Abstract
Background
Familiarity with environment, processes and equipment reduces the risk inherently associated with critical care transfers. Therefore, the North West London Critical Care Network decided to create a standardised ideal transfer bag and contents to improve patient safety.
Methods
A four-round modified Delphi survey developed a condensed and clinically tested content list. An expert panel then designed an ideal transfer bag based on agreed important principles.
Results
Participants completed two rounds of an electronic survey. Round 3 comprised an expert clinical panel review, while round 4 tested the contents over 50 clinical transfers. The prototype bag’s design was adjusted after clinical use and feedback.
Discussion
This project has introduced a standardised critical care transfer bag across our network. A similar technique could be used for other healthcare regions. Alternatively, the above critical care transfer bag could be adopted or adapted for regional use by clinicians.
Keywords: Critical care, patient transfer, patient safety, equipment and supplies, Delphi technique
Background
Critical Care transfers are common and inherently associated with risk. Unfamiliarity with environment, processes and equipment contribute to this risk.1–3 Frequent rotation of medical staff undertaking transfers and a lack of standardised equipment, particularly the transfer bag, are exacerbating factors. The North West London Critical Care Network (NWLCCN) has shown that patient safety during critical care transfers can be improved by standardising regional transfer training and education material.4 These methods increase clinicians’ familiarity with transfer processes and equipment.
A vital piece of transfer equipment is the transfer bag, which contains life-sustaining and supporting equipment. Despite showing that standardisation reduces risk, there continues to be a considerable variation in the contents and designs of transfer bags even within regions and their constituent hospitals. It is not uncommon to find large wheel-based suitcases that create a struggle to manoeuvre into lifts and along corridors. Therefore, NWLCCN embarked upon a project to create the ideal transfer bag design and content list. This article describes the development of this bag and its introduction into the clinical environment.
Methods
Stage 1: Creating the bag contents list
The initial list of transfer contents was all inclusive (Table 1) and generated from the combination of the Intensive Care Society 2011 list of ‘Supplementary equipment for use during transport’,5 North West London Critical Care transfer bags and London HEMS (Helicopter Emergency Medical Service) and RAF CCAST (Critical Care Air Support Team) bags. A modified Delphi Survey with four “rounds” enabled the list to be condensed appropriately.
Table 1.
Initial all inclusive list of transfer contents.
| Airway 1. Guedel airways size 2 2. Guedel airways size 3 3. Guedel airways size 4 4. Nasopharyngeal airways 6 5. Nasopharyngeal airways 7 6. LMA size 3 7. LMA size 4 8. Igel size 3 9. Igel size 4 10. Igel size 5 11. ET tube 6 12. ET tube 7 13. ET tube 8 14. ET tube 9 15. Laryngoscope Handle + bulbs + batteries 16. Laryngoscope Blades 3 17. Laryngoscope Blades 4 18. Endo Tracheal ties 19. Tracheostomy ties 20. Magill Forceps 21. Tape for securing ET 22. lubricating gel 23. Stylet 24. Gum elastic bougie 25. Stethoscope 26. Sterile scissors 27. Scalpel | Breathing/Ventilation 1. Ventilation/breathing 2. Self inflating bag and mask with oxygen reservoir and tubing (BVM) 3. spare Bodock seals (for pin index oxygen regulators) 4. Airway filters/HME filter 5. Cather mounts 6. Oxygen Mask - rebreathe size 4 7. Oxygen Mask - rebreathe size 5 8. Trache mask 9. Waters circuit 10. Nasal specs 11. Nebuliser set + tubing 12. Oxygen tubing 13. ETC02 indicators (easy cap) 14. Anaesthetic masks - green and orange 15. Chest drain (seldinger type) 16. Heimlich flutter valve 17. Pocket mask 18. 24% oxygen spikes 19. 40% oxygen spikes 20. 60% oxygen spikes 21. Ventimask | Circulation 1. IV cannula size 14G 2. IV cannula sizes 16G 3. IV cannula sizes 18G 4. IV cannula sizes 20G 5. IV cannula sizes 22G 6. Arterial cannula 7. Central venous cannula 8. non sterile gloves 9. aprons 10. Luer lock syringes 20 ml 11. Luer lock syringes 50 ml 12. Needles Green 13. Needles Blue 14. Needles white 15. Drawing up needles 16. Arterial blood gas syringes (no portable blood gas analysis available) 17. Bladder syringe 18. Chloraprep skin prep 19. Alcohol wipes 20. Tourniquet 21. Blood/colloid fluid giving set (gravity) 22. Blood/colloid fluid giving set (volumetric) 23. Infusion device giving sets 24. Infusion device extension sets 25. 3-way taps 26. Obturators (red and/or white bungs) 27. Micro pore tape 28. Gauze 29. Cannula dressings 30. Labels 31. Transducer set – Art 32. Transducer set – Art/CVP 33. CVP line dressings 34. Pressure bag 35. Art Line insertion pack 36. Minor instrument – cut down set 37. Sterile towels 38. EMLA cream 39. Sodium chloride ampoules (flush) 40. Sterile gloves 6 41. Sterile gloves 7 42. Sterile gloves 8 43. IV Fluids (colloid) 500 ml 44. IV Fluids (crystalloid) 500 ml 45. EZ-IO intraosseous device 46. EZ-IO needles Other 1. Eye shields 2. Blue clamps 3. Trauma shear scissors 4. Scalpel (22 blade) 5. Spencer Wells forceps (8 in) 6. Hand held silk 1/0 suture 7. Sleek roll |
| NG/Enteral 1. Nasogastric tubes (assorted sizes) 2. Litmus paper 3. 50 ml bladder syringe 4. Drainage bags 5. Spigots | Monitoring (supplemental) 1. Tempa dots 2. ECG electrodes 3. Defibrillator pads (local) 4. Oesophageal temp probe 5. Sphygmanonometer 6. Wave form capnograph 7. Torch | |
| Drugs 1. Adrenaline 1:10,000 Pre-filled syringe 2. Atropine 3 mg pre-filled syringe 3. Amiodarone 300 mg Pre-filled syringe 4. Metaraminol 10 mg/1 ml 5. Adrenaline 1:1000 5 ml 6. Noradrenaline 4 mg/4 ml 7. Propofol 1% 100 ml bottle 8. Midazolam 5 mg/5 ml 9. Salbutamol 5 mg neb 10. Calcium chloride 10 ml/10 mmol – pre-pilled syringe 11. Sodium bicarbonate 12. 50 % Glucose 13. Vecuronium 14. Thiopentone 15. Lignocaine 1% 16. Hydrocortisone 17. Chlorphenamine 18. Naloxone 400 mcg | Suction 1. Yankauer sucker 2. Suction catheters (10F) 3. Suction catheters (12F) 4. Suction catheters (14F) 5. Closed suction system (ET) 6. Closed suction system (Trache) 7. Suction tubing 8. Hand held portable suction 9. Tracheal dilator Infection Control 1. Non sterile gloves 2. Aprons 3. Clinical waste bags 4. Catheter bag 5. Face mask 6. Sharps box | |
Round 1 was an electronically mailed spreadsheet of all 146 items separated into categories (Airway, Breathing, Suction, Circulation, Enteral, Drugs, Infection Control, Monitoring and Other). This was sent to clinicians within North West London comprising nurses, physicians and paramedics working within different departments (Critical Care, Emergency, Anaesthetics and Ambulance service) with a range of seniority. They were asked to rate items using a 5-point Likert scale (‘Very unimportant,’ ‘Quite unimportant,’ ‘Neither,’ ‘Quite important,’ ‘Very important’) and decide how many of each item would be needed within the final bag. An additional question asked if the clinician had used the item during any previous transfers to prompt consideration of its need in the final ideal bag. A pilot study consisting of 10 individuals was undertaken to determine if completion of the extensive questionnaire was achievable in a reasonable length of time and if adjustments were needed.
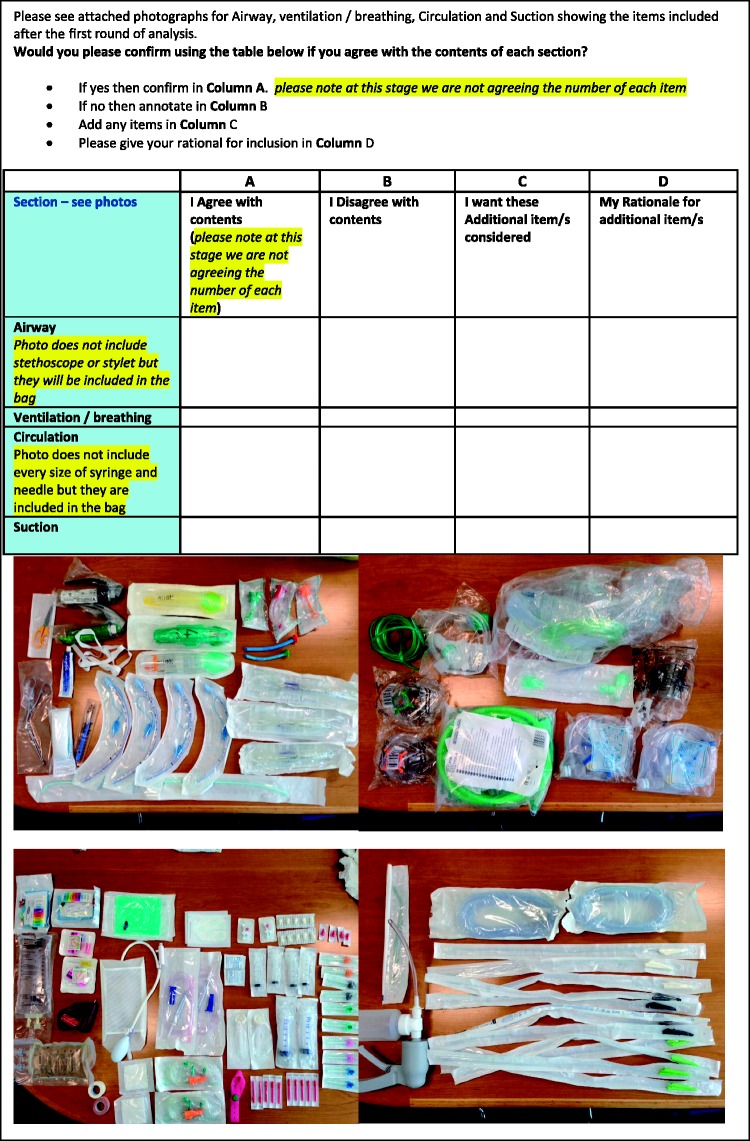
Round 2 was an electronically mailed questionnaire comprising photographs of the items (Figure 1), which were deemed ‘Very important’ or ‘Quite important’ by at least 80% of respondents from round one. This was simple and quick (less than 5 min) to complete and questioned whether the respondent agreed with the items or if additional items were needed and if so, what the rationale was.
Figure 1.
Electronically mailed questionnaire to decide on selected transfer bag contents.
Round 3 consisted of an expert panel of 22 clinicians from the NWLCCN Transfer faculty who met face-to-face to discuss the content list and review the numbers of each item required.
Round 4 involved the clinical use of a transfer bag packed with the agreed items during 50 intra-hospital transfers in three North West London hospitals. A further 105 clinicians reviewed the contents over three NWLCCN transfer training courses. Feedback was obtained during both processes.
Stage 2: Creating the bag design
The process of designing the ideal critical care transfer bag was initiated by reviewing five transfer bags in current use across London. The same expert panel of 22 NWLCCN clinicians met to discuss the advantages and disadvantages of each. The key principles and features to be included were outlined and agreed, including the addition of a ‘Patient Pocket’ which allowed clinicians the flexibility to add bespoke items for that specific patient transfer.
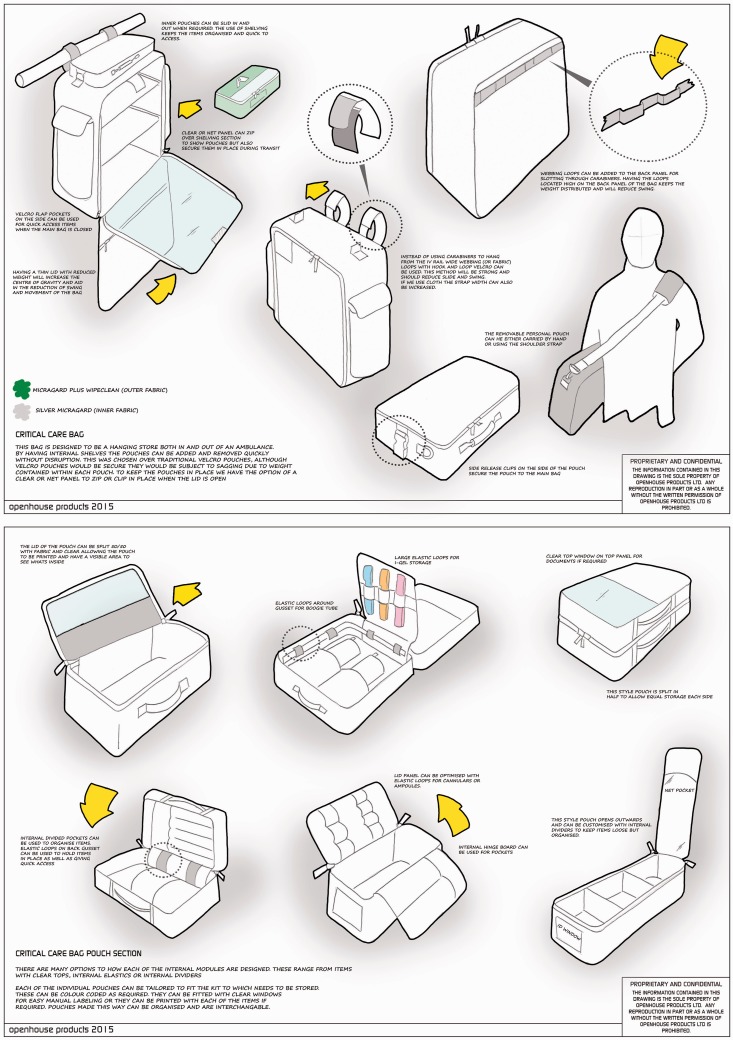
Having discussed the project with several bag designers, one design company, Openhouse™, was approached with the agreed principles and features required for the ideal transfer bag. A schematic diagram was drawn up for review and discussion. The filled control transfer bag provided information about the weight and dimensions of the equipment items.
Feedback about the bag design was collected from the Annual NWLCCN Education Event where the packed prototype bag was presented to the audience with an explanation of the process leading up to it.6 Clinicians were given an opportunity during the day to handle the bag and manoeuvre it on and off an ambulance. Afterwards, the prototype bag was taken to all the 19 hospitals in the NWLCCN and to the Emergency, Critical care, High Dependency, Outreach and Anaesthetic departments for further comments and feedback.
Once the bag design had been adjusted from the collated feedback, a further quality assessment was made in the form of ‘time to check’ tests. During several transfer training courses, candidates were timed against each other, one checking an original transfer bag and the other checking the new NWLCCN prototype, to determine which was fastest and easiest.
Results
Results –Stage 1
The pilot study revealed that the spreadsheet lines were quite hard to follow due to the extensive number of items. Alternate line shading was used to make the form easier to read. Completion took 30 min, which was considered acceptable.
Round 1 (spreadsheet) was sent to 125 participants and 92 replies (Table 2) were received. Repeated reminders were sent electronically and communicated personally in order to maximise return rates. The section on importance of items was completed well, although some of the comments showed there was confusion if an item was in two categories. There was a poor response to the questions asking how many items were required and whether clinicians had used items during previous transfers. We re-evaluated the usefulness of the last of these questions, as an item such as an endotracheal tube is not necessarily de-valued because it is rarely used.
Table 2.
Round 1: summary of responses.
| 92 replies | |||
|---|---|---|---|
| Department respondent from: | Type of clinician: | ||
| ICU | 67 | Nurse | 64 |
| Outreach | 3 | Resuscitation officer | 6 |
| Resuscitation | 6 | Doctor | 20 |
| Emergency | 14 | Paramedic | 2 |
| Ambulance service | 2 | ||
| Additional items | |||
| Airway: | Requested by: | ||
| • Emergency needle/ surgical airway set | 3 | ||
| • Tracheostomy tubes or ‘passport box’ | 3 | ||
| • Choice of ‘Airtraq’ laryngoscopes | 1 | ||
| Breathing: | |||
| • Chest drain kit | 2 | ||
| Suction | |||
| • Suction liners | 1 | ||
| • 50 ml bladder syringe with tubing for suctioning | 1 | ||
| NG/Enteral | |||
| • Lubricant | 1 | ||
| Drugs | |||
| • Ketamine | 4 | ||
| • Suxamethonium | 1 | ||
| • Rocuronium | 2 | ||
| • 10% dextrose | 1 | ||
| • Opiates | 1 | ||
| • Antibiotic | 1 | ||
| • Water ampoule | 1 | ||
| Infection control | |||
| • Incontinence pads | 2 | ||
| • Sharps bin | 1 | ||
| Monitoring | |||
| • Defibrillator | 2 | ||
| • Head torches | 1 | ||
Round 2 (photographic) was sent to 137 participants and a total of 57 replies were received. The increase in participant number from the previous round was due to additional clinicians from the Royal Air Force and outside North West London who expressed an interest in the project. The vast majority agreed with photographed items (Table 3): Airway 100% agreed, Breathing 89%, Circulation 96% and Suction 98%.
Table 3.
Round 2: summary of responses.
| Airway | Breathing | Circulation | Suction |
|---|---|---|---|
| 57 (100%) agreed with contents shown from round two | 51 (89%) agreed with contents shown from round two | 55 (96%) agreed with contents shown from round two | 56 (98%) agreed with contents shown from round two |
| Additional items: | Comments: | Additional items: | |
| -More ETT sizes -Syringe for cuff -Igel not LMA (3 respondents) | -‘Less catheters than shown in photo’ | - Arterial line - Sterile set |
Round 3 (expert panel) reviewed the results and refined the content list. At this stage, there was also a ‘common sense check' regarding the final items, for example, moving a 10 ml syringe to the airway section for cuff inflation during intubation. Unique bags were then filled with the finalised contents list (Table 4). These were different from any transfer bags in clinical use to distinguish them for the study. The layout was compromised as the contents did not fit perfectly into the designated sections but at this stage only the contents were being tested. Four bags were packed, three for clinical use and a fourth as a control to be held at the network office and taken to training events. Any practical changes were made to all four bags simultaneously.
Table 4.
The finalised contents list.
| Advanced Airway pocket 1. 1 × ET tube 6 2. 1 × ET tube 7 3. 1 × ET tube 8 4. 1 × ET tube 9 5. 2 × Laryngoscope Handles + bulbs + batteries 6. 1 × Laryngoscope Blades 3 7. 1 × Laryngoscope Blades 4 8. 2 × Endotracheal ties 9. 1 × Magill Forceps 10. 1 × Tape for securing ET 11. 3 × Lubricating gels 12. 1 × Stylet 13. 1 × Gum elastic bougie 14. 1 × Tracheal dilator 15. 1 × Scalpel size 22 16. 1 × 10 ml syringe 17. 1 × Torch 18. 2 × Face masks 19. 1 × ETCO2 indicator | Breathing pocket 1. 1 × I-gel size 3 2. 1 × I-gel size 4 3. 1 × I-gel size 5 4. 1 × Airway HME filter 5. 1 × Catheter mount 6. 1 × Waters circuit 7. 1 × Sterile scissors 8. 1 × Anaesthetic mask size 4 green 9. 1 × Anaesthetic mask size 5 orange 10. 1 × Stethoscope 11. 1 × Wave form capnograph | Circulation pocket 1. 2 × IV cannula size 14G 2. 2 × IV cannula size 16G 3. 2 × IV cannula size 18G 4. 2 × IV cannula size 20G 5. 2 × IV cannula size 22G 6. 10 × Pairs of non sterile gloves 7. 5 × Luer lock syringes 20 ml 8. 4 × Luer lock syringes 50 ml 9. 3 × Chloraprep skin wipes 10. 10 × Alcohol wipes 11. 2 × Blood/colloid fluid giving sets (gravity) 12. 5 × Infusion device giving sets 13. 5 × Infusion device extension sets 14. 5 × 3-way taps (or equivalent) 15. 10 × Obturators (red and/or white bungs) 16. 1 × Micropore tape 17. 4 × Gauze 18. 5 × Cannula dressings 19. 12 × ECG electrodes 20. 1 × Trauma shear scissors 21. 10 × Labels |
| Suction pocket 1. 2 × Yankauer suckers 2. 2 × Suction catheters (10F) 3. 2 × Suction catheters (12F) 4. 2 × Suction catheters (14F) 5. 2 × Suction tubing | ||
| Self-ventilating pocket 1. 1 × Guedel airways size 2 2. 1 × Guedel airways size 3 3. 1 × Guedel airways size 4 4. 1 × Nasopharyngeal airways 6 5. 1 × Nasopharyngeal airways 7 6. 1 × Oxygen Mask- non rebreathe size 4 7. 1 × Oxygen Mask- non rebreathe size 5 8. 2 × Oxygen tubing | External pocket 1. 1 × Self-inflating bag and mask with oxygen reservoir and tubing (BVM) | 22. 10 × Sodium Chloride ampoules (flush) Interventional circulation 1. 1 × EZ-IO Intraosseous Device 2. 3 × EZ-IO Needles 3. 5 × Needles Green 4. 5 × Needles Blue 5. 5 × Needles white 6. 5 × Drawing up needles 7. 2 × Tourniquets |
| Inside pouch on side of bag 1. 2 × Clinical waste bags 2. 1 × Sharps box (to be sourced locally) 3. 1 × Hand-held portable suction 4. 3 × IV Fluids (crystalloid) 500 ml 5. 1 × Pressure bag |
Round 4 (clinical transfers) tested the contents during 50 transfers across three North West London Hospitals. Feedback received was very positive, particularly in regard to the reduced weight with the condensed kit. Over a 10-week period, very little kit was actually used which demonstrated the feasibility of equipment reduction. The outreach team’s broader use for the bag (patient stabilisation), which was not part of the bag’s remit, meant that the lack of arterial lines and transducer set was highlighted –a ‘grab bag’ is in development for these teams. Specialised services, for example, Extra-corporeal Membrane Oxygenation (ECMO) acknowledged that they would need to add to the standardised transfer bag.
Results – Stage 2
The initial schematic diagram of the bag is shown in Figure 2. This was the result of the key features and principles (Table 5) that were decided on by the panel of NWLCCN clinicians in June 2014. Several further adaptations were made after the prototype bag. Initial adjustments were made after comments (Table 6) were received from the majority of the 89 attendees at the annual NWLCCN event in December 2015. Further modifications were needed after the bags were tried and tested on various trolleys and beds within different hospitals across North West London and on London Ambulances (Figures 3 to 7).
Figure 2.
Initial schematic diagram of the transfer bag. ® This design is copywritten.
Table 5.
Key principles and features as outlined by NWLCCN transfer and retrieval faculty.
| Principles |
| • Intra or inter hospital transfers would use the same core basic bag |
| • Drugs module would be separate due to CQC (Care Quality Commission) demands regarding storage of drugs, fridge requirement and expiry date management |
| • Waveform capnography would need to be locally provided and this would vary site to site |
| • Designed to be secured on either the bed or trolley depending on the type of transfer |
| • To reduce variation all Trusts in NWLCCN would use the same kit |
| • Patient transfer bag rather than a stabilisation or pre-hospital bag |
| • Adult transfers only |
| Features |
| • Able to be secured on bed, trolley and ambulance |
| • Accessibility of contents when hanging |
| • A ‘Patient Pocket’ would be designed on the outside of the bag, this would be made of clear wipeable material for housing patient specific equipment or consumables e.g. Tracheostomies, chest drains, extra syringes of sedatives or vasopressors for that specific patient transfer |
| • Ability to check ‘at a glance’ to reduce staff checking time |
| • Filled weight less than 13 kilograms |
| • Able to be carried as a back pack for teams returning after patient transfer completed |
Table 6.
Modifications following NWLCCN annual event and feedback from pilot sites.
| External |
| • Bag Valve Mask pocket needs to have picture of BVM in silver reflective pattern and the letters ‘BVM’ |
| • Make the BVM pocket bigger (same footprint as main bag) |
| • Add the word ‘patient’ to top of bag therefore: ‘Patient Transfer Bag’ |
| • Add card holder to identify where the bag originates (HDU ICU AE, etc.) on the top of the bag |
| • Backpack straps need more padding – secured at one end only so when carried like a backpack, patient pocket is uppermost |
| • Straps for securing on the trolley, bed, stack, etc. need to be more robust with an anchor around the whole bag. They also need to tighten and lock into place. The current configuration is the wrong way around |
| • More reflective flashes for teams out at night by repeating patient transfer bag in portrait. This will also assist with orientation of the backpack position |
| • Seams on the outside appeared curled over? |
| • Straps need to be tidier |
| Internal |
| • Addition of something to improve the rigidity of the insert sleeves. Allowing for better visibility in the bag and also to assist with repacking the bag |
| • Card holders for checklist that do not cover or block out the kit |
| • Circulation pouch needs attention – make entire pocket from red material, add wording to the outer cover indicating that there are items to check inside |
| • Addition of a documentation wallet to the inside of the main bag lid. Needs to be securable and orientated in such a way that when in use documents remain in |
| • Move the fluids for better weight distribution |
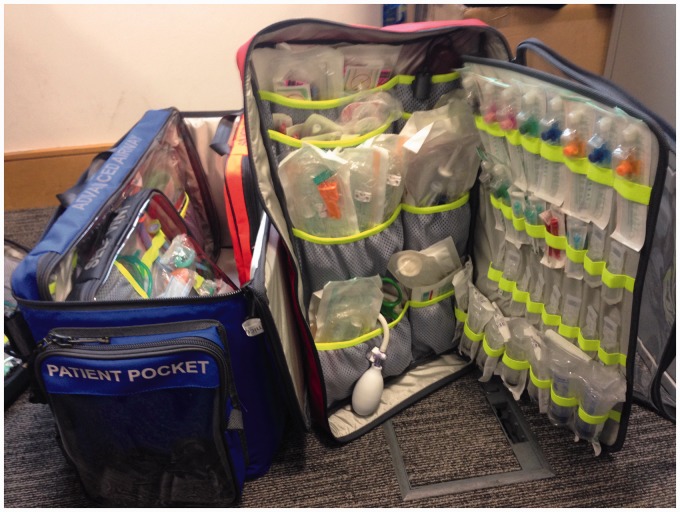
Figure 3.
The critical care transfer bag showing the insert sleeves and clear patient pocket.
Figure 4.
The ‘open book' design and clear panels enabling quick retrieval and checking of equipment.
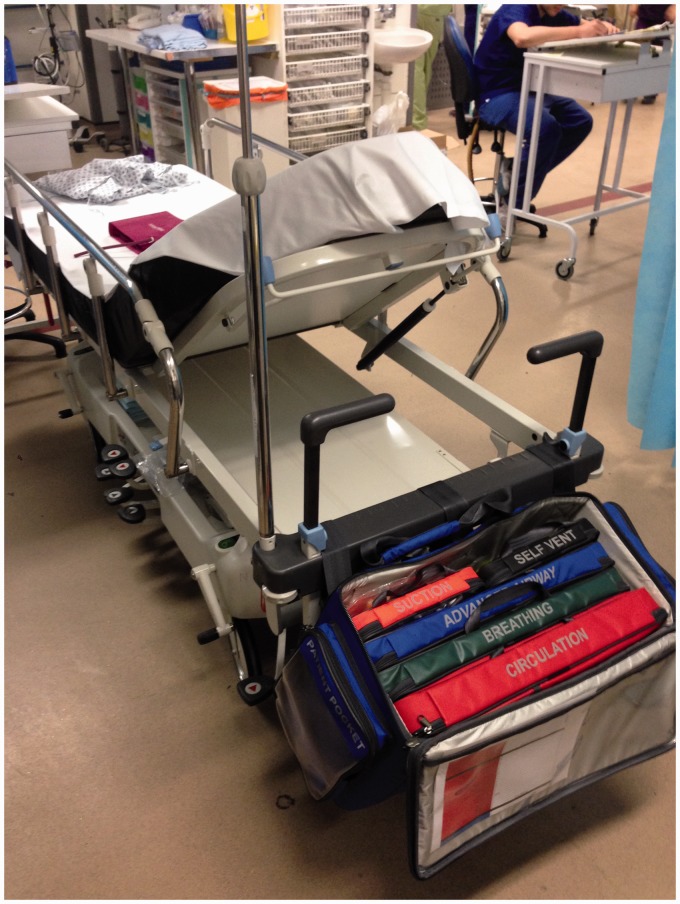
Figure 5.
The transfer bag securely attached to a hospital bed.
Figure 6.
The bag attached to an Emergency or Theatre patient trolley with easily accessible insert sleeves.
Figure 7.
The transfer bag attached to an ambulance patient trolley.
The ability to check the bag ‘at a glance’ due to the clear panels or ‘open book’ design of the pockets drastically reduced the time to check compared to the conventional critical transfer bags in use currently. The results from the trials timing staff checking the contents of transfer bags revealed an average time of less than 5 min for the NWLCCN prototype versus a minimum of 20 min for the current bags in use.
Discussion
The original aim of this project was to create a standardised ‘ideal’ critical care transfer bag with a condensed list of contents to reduce the problem of unfamiliarity with equipment that has been shown to increase the risk associated with critical care transfers. The modified Delphi method used has enabled a large group and a wide variety of clinicians to be involved in this process. The NWLCCN Transfer Bag and its contents have been ‘road tested’ in the clinical environment in multiple settings by large numbers of personnel to enable further modifications to make sure it is as ideal as possible. The NWLCCN Network is now applying the same methodology to paediatric and ECMO transfer bags.
This critical care transfer bag provides a standardised solution for our critical care network. A similar technique could be used to design a transfer bag for other regions. Alternatively, readers are welcome to adapt or adopt the above critical care transfer bag.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Haji-Michael P. Critical care transfers – a danger foreseen is half avoided. Crit Care 2005; 9: 343–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beckmann U, Gillies DM, Berenholtz SM, et al. Incidents relating to the intra-hospital transfer of critically ill patients. An analysis of the reports submitted to the Australian Incident Monitoring Study in Intensive Care. Intensive Care Med 2004; 30: 1579–1585. [DOI] [PubMed] [Google Scholar]
- 3.Droogh JM, Smit M, Hut J, et al. Inter-hospital transport of critically ill patients; expect surprises. Crit Care 2012; 16: R26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Handy JM, Suntharalingam G, Walsh A, et al. Improved patient safety during critical care transfers resulting from a sustained Network approach. Presented at International Forum on Quality and Safety in Healthcare (IHI), Paris, 2008.
- 5.The Intensive Care Society. Guidelines for the transport of the critically ill adult. 3rd ed. 2011. Appendix 6, Supplementary equipment for use during transport.
- 6.Dransfield M and Van Zwanenberg G. The network transfer bag. Presented at Annual NWLCCN Education Event. London, December 2015.