irradiation, comorbidities, and surgeons’ preference. BMP-2 (INFUSE, Medtronic, Minneapolis, MN, USA) was used off-label for posterolateral fusion in some cases. Cement vertebroplasty at the UIV and/or UIV+1 (off-label) were also used in some cases based on surgeons’ preference.
Patient Data
Baseline characteristics including age at surgery, sex, body mass index (BMI), history of smoking, osteoporosis or osteopenia, prior history of lumbosacral surgery, preoperative diagnosis, and symptoms at initial presentation were collected. Operative data, including operated levels, number of surgical stages, total operative time, total estimated blood loss (EBL), L5-S1 interbody fusion (ALIF, PLIF, or TLIF), osteotomies utilized, total BMP-2 dosage, total length of hospital stay, and total length of intensive care unit (ICU) stay, was reviewed. Additionally, complication data was collected. Reoperation was defined as any unexpected surgery for the treatment of PJK and/or proximal junctional failure (PJF), pseudarthrosis, device failure, surgical site infection (SSI), or wound dehiscence. The reason for reoperation and the time to reoperation were also reviewed on subanalyses. PJK was defined as “proximal junctional sagittal Cobb angle between the lower endplate of the uppermost instrumented vertebra and the upper endplate of the two supra-adjacent vertebrae ≥10° and at least 10° greater than the preoperative measurement.”35 PJF, which required revision surgery, was separately analyzed. Distal device failure was defined as fractures or pull-out of devices in the L4-pelvis regions.
Radiographical Evaluation
Radiographical evaluation included measurement of pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), lumbar lordosis (LL) (defined as the angle formed between the superior end plate of L1 and superior endplate of S1), PI-LL mismatch, thoracic kyphosis (TK) (defined as the angle formed between the superior end plate of T5 and the inferior end plate of T12), sagittal vertical axis (SVA) (defined as the distance from the posterosuperior edge of the S1 to the C7 plumb-line), and Cobb angle of the coronal plane deformity. The above parameters were measured at the time of initial presentation and at last follow-up by 2 independent observers in a blinded fashion and the averages were calculated for each parameter. The fusion status was initially evaluated based on static radiographs with an assessment of bridging bone. If fusion status was unclear, computed tomography scans and/or flexion-extension dynamic radiographs were also obtained.
Pain and Functional Evaluations
To quantitate pain and functional outcomes, visual analogue scale (VAS) scores for back pain and ambulatory status (AS), which was rated on a 4-point scale (4, independently ambulatory; 3, requiring a cane; 2, requiring a walker; and 1, wheelchair bound),36 were determined both preoperatively and postoperatively at last follow-up.
Statistical Analysis
Intergroup comparison of binary variables was achieved using Fisher’s exact test. Intergroup comparison of continuous variables was conducted using unpaired t tests. For survival analyses on reoperation, Kaplan-Meier survival curves for each group were drawn and compared between the 2 groups by the log-rank test. As an exception, the time to reoperation due to SSI was analyzed using the Mantel-Haenszel test, since none of the patients in the S2AI group underwent reoperation due to SSI. Additionally, hazard ratios (HRs) were calculated, which were reported along with 95% confidence intervals (CIs). The perioperative changes in radiographical parameters were also analyzed using paired t tests. The interobserver reliability was calculated, using intraclass correlation coefficient. For the analyses on pain and functional outcomes, the perioperative comparisons for each group and intergroup comparisons were conducted using the Wilcoxon signed-rank test and the Mann-Whitney U test, respectively, as they were nonparametric continuous variables. Data is presented as means ± standard deviations unless stated otherwise. All reported P values are 2-sided and P values <.05 were regarded as statistically significant. All statistical analyses were performed utilizing GraphPad Prism (version 6; GraphPad Software, Inc, La Jolla, CA, USA).
Results
Baseline Characteristics
No statistically significant differences were identified (Table 1) in age, sex, BMI, follow-up period, history of smoking, osteoporosis, osteopenia, preoperative diagnosis, or presenting symptoms between the IS group and the S2AI screw group.
Table 1.
Baseline Characteristics of the IS Group and the S2AI Group.
| Characteristic | IS (n = 17) | S2AI (n = 46) | P |
|---|---|---|---|
| Age (years), mean ± SD | 64.3 ± 11.4 | 61.5 ± 10.7 | .37 |
| Sex (Female), n (%) | 12 (70.6) | 31 (67.4) | .63 |
| BMI (kg/m2), mean ± SD | 33.0 ± 7.3 | 30.2 ± 6.9 | .17 |
| Follow-up period (months), mean ± SD | 22.9 ± 7.4 | 20.4 ± 10.0 | .36 |
| Smoking, n (%) | 9 (52.9) | 26 (56.5) | .49 |
| Osteoporosis, n (%) | 1 (5.9) | 5 (10.9) | >.99 |
| Osteopenia, n (%) | 4 (23.5) | 11 (23.9) | .72 |
| Prior history of any lumbosacral surgery, n (%) | 14 (82.4) | 39 (84.8) | >.99 |
| Prior history of lumbosacral fusion surgery, n (%) | 7 (41.2) | 12 (26.1) | |
| Primary Diagnosis | |||
| Degenerative scoliosis, n (%) | 11 (64.7) | 26 (56.5) | .77 |
| Adult idiopathic scoliosis, n (%) | 3 (17.6) | 12 (26.1) | .74 |
| Combination, n (%) | 3 (17.6) | 8 (17.4) | >.99 |
| Secondary Diagnosisa | IS (n = 14) | S2AI (n = 39) | |
| PJK secondary to prior lumbosacral surgery, n (%) | 4 (28.6) | 12 (30.8) | >.99 |
| CI secondary to prior lumbosacral surgery, n (%) | 4 (28.6) | 11 (28.2) | >.99 |
| SI secondary to prior lumbosacral surgery, n (%) | 7 (50.0) | 25 (64.1) | .53 |
| Preoperative Symptoms | IS (n = 17) | S2AI (n = 46) | |
| Mechanical back pain, n (%) | 15 (88.2) | 42 (91.3) | .66 |
| Radiculopathy, n (%) | 12 (70.6) | 30 (65.2) | .77 |
| Neurogenic claudication, n (%) | 5 (29.4) | 10 (21.7) | .52 |
| Bladder or bowel dysfunction, n (%) | 0 (0.0) | 1 (2.2) | >.99 |
Abbreviations: IS, iliac screw; S2AI, S2-alar-iliac, BMI, body mass index; PJK, proximal junctional kyphosis; CI, coronal imbalance, SI, sagittal imbalance
aDiagnoses before revision surgery. Some patients had multiple diagnoses.
Operative Data
As shown in Table 2, there were no statistically significant differences between the 2 groups in terms of operative data. Of note, the techniques utilized in L5-S1 interbody fusion were not significantly different between the 2 groups (ALIF: 33.3% in the IS group vs 67.7% in the S2AI group, P = .12).
Table 2.
Operative Data of the IS and the S2AI Groups.
| IS (n = 17) | S2AI (n = 46) | P | |
|---|---|---|---|
| No. of operated levels, mean ± SD | 7.5 ± 1.9 | 7.8 ± 2.9 | .68 |
| Uppermost instrumented vertebra, n (%) | .83 | ||
| T9 and above | 0 (0.0) | 3 (6.5) | |
| T10 | 7 (41.2) | 12 (26.1) | |
| T11 | 5 (29.4) | 14 (30.4) | |
| T12 | 1 (5.9) | 3 (6.5) | |
| L1 and below | 4 (23.5) | 14 (30.4) | |
| Staged operations, n (%) | .67 | ||
| 3 stages | 0 (0.0) | 4 (8.7) | |
| 2 stages | 7 (41.2) | 17 (37.0) | |
| 1 stage | 10 (58.8) | 25 (54.3) | |
| Total operative time (minutes), mean ± SD | 733.2 ± 261.1 | 652.0 ± 252.8 | .27 |
| Total EBL (mL), mean ± SD | 2557.6 ± 1572.2 | 2195.8 ± 1548.0 | .42 |
| L5-S1 interbody fusion, n (%) | 9 (52.9) | 31 (67.4) | .63 |
| ALIF, n (%) | 3 (33.3) | 21 (67.7) | .12 |
| PLIF or TLIF, n (%) | 6 (66.7) | 10 (32.3) | |
| Cement vertebroplasty at UIV and/or UIV+1, n (%) | 7 (41.2) | 19 (41.3) | >.99 |
| Smith-Peterson osteotomy, n (%) | 12 (70.6) | 41 (89.1) | .12 |
| Pedicle subtraction osteotomy, n (%) | 5 (29.4) | 6 (13.0) | .15 |
| Received BMP-2, n (%) | 7 (41.2) | 26 (56.5) | .36 |
| Mean dosage of BMP-2 (mg), mean ± SD | 8.5 ± 11.8 | 13.8 ± 14.1 | .17 |
| Total length of stay (days), mean ± SD | 10.9 ± 6.7 | 10.0 ± 7.9 | .65 |
| Total length of ICU stay (days), mean ± SD | 2.6 ± 3.2 | 3.0 ± 4.6 | .74 |
Abbreviations: IS, iliac screw; S2AI, S2-alar-iliac; UIV, uppermost instrumented vertebra; EBL, estimated blood loss; ALIF, anterior lumbar interbody fusion; PLIF, posterior lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion; UIV+1, the supra-adjacent level of UIV; BMP-2, bone morphogenetic protein–2; ICU, intensive care unit.
Complications
The summary of complications in each group is presented in Table 3. With mean follow-up of 21.1 months, the overall reoperation rate was significantly lower in the S2AI group than in the IS group (21.7% vs 58.8%, P = .01), but no significant difference was identified in the incidence of PJF requiring reoperation between the 2 groups (13.0% vs 29.4%, P = .16). There were no significant intergroup differences in the incidence of PJK in general (32.6% [S2AI] vs 35.3% [IS], P > .99) and L5-S1 pseudarthrosis (4.3% [S2AI] vs 11.8% [IS], P = .18). SSIs occurred more frequently in the IS group than in the S2AI group (23.5% vs 2.2%, P = .02) and the S2AI group trended toward a lower rate of wound dehiscence (2.2% vs 17.6%, P = .06). No statistically significant differences were identified in the incidence of other complications.
Table 3.
Comparison of Complications Between IS and S2AI.
| IS (n = 17) | S2AI (n = 46) | ||||
|---|---|---|---|---|---|
| n | % | n | % | P a | |
| Reoperation | 10 | 58.8 | 10 | 21.7 | .01 |
| PJF requiring reoperation | 5 | 29.4 | 6 | 13.0 | .16 |
| PJK | 6 | 35.3 | 15 | 32.6 | >.99 |
| L5-S1 pseudarthrosis | 2 | 11.8 | 1 | 4.3 | .18 |
| Distal device failurea | 3 | 17.6 | 3 | 6.5 | .33 |
| SSI | 4 | 23.5 | 1 | 2.2 | .02 |
| Wound dehiscence | 3 | 17.6 | 1 | 2.2 | .06 |
| Incidental durotomy | 1 | 5.9 | 5 | 10.9 | >.99 |
| DVT | 1 | 5.9 | 3 | 6.5 | >.99 |
Abbreviations: IS, iliac screw; S2AI, S2-alar-iliac screw; PJF, proximal junctional failure; PJK, proximal junctional kyphosis; SSI, surgical site infection; DVT, deep vein thrombosis.
a P values in boldface indicate statistical significance.
bFracture or pull-out of instrumentation in the L4-pelvis region.
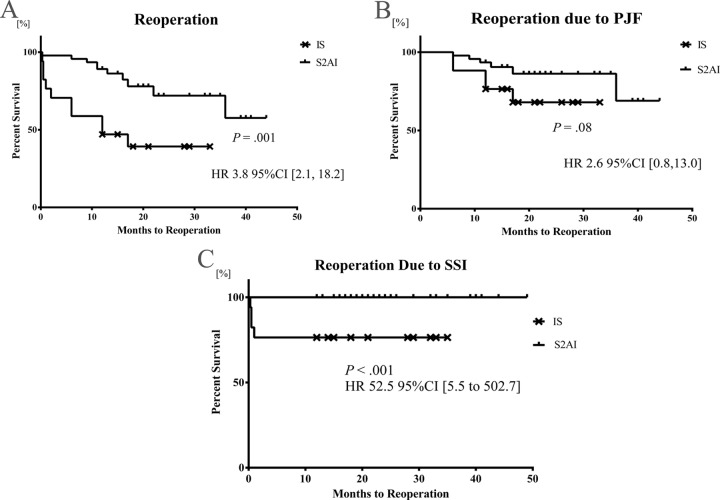
Survival Analyses on Reoperation
The median time to any reoperation, reoperation due to PJF, and reoperation due to SSI were 4 months (range: 0.3-17 months], 12 months (range: 6-17 months], and 0.5 months (range: 0.3-1 month], respectively, in the IS group, and 12 months (range: 0.2-36 nonths) for any reoperation and 12 months (range: 6-36 months) for reoperation due to PJF in the S2AI group. None of patients in the S2AI group developed SSI requiring surgical intervention. The Kaplan-Meier curves for each analysis are shown in Figure 1. The time to reoperation and reoperation due to SSI for patients receiving ISs was significantly shorter than that for patients receiving S2AI screws (P = .001 and P < .001, respectively). Also, there was a trend toward shorter time to reoperation due to PJF in the IS group (P = .08). Use of ISs was significantly associated with early reoperation and early reoperation due to SSI, with HRs of 3.8 (95% CI = 2.1-18.2; P = .001) and 52.5 (95% CI = 5.5-502.7; P < .001), respectively.
Figure 1.
The Kaplan-Meier survival curves for any reoperation (A), reoperation due to proximal junctional failure (B), and reoperation due to surgical site infection. Data is presented with hazard ratios plus 95% confidence intervals.
Radiographical Outcomes
As shown in Table 4, Cobb angle, PI-LL, TK, and LL were significantly improved postoperatively in both groups. The perioperative changes in PI were only significant in the S2AI group (63.4 ± 12.3 vs 57.4 ± 9.6, P = .001). In intergroup comparisons, there were no statistically significant differences in any of the perioperative parameters other than preoperative SS, postoperative PT and the changes in PI. In the IS group, PI increased by 2.9 ± 6.7, whereas in the S2AI group, PI decreased by -6.0 ± 12.5, and these changes were significantly different between the 2 groups (P = .008). The perioperative changes in SS and PT were not statistically significant in either of the 2 groups. The IS group demonstrated a trend toward larger change in LL than the S2AI group (14.3 ± 13.7 vs 6.7 ± 18.9, P = .06).
Table 4.
Comparison of Radiographical Outcomes Between IS and S2AI.
| IS (n = 17), Mean ± SD | P a,b | S2AI (n = 46), Mean ± SD | P a,b | P a,c | Interobserver Agreement | |
|---|---|---|---|---|---|---|
| Pre Cobb | 20.6 ± 10.0 | .04 | 22.6 ± 14.5 | <.001 | .61 | 0.87 |
| Post Cobb | 10.8 ± 3.6 | 10.2 ± 8.5 | .26 | 0.85 | ||
| Change in Cobb | −9.8 ± 11.5 | −12.4 ± 12.5 | .93 | |||
| Pre LL | 32.4 ± 13.9 | <.001 | 38.6 ± 18.5 | .01 | .07 | 0.73 |
| Post LL | 46.7 ± 9.7 | 45.3 ± 9.8 | .08 | 0.75 | ||
| Change in LL | 14.3 ± 13.7 | 6.7 ± 18.9 | .06 | |||
| Pre TK | 32.7 ± 13.8 | .007 | 34.0 ± 20.6 | .004 | .70 | 0.83 |
| Post TK | 45.4 ± 14.6 | 40.6 ± 11.7 | .18 | 0.81 | ||
| Change in TK | 12.7 ± 19.0 | 6.6 ± 18.0 | .43 | |||
| Pre PT | 26.6 ± 7.6 | .33 | 29.3 ± 9.8 | .43 | .22 | 0.71 |
| Post PT | 28.3 ± 6.8 | 28.4 ± 7.8 | .04 | 0.72 | ||
| Change in PT | 1.7 ± 6.4 | −0.9 ± 11.2 | .67 | |||
| Pre SS | 26.7 ± 8.3 | .36 | 34.1 ± 9.9 | .06 | <.001 | 0.75 |
| Post SS | 27.9 ± 5.2 | 30.1 ± 9.0 | .83 | 0.73 | ||
| Change in SS | 1.1 ± 6.5 | −4.0 ± 11.5 | .10 | |||
| Pre PI | 53.3 ± 14.1 | .07 | 63.4 ±12.3 | .001 | .06 | 0.71 |
| Post PI | 56.3 ± 11.6 | 57.4 ± 9.6 | .60 | 0.74 | ||
| Change in PI | 2.9 ± 6.7 | −6.0 ± 12.5 | .008 | |||
| Pre PI-LL | 20.9 ± 17.2 | .03 | 24.8 ± 18.8 | .01 | .75 | 0.72 |
| Post PI-LL | 9.6 ± 7.9 | 12.1 ± 9.7 | .50 | 0.74 | ||
| Change in PI-LL | −11.3 ± 13.9 | −12.7 ± 19.7 | .98 | |||
| Pre SVA | 9.4 ± 6.2 | .26 | 10.4 ± 7.7 | .02 | .56 | 0.86 |
| Post SVA | 6.6 ± 4.8 | 7.5 ± 3.9 | .41 | 0.89 | ||
| Change in SVA | −2.8 ± 8.0 | −2.8 ± 6.9 | .97 |
Abbreviations: IS, iliac screw; S2AI, S2-alar-iliac; Pre, preoperative; Post, postoperative; Cobb, Cobb angle; LL, lumbar lordosis; TK, thoracic kyphosis; PT, pelvic tilt; SS, sacral slope; PI, pelvic incidence; PI-LL, pelvic incidence–lumbar lordosis mismatch; SVA, sagittal vertical axis.
a P values in boldface indicate statistical significance.
bComparison between preoperative and postoperative outcomes.
cComparison between IS and S2AI.
Pain and Functional Outcomes
In terms of VAS back pain and AS, there were statistically significant improvements in both groups (Table 5), but no differences between S2AI and IS screws. Preoperative AS in the IS group was lower than in the S2AI group with statistical significance (2.6 ± 0.8 vs 3.2 ± 0.8, P = .01), and there remained a trend toward improved AS in the S2AI group at final follow-up.
Table 5.
Perioperative VAS and AS of the IS Group and the S2AI Group.
| IS (n = 17); Mean ± SD | P a,b | S2AI (n = 46); Mean ± SD | P a,b | P a,c | |
|---|---|---|---|---|---|
| Preoperative VAS | 5.8 ± 3.1 | 5.5 ± 2.4 | .68 | ||
| Postoperative VAS | 3.2 ± 3.1 | 3.1 ± 2.6 | .99 | ||
| Change in VAS | −2.5 ± 3.6 | .03 | −2.6 ± 2.0 | <.001 | |
| Preoperative AS | 2.6 ± 0.8 | 3.2 ± 0.8 | .01 | ||
| postoperative AS | 3.1 ± 0.7 | 3.5 ± 0.8 | .11 | ||
| Change in AS | 0.5 ± 0.6 | .01 | 0.2 ± 0.4 | .04 |
Abbreviations: IS, iliac screw; S2AI, S2-alar-iliac; VAS, visual analogue scale; AS, ambulatory status.
a P values in boldface indicate statistical significance.
bMann-Whitney U test between preoperative and postoperative outcomes.
cWilcoxon signed rank test between IS and S2AI.
Discussion
To the best of our knowledge, this is the first study to compare the IS technique with the S2AI technique particularly in adult spinal deformity patients with special attention to reoperation and radiographical parameters. Of note, the S2AI technique demonstrated lower rates of overall reoperation and reoperation due to SSI, a similar rate of PJK, longer time to reoperation, and a trend toward longer time to reoperation due to PJF. Furthermore, interestingly, the S2AI technique resulted in a significant reduction in PI compared with the IS technique.
First, the overall reoperation rate was significantly lower in the S2AI group than in the IS group. It is noteworthy that with further stratification and analysis, 5 out of 10 cases of reoperation in the IS group and 6 out of 10 cases in the S2AI group were due to PJK/PJF, which is often considered somewhat unavoidable in a percentage of patients undergoing sagittal plane deformity correction surgery. If those patients are subtracted, the reoperation rate would be 8.7% for the S2AI group versus 29.4% (P = .009) for the IS group, and the majority of reoperations in the IS group were attributable to SSI. Since the decision making in performing revision surgery for PJK/PJF is oftentimes subjective, we additionally demonstrated that the incidence of surgical site infection (2.2% vs 23.5%, P = .02) and reoperation due to severe surgical site infection (0% vs 23.5%, P < .01), both of which are comparatively objective, was less frequent in the S2AI group than in the IS group. This is compatible with previous data published by Mazur et al,27 where a decreased reoperation rate of 8.6% for S2AI screws (vs 35% for ISs) was reported, and Ilyas et al,28 who reported that the S2AI technique showed an absolute risk reduction of 13.0% in acute infection over the IS technique. Our additional analyses on time to reoperation revealed that the benefit of lower rates of reoperation and SSI could be observed in a time-dependent manner as well. In other words, patients receiving ISs tended to undergo more reoperations in the earlier postoperative stages.
It is also interesting that although the incidence of PJK was similar between the 2 groups with the mean follow-up period of 21.1 months, the Kaplan-Meier survival analysis on reoperation due to PJF demonstrated a trend toward earlier revision surgery in the IS group (P = .08). This indicated the potential influence of pelvic fixation methods on PJK/PJF. Although the exact mechanism is unclear, distal fixation has previously been shown to impact the rate of PJK. For instance, Yagi et al9 found that fusion to the sacrum was significantly associated with PJK in a retrospective review of 76 patients, as well as in a prior retrospective review.43 Interestingly, Mummaneni et al17 recently tested the hypothesis that minimally invasive percutaneous posterior instrumentation for adult spinal deformities could reduce the risk of PJK, as it could prevent disruption of the posterior elements of spine. Although no significant differences were observed, this concept could potentially be applied to pelvic fixation, since it has already been shown that percutaneous pelvic fixation is also feasible for this approach.24,44 In addition to these factors, a wide variety of factors have been demonstrated to be associated with PJK/PJF, such as overcorrection of thoracic kyphotic deformities5,6 or LL,7 combined anterior and posterior spinal fusion,8 fusion to the sacrum,9 and selection of the UIV.2 In our study, it was impossible to factor in all of the aforementioned variables due to the limited number of patients. Moreover, the median follow-up period of patients included in this study was not enough in order for us to detect PJK/PJF in the long-term, which may have biased the results. Because of these limitations, it was difficult to draw strong conclusions from our study as it relates to PJK/PJF. Future prospective, comparative studies which focus on risk factors for PJK with pelvic fixation, may be necessary to more definitively clarify this issue.
Of note, an overall L5-S1 fusion rate of 95.2% was noted, which was compatible with prior studies. For instance, Annis et al19 reported an L5-S1 fusion rate of 97% with low-dose BMP-2 and pelvic fixation with or without L5-S1 interbody fusion, whereas Tsuchiya et al45 described use of IS in high-grade spondylolisthesis with an L5-S1 fusion rate of 92.5% at 5-year follow-up.
Intriguingly, the influence of pelvic fixation on changes in spinopelvic parameters has recently been investigated. PI is considered a constant parameter in the absence of pelvic fractures or sacropelvic tumor resection, but Lee et al37 recently published intriguing data, reporting that in adult sagittal deformity correction, PI in those who underwent sacropelvic fixation with ISs increased by 5.9°, whereas PI in those without pelvic fixation increased by 11.4°, and these increases were significantly different between the 2 groups. Based on our results, PI in the S2AI group decreased by 6.0° with statistical significance, while PI in the IS group increased by 2.9°, although it did not reach statistical significance. Hence, it can be speculated that S2AI screws may prevent the postoperative increase in PI, compared with ISs or fixation without any pelvic screws. If SS and PT were analyzed separately, perioperative changes in the 2 groups were not statistically significant in either of the parameters, presumably due to the small sample size, but it would be of great interest to discover which one of them had a greater contribution to the change in PI, and if it is reproducible in future prospective studies.
Theoretically, there are several key differences in biomechanics between the IS technique and the S2AI technique. First, the screw insertion point is more medial and deeper in the S2AI technique.30,33 Second, the angle of screw trajectory in the IS group is usually between 20° to 45° caudal and 30° to 45° degrees lateral, whereas in the S2AI group, the trajectory is 20° to 30° degrees caudal and 40° to 50° lateral.34 Additionally, S2AI screws can purchase tricortical layers, namely, bicortical layers of the sacrum and a monocortical layer of ilium, whereas ISs typically have mono- or bicortical purchase of ilium.
The change in PI may be due to motion at the sacroiliac joints. According to cadaveric data, 60% of S2AI screws violated the sacroiliac joints.33 Slight modification of the alignment of the sacroiliac joints during S2AI screw placement could potentially affect PI. Additionally, following a long-segment fusion, the mechanisms for compensatory motion in the lumbosacral spine are eliminated, leaving motion only at the sacroiliac joint. Degeneration or disruption of sacroiliac joints may affect postoperative PI over the long term, especially if there is screw loosening.37,38,46 Although PI is felt to be a constant value, this remains true only if the relationship between the sacrum and pelvis remains constant.39 Although postoperative sacroiliac joint motion is controversial, the sacroiliac joint is susceptible to shear forces, with components of both rotation and translation,40,41 and hypermobility of the sacroiliac joint has been reported following fusion to the sacrum.42 Perioperative changes in spinopelvic parameters are a complicated biological phenomenon in vivo, which are challenging to test in cadavers or biomechanically. However, this result provides some insight into how spinal alignment may be affected by instrumentation and how it is translated into clinical outcomes, though further prospective study is warranted.
Additional limitations of this study include the fact that the data was obtained from a single-center in a retrospective manner with relatively small sample size. Additional bias may also be introduced due to temporal differences in treatment selection as well as asymmetry in the number of patients in the two groups. This asymmetry was primarily due to our treatment selection process, where S2AI screws and ISs were equally selected based on surgeons’ preference from October 2010 to December 2013, but S2AIs were preferentially utilized from January 2014 to February 2015, since we were aware of the improved clinical outcomes via the S2AI technique. For instance, as IS screws were mainly used earlier in the study period, and there may be improvement in overall deformity surgery technique over time, which may benefit the S2AI group, although our subsequent analysis revealed that if we compared patients operated on before January, 2014 in the S2AI group with after January, 2014, there were no intergroup differences in the overall reoperation rate, reoperation rates due to SSI or PJF, which essentially means the aforementioned potential bias was not that influential. As such, the outcomes of this study should be interpreted carefully and there is a substantial need for prospective, multi-center, randomized studies to further clarify the differences in clinical outcomes and perioperative changes in radiographical parameters between the two groups.
Conclusions
Compared with the IS technique, the S2AI technique demonstrated lower rates of overall reoperation and reoperation due to SSI, a similar rate of PJK/PJF, longer time to reoperation, and possible reduction in PI. Future studies may be warranted to clarify the mechanism of these results and how they can be translated into improved patient care.
Footnotes
Authors’ Note: This article represents the views of the authors and should not be construed to represent the US Food and Drug Administration’s views or policies.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Author CRG is a UNCF-Merck Postdoctoral Fellow and is supported by an award from the Burroughs Wellcome Fund. Author AB received a research grant from DePuy Synthes Spine and serves on the clinical advisory board of MedImmune, LLC. Author ZLG has stock ownership in US Spine and Spinal Kinetics, consulting, speaking, and teaching agreements for the AO Foundation, and research support from DePuy Synthes, NREF, AOSpine and AO North America. Author DMS received honoraria from Depuy Synthes, and has had consulting agreements with Medtronic, Globus, Stryker, and Orthofix. Author TFW receives research support from the Gordon and Marilyn Macklin Foundation, and has received complementary research medications from Eli Lilly and Company.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research support provided by the Gordon and Marilyn Macklin Foundation.
References
- 1. Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976). 2005;30:1643–1649. [DOI] [PubMed] [Google Scholar]
- 2. Kim HJ, Yagi M, Nyugen J, Cunningham ME, Boachie-Adjei O. Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res. 2012;470:1633–1639. doi:10.1007/s11999-011-2179-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Edwards CC, Bridwell KH, Patel A, Rinella AS, Berra A, Lenke LG. Long adult deformity fusions to L5 and the sacrum. A matched cohort analysis. Spine (Phila Pa 1976). 2004;29:1996–2005. [DOI] [PubMed] [Google Scholar]
- 4. Finger T, Bayerl S, Onken J, Czabanka M, Woitzik J, Vajkoczy P. Sacropelvic fixation versus fusion to the sacrum for spondylodesis in multilevel degenerative spine disease. Eur Spine J. 2014;23:1013–1020. doi:10.1007/s00586-014-3165-6. [DOI] [PubMed] [Google Scholar]
- 5. Lowe TG, Kasten MD. An analysis of sagittal curves and balance after Cotrel-Dubousset instrumentation for kyphosis secondary to Scheuermann’s disease. A review of 32 patients. Spine (Phila Pa 1976). 1994;19:1680–1685. [DOI] [PubMed] [Google Scholar]
- 6. Wang J, Zhao Y, Shen B, Wang C, Li M. Risk factor analysis of proximal junctional kyphosis after posterior fusion in patients with idiopathic scoliosis. Injury. 2010;41:415–420. doi:10.1016/j.injury.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 7. Maruo K, Ha Y, Inoue S, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976). 2013;38:E1469–E1476. doi:10.1097/BRS.0b013e3182a51d43. [DOI] [PubMed] [Google Scholar]
- 8. Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976). 2008;33:2179–2184. doi:10.1097/BRS.0b013e31817c0428. [DOI] [PubMed] [Google Scholar]
- 9. Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976). 2012;37:1479–1489. doi:10.1097/BRS.0b013e31824e4888. [DOI] [PubMed] [Google Scholar]
- 10. Cammarata M, Aubin C-É, Wang X, Mac-Thiong J-M. Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine (Phila Pa 1976). 2014;39:E500–E507. doi:10.1097/BRS.0000000000000222. [DOI] [PubMed] [Google Scholar]
- 11. Park WM, Choi DK, Kim K, Kim YJ, Kim YH. Biomechanical effects of fusion levels on the risk of proximal junctional failure and kyphosis in lumbar spinal fusion surgery. Clin Biomech. 2015;30:1162–1169. doi:10.1016/j.clinbiomech.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 12. Lau D, Clark AJ, Scheer JK, et al. Proximal junctional kyphosis and failure after spinal deformity surgery. Spine (Phila Pa 1976). 2014;39:2093–2102. doi:10.1097/BRS.0000000000000627. [DOI] [PubMed] [Google Scholar]
- 13. Kebaish KM, Martin CT, O’Brien JR, LaMotta IE, Voros GD, Belkoff SM. Use of vertebroplasty to prevent proximal junctional fractures in adult deformity surgery: a biomechanical cadaveric study. Spine J. 2013;13:1897–1903. doi:10.1016/j.spinee.2013.06.039. [DOI] [PubMed] [Google Scholar]
- 14. Kayanja MM, Schlenk R, Togawa D, Ferrara L, Lieberman I. The biomechanics of 1, 2, and 3 levels of vertebral augmentation with polymethylmethacrylate in multilevel spinal segments. Spine (Phila Pa 1976). 2006;31:769–774. doi:10.1097/01.brs.0000207466.40955.31. [DOI] [PubMed] [Google Scholar]
- 15. Hart RA, Prendergast MA, Roberts WG, Nesbit GM, Barnwell SL. Proximal junctional acute collapse cranial to multi-level lumbar fusion: a cost analysis of prophylactic vertebral augmentation. Spine J. 2008;8:875–881. doi:10.1016/j.spinee.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 16. Ha K-Y, Seo J-Y, Kwon S-E, Son I-N, Kim K-W, Kim Y-H. Posterior dynamic stabilization in the treatment of degenerative lumbar stenosis: validity of its rationale. J Neurosurg Spine. 2013;18:24–31. doi:10.3171/2012.9.SPINE12392. [DOI] [PubMed] [Google Scholar]
- 17. Mummaneni PV, Park P, Fu K-M, et al. Does minimally invasive percutaneous posterior instrumentation reduce risk of proximal junctional kyphosis in adult spinal deformity surgery? A propensity-matched cohort analysis. Neurosurgery. 2016;78:101–108. doi:10.1227/NEU.0000000000001002. [DOI] [PubMed] [Google Scholar]
- 18. Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS. Outcome and complications of long fusions to the sacrum in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976). 2002;27:776–786. doi:10.1097/00007632-200204010-00017. [DOI] [PubMed] [Google Scholar]
- 19. Annis P, Brodke DS, Spiker WR, Daubs MD, Lawrence BD. The fate of L5-S1 with low dose BMP-2 and pelvic fixation, with or without interbody fusion, in adult deformity surgery. Spine (Phila Pa 1976). 2015;40:E634–E639. doi:10.1097/BRS.0000000000000867. [DOI] [PubMed] [Google Scholar]
- 20. Rahman RK, Buchowski JM, Stephens B, Dorward IG, Koester LA, Bridwell KH. Comparison of TLIF with rhBMP-2 versus no TLIF and higher posterolateral rhBMP-2 dose at L5-S1 for long fusions to the sacrum with sacropelvic fixation in patients with primary adult deformity. Spine (Phila Pa 1976). 2013;38:2264–2271. doi:10.1097/BRS.0000000000000045. [DOI] [PubMed] [Google Scholar]
- 21. Sponseller PD. The S2 portal to the ilium. Semin Spine Surg. 2007;2:83–87. doi:10.1017/CBO9781107415324.004. [Google Scholar]
- 22. Kebaish KM. Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976). 2010;35:2245–2251. doi:10.1097/BRS.0b013e3181f5cfae. [DOI] [PubMed] [Google Scholar]
- 23. Guler UO, Cetin E, Yaman O, et al. Sacropelvic fixation in adult spinal deformity (ASD): a very high rate of mechanical failure. Eur Spine J. 2015;24:1085–1091. doi:10.1007/s00586-014-3615-1. [DOI] [PubMed] [Google Scholar]
- 24. Martin CT, Witham TF, Kebaish KM. Sacropelvic fixation two case reports of a new percutaneous technique. Spine (Phila Pa 1976). 2011;36:E618–E621. doi:10.1097/BRS.0b013e3181f79aba. [DOI] [PubMed] [Google Scholar]
- 25. Ray WZ, Ravindra VM, Schmidt MH, Dailey AT. Stereotactic navigation with the O-arm for placement of S-2 alar iliac screws in pelvic lumbar fixation. J Neurosurg Spine. 2013;18:490–495. doi:10.3171/2013.2.SPINE12813. [DOI] [PubMed] [Google Scholar]
- 26. Mattei TA, Fassett DR. Low-profile pelvic fixation with sacral alar-iliac screws. Acta Neurochir (Wien). 2013;155:293–297. doi:10.1007/s00701-012-1560-5. [DOI] [PubMed] [Google Scholar]
- 27. Mazur MD, Ravindra VM, Schmidt MH, et al. Unplanned reoperation after lumbopelvic fixation with S-2 alar-iliac screws or iliac bolts. J Neurosurg Spine. 2015;23:67–76. doi:10.3171/2014.10.SPINE14541. [DOI] [PubMed] [Google Scholar]
- 28. Ilyas H, Place H, Puryear A. A Comparison of early clinical and radiographic complications of iliac screw fixation versus S2 alar iliac (S2AI) fixation in the adult and pediatric populations. J Spinal Disord Tech. 2015;28:199–205. [DOI] [PubMed] [Google Scholar]
- 29. Sponseller PD, Zimmerman RM, Ko PS, et al. Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine (Phila Pa 1976). 2010;35:1887–1892. doi:10.1097/BRS.0b013e3181e03881. [DOI] [PubMed] [Google Scholar]
- 30. Chang T-L, Sponseller PD, Kebaish KM, Fishman EK. Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976). 2009;34:436–440. doi:10.1016/j.spinee.2008.06.757. [DOI] [PubMed] [Google Scholar]
- 31. Shabtai L, Andras LM, Portman M, et al. Sacral alar iliac (SAI) screws fail 75% less frequently than iliac screws in neuromuscular scoliosis [published online January 11 2016]. J Pediatr Orthop. doi:10.1097/BPO.0000000000000720. [DOI] [PubMed] [Google Scholar]
- 32. Elder BD, Ishida W, Lo S-FL, et al. Use of S2-alar-iliac screws associated with less complications than iliac screws in adult lumbosacropelvic fixation. Spine (Phila Pa 1976). 2017;42:E142–E149. doi:10.1097/BRS.0000000000001722. [DOI] [PubMed] [Google Scholar]
- 33. O’Brien JR, Yu WD, Bhatnagar R, Sponseller P, Kebaish KM. An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine (Phila Pa 1976). 2009;34: E439–E442. doi:10.1097/BRS.0b013e3181a4e3e4. [DOI] [PubMed] [Google Scholar]
- 34. Ishida W, Elder BD, Lo SL, Witham TF. Spinopelvic reconstruction following lumbosacral tumor resection. World Spine Column J. 2016;7:25–30. [Google Scholar]
- 35. Cho SK, Shin JI, Kim YJ. Proximal junctional kyphosis following adult spinal deformity surgery. Eur Spine J. 2014;23:2726–2736. doi:10.1007/s00586-014-3531-4. [DOI] [PubMed] [Google Scholar]
- 36. Wang MY, Widi G, Levi AD. The safety profile of lumbar spinal surgery in elderly patients 85 years and older. Neurosurg Focus. 2015;39:E3 doi:10.3171/2015.7.FOCUS15180. [DOI] [PubMed] [Google Scholar]
- 37. Lee J-H, Na K-H, Kim J-H, Jeong H-Y, Chang D-G. Is pelvic incidence a constant, as everyone knows? Changes of pelvic incidence in surgically corrected adult sagittal deformity. Eur Spine J. 2016;25:3707–3714. doi:10.1007/s00586-015-4199-0. [DOI] [PubMed] [Google Scholar]
- 38. Gottfried ON, Omeis I, Mehta VA, Solakoglu C, Gokaslan ZL, Wolinsky J-P. Sacral tumor resection and the impact on pelvic incidence. J Neurosurg Spine. 2011;14:78–84. doi:10.3171/2010.9.SPINE09728. [DOI] [PubMed] [Google Scholar]
- 39. Lafage V, Schwab F, Patel A, Hawkinson N, Farcy J-P. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009;34:E599–E606. doi:10.1097/BRS.0b013e3181aad219. [DOI] [PubMed] [Google Scholar]
- 40. Jacob HAC, Kissling RO. The mobility of the sacroiliac joints in healthy volunteers between 20 and 50 years of age. Clin Biomech (Bristol, Avon). 1995;10:352–361. [DOI] [PubMed] [Google Scholar]
- 41. Sturesson B, Selvik G, Udén A. Movements of the sacroiliac joints. A roentgen stereophotogrammetric analysis. Spine (Phila Pa 1976). 1989;14:162–165. [DOI] [PubMed] [Google Scholar]
- 42. Frymoyer JW, Howe J, Kuhlmann D. The long-term effects of spinal fusion on the sacroiliac joints and ilium. Clin Orthop Relat Res. 1978;(134):196–201. [PubMed] [Google Scholar]
- 43. Yagi M, Akilah KB, Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976). 2011;36:E60–E68. doi:10.1097/BRS.0b013e3181eeaee2. [DOI] [PubMed] [Google Scholar]
- 44. O’Brien JR, Matteini L, Yu WD, Kebaish KM. Feasibility of minimally invasive sacropelvic fixation: percutaneous S2 alar iliac fixation. Spine (Phila Pa 1976). 2010;35:460–464. doi:10.1097/BRS.0b013e3181b95dca. [DOI] [PubMed] [Google Scholar]
- 45. Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006;31:303–308. doi:10.1097/01.brs.0000197193.81296.f1. [DOI] [PubMed] [Google Scholar]
- 46. Camisa W, Bess S, Yi S, et al. Biomechanical demands on S2AI sacral and pelvic instrumentation in long fusion constructs with and without interbody supplementation. Spine J. 2014;14(11 suppl):S166 doi:10.1016/j.spinee.2014.08.400. [Google Scholar]