Abstract
Background
Family members of critically ill patients report high levels of conflict with clinicians, have poor understanding of prognosis, struggle to make decisions, and experience substantial symptoms of anxiety, depression, and post-traumatic stress regardless of patient survival status. Efficient interventions are needed to prepare these families to act as patient proxies.
Objectives
To assess a brief “patient activation” intervention designed to set expectations and prepare families of adult intensive care unit (ICU) patients to communicate effectively with the clinical team.
Design
Phase I study of acceptability and immediate side effects.
Setting and participants
122 healthcare proxies of 111 consecutive patients with a stay of ≥24 hours in the Johns Hopkins Hospital Medical ICU (MICU), in Baltimore, Maryland.
Intervention
Reading aloud to proxies from a booklet (Flesch-Kincard reading grade level 3.8) designed with multidisciplinary input including from former MICU proxies.
Results
Enrolled proxies had a median age of 51 years old with 83 (68%) female, and 55 (45%) African-American. MICU mortality was 18%, and 37 patients (33%) died in hospital or were discharged to hospice. Among proxies 98% (95% CI: 94% - 100%) agreed or strongly agreed that the intervention was appropriate, 98% (95% CI: 92% - 99%) agreed or strongly agreed that it is important for families to know the information in the booklet, and 54 (44%, 95% CI 35%– 54%) agreed or strongly agreed that parts of the booklet are upsetting. Upset vs. non-upset proxies were not statistically or substantially different in terms of age, sex, education level, race, relation to the patient, or perceived decision-making authority.
Conclusions
This patient activation intervention was acceptable and important to nearly all proxies. Frequently, the intervention was simultaneously rated as both acceptable/important and upsetting. Proxies who rated the intervention as upsetting were not identifiable based on readily available proxy or patient characteristics.
Introduction
The proportion of Medicare beneficiaries mechanically ventilated during the last month of life has risen steadily over the last 10 years.[1,2] The majority of these patients lack decision-making capacity and reply on family members to communicate with the intensive care unit (ICU) clinical team.[3,4] These family members report high levels of conflict with clinicians,[5,6] have poor understanding of prognosis,[7–10] struggle to make decisions,[11–13] and experience substantial symptoms of anxiety, depression[14,15], and post-traumatic stress [16–19] regardless of patient survival status. In response to these challenges, the Society of Critical Care Medicine and the American Thoracic Society have endorsed clinical practice guidelines on family-centered care in the ICU[20] and engaging family members in shared decision making[21].
ICU clinicians commonly report that family members’ incorrectly optimistic expectations for patient recovery is a major challenge to effective communication [22–25]. Effective communication with families is also time-consuming, not consistently taught during critical care training programs[26], and requires advanced communication skills [27,28]. It is therefore unsurprising that prompt, multi-disciplinary family meetings have not been widely adopted[29,30] despite their endorsement as an indicator of high-quality ICU care [31].
Against this background, we recognize that family members of incapacitated patients have strong incentives to ensure that communication with ICU clinicians is clear and meaningful. “Patient activation” is a type of intervention that seeks to equip patients with the skills and confidence required to effectively engage healthcare providers for purposes of clinical decision-making [32,33]. Although traditionally used directly with patients in the outpatient setting, patient activation can be adapted to provide a similar intervention for ICU families. Therefore, we designed an intervention to help set appropriate expectations about patient recovery, explain the role of a healthcare proxy in the ICU, and prepare families to communicate effectively with the ICU clinical team. We recognize that family members prefer different decision-making roles and that some family members have strong emotional or psychological aversions to assuming decision-making responsibility[34]. Hence, this evaluation was designed as a Phase I study to assess the acceptability and immediate side effects of this brief activation intervention for ICU families.
Methods
Intervention design
The intervention was designed to 1) help set expectations about patient recovery from critical illness 2) educate adult family members in the medical intensive care unit (MICU) at Johns Hopkins Hospital (JHH) about the role of a healthcare proxy and 3) prepare proxies to communicate effectively with their ICU clinical team. Input from multi-disciplinary stakeholders was solicited during design of the intervention. First, as part of a qualitative study of physician-perceived facilitators and barriers to discussing post-hospitalization outcomes with ICU families,[24] intensivists at 20 hospitals across the U.S. were asked to describe the behaviors of effective ICU proxies, and to suggest questions that proxies should ask intensivists. We used these responses to draft an initial version of a short booklet and elicited feedback from the following JHH stakeholders: the JHH Patient and Family Advisory Council, MICU social workers, risk management (legal counsel), patient relations, chaplaincy and spiritual care, the MICU end-of-life interest group (primarily comprised of nurses), MICU nurse practitioners and physician assistants, as well as pulmonary and critical care fellows and MICU attending physicians. Iterative changes were made based on feedback throughout this process. The families of 6 current MICU patients who were not enrolled in the study also were asked to provide feedback.
The resulting intervention consisted of reading aloud from the final version of the booklet and then providing participants with the booklet for review. The 554-word booklet used in this study required 3.5 minutes to read aloud, with a Flesch-Kincard reading grade level of 3.8 and Flesch reading ease score of 85. The booklet contains black-and-white icons designed to be recognizable to a socio-economically and racially diverse population [35], and is freely available for download under at www.piperscience.org/proxy-activation. All interactions with study participants, including recruiting, consenting, and delivering the intervention were performed by white females (A.E.T., C.M.C., R.K.C.) of similar age (25–35 years old).
Study design
This investigation was designed as a Phase I study to assess the intervention’s acceptability to ICU families and identify immediate side effects [36]. We assessed acceptability by asking all participants to respond to the following two statements using a 5-point Likert scale ranging from Strongly agree to Strongly disagree: 1) “The booklet is appropriate for adult friends and family-members of ICU patients.” 2) “It is important for families of ICU patients to know the information in the booklet.” On an a priori basis, we defined the intervention as acceptable if ≥80% of participants described the intervention as both appropriate and important for adult friends and family members of ICU patients. Study sample size was designed to estimate the proportions of ICU proxies who rated the intervention as appropriate and important with a 5% margin of error (95% confidence interval width of 10%). We also anticipated that participants might find information in the booklet upsetting at the time of the intervention and treated this as a potential immediate side-effect. This outcome was evaluated by asking all participants to respond to the statement “Parts of the booklet are upsetting” using the same 5-point Likert scale.
Recruitment
All recruitment took place in the JHH MICU, located in the inner city of Baltimore, Maryland between January and May 2016. The MICU census was screened 7 days per week to identify all consecutive eligible study participants. Family members[20] became eligible for recruitment as soon as their loved one had been a patient in the MICU for 24 hours. When multiple members of the family were available to participate the study team members enrolled the patient’s health agent or surrogate. Evaluation of this recruitment strategy have been previously published.[37] In this paper we refer to these people as proxies to encompass both healthcare agents and healthcare surrogates who have distinct legal definitions under Maryland state law.[38,39] If the family member initially enrolled was not the patient’s legal healthcare proxy, additional attempts were made to also enroll a legal proxy. Interviews were conducted in private spaces within the MICU but outside the patient’s room. Participants provided oral, in-person consent, which was documented using a standardized consent form and received a $10 gift card upon interview completion. Additional information about family recruitment and data collection are provided in Table A of S1 File. Johns Hopkins Medicine IRB Committee X approved this study number: IRB00080137. The IRB deemed oral consent as appropriate because participating in the study did not involve any procedure for which written consent is normally required outside of the research context.
Analyses
The primary outcomes were the proportions of participants who agreed or strongly agreed that the intervention is appropriate and that it is important for families of ICU patients to know the information conveyed by the intervention. Starting during the third week of the study, participants who agreed or strongly agreed that the information was important were asked to identify the most important pages in the booklet, and asked their opinion, via multiple-choice survey questions, regarding when and how the intervention should be delivered.
The secondary outcome was the proportion of participants who agreed or strongly agreed that the intervention was upsetting. Participants who found the intervention upsetting were asked to discuss what they found upsetting via an open-ended question. Transcribed narrative responses to this question were analyzed using a limited application of the framework method[40] with A.E.T., C.M.C., and R.K.C each independently applying open coding, then agreeing on themes, and finally independently charting the themes present in each response.
Participants who agreed or strongly agreed that the intervention was upsetting versus those who did not agree were compared for differences using descriptive statistics, the Wilcoxon-Mann-Whitney two-sample test for continuous variables, the Chi-square test for categorical values, and the Fisher’s exact test when cells counts were <10. The study was not powered or designed to test hypotheses about differences in the distribution of participant or patient characteristics; therefore, to encourage appropriate interpretation of statistical comparisons, we report both the p-value and the absolute value of the effect size (Cohen’s d) to provide an indication of the magnitude of effect.[41,42] The “Neither Agree or Disagree” response was combined with the Strongly agree and Agree responses as a sensitivity analysis. All statistics were generated using the R programming language version 3.3.2 (Vienna, Austria).
Results
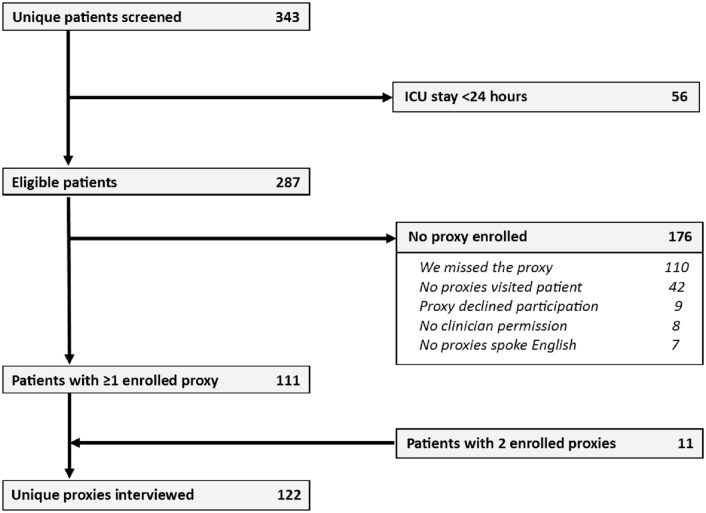
We enrolled 122 proxies representing 111 eligible patients (Fig 1). Enrolled proxies had a median age of 51 years old (interquartile range (IQR) 39, 61) and 14 years of formal education (IQR 12, 16), with 83 (68%) female, 55 (45%) Black or African-American, and 79 (65%) the legal healthcare proxy according to Maryland law (Table 1). Patients had a median length of stay of 5 days (IQR 3,9) in the ICU and of 11 days (IQR 7, 25) in the hospital,(Table 2) with 101 patients (91%) living at home prior to hospitalization. ICU mortality was 18% and 37 patients (33%) died in hospital or were discharged to hospice.
Fig 1. Study flow diagram.
Table 1. Characteristics of interviewed proxies.
| Characteristic | N = 122 |
|---|---|
| Agea, median (IQR) | 51 (39, 61) |
| Femalea, n (%) | 83 (68%) |
| Self-identified racea, n (%) | |
| Black or African American | 55 (45%) |
| White | 55 (45%) |
| Other | 8 (7%) |
| Years of education, median (IQR) | 14 (12, 16) |
| Have you ever supported a loved one in an ICU before?a Yes (%) | 75 (61%) |
| Patient's legal surrogate decision-maker | 79 (65%) |
| Relation to Patientb | |
| Daughter | 31 (25%) |
| Female Spouse or Partner | 31 (25%) |
| Male Spouse or Partner | 15 (12%) |
| Parent | 14 (11%) |
| Sibling | 12 (10%) |
| Non-nuclear family member | 10 (8%) |
| Son | 9 (7%) |
a Proxies declined to report age (n = 2), sex (n = 2), race (n = 4), and previous experience as an ICU proxy (n = 3)
b Percentages do not sum to 100% due to rounding
Table 2. Patient characteristics and outcomes.
| Characteristic | N = 111 |
|---|---|
| Age, Median (IQR) | 58 (48,69) |
| Female, N (%) | 56 (50%) |
| Race, N (%) | |
| White | 49 (44%) |
| Black or African American | 48 (43%) |
| Other | 14 (13%) |
| Median income of zip code, $1000s of USDa, Median (IQR) | 59.1 (36.0, 81.8) |
| Location prior to hospitalizationb, N (%) | |
| House/Apt (independent) | 72 (65%) |
| House/Apt (with assistance) | 29 (26%) |
| Long-Term ventilator/acute rehabilitation/nursing home | 9 (8%) |
| Admission diagnosis, N (%) | |
| Respiratory failure | 49 (44%) |
| Sepsis | 23 (21%) |
| Gastrointestinal | 11 (10%) |
| Cardiovascular | 6 (6%) |
| Other | 22 (20%) |
| Code Status after 24 hours in ICU, N (%) | |
| Full codec | 97 (87%) |
| Full code with specific treatment limitations (e.g., No hemodialysis) | 6 (5%) |
| Do Not Resuscitate and Do Not Intubate | 8 (7%) |
| ICU length of stay in days, median (IQR) | 5 (3,9) |
| Subsequent withdrawal of life-support in the ICUb, N (%) | 21 (19%) |
| Subsequent death in ICU, N (%) | 20 (18%) |
| Hospital length of stay in days, median (IQR) | 11 (7,25) |
| Subsequent hospital discharge disposition, N (%) | |
| House/Apt (independent) | 34 (31%) |
| House/Apt (with home care) | 14 (13%) |
| Died | 29 (26%) |
| Hospice | 8 (7%) |
| Other, including inpatient facilities | 26 (23%) |
Abbreviation: DNI, Do not intubate; DNR, Do not resuscitate; ICU, Intensive care unit; IQR, Interquartile Range
a U.S. Census Bureau 2010–2014; $41,819 median household income for Baltimore City; $74,194 median household income for MD state. No zip code was provided for 1 patient from Saudi Arabia.
b Missing for one patient
c 51 (53%) of patients herein designated as full code didn’t have a documented code status 24 hours after ICU admission.
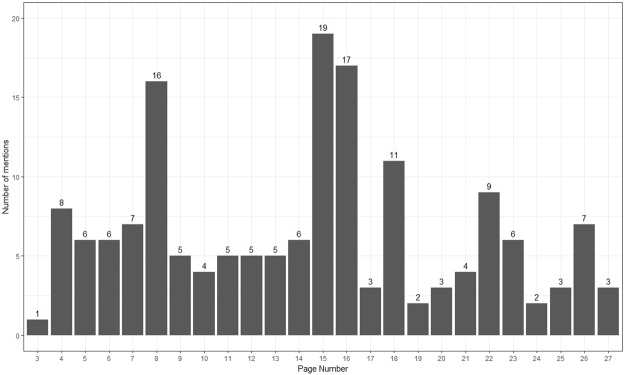
Among the 122 proxies interviewed, 120 (98%, 95% CI 94% - 100%) agreed or strongly agreed that the intervention booklet was appropriate for adult friends and family of ICU patients, and 119 (98%, 95% CI 92% - 99%) agreed or strongly agreed that it is important for families to know the information in the booklet (Table 3). Although every page was cited by at least one proxy as being the most important, the most frequently cited pages page 15, which guides proxies who believe their loved one may be dying on what to ask their doctor, and page 16 which stresses that proxies are not alone and are welcome to work with their family or religious leader (Fig 2). Rather than citing a specific page as being important, many proxies instead indicated a section or theme of the booklet. The section with questions that proxies should ask was cited by 33 unique proxies (Table 4).
Table 3. Proxy responses to questions about booklet content and delivery.
| The 3 questions below were asked of all 122 proxies. | No. proxies |
| "The booklet is appropriate for adult friends and family-members of ICU patients." n (%) | |
| Strongly agree | 46 (38%) |
| Agree | 74 (61%) |
| Neither agree or disagree | 0 (0%) |
| Disagree | 2 (2%) |
| Strongly disagree | 0 (0%) |
| "It is important for families of ICU patients to know the information in the booklet." n (%) | |
| Strongly agree | 69 (57%) |
| Agree | 50 (41%) |
| Neither agree or disagree | 2 (2%) |
| Disagree | 1 (1%) |
| Strongly disagree | 0 (0%) |
| "Parts of the booklet are upsetting." n (%) | |
| Strongly Agree | 6 (5%) |
| Agree | 48 (39%) |
| Neither agree or disagree | 7 (6%) |
| Disagree | 49 (40%) |
| Strongly Disagree | 12 (10%) |
| The following question was asked of all proxies who agreed or strongly agreed that it is important for families of ICU patients to know the information in the booklet. | |
| "In your opinion, which pages in the booklet are most important for ICU proxies to know?" (list all pages mentioned)a | Number of mentions |
| Pages with background information about proxy decision-makers | 42 (34%) |
| Pages that address formulating treatment goals | 39 (32%) |
| Tips for being a great proxy and recommended questions to ask doctors | 79 (65%) |
| Contact information for support resources (social work, chaplaincy, etc.) | 21 (17%) |
| The 2 questions below were added to the interview in week 3 of the study and were only asked of proxies who agreed or strongly agreed that it was important for families to know the information in the booklet, generating 97 responses. | |
| "In your opinion, when should ICU proxies receive the information in the booklet?" n (%) | |
| As soon as they arrive in the ICU | 57 (59%) |
| After they’ve had a chance to speak to a doctor about their loved ones care | 33 (34%) |
| Only if their loved one’s health isn’t improving | 6 (6%) |
| Declined | 1 (1%) |
| "In your opinion, what is the best way to share the information in the booklet with ICU proxies?" n (%) | |
| In a face-to-face conversation | 54 (56%) |
| On paper (for example the booklet) | 32 (33%) |
| In a video (for example on an iPad or on YouTube) | 9 (9%) |
| In a conversation on the phone | 2 (2%) |
a While some proxies cited specific page numbers, others cited entire sections of the booklet such as "The goals section" or "The pages with questions to ask the doctors." The number of times individual pages in the booklet were cited is provided in Supplemental information.
Fig 2. Important booklet pages according to ICU proxies.
Table 4. Proxies responses to the question: “Which page or part of the booklet did you find upsetting and why was it upsetting?” (N = 122).
| Theme and exemplar quotes | Number of quotes |
|---|---|
| Acknowledgement that critically ill patients may die | 15 (12%) |
| “Anytime you talk about death that's always upsetting because people don't want to address that option, even though it is inevitable.” | |
| “The part that talked about the patient could die.” | |
| Page 15 which states: “Some patients are so sick, that their goals cannot be reached. If you are worried that your loved one is dying and treatment will not help, ask a doctor: “Is it time to let go?”) | 12 (10%) |
| “Page 15—it’s hard to see!” | |
| “Page 15. It’s hard to ask the doctor: ‘Is it time to give up?’” | |
| The section of the booklet containing examples of patient goals | 10 (8%) |
| “The goals are sad.” | |
| “Reading about goals.” | |
| Making decisions | 9 (7%) |
| “Just the fact that they [proxies] will have to make decisions.” | |
| “The reality of letting go and needing to make a decision.” | |
| Uncertainty about the patient’s prognosis | 8 (7%) |
| “When it says [that] no one knows exactly what will happen.” | |
| “You never really know what will happen to someone you love.” | |
| Parts of the booklet related directly to the proxy’s loved one in the ICU | 7 (6%) |
| “Page 23 because that is what it looked like when we were talking about whether to take him off the ventilator.” | |
| “Because we are here with a son who may die.” | |
| Acknowledgement that some patients aren’t able to return to living in their homes | 6 (5%) |
| “Knowing that a patient’s not going to come home. I don’t like to hear that part.” | |
| “Thinking about if they won’t come home.” | |
| The situation faced by families in the ICU is upsetting–not the booklet content | 6 (5%) |
| “The whole situation is upsetting, not one particular page.” | |
| “Some people don’t realize the seriousness of this situation. People could die!” | |
| Page 11 which states: “But many people have problems that cannot be cured like severe lung disease, kidney failure, and end-stage cancer. These people have important goals too.” | 6 (5%) |
| “Page 11, because some of these run in my family.” | |
| “Page 11. My husband has some of those.” | |
| Use of the word “die” | 3 (2%) |
| “The use of the word ‘die.’ It feels a little cold. Maybe use something with less of a punch like ‘passing.’” | |
| “All the pages that have the death word because it’s just too upsetting to think your loved one is going to die.” | |
| Negativity | 1 (1%) |
| “Because it was negative. Because God can heal anything. It was negativity that you’re putting on people.” |
Histogram of booklet pages cited by proxies in response to the question: “In your opinion, which pages in the booklet are most important for ICU proxies to know?” Many proxies cited multiple pages of the booklet as being important. The written content of each page is provided within Table B of S1 File. Complete content including images are available for download at www.piperscience.org/proxy-activation.
Of these same 122 proxies, 54 (44%, 95% CI 35%– 54%) agreed or strongly agreed that parts of the booklet are upsetting. Among the proxies who found the intervention upsetting, 51 (94%) agreed or strongly agreed that the intervention was simultaneously acceptable and important. In fact, 5 of the 6 proxies who strongly agreed that the booklet was upsetting, also strongly agreed that it is important for families to know the information in the booklet. Among proxies asked to elaborate on what was upsetting, the most common theme mentioned by 15 proxies (12%, 95% CI 7%– 20%) was acknowledgment that critically ill patients may die, and the second most common theme cited by 12 proxies (10%, 95% CI 5% - 17%) related to page 15 (Table 4).
When compared to the 68 proxies who did not find the booklet upsetting, proxies who found the booklet upsetting were not statistically or substantially different in age, sex, education level, race, relation to the patient, ICU day at time of the interview, perceived decision-making authority, or prior experience in ICUs (absolute value of all effect sizes ≤0.38) (Table 5). The patients whose proxies who found the booklet upsetting were of similar age, lived in zip codes with similar median incomes, and experienced similar rates of hospital mortality (absolute value of all effect sizes ≤0.32). Results were qualitatively similar in the sensitivity analysis (Table C of S1 File).
Table 5. Participant characteristics by response to the statement: "Parts of the booklet are upsetting".
| Strongly Agree or Agree | Strongly Disagree, Disagree, Neither | P-valuea | Absolute effect sizea | |
|---|---|---|---|---|
| Proxy and interview characteristics | (N = 54) | (N = 68) | ||
| Age, median (IQR)b | 47 (34, 60) | 54 (46, 63) | 0.04 | 0.38 |
| Female, n (%)b | 37 (70%) | 46 (69%) | 1.00 | 0.03 |
| Years of education, median (IQR) | 14 (12, 16) | 14 (12, 16) | 0.20 | 0.10 |
| Self-identified race, n (%)b | ||||
| Black or African American | 22 (41%) | 33 (49%) | 0.50 | 0.29 |
| White | 26 (48%) | 29 (43%) | ||
| Other | 2 (4%) | 6 (9%) | ||
| Relation to Patient, n (%)c | ||||
| Spouse/Partner | 21 (39%) | 25 (37%) | 0.55 | 0.06 |
| Adult child | 17 (32%) | 23 (34%) | ||
| Parent | 6 (11%) | 8 (12%) | ||
| Other | 10 (19%) | 12 (18%) | ||
| ICU day at time of interview, median (IQR) | 2 (1, 3) | 2 (1, 3) | 0.79 | 0.04 |
| "Do you have legal authority to speak for [patient's name] if he/she is unable to make decisions about medical treatment?" This question was asked BEFORE the proxy viewed the booklet. | ||||
| Yes | 33 (61%) | 48 (71%) | 0.36 | 0.21 |
| "Have you ever supported a loved one in an ICU before?", n (%)b | ||||
| Yes | 33 (61%) | 42 (62%) | 0.89 | 0.06 |
| Patients characteristics & Outcomesd | ||||
| Age, median (IQR) | 58 (45, 69) | 58 (50, 70) | 0.41 | 0.14 |
| Female, n (%) | 25 (46%) | 35 (51%) | 0.70 | 0.10 |
| Income of zip code in $1000s of USD, median (IQR)e | 58.6 (36.0, 74.1) | 59.1 (36.0, 82.0) | 0.90 | 0.03 |
| Is the patient "full code" during the interview?f | ||||
| Yes | 43 (80%) | 60 (88%) | 0.29 | 0.32 |
| Location prior to hospitalization, n (%)b | ||||
| House/Apartment (independent) | 39 (72%) | 42 (62%) | 0.32 | 0.32 |
| House/Apartment (with assistance) | 13 (24%) | 18 (26%) | ||
| Other | 2 (4%) | 7 (10%) | ||
| Admission diagnosis, n (%) | ||||
| Respiratory failure | 27 (50%) | 29 (43%) | 0.28 | 0.35 |
| Sepsis | 10 (19%) | 14 (21%) | ||
| Gastrointestinal | 7 (13%) | 4 (6%) | ||
| Other | 10 (19%) | 21 (31%) | ||
| In-hospital death, n (%) | 15 (28%) | 19 (28%) | 1.00 | 0.00 |
Abbreviation: ICU, Intensive care unit; IQR, Interquartile Range; USD, United States Dollar
a Absolute effect size = absolute value of difference in means or proportions divided by standard error. P-values obtained from the Wilcoxon-Mann-Whitney two-sample test for continuous values, and the Chi-square test for categorical values with Fisher’s exact test for cell-sizes <10.
b Proxies declined to report age (n = 2), sex (n = 2), race (n = 4), and prior experience as an ICU proxy (n = 3). Location prior to hospitalization missing for 1 patient.
c Percentages do not sum to 100% due to rounding.
d 2 proxies were interviewed for 11 patients, creating 11 pairs of proxies independently answering questions about the same patient at different times during the ICU stay. In 4 dyads, the proxies gave discordant responses about whether the booklet was upsetting.
e US Census Bureau 2010–2014; $41,819 median household income for Baltimore City; $74,194 median household income for MD state. No zip code was provided for 1 international patient.
f 54 (53%) of patients who are herein designated as full code didn’t have any documented code status during the interview.
There were 97 proxies enrolled after the third week of the study who agreed or strongly agreed that the study information was important. Asked when and how the information in the intervention should be conveyed, 57 (59%, 95% CI 48% - 69%) said as soon as the proxy arrived in the ICU, 33 (34%, 95% CI 25% - 44%) said after the proxy spoke to a doctor about their loved ones care, and 6 (6%, 95% CI 3% - 14%) said only if their loved ones health was not improving. When asked about how to provide the information, 54 (56%, 95% CI 45% - 66%) wanted to have a face-to-face conversation, 32 (33%, 95% CI 24% - 43%) wanted to receive a paper version of the booklet and 9 (9%, 95% CI 5% - 17%) preferred viewing a video.
Discussion
In this Phase I study of an intervention to educate ICU families about the role of a healthcare proxy and prepare them to communicate effectively with clinicians, 98% of proxies rated the intervention as both appropriate and important, and 44% also found the intervention upsetting. Proxies considered recommended questions for intensivists the most important information within the intervention. Demographics of proxies and patients were similar comparing proxies who did versus did not find the intervention upsetting.
Providing ICU families with an informational leaflet is endorsed by the Agency for Healthcare Research and Quality as a process measure of high quality palliative care in the ICU [43]. Previous leaflets designed for use in the ICU [29,44–47] have largely targeted the families of dying patients, and provided information about the clinical environment such as commonly used medical jargon, procedures, ICU rules, and explanations of the equipment in a patient’s room. Our intervention was markedly different from previous leaflets in four important ways. First, our intervention was designed to be appropriate for all adult family members of ICU patients regardless of survival prognosis. Second, the booklet in our intervention functioned not as information that a family could choose to access, but as a script that was read aloud and verbatim to each participant. Reading aloud demonstrates that saying the words “death” and “dying” is acceptable in the ICU setting and ensures that all participants receive the same intervention regardless of available time, interest, or health literacy. Third, the intervention directly addressed that not all ICU patients survive or recover sufficiently to live at home, thereby helping to set appropriate expectations. Finally, our intervention made no attempt to explain a patient’s diagnosis, clinical care, prognosis, or treatment options; rather, we focused on how proxies should attempt to obtain this information from ICU clinicians.
Providing families with information is not sufficient to ensure engagement or shared decision-making [48]. Those who choose to be proxies must see themselves as active participants, bestowed with the authority to convey information about the patient’s goals and values, as well as a responsibility to obtain information about prognosis and treatment options. This challenge requires redefining the family member’s role, similar to patient activation in the outpatient setting [49,50]. We addressed this challenge by describing ICU proxies as people who volunteer for a responsibility that is respected, psychologically taxing, and vitally important.
The high prevalence of proxies rating the intervention as upsetting and the inability to anticipate which proxies will be upset means that the intervention booklet should not be left in waiting rooms. Although 56% of proxies said they wanted to receive information via a face-to-face conversation, we believe this rate would have been even higher if proxies had been permitted to select multiple responses to this question since many proxies said they preferred to have both a face-to-face conversation and receive written material that could be shared with other family members. As one proxy explained: “It’s really important to talk to someone. I would have thrown this away if it had just been handed to me on admission.”
This Phase I study had potential limitations. It was conducted in a single ICU and excluded families who did not physically visit the ICU or did not speak English. Similar interventions will need to be tailored to their jurisdiction given that statutes about who can serve as a proxy for patients who lack decisional capacity vary widely across states.[51] The study also only addressed proxy’s immediate reactions to the intervention which may have changed over time, particularly after discharge. Further study is needed to determine whether describing parts of the booklet as “upsetting” immediately following the intervention correlates with any long-term mental health symptoms.[52,53] As a Phase I study there was no attempt to estimate the intervention’s impact on proxy behavior or patient care. Despite these limitations, the study has important strengths including being designed to ensure all participants received the same exposure to the intervention, being conducted in a socio-economically diverse population, and being developed with input from ICU proxies and a large multi-disciplinary group of relevant stakeholders.
Many questions remain to be answered about this intervention. The most pressing question is whether it impacts proxy behavior and communication. Additional research is needed to determine if the intervention improves proxy activation. There are also logistical questions, namely who should deliver the intervention, as well as issues of cost-effectiveness. If the intervention positively impacts proxy behavior and is cost-neutral, it will face the same challenges which limit the use of interventions designed to foster patient/family engagement and shared decision-making, namely, resistance to change and the lack of reward for clinical utilization [54].
Conclusions
This Phase I, single-center study of a brief intervention designed to set expectations, explain an ICU proxy’s role in the ICU setting, and prepare proxies to communicate effectively with clinicians was acceptable and important to nearly all 122 participating ICU proxies. Frequently, the intervention was simultaneously rated as upsetting by these same proxies, with neither patient nor proxy characteristics associated with this finding. This intervention represents the early stages of an attempt to adapt the principles of patient activation to the ICU setting. Additional research is required to determine if this approach impacts proxy behavior.
Supporting information
(PDF)
Acknowledgments
The authors wish to thank the Johns Hopkins Hospital Patient and Family Advisory Council, Jeanne-Marie LaFrance and Amy Durocher of the Johns Hopkins MICU social work team, the MICU nurse practitioners and physician assistants, Jeffrey Natterman of the Johns Hopkins Health System risk management and patient care, Jane Hill and Markia Dallas from Johns Hopkins Hospital Patient Relations, Matt Norvell and John Ponnala from Johns Hopkins Chaplaincy & Spiritual care, and the Johns Hopkins MICU end-of-life interest group. All booklet illustrations were created by Susie Hancock and Khoon Lay Gan. An To and Mohammad Shaear assisted with data collection. Anahita Rabiee, Mohamed Hashem, and Victor Dinglas assisted with data management.
Data Availability
De-identified data files are available from the Johns Hopkins University Data Archive Dataverse, Turnbull, Alison E., DVM, MPH, PhD; Mohamed D. Hashem, MD; Anahita Rabiee, MD; An To, MS; Caroline M. Chessare, MS; Mohammad Shaear, MD; Rachel Coffin, BSN; Dale M. Needham, FCPA, MD, PhD, 2017, "Data associated with the PLoS ONE publication 'A Brief Intervention for Preparing ICU Families to be Proxies: A Phase I Study' by Turnbull et al. 2017", doi:10.7281/T1/ZHG9BB.
Funding Statement
This research was supported by the Johns Hopkins School of Medicine, Division of Pulmonary and Critical Care Medicine. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Teno JM G P. Change in end-of-life care for medicare beneficiaries: Site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309: 470–477. doi: 10.1001/jama.2012.207624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Teno JM, Gozalo P, Khandelwal N, Curtis JR, Meltzer D, Engelberg R, et al. Association of Increasing Use of Mechanical Ventilation Among Nursing Home Residents With Advanced Dementia and Intensive Care Unit Beds. JAMA Intern Med. 2016;176: 1809–1816. doi: 10.1001/jamainternmed.2016.5964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luce JM. A national survey of end-of-life care for critically ill patients. Am J Respir Crit Care Med. 1998;158: 1163–1167. doi: 10.1164/ajrccm.158.4.9801108 [DOI] [PubMed] [Google Scholar]
- 4.Torke AM, Sachs GA, Helft PR, Montz K, Hui SL, Slaven JE, et al. Scope and outcomes of surrogate decision making among hospitalized older adults. JAMA Intern Med. 2014;174: 370–377. doi: 10.1001/jamainternmed.2013.13315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abbott KH, Sago JG, Breen CM, Abernethy AP, Tulsky JA. Families looking back: one year after discussion of withdrawal or withholding of life-sustaining support. Crit Care Med. 2001;29: 197–201. [DOI] [PubMed] [Google Scholar]
- 6.Schuster RA, Hong SY, Arnold RM, White DB. Investigating conflict in ICUs-is the clinicians’ perspective enough? Crit Care Med. 2014;42: 328–335. doi: 10.1097/CCM.0b013e3182a27598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.LeClaire MM, Oakes JM, Weinert CR. Communication of prognostic information for critically ill patients. Chest. 2005;128: 1728–1735. doi: 10.1378/chest.128.3.1728 [DOI] [PubMed] [Google Scholar]
- 8.Lee Char SJ, Evans LR, Malvar GL, White DB. A randomized trial of two methods to disclose prognosis to surrogate decision makers in intensive care units. Am J Respir Crit Care Med. 2010;182: 905–909. doi: 10.1164/rccm.201002-0262OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiarchiaro J, Buddadhumaruk P, Arnold RM, White DB. Quality of Communication in the ICU and Surrogate’s Understanding of Prognosis*: Crit Care Med. 2015;43: 542–548. doi: 10.1097/CCM.0000000000000719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alonso W, Hupcey JE, Kitko L. Caregivers’ perceptions of illness severity and end of life service utilization in advanced heart failure. Heart Lung J Acute Crit Care. 2017;46: 35–39. doi: 10.1016/j.hrtlng.2016.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wendler D, Rid A. Systematic Review: The Effect on Surrogates of Making Treatment Decisions for Others. Ann Intern Med. 2011;154: 336–346. doi: 10.7326/0003-4819-154-5-201103010-00008 [DOI] [PubMed] [Google Scholar]
- 12.Schenker Y, Crowley-Matoka M, Dohan D, Tiver GA, Arnold RM, White DB. I don’t want to be the one saying “we should just let him die”: intrapersonal tensions experienced by surrogate decision makers in the ICU. J Gen Intern Med. 2012;27: 1657–1665. doi: 10.1007/s11606-012-2129-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chiarchiaro J, Buddadhumaruk P, Arnold RM, White DB. Prior Advance Care Planning Is Associated with Less Decisional Conflict among Surrogates for Critically Ill Patients. Ann Am Thorac Soc. 2015;12: 1528–1533. doi: 10.1513/AnnalsATS.201504-253OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Beusekom I, Bakhshi-Raiez F, de Keizer NF, Dongelmans DA, van der Schaaf M. Reported burden on informal caregivers of ICU survivors: a literature review. Crit Care. 2016;20: 16 doi: 10.1186/s13054-016-1185-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cameron JI, Chu LM, Matte A, Tomlinson G, Chan L, Thomas C, et al. One-Year Outcomes in Caregivers of Critically Ill Patients. N Engl J Med. 2016;374: 1831–1841. doi: 10.1056/NEJMoa1511160 [DOI] [PubMed] [Google Scholar]
- 16.Jones C, Skirrow P, Griffiths RD, Humphris G, Ingleby S, Eddleston J, et al. Post-traumatic stress disorder-related symptoms in relatives of patients following intensive care. Intensive Care Med. 2004;30: 456–460. doi: 10.1007/s00134-003-2149-5 [DOI] [PubMed] [Google Scholar]
- 17.Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171: 987–994. doi: 10.1164/rccm.200409-1295OC [DOI] [PubMed] [Google Scholar]
- 18.Anderson WG, Arnold RM, Angus DC, Bryce CL. Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. J Gen Intern Med. 2008;23: 1871–1876. doi: 10.1007/s11606-008-0770-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McAdam JL, Fontaine DK, White DB, Dracup KA, Puntillo KA. Psychological symptoms of family members of high-risk intensive care unit patients. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses. 2012;21: 386–393; quiz 394. doi: 10.4037/ajcc2012582 [DOI] [PubMed] [Google Scholar]
- 20.Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, et al. Guidelines for Family-Centered Care in the Neonatal, Pediatric, and Adult ICU. Crit Care Med. 2017;45: 103–128. doi: 10.1097/CCM.0000000000002169 [DOI] [PubMed] [Google Scholar]
- 21.Kon AA, Davidson JE, Morrison W, Danis M, White DB. Shared Decision Making in ICUs: An American College of Critical Care Medicine and American Thoracic Society Policy Statement. Crit Care Med. 2015;44: 188–201. doi: 10.1097/CCM.0000000000001396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.You JJ, Downar J, Fowler RA, Lamontagne F, Ma IWY, Jayaraman D, et al. Barriers to Goals of Care Discussions With Seriously Ill Hospitalized Patients and Their Families: A Multicenter Survey of Clinicians. JAMA Intern Med. 2015;175: 549–556. doi: 10.1001/jamainternmed.2014.7732 [DOI] [PubMed] [Google Scholar]
- 23.Hillman KM, Cardona-Morrell M. The ten barriers to appropriate management of patients at the end of their life. Intensive Care Med. 2015;41: 1700–1702. doi: 10.1007/s00134-015-3712-6 [DOI] [PubMed] [Google Scholar]
- 24.Turnbull AE, Davis WE, Needham DM, White DB, Eakin MN. Intensivist-reported Facilitators and Barriers to Discussing Post-Discharge Outcomes with Intensive Care Unit Surrogates: A Qualitative Study. Ann Am Thorac Soc. 2016;13: 1546–1552. http://dx.doi.org/10.1513/AnnalsATS.201603-212OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wysham NG, Hua M, Hough CL, Gundel S, Docherty SL, Jones DM, et al. Improving ICU-Based Palliative Care Delivery: A Multicenter, Multidisciplinary Survey of Critical Care Clinician Attitudes and Beliefs. Crit Care Med. 2016; doi: 10.1097/CCM.0000000000002099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Richman PS, Saft HL, Messina CR, Berman AR, Selecky PA, Mularski RA, et al. Palliative and end-of-life educational practices in US pulmonary and critical care training programs. J Crit Care. 2016;31: 172–177. doi: 10.1016/j.jcrc.2015.09.029 [DOI] [PubMed] [Google Scholar]
- 27.Sullivan AM, Rock LK, Gadmer NM, Norwich DE, Schwartzstein RM. The Impact of Resident Training on Communication with Families in the ICU: Resident and Family Outcomes. Ann Am Thorac Soc. 2016; doi: 10.1513/AnnalsATS.201508-495OC [DOI] [PubMed] [Google Scholar]
- 28.Schwarze ML, Campbell TC, Cunningham TV, White DB, Arnold RM. You Can’t Get What You Want: Innovation for End-Of-Life Communication in the ICU. Am J Respir Crit Care Med. 2016;193: 14–16. doi: 10.1164/rccm.201508-1592OE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Penrod JD, Luhrs CA, Livote EE, Cortez TB, Kwak J. Implementation and evaluation of a network-based pilot program to improve palliative care in the intensive care unit. J Pain Symptom Manage. 2011;42: 668–671. doi: 10.1016/j.jpainsymman.2011.06.012 [DOI] [PubMed] [Google Scholar]
- 30.Kohn R, Madden V, Kahn JM, Asch DA, Barnato AE, Halpern SD, et al. Diffusion of Evidence-based Intensive Care Unit Organizational Practices. A State-Wide Analysis. Ann Am Thorac Soc. 2017;14: 254–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nelson JE, Mulkerin CM, Adams LL, Pronovost PJ. Improving comfort and communication in the ICU: a practical new tool for palliative care performance measurement and feedback. Qual Saf Health Care. 2006;15: 264–271. doi: 10.1136/qshc.2005.017707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): Conceptualizing and Measuring Activation in Patients and Consumers. Health Serv Res. 2004;39: 1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff Proj Hope. 2013;32: 207–214. doi: 10.1377/hlthaff.2012.1061 [DOI] [PubMed] [Google Scholar]
- 34.DeKeyser Ganz F, Engelberg R, Torres N, Curtis JR. Development of a Model of Interprofessional Shared Clinical Decision Making in the ICU: A Mixed-Methods Study. Crit Care Med. 2015; [DOI] [PubMed] [Google Scholar]
- 35.Isotype: Design and Contexts 1925–1971 by Christopher Burke. Hyphen Press; 2013. [Google Scholar]
- 36.FAQClinicalTrials.gov—Clinical Trial Phases [Internet]. [cited 26 Jan 2017]. https://www.nlm.nih.gov/services/ctphases.html
- 37.Turnbull AE, Hashem MD, Rabiee A, To A, Chessare CM, Needham DM. Evaluation of a strategy for enrolling the families of critically ill patients in research using limited human resources. PLOS ONE. 2017;12: e0177741 doi: 10.1371/journal.pone.0177741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schwartz AAGJS. Who Can Make Health Care Decisions For Another? Defining Health Care Proxies Under Maryland Law [Internet]. 2006. http://www.marylandattorneygeneral.gov/Health%20Policy%20Documents/proxies_definition.pdf
- 39.Frosh, Attorney General Brian E. Summary Of Maryland Health Care Decisions Act [Internet]. 2014. http://www.marylandattorneygeneral.gov/Health%20Policy%20Documents/HCDAsummary.pdf
- 40.Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13: 117 doi: 10.1186/1471-2288-13-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sullivan GM, Feinn R. Using Effect Size—or Why the P Value Is Not Enough. J Grad Med Educ. 2012;4: 279–282. doi: 10.4300/JGME-D-12-00156.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chavalarias D, Wallach J, Li A, Ioannidis JA. Evolution of reporting p values in the biomedical literature, 1990–2015. JAMA. 2016;315: 1141–1148. doi: 10.1001/jama.2016.1952 [DOI] [PubMed] [Google Scholar]
- 43.Penrod JD, Pronovost PJ, Livote EE, Puntillo KA, Walker AS, Wallenstein S, et al. Meeting standards of high-quality intensive care unit palliative care: clinical performance and predictors. Crit Care Med. 2012;40: 1105–1112. doi: 10.1097/CCM.0b013e3182374a50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Daly K, Kleinpell RM, Lawinger S, Casey G. The effect of two nursing interventions on families of ICU patients. Clin Nurs Res. 1994;3: 414–422. doi: 10.1177/105477389400300409 [DOI] [PubMed] [Google Scholar]
- 45.Azoulay E, Pochard F, Chevret S, Jourdain M, Bornstain C, Wernet A, et al. Impact of a family information leaflet on effectiveness of information provided to family members of intensive care unit patients: a multicenter, prospective, randomized, controlled trial. Am J Respir Crit Care Med. 2002;165: 438–442. doi: 10.1164/ajrccm.165.4.200108-006oc [DOI] [PubMed] [Google Scholar]
- 46.Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007;356: 469–478. doi: 10.1056/NEJMoa063446 [DOI] [PubMed] [Google Scholar]
- 47.Mistraletti G, Umbrello M, Mantovani ES, Moroni B, Formenti P, Spanu P, et al. A family information brochure and dedicated website to improve the ICU experience for patients’ relatives: an Italian multicenter before-and-after study. Intensive Care Med. 2016; 1–11. doi: 10.1007/s00134-016-4592-0 [DOI] [PubMed] [Google Scholar]
- 48.Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns. 2014;94: 291–309. doi: 10.1016/j.pec.2013.10.031 [DOI] [PubMed] [Google Scholar]
- 49.Joseph-Williams N, Edwards A, Elwyn G. Power imbalance prevents shared decision making. BMJ. 2014;348: g3178–g3178. doi: 10.1136/bmj.g3178 [DOI] [PubMed] [Google Scholar]
- 50.Hibbard JH, Gilburt H. Supporting people to manage their health: An introduction to patient activation. London: The King’s Fund; 2014. [Google Scholar]
- 51.DeMartino ES, Dudzinski DM, Doyle CK, Sperry BP, Gregory SE, Siegler M, et al. Who Decides When a Patient Can’t? Statutes on Alternate Decision Makers. N Engl J Med. 2017;376: 1478–1482. doi: 10.1056/NEJMms1611497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carson SS, Cox CE, Wallenstein S, et al. Effect of palliative care–led meetings for families of patients with chronic critical illness: A randomized clinical trial. JAMA. 2016;316: 51–62. doi: 10.1001/jama.2016.8474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kentish-Barnes N, Chevret S, Champigneulle B, Thirion M, Souppart V, Gilbert M, et al. Effect of a condolence letter on grief symptoms among relatives of patients who died in the ICU: a randomized clinical trial. Intensive Care Med. 2017; 1–12. doi: 10.1007/s00134-016-4523-0 [DOI] [PubMed] [Google Scholar]
- 54.Elwyn G, Scholl I, Tietbohl C, Mann M, Edwards AG, Clay C, et al. “Many miles to go …”: a systematic review of the implementation of patient decision support interventions into routine clinical practice. BMC Med Inform Decis Mak. 2013;13: S14 doi: 10.1186/1472-6947-13-S2-S14 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
De-identified data files are available from the Johns Hopkins University Data Archive Dataverse, Turnbull, Alison E., DVM, MPH, PhD; Mohamed D. Hashem, MD; Anahita Rabiee, MD; An To, MS; Caroline M. Chessare, MS; Mohammad Shaear, MD; Rachel Coffin, BSN; Dale M. Needham, FCPA, MD, PhD, 2017, "Data associated with the PLoS ONE publication 'A Brief Intervention for Preparing ICU Families to be Proxies: A Phase I Study' by Turnbull et al. 2017", doi:10.7281/T1/ZHG9BB.