Abstract
Background
One of the most common cancers in head and neck is nasopharynx. Knowledge about the incidence and mortality of this disease and its distribution in terms of geographical areas is necessary for further study, better planning and prevention. Therefore, this study aimed to determine the incidence and mortality of nasopharynx cancer and its relationship with human development index (HDI) in the world in 2012.
Methods
This study was an ecological study conducted based on GLOBOCAN project of World Health Organization (WHO) for the countries in world. The correlation between standardized incidence rates (SIRs) and standardized mortality rates (SMRs) of nasopharynx cancer with HDI and its components was assessed with correlation coefficient by using SPSS 15.
Results
In 2012, 86,691 nasopharynx cancer cases occurred in the world, so that 60,896 new cases were seen in men and 25,795 new cases in women (sex ratio = 2.36). SIR of the cancer was 1.2 per 100,000 (1.7 in men and 0.7 in women per 100,000) in the world. In 2012, 50,831 nasopharynx death cases occurred in the world, so that 35,756 death cases were seen in men and 15,075 death cases in women (sex ratio = 2.37). SIR of mortality from the cancer was 0.7 per 100,000 (0.7 in women and 1 in men per 100,000) in the world. The results of correlation analysis showed a negative correlation between the SIR and HDI (r = -0.037, P = 0.629), and also the results of correlation analysis showed a negative correlation between the SMR and HDI (r = -0.237, P = 0.002).
Conclusion
Nasopharyngeal cancer is native to Southeast Asia and the highest incidence and mortality were seen in countries with moderate and low HDI. It is suggested that studies are conducted on determining the causes of the cancer incidence and mortality in the world and the differences between various regions.
Keywords: Incidence, Mortality, Nasopharynx cancer, Human development index, World
Introduction
Cancer is a major cause of morbidity and mortality in all communities [1]. Head and neck malignancies are relatively common cancers in human and involve the various anatomical parts of the head and neck [2]. One of the most common cancers in head and neck is nasopharyngeal cancer [3, 4], which is associated with a very unique geographical distribution pattern. It is reported that there are about 86,500 cases of nasopharynx cancer and 50,000 deaths from the disease worldwide [5]. The cancer is malignant and its incidence is affected by geographical and racial variations from the epidemiological perspective. In most parts of the world, the age-standardized incidence rate (ASIR) of nasopharynx cancer, regardless of gender, was reported about less than 1 per 100,000 person-years [6-8]. The southern part of China, parts of Southeast Asia, North and South Africa and Alaska have the highest incidence rate. In Europe, ASIR is generally less than two cases per 100,000 in 1 year among men and less than one case per 100,000 among women [9]. In contrast, in China, Southeast Asia and the Arctic region [7], as well as in immigrants from those regions [10], an incidence of 30 cases per 100,000 in men and 10 cases per 100,000 in female subjects were observed [9]. The cancer has an uneven geographical distribution: 81% of new cases in Asia and 9% in Africa. According to the burden of disease, Southeast Asian countries include 67% of the global burden of cancer [11]. Nasopharyngeal cancer is mainly related to the use of tobacco and alcohol [12] and other known risk factors, such as human papilloma virus (HPV) [13], infection with Epstein-Barr virus (EBV) [7] and low intake of fruits and vegetables [14]. There is an increased risk of nasopharyngeal cancer and some other cancers in first-degree relatives because of genetic and environmental risk factors [15]. Nasopharyngeal cancer is diagnosed in advanced stages, but associated with very poor prognosis. However, the cancer is potentially curable in early stages. Therefore, early detection screening may lead to improved outcomes [16]. A lack of knowledge of general practitioners working in health centers in Asian countries about the various aspects of nasopharyngeal cancer may lead to delay in diagnosis [17]. Due to the sensitive nature of the cancer, chemotherapy and radiation therapy are major treatments of this cancer [18-21]. However, about 10-15% of recurrences occur in patients with metastasis in distant organs when chemotherapy and radiation therapy are operated [22, 23].
One of the reasons for differences in cancer incidence and mortality in different regions is socio-economic status (SES), education level and life expectancy that are highlighted by the human development index (HDI). HDI classification is useful to compare the incidence and mortality of cancer on a global level [23] and is one of the indicators which evaluate the status of illnesses and deaths between countries [24]. In fact, this index is associated with the incidence and mortality of many diseases and is an appropriate indicator for awareness of the status of countries in terms of a specific disease [25-27]. The relationship between HDI and some types of cancer is studied and investigation on this relationship can lead to a more accurate understanding of cancer distribution and its risk factors [28]. Knowing nasopharynx cancer incidence and mortality can be useful for health programs and research activities and considering the possible role of the HDI, this study aimed to determine the incidence and mortality of nasopharyngeal carcinoma and its relationship with HDI and its components in the world in 2012.
Materials and Methods
This study was an ecologic study in the world for assessing the correlation between age-specific incidence and mortality rate (ASR) with HDI and its details, including life expectancy at birth, mean years of schooling, and gross national income (GNI) per capita. Data were about the ASR for all country in 2012 obtained from the global cancer project; available at http://globocan.iarc.fr/Default.aspx [29] and HDI from Human Development Report 2013 [30], that includes information about HDI and its details for every country in the world in 2012.
Method for estimating the ASRs in global cancer project by international agency for research on cancer
Age-specific incidence rate estimate
The methods of estimation are country specific, and the quality of the estimation depends upon the quality and on the amount of the information available for each country. In theory, there are as many methods as countries, and because of the variety and the complexity of these methods, an overall quality score for the incidence and mortality estimates combined is almost impossible to establish. However, an alphanumeric scoring system which independently describes the availability of incidence and mortality data has been established at the country level. The combined score is presented together with the estimates for each country with an aim of providing a broad indication of the robustness of the estimation.
The methods to estimate the sex- and age-specific incidence rates of cancer for a specific country fall into one of the following broad categories, in priority order: 1) rates projected to 2012 (38 countries); 2) most recent rates applied to 2012 population (20 countries); 3) estimated from national mortality by modeling, using incidence mortality ratios derived from recorded data in country-specific cancer registries (13 countries); 4) estimated from national mortality estimates by modeling, using incidence mortality ratios derived from recorded data in local cancer registries in neighboring countries (nine European countries); 5) estimated from national mortality estimates using modeled survival (32 countries); 6) estimated as the weighted average of the local rates (16 countries); 7) one cancer registry covering a part of a country is used as representative of the country profile (11 countries); 8) age-/sex-specific rates for “all cancers” were partitioned using data on relative frequency of different cancers (by age and sex) (12 countries); 9) the rates are those of neighboring countries or registries in the same area (33 countries) [29].
Age-specific mortality rate estimate
Depending on the degree of detail and accuracy of the national mortality data, six methods have been utilized in the following order of priority: 1) rates projected to 2012 (69 countries); 2) most recent rates applied to 2012 population (26 countries); 3) estimated as the weighted average of regional rates (one country); 4) estimated from national incidence estimates by modeling, using country-specific survival (two countries); 5) estimated from national incidence estimates using modeled survival (83 countries); 6) the rates are those of neighboring countries or registries in the same area (three countries) [31].
HDI
HDI is a composite measure of indicators along three components, including life expectancy, educational attainment, and command over the resources needed for a decent living. All groups and regions have seen notable improvement in all HDI components, with faster progress in low and medium HDI countries. On this basis, the world is becoming less unequal. Nevertheless, national averages hide large variations in human experience. Wide disparities remain within countries of both the North and the South, and income inequality within and between many countries has been rising. According to HDI, countries in the world are divided into four categories as follows: countries with very high HDI (HDI ≥ 0.80), countries with a high HDI (0.80 > HDI > 0.710), medium HDI countries (0.710 ≥ HD ≥ 0.535), and countries with a low HDI (HDI < 0.535) [30].
Statistical analysis
In this study, we used correlation bivariate method for assessment of the correlation between ASR with HDI and its details, which include life expectancy at birth, mean years of schooling, and GNI per capita. Statistical significance was assumed if P < 0.05. All reported P-values are two-sided. Statistical analyses were performed using SPSS (version 15.0, SPSS Inc.).
Results
Nasopharynx cancer cases
In 2012, 86,691 nasopharynx cancer cases occurred in the world, so that 60,896 new cases were seen in men and 25,795 new cases in women (sex ratio = 2.36). Of all cases, 8,863 cases occurred in countries with very high HDI, 8,053 cases in countries with high HDI, 61,229 cases in countries with moderate HDI, and 8,535 cases in countries with low HDI. The highest number of cancer cases was seen in five countries such as China with about 33,198 cases, Indonesia 13,084, Vietnam about 4,931, India 3,947 and Malaysia with about 2,030 cases, respectively. Five countries that had the largest number of nasopharynx cancer in men were China about 23,581, Indonesia about 9,355, Vietnam 3,301, India 2,956 and Malaysia 1,487 cases, respectively. The highest number in women was seen in five countries including China 9,617, Indonesia 3,729 cases, Vietnam 1,630, India 991 cases and the United States about 599 cases, respectively.
ASIR
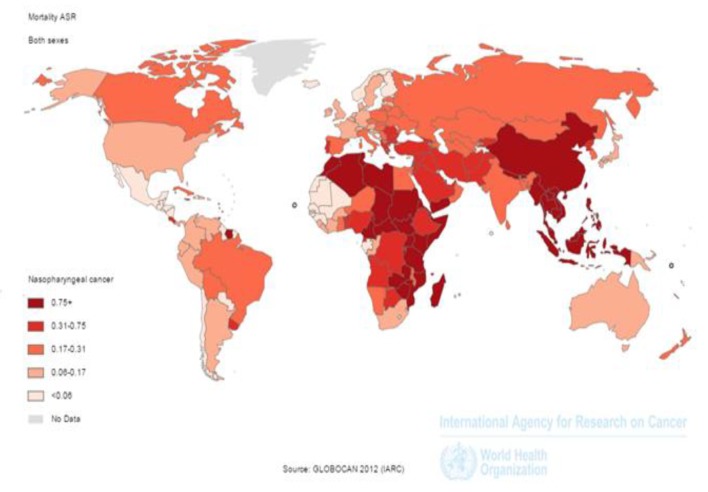
SIR of the cancer was 1.2 per 100,000 (1.7 in men and 0.7 in women per 100,000) in the world. The incidence rate in countries with very high HDI was 0.6 per 100,000, in countries with a high HDI 0.7 per 100,000, in countries with medium HDI 1.7 per 100,000, and in countries with a low HDI 1 per 100,000. Five countries that had the highest ASIR were Malaysia 7.2 per 100,000, Singapore 6.4 per 100,000, Indonesia 5.6 per 100,000, Vietnam 5.4 per 100,000 and Brunei 5 per 100,000, respectively. Five countries with the highest ASIR for men included Malaysia 10.6 per 100,000, Singapore 9.7 per 100,000, Indonesia 8.3 per 100,000, Vietnam 7.7 per 100,000 and Brunei 7.6 per 100,000, respectively. Five countries also had the highest ASIR for women were Malaysia 9.3 per 100,000, Vietnam 9.3 per 100,000, Singapore 3.2 per 100,000, Indonesia 3 per 100,000 and Kenya 2 per 100,000, respectively (Fig. 1).
Figure 1.
Distribution of standardized nasopharynx cancer incidence rate in the world (extracted from GLOBOCAN, 2012).
The number of deaths from cancer
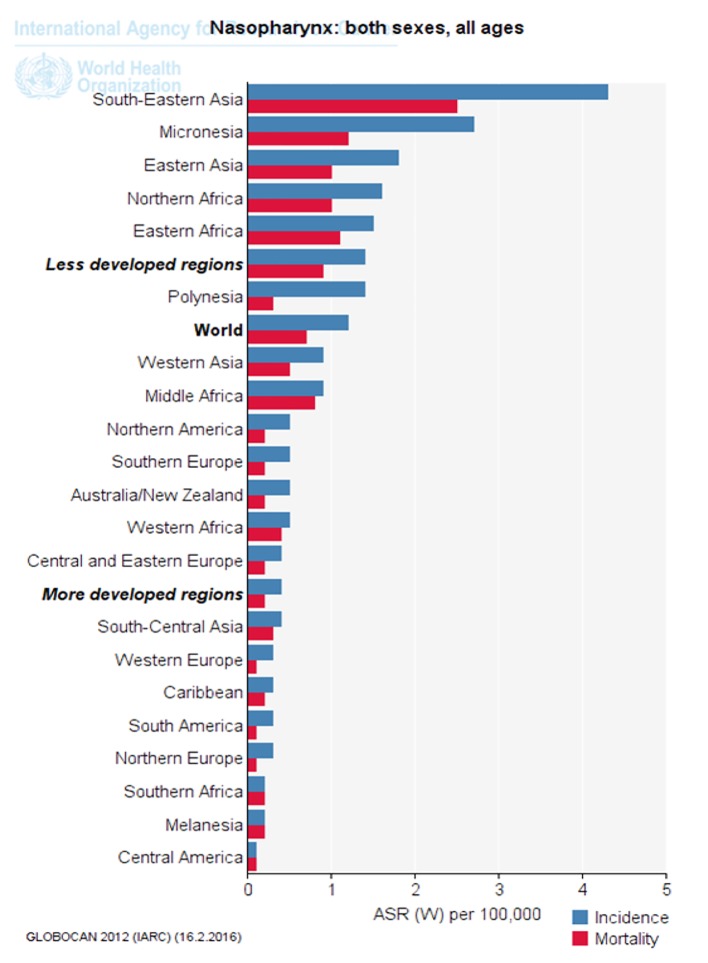
In 2012, 50,831 nasopharynx death cases occurred in the world, so that 35,756 death cases were seen in men and 15,075 death cases in women (sex ratio = 2.37). Of all cases, 3,948 death cases occurred in countries with very high HDI, 3,852 cases in countries with high HDI, 36,923 cases in countries with moderate HDI and 6,105 cases in countries with low HDI. The highest number of death cases was seen in countries such as China 20,404 cases, Indonesia 7,391, Vietnam 2,885, India 2,836 and Thailand 1,114 cases, respectively (Figs. 2 and 3).
Figure 2.
Distribution of standardized nasopharynx cancer mortality rate in the world (extracted from GLOBOCAN, 2012).
Figure 3.
Standardized incidence and mortality of nasopharynx cancer in different parts of the UN (extracted from GLOBOCAN, 2012).
The age-standardized mortality rate (ASMR)
SIR of mortality from the cancer was 0.7 per 100,000 (0.7 in women and 1in men per 100,000) in the world. The SMR in countries with very high HDI was 0.2 per 100,000, in countries with a high HDI 0.3 per 100,000, in countries with medium HDI 1 per 100,000, and in countries with a low HDI 0.7 per 100,000. Five countries that had the highest ASMR were Malaysia 3.3 per 100,000, Vietnam 3.3 per 100,000, Singapore 2.8 per 100,000, Malaysia 2.5 per 100,000 and Kenya 2.1 per 100,000, respectively. Five countries with the highest ASMR for men included Indonesia 5 per 100,000, Vietnam 4.8 per 100,000, Singapore 4.4 per 100,000, Malaysia 3.9 per 100,000 and Brunei 3.4 per 100,000, respectively. Five countries also had the highest ASMR for women were Vietnam 2 per 100,000, Indonesia 1.8 per 100,000, Bhutan 1.5 per 100,000, Uganda 1.4 per 100,000 and Burundi 1.4 per 100,000, respectively (Fig. 2).
Figure 3 shows nasopharynx cancer standardized incidence and mortality in different parts of the UN. As is clear, standardized cancer incidence and mortality of nasopharynx in underdeveloped countries, Southeast Asia and Africa was more than that in developed countries (Fig. 3).
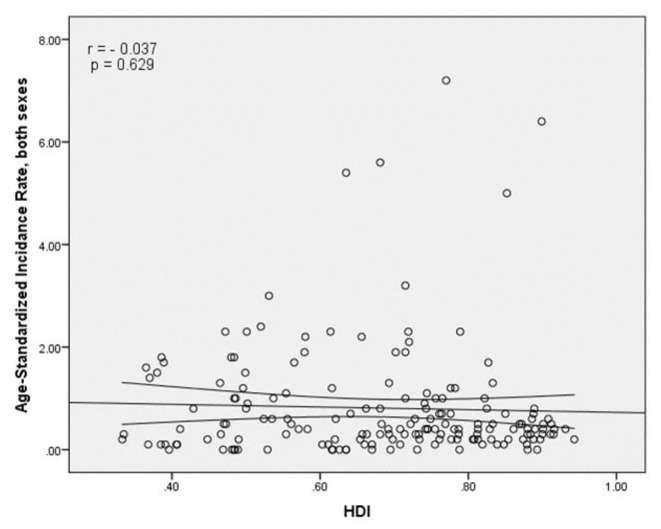
Correlation analysis between the SIR, and HDI and its components
The results of correlation analysis showed a negative correlation between the SIR and HDI (r = -0.037, P = 0.629) (Fig. 4). A positive correlation was observed between HDI components and SIR, so that there was a positive correlation between the SIR and life expectancy at birth (r = 0.011, P = 0.891), a negative correlation between the SIR and average years of schooling (r = -0.121, P = 0.118), and a positive correlation between the SIR and the level of income per person of population (r = 0.054, P = 0.483) (Table 1).
Figure 4.
The relationship between the standardized incidence rate and the human development index.
Table 1. Correlation Between ASIR, ASMR With HDI and Its Components.
| Variables | HDI | LEY | Literacy | GNP |
|---|---|---|---|---|
| ASIR | r = -0.037 P = 0.629 |
r = 0.011 P = 0.891 |
r = -0.121 P = 0.118 |
r = 0.054 P = 0.483 |
| ASMR | r = -0.237 P = 0.002 |
r = -0.171 P = 0.027 |
r = -0.298 P < 0.001 |
r = -0.11 P = 0.156 |
ASIR: age-standardized incidence rate; ASMR: age-standardized mortality rate.
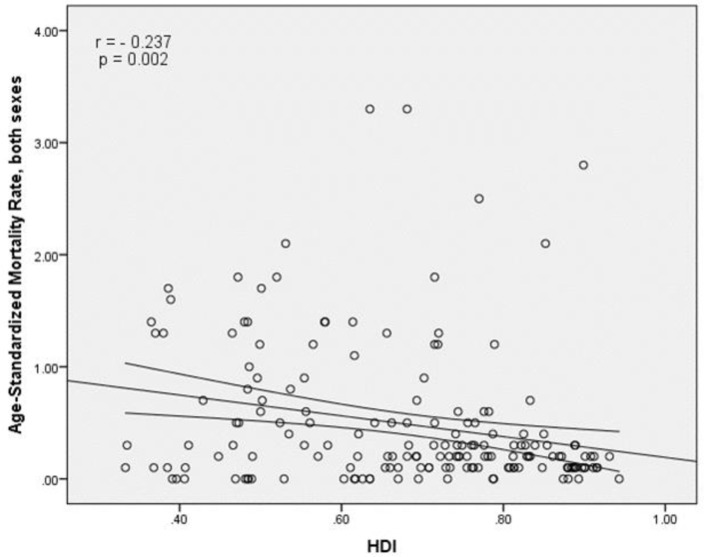
Correlation analysis between the SMR, and HDI and its components
The results of correlation analysis showed a negative correlation between the SMR and HDI (r = -0.237, P = 0.002) (Fig. 5). A negative correlation was observed between HDI components and SMR, so that there was a negative correlation between the SMR and life expectancy at birth (r = -0.171, P < 0.027), the SMR and average years of schooling (r = -0.298, P < 0.001) and the SMR and the level of income per person of population (r = -0.11, P = 0.156) (Table 1).
Figure 5.
Relationship between standardized mortality rate and the human development index.
Discussion
Overall, in 2012, 86,691 new cases and 50,831 deaths of nasopharyngeal cancer have been documented in the world with sex ratio (male to female) of nasopharyngeal cancer risk about 2.36 and sex ratio (male to female) of nasopharyngeal cancer deaths about 2.37. The highest incidence and mortality were seen in countries with medium and low HDI. Nasopharyngeal cancer prevalence in countries with medium and low HDI is greater due to higher exposure to a variety of risk factors related to the cancer and less budget allocations for health. Therefore, because of the diagnosis at an advanced stage and lack of access to treatment, metastasis of nasopharynx cancer can be observed more in these areas [32, 33].
The countries with the highest incidence of nasopharyngeal cancer had higher HDI that includes very high HDI countries of Singapore and Brunei, high HDI countries of Malaysia and countries with the moderate HDI of Indonesia and Vietnam. According to previous studies in Singapore, nasopharyngeal cancer is the eighth most common cancer in men, with ASIR of 9.5 per 100,000 per year [34]. The relatively high incidence was reported from Indonesia, at least 5.7 per 100,000 among men and 1.9 per 100,000 among women, compared with the incidence of 1.9 per 100,000 among men and 0.8 per 100,000 among women worldwide [35], while significant lowest incidence of nasopharyngeal carcinoma has been reported from parts of the United States and Europe. Nasopharyngeal cancer in Europe and North America included less than 1% of all cancer cases [9]. This peculiar geographical distribution reflects differences between pathology of nasopharyngeal carcinoma and its epidemiology in these areas [9, 36]. Regardless of ethnicity, genetics plays an important part in the pathogenesis of nasopharyngeal carcinoma. The incidence of the cancer is higher about 20 - 50 times in southern China compared with Western countries. In spite of immigration of the second and third generation Chinese to the United States (low prevalence area), in past years, they are at risk for nasopharyngeal cancer [37]. According to the causes of cancer (tobacco and alcohol), despite the declining prevalence of smoking in Europe [38], the incidence of epithelial cancers of the nasopharynx, hypopharynx and larynx cancer remains quite stable, while the oropharynx and oral cavity cancer is on the rise [39]. The results showed that wood dust severely causes to paranasal sinuses and nasal passages cancer, but its association with nasopharyngeal cancer has been weak [40]. Evidence is scattered for a link between diet and the risk of nasopharyngeal cancer, though in general a protective effect has been accessed from non-starchy vegetables, fresh fruit [41-44], vegetables and yellow/red fruits [45-48]. Although examination of the role of dietary habits in the cause of nasopharyngeal cancer, especially about features of some foods and cooking methods and food preservation, are widely surveyed in areas with higher incidence, the results also were generalized to areas with lower incidence [42, 49]. In the United States (population with low incidence), only two studies were conducted [47, 50] that mainly had focus on fruits and vegetables [51]. In our study, the countries with the highest mortality rate of nasopharyngeal cancer were medium and low HDI countries. As well as other studies have shown that one of the main causes of death in these countries is nasopharyngeal cancer which in early detection, 80% of patients are at an advanced stage [17]. Older patients diagnosed with stage 2 or stages 3 are more at higher risk of recurrence and lower overall survival [52]. However, nasopharyngeal cancer treated with radiation therapy, but the outcome varies widely around the world. Almost 80% of new cases occur in countries with poor treatment outcome. Global inequality in access and need to a plan for optimal services shows a significant relationship between survival and access to radiation therapy [11]. In the past two decades, the treatment of nasopharyngeal cancer remarkably improved through introducing chemotherapy and radiotherapy at the same time. However, the overall incidence of patients with metastatic status remains 25-34% and survival of these patients is low [53, 54]. In low- and middle-income countries, the expertise required to delivering the appropriate therapy is a major health challenge. Only there are a third of global radiation therapy centers to treat nearly 60% of cancer patients in the world, in countries with low and middle income [55].
In this study, no significant relationship was seen between the incidence of nasopharyngeal cancer and HDI, while the SMRs of nasopharyngeal cancer were correlated with the index. Also, between the SIR of nasopharyngeal cancer and one of the components of the HDI (life expectancy), there was no significant relationship, but between SMR and life expectancy, a significant relationship has been observed. In other studies, increased life expectancy leads to an increase in the global cancer burden and future changes in population growth and aging shows that new cases of nasopharyngeal cancer and mortality from it will increase in elderly people and the increase in developing countries with a low HDI is more than in developed countries with high HDI (76% vs. 25%) [56-59]. Also in this study between the SIR of the cancer and another component of the HDI (level of education or average years of schooling), there was no significant relationship, while a significant relationship was seen between the SMR and level of education or average years of schooling. According to other studies, in countries with highly educated individuals typically they have healthier habits and more appropriate behaviors when exposed to risk factors such as smoking, inappropriate diet, compared with those in countries with a poor education [60, 61]. In the United States, the risk factors with a higher prevalence of cancers associated with head and neck were as follows: single in terms of marital status, lower educational (pre high school) as well as lower income (household income less than $20,000) [62]. In some developed countries, such as Ontario and Canada, the incidence of cancers associated with head and neck similarly with lower levels of education (less than grade 8 of education) and average family income is less relevant [63]. The incidence and mortality of nasopharyngeal cancer had no significant relationship with another component of the HDI, income levels (GDP). In studies on nasopharyngeal cancer, the relationship between nasopharyngeal cancer, and socioeconomic status, lifestyle and geographical position is known. In Asian countries, an increase in the cancer can be seen more among men and women with lower economic status [64]. Also, no difference has been seen in the death of people living in rural areas with lower socio-economic compared with urban areas [65, 66]. Studies in the United States, Canada and Europe have shown that nasopharyngeal cancer is more common in deprived socio-economic population [62, 63, 67-70]. The evidence is mainly related to the risk factors associated with lower SES, such as tobacco and alcohol use and poor health so that after controlling for the risk factors, higher prevalence of nasopharyngeal cancer is associated with lower SES [62, 63, 69]. MacKillop et al concluded that there is a strong inverse relationship between income level and areas involved with head and neck cancer in the United States and Ontario [71].
Conclusion
Nasopharyngeal cancer is native to Southeast Asia and the highest incidence and mortality were seen in countries with moderate and low HDI. It is suggested that studies are conducted on determining the causes of the cancer incidence and mortality in the world and the differences between various regions.
Limitations
This study was an ecological study and the limitations include ecological misleading and lack of relation of group results with individuals. Also, in this study, the exact survey about the connection between exposure and outcome is not clearly obvious and all other seen relations were in group and regional level.
Conflicts of Interest
None.
References
- 1.Esmail Nasab N, Moradi G, Zareie M, Ghaderi E, Gheytasi B. Survey of epidemilogic status and incidence rates of cancers in the patients above 15 years old in Kurdistan province. Scientific Journal of Kurdistan University of Medical Sciences. 2007;11(4):18–25. [Google Scholar]
- 2.Devita, Principles and practice of oncology. 2001. pp. 1880–1904. [Google Scholar]
- 3.Tsao SW LK, Huang DP. In: Epsteion-Bar virus. Tselis AC, Jenson H, editors. Hamilton: Taylor & Francis; 2006. Nasopharyngeal carcinoma; pp. 273–295. [DOI] [Google Scholar]
- 4.N R-T. In: Epstein-Barr virus Wymondham. Robertson ES, editor. Norfolk: Caister Academic Press; 2005. Epstein-Bar virus in the pathogenesis of NPC; pp. 71–92. [Google Scholar]
- 5.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55(2):74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 6.Busson P, Keryer C, Ooka T, Corbex M. EBV-associated nasopharyngeal carcinomas: from epidemiology to virus-targeting strategies. Trends Microbiol. 2004;12(8):356–360. doi: 10.1016/j.tim.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Chang ET, Adami HO. The enigmatic epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol Biomarkers Prev. 2006;15(10):1765–1777. doi: 10.1158/1055-9965.EPI-06-0353. [DOI] [PubMed] [Google Scholar]
- 8.Ferlay J, Shin H, Bray F, Forman D, Mathers C, Parkin D. Incidence/mortality data. GLOBOCAN 2008 v2.0. Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10 [Internet]. Lyon, France: International Agency for Research on Cancer. 2010.
- 9.Curado MP EB, Shin HR, Storm H, Ferlay J, Heanue M, editors. Cancer incidence in five continents, Vol. IX. IARC; Lyon: 2007. IARC Sci Publ No. 160. [Google Scholar]
- 10.Mousavi SM, Sundquist J, Hemminki K. Nasopharyngeal and hypopharyngeal carcinoma risk among immigrants in Sweden. International Journal of Cancer. 2010;127(12):2888–2892. doi: 10.1002/ijc.25287. [DOI] [PubMed] [Google Scholar]
- 11.Lam KO, Lee AW, Choi CW, Sze HC, Zietman AL, Hopkins KI, Rosenblatt E. Global Pattern of Nasopharyngeal Cancer: Correlation of Outcome With Access to Radiation Therapy. Int J Radiat Oncol Biol Phys. 2016;94(5):1106–1112. doi: 10.1016/j.ijrobp.2015.11.047. [DOI] [PubMed] [Google Scholar]
- 12.Lubin JH, Purdue M, Kelsey K, Zhang ZF, Winn D, Wei Q, Talamini R. et al. Total exposure and exposure rate effects for alcohol and smoking and risk of head and neck cancer: a pooled analysis of case-control studies. Am J Epidemiol. 2009;170(8):937–947. doi: 10.1093/aje/kwp222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mork J, Lie AK, Glattre E, Clark S, Hallmans G, Jellum E. et al. Human papillomavirus infection as a risk factor for squamous-cell carcinoma of the head and neck. New England Journal of Medicine. 2001;344(15):1125–1131. doi: 10.1056/NEJM200104123441503. [DOI] [PubMed] [Google Scholar]
- 14.Keane MG, Horsfall LJ, Rait G, Pereira SP. Sociodemographic trends in the incidence of pancreatic and biliary tract cancer in UK primary care. PLoS One. 2014;9(9):e108498. doi: 10.1371/journal.pone.0108498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Z, Fang F, Chang ET, Ye W. Cancer risk in the relatives of patients with nasopharyngeal carcinoma-a register-based cohort study in Sweden. Br J Cancer. 2015;112(11):1827–1831. doi: 10.1038/bjc.2015.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang S, Wu S, Zhou J, Chen XY. Screening for nasopharyngeal cancer. 2015;(11) doi: 10.1002/14651858.CD008423.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fles R. et al. Knowledge of general practitioners about nasopharyngeal cancer at the Puskesmas in Yogyakarta, Indonesia. BMC medical education. 2010;10(1):1. doi: 10.1186/1472-6920-10-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Sarraf M, LeBlanc M, Giri PG, Fu KK, Cooper J, Vuong T, Forastiere AA. et al. Chemoradiotherapy versus radiotherapy in patients with advanced nasopharyngeal cancer: phase III randomized Intergroup study 0099. J Clin Oncol. 1998;16(4):1310–1317. doi: 10.1200/JCO.1998.16.4.1310. [DOI] [PubMed] [Google Scholar]
- 19.Huncharek M, Kupelnick B. Combined chemoradiation versus radiation therapy alone in locally advanced nasopharyngeal carcinoma: results of a meta-analysis of 1,528 patients from six randomized trials. Am J Clin Oncol. 2002;25(3):219–223. doi: 10.1097/00000421-200206000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Langendijk JA, Leemans CR, Buter J, Berkhof J, Slotman BJ. The additional value of chemotherapy to radiotherapy in locally advanced nasopharyngeal carcinoma: a meta-analysis of the published literature. J Clin Oncol. 2004;22(22):4604–4612. doi: 10.1200/JCO.2004.10.074. [DOI] [PubMed] [Google Scholar]
- 21.Zhang L, Zhao C, Ghimire B, Hong MH, Liu Q, Zhang Y, Guo Y. et al. The role of concurrent chemoradiotherapy in the treatment of locoregionally advanced nasopharyngeal carcinoma among endemic population: a meta-analysis of the phase III randomized trials. BMC Cancer. 2010;10:558. doi: 10.1186/1471-2407-10-558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang J, Shi M, Hsia Y, Luo S, Zhao L, Xu M, Xiao F. et al. Failure patterns and survival in patients with nasopharyngeal carcinoma treated with intensity modulated radiation in Northwest China: a pilot study. Radiat Oncol. 2012;7:2. doi: 10.1186/1748-717X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu MT, Hsieh CY, Chang TH, Lin JP, Huang CC, Wang AY. Prognostic factors affecting the outcome of nasopharyngeal carcinoma. Jpn J Clin Oncol. 2003;33(10):501–508. doi: 10.1093/jjco/hyg092. [DOI] [PubMed] [Google Scholar]
- 24.Rafiemanesh H, Mehtarpour M, Khani F, Hesami SM, Shamlou R, Towhidi F, Salehiniya H. et al. Epidemiology, incidence and mortality of lung cancer and their relationship with the development index in the world. J Thorac Dis. 2016;8(6):1094–1102. doi: 10.21037/jtd.2016.03.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pakzad R, Mohammadian-Hafshejani A, Ghoncheh M, Pakzad I, Salehiniya H. The incidence and mortality of prostate cancer and its relationship with development in Asia. Prostate Int. 2015;3(4):135–140. doi: 10.1016/j.prnil.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pakzad R, Mohammadian-Hafshejani A, Ghoncheh M, Pakzad I, Salehiniya H. The incidence and mortality of lung cancer and their relationship to development in Asia. Transl Lung Cancer Res. 2015;4(6):763–774. doi: 10.3978/j.issn.2218-6751.2015.12.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahdavifar N, Ghoncheh M, Pakzad R, Momenimovahed Z, Salehiniya H. Epidemiology, Incidence and Mortality of Bladder Cancer and their Relationship with the Development Index in the World. Asian Pac J Cancer Prev. 2016;17(1):381–386. doi: 10.7314/APJCP.2016.17.1.381. [DOI] [PubMed] [Google Scholar]
- 28.Franceschi S, Wild CP. Meeting the global demands of epidemiologic transition - the indispensable role of cancer prevention. Mol Oncol. 2013;7(1):1–13. doi: 10.1016/j.molonc.2012.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ferlay Jea. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://globocan.iarc.fr, accessed on 2/2/2016. 2016.
- 30.Malik K. Human Development Report 2013. The rise of the South: Human progress in a diverse world. The Rise of the South: Human Progress in a Diverse World (March 15, 2013) UNDP-HDRO Human Development Reports. 2013
- 31.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM. et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 32.Adham M, Stoker SD, Wildeman MA, Rachmadi L, Gondhowiardjo S, Atmakusumah D, Gatot D. et al. Current status of cancer care for young patients with nasopharyngeal carcinoma in Jakarta, Indonesia. PLoS One. 2014;9(7):e102353. doi: 10.1371/journal.pone.0102353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wildeman MA, Fles R, Herdini C, Indrasari RS, Vincent AD, Tjokronagoro M, Stoker S. et al. Primary treatment results of Nasopharyngeal Carcinoma (NPC) in Yogyakarta, Indonesia. PLoS One. 2013;8(5):e63706. doi: 10.1371/journal.pone.0063706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teo MC, Soo KC. Cancer trends and incidences in Singapore. Jpn J Clin Oncol. 2013;43(3):219–224. doi: 10.1093/jjco/hys230. [DOI] [PubMed] [Google Scholar]
- 35.Valean S, Acalovschi M, Diculescu M, Manuc M, Goldis A, Sfarti C, Trifan A. Mortality in Digestive Cancers, 2012: International Data and Data from Romania. J Gastrointestin Liver Dis. 2015;24(4):507–514. doi: 10.15403/jgld.2014.1121.244.rom. [DOI] [PubMed] [Google Scholar]
- 36.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 37.Buell P. The effect of migration on the risk of nasopharyngeal cancer among Chinese. Cancer Res. 1974;34(5):1189–1191. [PubMed] [Google Scholar]
- 38.Eriksen MMJ, Ross H. The tobacco atlas. 4th ed. Atlanta: American Cancer Society; 2012. [Google Scholar]
- 39.Fuchs CS, Colditz GA, Stampfer MJ, Giovannucci EL, Hunter DJ, Rimm EB, Willett WC. et al. A prospective study of cigarette smoking and the risk of pancreatic cancer. Arch Intern Med. 1996;156(19):2255–2260. doi: 10.1001/archinte.1996.00440180119015. [DOI] [PubMed] [Google Scholar]
- 40.Muscat JE, Stellman SD, Hoffmann D, Wynder EL. Smoking and pancreatic cancer in men and women. Cancer Epidemiol Biomarkers Prev. 1997;6(1):15–19. [PubMed] [Google Scholar]
- 41.Gallicchio L, Matanoski G, Tao XG, Chen L, Lam TK, Boyd K, Robinson KA. et al. Adulthood consumption of preserved and nonpreserved vegetables and the risk of nasopharyngeal carcinoma: a systematic review. Int J Cancer. 2006;119(5):1125–1135. doi: 10.1002/ijc.21946. [DOI] [PubMed] [Google Scholar]
- 42.Hassan MM, Bondy ML, Wolff RA, Abbruzzese JL, Vauthey JN, Pisters PW, Evans DB. et al. Risk factors for pancreatic cancer: case-control study. Am J Gastroenterol. 2007;102(12):2696–2707. doi: 10.1111/j.1572-0241.2007.01510.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Feng BJ, Jalbout M, Ayoub WB, Khyatti M, Dahmoul S, Ayad M, Maachi F. et al. Dietary risk factors for nasopharyngeal carcinoma in Maghrebian countries. Int J Cancer. 2007;121(7):1550–1555. doi: 10.1002/ijc.22813. [DOI] [PubMed] [Google Scholar]
- 44.Jia WH, Luo XY, Feng BJ, Ruan HL, Bei JX, Liu WS, Qin HD. et al. Traditional Cantonese diet and nasopharyngeal carcinoma risk: a large-scale case-control study in Guangdong, China. BMC Cancer. 2010;10:446. doi: 10.1186/1471-2407-10-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Armstrong RW, Imrey PB, Lye MS, Armstrong MJ, Yu MC, Sani S. Nasopharyngeal carcinoma in Malaysian Chinese: salted fish and other dietary exposures. Int J Cancer. 1998;77(2):228–235. doi: 10.1002/(SICI)1097-0215(19980717)77:2<228::AID-IJC11>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 46.Yuan JM, Wang XL, Xiang YB, Gao YT, Ross RK, Yu MC. Preserved foods in relation to risk of nasopharyngeal carcinoma in Shanghai, China. Int J Cancer. 2000;85(3):358–363. doi: 10.1002/(SICI)1097-0215(20000201)85:3<358::AID-IJC11>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 47.Kasum CM, Jacobs DR Jr, Nicodemus K, Folsom AR. Dietary risk factors for upper aerodigestive tract cancers. Int J Cancer. 2002;99(2):267–272. doi: 10.1002/ijc.10341. [DOI] [PubMed] [Google Scholar]
- 48.Liu YT, Dai JJ, Xu CH, Lu YK, Fan YY, Zhang XL, Zhang CX. et al. Greater intake of fruit and vegetables is associated with lower risk of nasopharyngeal carcinoma in Chinese adults: a case-control study. Cancer Causes Control. 2012;23(4):589–599. doi: 10.1007/s10552-012-9923-z. [DOI] [PubMed] [Google Scholar]
- 49.Jia WH, Qin HD. Non-viral environmental risk factors for nasopharyngeal carcinoma: a systematic review. Semin Cancer Biol. 2012;22(2):117–126. doi: 10.1016/j.semcancer.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 50.Farrow DC, Vaughan TL, Berwick M, Lynch CF, Swanson GM, Lyon JL. Diet and nasopharyngeal cancer in a low-risk population. Int J Cancer. 1998;78(6):675–679. doi: 10.1002/(SICI)1097-0215(19981209)78:6<675::AID-IJC2>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 51.Polesel J, Serraino D, Negri E, Barzan L, Vaccher E, Montella M, Zucchetto A. et al. Consumption of fruit, vegetables, and other food groups and the risk of nasopharyngeal carcinoma. Cancer Causes Control. 2013;24(6):1157–1165. doi: 10.1007/s10552-013-0195-z. [DOI] [PubMed] [Google Scholar]
- 52.Mak HW, Lee SH, Chee J, Tham I, Goh BC, Chao SS, Ong YK. et al. Clinical Outcome among Nasopharyngeal Cancer Patients in a Multi-Ethnic Society in Singapore. PLoS One. 2015;10(5):e0126108. doi: 10.1371/journal.pone.0126108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen MY, Jiang R, Guo L, Zou X, Liu Q, Sun R, Qiu F. et al. Locoregional radiotherapy in patients with distant metastases of nasopharyngeal carcinoma at diagnosis. Chin J Cancer. 2013;32(11):604–613. doi: 10.5732/cjc.013.10148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee AW, Lin JC, Ng WT. Seminars in radiation oncology. Elsevier; 2012. Current management of nasopharyngeal cancer. [DOI] [PubMed] [Google Scholar]
- 55.Datta NR, Samiei M, Bodis S. Radiation therapy infrastructure and human resources in low- and middle-income countries: present status and projections for 2020. Int J Radiat Oncol Biol Phys. 2014;89(3):448–457. doi: 10.1016/j.ijrobp.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 56.Chan AT, Teo PM, Johnson PJ. Nasopharyngeal carcinoma. Ann Oncol. 2002;13(7):1007–1015. doi: 10.1093/annonc/mdf179. [DOI] [PubMed] [Google Scholar]
- 57.Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008-2030): a population-based study. Lancet Oncol. 2012;13(8):790–801. doi: 10.1016/S1470-2045(12)70211-5. [DOI] [PubMed] [Google Scholar]
- 58.Giovino GA, Mirza SA, Samet JM, Gupta PC, Jarvis MJ, Bhala N, Peto R. et al. Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet. 2012;380(9842):668–679. doi: 10.1016/S0140-6736(12)61085-X. [DOI] [PubMed] [Google Scholar]
- 59.Bosetti C, Lucenteforte E, Silverman DT, Petersen G, Bracci PM, Ji BT, Negri E. et al. Cigarette smoking and pancreatic cancer: an analysis from the International Pancreatic Cancer Case-Control Consortium (Panc4) Ann Oncol. 2012;23(7):1880–1888. doi: 10.1093/annonc/mdr541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stelmach W, Kaczmarczyk-Chalas K, Bielecki W, Drygas W. The impact of income, education and health on lifestyle in a large urban population of Poland (Cindi programme) Int J Occup Med Environ Health. 2004;17(3):393–401. [PubMed] [Google Scholar]
- 61.Shi L. Sociodemographic characteristics and individual health behaviors. South Med J. 1998;91(10):933–941. doi: 10.1097/00007611-199810000-00007. [DOI] [PubMed] [Google Scholar]
- 62.Johnson S, McDonald JT, Corsten MJ. Socioeconomic factors in head and neck cancer. J Otolaryngol Head Neck Surg. 2008;37(4):597–601. [PubMed] [Google Scholar]
- 63.Johnson S, McDonald JT, Corsten M, Rourke R. Socio-economic status and head and neck cancer incidence in Canada: a case-control study. Oral Oncol. 2010;46(3):200–203. doi: 10.1016/j.oraloncology.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 64.Mimi CY, HYuan J-M. Seminars in cancer biology. Elsevier; 2002. Epidemiology of nasopharyngeal carcinoma. [DOI] [PubMed] [Google Scholar]
- 65.Yu MC, Ho JH, Ross RK, Henderson BE. Nasopharyngeal carcinoma in Chinese - salted fish or inhaled smoke? Prev Med. 1981;10(1):15–24. doi: 10.1016/0091-7435(81)90002-5. [DOI] [PubMed] [Google Scholar]
- 66.Armstrong RW, Kannan Kutty M, Dharmalingam SK, Ponnudurai JR. Incidence of nasopharyngeal carcinoma in Malaysia, 1968 - 1977. Br J Cancer. 1979;40(4):557–567. doi: 10.1038/bjc.1979.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Conway DI, Brewster DH, McKinney PA, Stark J, McMahon AD, Macpherson LM. Widening socio-economic inequalities in oral cancer incidence in Scotland, 1976-2002. Br J Cancer. 2007;96(5):818–820. doi: 10.1038/sj.bjc.6603621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Greenwood M, Thomson PJ, Lowry RJ, Steen IN. Oral cancer: material deprivation, unemployment and risk factor behaviour - an initial study. Int J Oral Maxillofac Surg. 2003;32(1):74–77. doi: 10.1054/ijom.2002.0274. [DOI] [PubMed] [Google Scholar]
- 69.Greenberg RS, Haber MJ, Clark WS, Brockman JE, Liff JM, Schoenberg JB, Austin DF. et al. The relation of socioeconomic status to oral and pharyngeal cancer. Epidemiology. 1991;2(3):194–200. doi: 10.1097/00001648-199105000-00006. [DOI] [PubMed] [Google Scholar]
- 70.Arsenijevic S, Pantovic V, Gledovic Z, Stojanovic J, Belic B. Demographic characteristics of patients with laryngeal cancer and their socioeconomic status. J BUON. 2010;15(1):131–135. [PubMed] [Google Scholar]
- 71.Mackillop WJ, Zhang-Salomons J, Boyd CJ, Groome PA. Associations between community income and cancer incidence in Canada and the United States. Cancer. 2000;89(4):901–912. doi: 10.1002/1097-0142(20000815)89:4<901::AID-CNCR25>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]