Abstract
Quitting smoking and aerobic exercise each improve health. Although smokers may be concerned that quitting smoking will reduce their quality of life, recent research has shown that cessation is associated with quality of life benefits. Elements of smoking cessation interventions, such as exercise, may contribute to changes in quality of life. However, it is unknown whether initiating exercise in the context of smoking cessation is associated with greater or different effects on quality of life than smoking cessation alone. The current study is a secondary analysis of data from a randomized trial (n = 61) of an exercise intervention for smoking cessation. We hypothesized that smoking abstinence and engagement in exercise would have positive, additive effects on quality of life at end-of-treatment, 6- and, 12-month follow-ups. Sedentary adult smokers were randomized to the exercise intervention or a health education control (HEC) group. Additionally, all participants received smoking cessation counseling and nicotine patches. Data were analyzed using actual engagement in exercise, rather than group assignment as a proxy for exercise engagement, because some HEC participants also began exercising. Abstinence was positively associated with higher total and physical health quality of life at follow-up. Exercise was not associated with total quality of life and only marginally associated with physical health quality of life, but was positively related to overall sense of well-being. Emphasizing that smoking cessation is associated with higher quality of life may help motivate smokers to initiate quit attempts.
Keywords: Smoking Cessation, Tobacco Cessation, Exercise, Physical Activity, Quality of Life
Introduction
Cigarette smokers report that whereas their quit attempts are often motivated by knowledge of long-term physical health benefits (Baha & Le Faou, 2010; Duncan, Cummings, Hudes, Zahnd, & Coates, 1992; Marshall et al., 2009; McKenna et al., 2001), concerns about more immediate negative effects on quality of life (QOL) constitute a significant barrier to quitting (Hendricks, Wood, Baker, Delucchi, & Hall, 2011; McKee, O’Malley, Salovey, Krishnan-Sarin, & Mazure, 2005; Pisinger, Aadahl, Toft, & Jorgensen, 2011). Against this backdrop, there has been increasing interest in the effects of smoking cessation on QOL. If smoking cessation improves rather than reduces QOL, conveying this information to smokers could alleviate their concerns and motivate quit attempts (Piper, Kenford, Fiore, & Baker, 2012).
Current smokers report poorer physical and mental health-related QOL than both non-smokers and ex-smokers (Davila et al., 2011; Heikkinen, Jallinoja, Saarni, & Patja, 2008; Mody & Smith, 2006; Mulder, Tijhuis, Smit, & Kromhout, 2001; Sarna, Bialous, Cooley, Jun, & Feskanich, 2008). A recent study (2012) demonstrated that health-related QOL improved in quitters and declined in continuing smokers at both one and three years relative to baseline. Additionally, although other QOL domains as well as total QOL decreased at one and three years relative to baseline among both quitters and continuing smokers, quitters reported significantly smaller decreases. Elements of smoking cessation interventions, such as aerobic exercise (M. H. Ussher, Taylor, & Faulkner, 2012), may also contribute to changes in QOL. Acute exercise produces beneficial effects with respect to psychological QOL including decreased craving and withdrawal symptoms, and affect (Haasova et al., 2012; Roberts, Maddison, Simpson, Bullen, & Prapavessis, 2012; Taylor, Ussher, & Faulkner, 2007; M. H. Ussher et al., 2012). Furthermore, independent of smoking, exercise has well-documented benefits on QOL (Penedo & Dahn, 2005).
We analyzed relationships among smoking cessation, initiation of aerobic exercise, and QOL within the first year after a quit attempt among sedentary smokers who participated in a randomized trial of an aerobic exercise intervention for smoking cessation (Abrantes et al., 2014). We hypothesized that abstinence and engagement in exercise would be associated with higher QOL relative to continued smoking and inactivity, respectively. Additionally, we hypothesized an additive effect of exercise.
Methods
Participants and Procedure
This study was approved by the Institutional Review Board of Butler Hospital. Details on the sample and procedures are reported elsewhere (Abrantes et al., 2014). In brief, participants (N = 61) were 18–65 years old, smoked ≥ 10 cigarettes/day, and had not engaged in regular aerobic exercise (≥20 min/day on ≥3 days/wk) for ≥ 6 months. Exclusion criteria were substance use disorder (except nicotine), bipolar disorder, eating disorder, or psychotic disorder, current suicidality or homocidality, physical inability to exercise (i.e., denied medical clearance by physician), pregnancy, or current use of pharmacotherapy for smoking cessation. Participants were randomized to either 1) a 12-week, group aerobic exercise intervention (AE) or 2) a 12-week, group health education control intervention (HEC) equated to AE for contact time. All participants (AE and HEC) also received 8 sessions of telephone counseling for smoking cessation and 8 weeks of transdermal nicotine patch (TNP). Follow-up assessments occurred at 3- (end of treatment), 6-, and 12-months.
The AE intervention consisted of supervised, moderate intensity exercise sessions at the study site once per week in a small group format and instruction to engage in additional unsupervised moderate intensity exercise at home or in the community. Supervised sessions began at 20 minutes duration and progressed to 40 minutes, while total exercise was gradually increased to 150 minutes by the end of week 12. AE participants also attended weekly 20-minute group sessions in which they were given cognitive-behavioral strategies to motivate adherence to exercise and received financial incentives for compliance with exercise. HEC participants attended weekly hour-long health education sessions in which exercise was not discussed. HEC participants were provided with financial incentives for attendance matched in amount to the AE condition.
Measures
Demographics and Smoking Characteristics
Demographics and Smoking Characteristics included nicotine dependence (Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991).
Smoking Status
Self-reported 7-day point prevalence abstinence at follow-ups was verified by expired carbon monoxide (CO; < 10ppm cutoff) or, in one instance, by the report of a family member of the participant because the participant was unable to provide CO.
Exercise Engagement
At follow-ups, participants were asked 2 questions: “Over the past 3 months, to the best of your knowledge, how many days per week on average did you exercise?” and “When you did exercise, how much time did you spend exercising?”. Their answers were used to calculate a continuous variable of average minutes of exercise per week during the 12 weeks preceding each follow-up period. This approach is consistent with an Exercise is Medicine initiative called the Exercise Vital Sign (Coleman et al., 2012).
Quality of Life (QOL)
The Quality of Life Enjoyment and Satisfaction Questionnaire – Short Form (Q-LES-Q-SF) (Endicott, Nee, Harrison, & Blumenthal, 1993), which includes 16 domains rated on 5-point scales with respect to the past week, was administered at baseline and all follow-ups.
Data Analysis
Linear mixed models were used to examine the time-varying effects of smoking status (smoking vs. abstinent) and exercise engagement over time on QOL. We used exercise engagement as the independent variable, rather than group assignment (AE vs. HEC) as a proxy for exercise engagement, because preliminary analyses revealed that a significant proportion of HEC participants initiated exercise during the study (Abrantes et al., 2014) (see Table 1).
Table 1.
Demographics, Baseline Smoking Characteristics, and Exercise Engagement
| Exercise (n=30) | Health Education (n=31) | |
|---|---|---|
| Demographics (n unless specified) | ||
| Gender (female) | 19 | 21 |
| Age in Years (Mean and SD) | 47.1 (8.5) | 47.5 (10.7) |
| Non-Hispanic White | 28 | 26 |
| College graduate | 9 | 9 |
| Household Income < $30,000/year | 6 | 12 |
| Employed | 21 | 17 |
| Body Mass Index (Mean and SD) | 28.5 (4.2) | 28.9 (7.0) |
| Smoking (Means and SDs) | ||
| Smoking Age of Onset (Years) | 15.1 (3.5) | 15.9 (5.6) |
| Years of regular smoking | 27.4 (9.1) | 27.5 (11.1) |
| Number of lifetime quit attempts | 3.2 (2.8) | 4.4 (3.1) |
| Cigarettes/day | 20.3 (9.9) | 19.4 (8.1) |
| Nicotine Dependence (FTND) | 5.9 (2.1) | 5.6 (1.6) |
| Exercise Engagement in Minutes per Week (Means and SDs) | ||
| 3-month follow-up | 133.9 (81.2) | 95.7 (91.4) |
| 6-month follow-up | 113.3 (129.3) | 140.0 (132.7) |
| 12-month follow-up | 91.0 (138.9) | 92.8 (120.0) |
| Participants Exercising ≥ 150 Min/Week (n) | ||
| 3-month follow-up | 9 | 7 |
| 6-month follow-up | 7 | 9 |
| 12-month follow-up | 5 | 5 |
| Participants Exercising Continuously* (n) | 2 | 2 |
Note. SD = Standard Deviation,
≥ 150 min/week at all follow-ups
Specifically, we examined associations of smoking and exercise engagement with Q-LES-Q-SF total score, as well as with individual domains of physical health, overall sense of well-being (well-being), and overall life satisfaction and contentment (satisfaction). We limited our analysis to these three QOL domains to reduce risk of Type I error. For each Q-LES-Q-SF outcome (total score, physical health, well-being, satisfaction), we ran a model that included main effects of smoking and exercise engagement, and a second model that included main effects and a smoking status × exercise engagement interaction term. All models controlled for time, treatment condition (AE vs. HEC), gender, age, and corresponding baseline Q-LES-Q-SF score, and we considered p’s < .05 as significant. In all models, only the intercept was specified as random as allowing other time-varying predictors (i.e., smoking status and exercise engagement) did not improve model fit. Models were run with R Statistical Software 2.15.2 using the ‘lme’ function in the ‘nlme’ package. Due to missing data, the sample size analyzed in each model ranged from 48 to 51 participants.
Results
Baseline Characteristics and Preliminary Analyses
AE and HEC participants did not differ in baseline demographic or smoking characteristics (see Table 1). Trial outcomes have been reported previously (Abrantes et al., 2014). In brief, 7-day point prevalence abstinence rates were on average 2.02 times higher in AE vs. HEC: 40.0% vs. 22.6% at 3 months, 26.7% vs. 12.9% at 6 months, and 22.6% vs. 12.9% at 12 months. These differences were not statistically significant (all p’s > .05), likely due to the small sample size.
Q-LES-Q-SF Total Score and Physical Health
The main effects model revealed that abstinence was associated with higher total score (p = .02) (see Figure 1). However, there was no significant effect of exercise engagement (p = .19) on total score. Also, the interaction model revealed no significant interaction of smoking and exercise status on total score (p = .49). Results for physical health paralleled total score. See Table 2.
Figure 1.
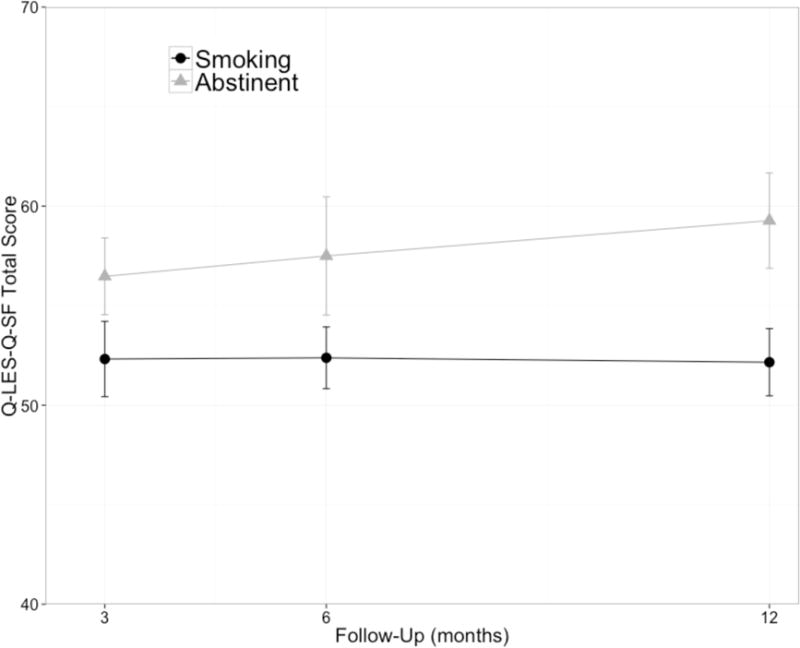
Mean score for Total QOL at each follow-up by smoking status (smoking vs. abstinent).
Table 2.
Linear Mixed Model Results for Q-LES-Q-SF
| Parameter | Total Score
|
Physical Health
|
Well-Being
|
Satisfaction
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI | p | Estimate | 95% CI | p | Estimate | 95% CI | p | Estimate | 95% CI | p | |
| Intercept | 13.66 | (−7.68, 35.0) | 0.21 | 1.81 | (0.52, 3.10) | 0.01 | 1.49 | (−0.02, 3.00) | 0.06 | 1.72 | (0.03, 3.41) | 0.05 |
| Time | 1.98 | (−1.53, 5.49) | 0.27 | 0.02 | (−0.41, 0.45) | 0.93 | 0.29 | (−0.18, 0.76) | 0.22 | 0.02 | (−0.39, 0.43) | 0.91 |
| Condition | −0.23 | (−4.48, 4.02) | 0.92 | 0.25 | (−0.10, 0.60) | 0.19 | 0.03 | (−0.34, 0.40) | 0.88 | 0.16 | (−0.25, 0.57) | 0.44 |
| Gender | 1.37 | (−3.04, 5.78) | 0.55 | 0.18 | (−0.19, 0.55) | 0.35 | 0.04 | (−0.35, 0.43) | 0.84 | −0.03 | (−0.46, 0.40) | 0.90 |
| Age | 0.06 | (−0.16, 0.28) | 0.58 | 0.01 | (−0.01, 0.03) | 0.55 | −0.01 | (−0.03, 0.01) | 0.56 | 0.00 | (−0.02, 0.02) | 0.94 |
| Baseline score | 0.59 | (0.30, 0.88) | 0.00 | 0.29 | (0.09, 0.49) | 0.01 | 0.55 | (0.33, 0.77) | 0.00 | 0.49 | (0.25, 0.73) | 0.00 |
| Smoking Status | 4.44 | (0.89, 7.99) | 0.02 | 0.47 | (0.10, 0.84) | 0.01 | 0.20 | (−0.19, 0.59) | 0.31 | 0.35 | (−0.04, 0.74) | 0.07 |
| Exercise (minutes) | 0.01 | (−0.004, 0.021) | 0.19 | 0.00 | (−0.000, 0.003) | 0.07 | 0.00 | (0.000, 0.003) | 0.047 | 0.00 | (−0.001, 0.001) | 0.93 |
Note: 95% CI = 95% confidence interval
Q-LES-Q-SF Well-Being and Satisfaction
The main effects model indicated a positive association between exercise engagement and well-being (p = .047) (see Figure 2). However, there was no significant effect of smoking status on well-being (p = .31). Abstinence was trend-level associated with greater satisfaction than smoking (p = .07), but no association between exercise engagement and satisfaction was found (p = .93). For both well-being and satisfaction, there was no significant interaction between smoking and exercise engagement (p = .13 and p = .11, respectively). See Table 2.
Figure 2.
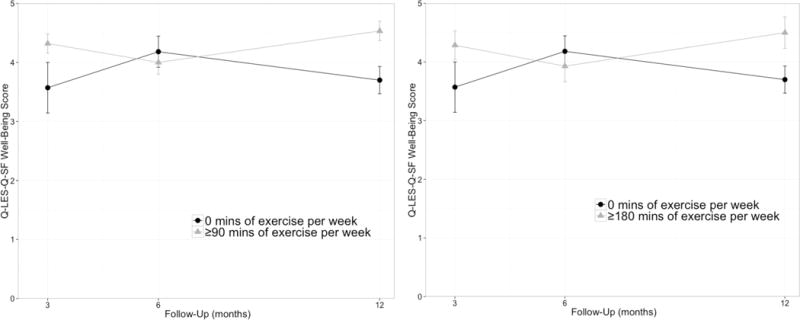
Mean score for Overall Sense of Well-Being at each follow-up by minutes of exercise per week.
Discussion
We predicted that smoking abstinence and engagement in aerobic exercise would have additive benefits for quality of life (QOL) within the first year following a quit attempt. Abstinence was indeed associated with higher total and physical health QOL than smoking, consistent with previous research (Piper et al., 2012). With respect to overall sense of well-being, there was a significant effect of exercise engagement, such that a higher activity level was associated with greater well-being, but there was no effect of abstinence. Contrary to our hypothesis, exercise engagement did not exert a significant effect on total QOL and had only a marginal effect (p = .07) on physical health QOL. Perhaps the effect of initiating exercise was overpowered or masked by the effects of quitting smoking. The primary physical health changes that occur upon smoking cessation are similar to increasing physical fitness (Asthana et al., 2012); participants who quit smoking and were highly active may have attributed changes in perceived physical health primarily to quitting smoking. Likewise, among participants who exercised but continued smoking, the negative effects of smoking on breathing and lung capacity may have obscured the benefits of the exercise. Research indicates that smokers may experience less benefit from exercise than non-smokers (Hashizume, Kusaka, & Kawahara, 1999) and perceive their exertion to be higher intensity than their heart rate indicates (M. Ussher, Nunziata, Cropley, & West, 2001).
Limitations and Future Directions
Our sample size was small (N = 61) and variability in responses to single items was low; therefore, our power to detect effects was limited. Replication in a larger sample using other QOL measures that include multiple items within each domain is recommended. Second, as neither smoking status nor exercise engagement was randomly assigned, direction of causality cannot be determined. Third, most participants were non-Hispanic White. Finally, exercise was self-reported; future research should incorporate objective measurement. Despite these limitations, these findings add to a growing body of research in support of potential QOL benefits associated with smoking cessation.
Acknowledgments
This work was supported by the National Institute on Drug Abuse under Grant K23 DA019950 awarded to Ana M. Abrantes, Ph.D.
Footnotes
The authors have no conflicts of interest to disclose.
References
- Abrantes AM, Bloom EL, Strong DR, Riebe D, Marcus BH, Desaulniers J, Brown RA. A preliminary randomized controlled trial of a behavioral exercise intervention for smoking cessation. Nicotine & Tobacco Research. 2014;16(8):1094–1103. doi: 10.1093/ntr/ntu036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asthana A, Piper ME, McBride PE, Ward A, Fiore MC, Baker TB, Stein JH. Long-term effects of smoking and smoking cessation on exercise stress testing: three-year outcomes from a randomized clinical trial. American Heart Journal. 2012;163(1):81–87 e81. doi: 10.1016/j.ahj.2011.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baha M, Le Faou AL. Smokers’ reasons for quitting in an anti-smoking social context. Public Health. 2010;124(4):225–231. doi: 10.1016/j.puhe.2010.02.011. [DOI] [PubMed] [Google Scholar]
- Coleman KJ, Ngor E, Reynolds K, Quinn VP, Koebnick C, Young DR, Sallis RE. Initial validation of an exercise “vital sign” in electronic medical records. Medicine and Science in Sports and Exercise. 2012;44(11):2071–2076. doi: 10.1249/MSS.0b013e3182630ec1. [DOI] [PubMed] [Google Scholar]
- Davila EP, Zhao W, Byrne M, Hooper MW, Messiah A, Caban-Martinez A, Lee DJ. Health-related quality of life and nicotine dependence, Florida 2007. American Journal of Health Behavior. 2011;35(3):280–289. doi: 10.5993/ajhb.35.3.3. [DOI] [PubMed] [Google Scholar]
- Duncan CL, Cummings SR, Hudes ES, Zahnd E, Coates TJ. Quitting smoking: reasons for quitting and predictors of cessation among medical patients. Journal of General Internal Medicine. 1992;7(4):398–404. doi: 10.1007/BF02599155. [DOI] [PubMed] [Google Scholar]
- Endicott J, Nee J, Harrison W, Blumenthal R. Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacology Bulletin. 1993;29(2):321–326. [PubMed] [Google Scholar]
- Haasova M, Warren FC, Ussher M, Janse Van Rensburg K, Faulkner G, Cropley M, Taylor AH. The acute effects of physical activity on cigarette cravings: Systematic review and meta-analysis with individual participant data (IPD) Addiction. 2012 doi: 10.1111/j.1360-0443.2012.04034.x. [DOI] [PubMed] [Google Scholar]
- Hashizume K, Kusaka Y, Kawahara K. Effects of cigarette smoking on endurance performance levels of 16- to 19-year-old males. Environmental Health and Preventive Medicine. 1999;4(2):75–80. doi: 10.1007/BF02931998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom test for nicotine dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Heikkinen H, Jallinoja P, Saarni SI, Patja K. The impact of smoking on health-related and overall quality of life: a general population survey in Finland. Nicotine & Tobacco Research. 2008;10(7):1199–1207. doi: 10.1080/14622200802163142. [DOI] [PubMed] [Google Scholar]
- Hendricks PS, Wood SB, Baker MR, Delucchi KL, Hall SM. The Smoking Abstinence Questionnaire: measurement of smokers’ abstinence-related expectancies. Addiction. 2011;106(4):716–728. doi: 10.1111/j.1360-0443.2010.03338.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall EC, Vujanovic AA, Kutz A, Gibson L, Leyro T, Zvolensky MJ. Reasons for quitting smoking prior to a self-quit attempt among smokers with and without posttraumatic stress disorder or other anxiety/mood psychopathology. American Journal on Addictions. 2009;18(4):309–315. doi: 10.1080/10550490902925763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee SA, O’Malley SS, Salovey P, Krishnan-Sarin S, Mazure CM. Perceived risks and benefits of smoking cessation: gender-specific predictors of motivation and treatment outcome. Addictive Behaviors. 2005;30(3):423–435. doi: 10.1016/j.addbeh.2004.05.027. [DOI] [PubMed] [Google Scholar]
- McKenna H, Slater P, McCance T, Bunting B, Spiers A, McElwee G. Qualified nurses’ smoking prevalence: their reasons for smoking and desire to quit. Journal of Advanced Nursing. 2001;35(5):769–775. doi: 10.1046/j.1365-2648.2001.01909.x. [DOI] [PubMed] [Google Scholar]
- Mody RR, Smith MJ. Smoking status and health-related quality of life: as findings from the 2001 Behavioral Risk Factor Surveillance System data. American Journal of Health Promotion. 2006;20(4):251–258. doi: 10.4278/0890-1171-20.4.251. [DOI] [PubMed] [Google Scholar]
- Mulder I, Tijhuis M, Smit HA, Kromhout D. Smoking cessation and quality of life: the effect of amount of smoking and time since quitting. Preventive Medicine. 2001;33(6):653–660. doi: 10.1006/pmed.2001.0941. [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Current Opinion in Psychiatry. 2005;18(2):189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- Piper ME, Kenford S, Fiore MC, Baker TB. Smoking cessation and quality of life: changes in life satisfaction over 3 years following a quit attempt. Annals of Behavioral Medicine. 2012;43(2):262–270. doi: 10.1007/s12160-011-9329-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisinger C, Aadahl M, Toft U, Jorgensen T. Motives to quit smoking and reasons to relapse differ by socioeconomic status. Preventive Medicine. 2011;52(1):48–52. doi: 10.1016/j.ypmed.2010.10.007. [DOI] [PubMed] [Google Scholar]
- Roberts V, Maddison R, Simpson C, Bullen C, Prapavessis H. The acute effects of exercise on cigarette cravings, withdrawal symptoms, affect, and smoking behaviour: systematic review update and meta-analysis. Psychopharmacology. 2012;222(1):1–15. doi: 10.1007/s00213-012-2731-z. [DOI] [PubMed] [Google Scholar]
- Sarna L, Bialous SA, Cooley ME, Jun HJ, Feskanich D. Impact of smoking and smoking cessation on health-related quality of life in women in the Nurses’ Health Study. Quality of Life Research. 2008;17(10):1217–1227. doi: 10.1007/s11136-008-9404-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor AH, Ussher MH, Faulkner G. The acute effects of exercise on cigarette cravings, withdrawal symptoms, affect and smoking behaviour: a systematic review. Addiction. 2007;102(4):534–543. doi: 10.1111/j.1360-0443.2006.01739.x. [DOI] [PubMed] [Google Scholar]
- Ussher M, Nunziata P, Cropley M, West R. Effect of a short bout of exercise on tobacco withdrawal symptoms and desire to smoke. Psychopharmacology. 2001;158(1):66–72. doi: 10.1007/s002130100846. [DOI] [PubMed] [Google Scholar]
- Ussher MH, Taylor A, Faulkner G. Exercise interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2012;1:CD002295. doi: 10.1002/14651858.CD002295.pub4. [DOI] [PubMed] [Google Scholar]


