Abstract
Objective
To analyze the effects of the acetabular fracture index (AFI) and other factors on the functional outcome of patients with acetabular fractures involving the posterior wall.
Methods
Forty-eight patients who underwent surgery in our department were reviewed. According to the AFI, which indicates the percentage of remaining intact posterior acetabular arc, the patients were divided into Group A (AFI ≤ 25%, 11 patients), Group B (25% < AFI ≤ 50%, 23 patients), Group C (50% < AFI ≤ 75%, 7 patients), and Group D (75% < AFI ≤ 100%, 7 patients). The AFI was measured with a computed tomography picture archiving and communication system or calculated with the cosine theorem. A nonparametric test and ordinal regression were used to determine the role of the AFI and other factors on the functional outcome. Perioperative information, including demographic and fracture-related data, reduction quality, physical therapy duration, association with a lower limb fracture and avascular necrosis of the femoral head were prospectively gathered.
Results
The mean AFIs of A, B, C, and D groups were 14.3%, 35.9%, 59.5%, and 81.2%, respectively. No statistically significant differences were observed among the groups for demographic and fracture-related data. A better reduction quality (OR = 4.21, 95%CI 1.42 ∼ 12.43, χ2 = 6.781, P = 0.009) and a larger value of AFI (OR = 2.56, 95%CI 1.18 ∼ 5.55, χ2 = 5.648, P = 0.017) result in a higher functional score. The functional outcome of a physical therapy duration of more than 12 months (OR = 0.15, 95%CI 0.02 ∼ 0.90, χ2 = 4.324, P = 0.038) was better than that of less than 12 months. Lower limb fracture (OR = 0.13, 95%CI 0.02 ∼ 0.74, χ2 = 5.235, P = 0.022) and avascular necrosis of femoral head (OR = 0.02, 95%CI 0.00 ∼ 0.87, χ2 = 4.127, P = 0.042) were found to correlate with a lower functional score.
Conclusion
With a greater of AFI, the functional outcome score would be better. Other factors, including reduction quality, physical therapy duration, association with a lower limb fracture, and avascular necrosis of the femoral head, most likely also affect hip functional recovery.
Keywords: Acetabular fracture index, posterior wall, fragment size, functional outcome
Introduction
Fracture of the posterior acetabular wall accounts for 47% of all acetabular fractures, ranking as the most common type of acetabular fracture.1 The combination of anatomic reduction of the articular surface, rigid internal fixation, and early mobilization has become the gold standard since a consensus on the operative treatment of these fractures was established in 1993.2 The incidence of a final unsatisfactory outcome of a posterior wall acetabular fracture is reportedly as high as 30%.3
Several factors contribute to poor outcomes of repair of posterior wall acetabular fractures, including advanced age, severe obesity, avascular necrosis, marginal impaction, severe intra-articular comminuted fracture, association with a posterior column fracture, femoral head or neck fracture, lower limb fracture, residual displacement of >2 mm, and delay in reduction of the hip for >12 hours.4–6 Computed tomography (CT) is more sensitive than plain radiographs for detecting comminution and deficits, loose fragments, marginal impaction, and femoral head lesions.7–11 Appropriate treatment is also affected by the CT findings.12,13 The acetabular fracture index (AFI), defined as the percentage of remaining intact posterior acetabular arc as measured by CT, is used to determine hip stability in patients with posterior wall acetabular fracture.14 The AFI is an objective index used to define the size of the posterior wall fragment. It can be easily attained from a CT scan and has obvious superiority to subjective parameters such as a large fragment, significant segment, incompetent posterior wall, and hip stability. The AFI is useful for preoperative and intraoperative evaluation when open reduction or internal fixation is needed and for predicting the prognosis of a posterior wall acetabular fracture.12
Several studies have been performed to evaluate the relationship between the AFI or fragment size and the stability of the hip,12,14,15 but few have determined the role of the AFI in the postoperative functional outcome in patients with posterior wall acetabular fracture. The aim of this retrospective case study was to determine the inter-relationship of the AFI and other factors with the functional outcome of acetabular fractures involving the posterior wall, including an isolated posterior wall fracture, a posterior column fracture with an associated posterior wall fracture, and a transverse fracture with an associated posterior wall fracture.
Patients and methods
Patients
A retrospective study was conducted on 52 patients presenting with an acetabular fracture involving the posterior wall. All patients underwent surgical treatment by the corresponding author at the Traumatic Orthopaedics Department of Xiangya Hospital from June 2007 to October 2013. Four patients were excluded: one because of total hip arthroplasty and three because of unavailable CT images. Ultimately, 48 patients were included in the study.
Clinical data
Of these 48 patients, 41 were male (85.4%) and 7 were females (14.6%), with a mean age of 44.25 ± 12.17 years (range, 16–73 years). Twenty fractures were on the right side (41.7%), 27 were on the left (56.2%), and 1 was bilateral (2.0%). The fracture etiologies included traffic accidents (35 patients, 72.9%), falls from a height (7 patients, 14.6%), and crush injuries (6 patients, 12.5%). With respect to complications, 31 patients had hip dislocation (64.6%), 11 had primary sciatic nerve injury (22.9%), 17 had lower limb fracture (35.4%), 5 had brain injury (10.4%), and 1 had iatrogenic sciatic nerve injury (2.1%). The mean duration from fracture to surgery was 9 days (range, 3–30 days). The average surgical duration was 149.5 minutes (range, 75–360 minutes), and the mean blood loss was 725 ml (range, 300–3300 ml). The average duration of physical therapy was 24 months (range, 6–68 months). Follow-up evaluations were performed in our clinic at 2, 4, 6, 12, 24, and 36 months after surgery. Physical therapy, such as lower extremity muscle activity and continuous passive motion, was encouraged in all patients. Some patients came from rural areas and had no access to a physical therapy center for physical therapy. All patients were traced for follow-up functional assessment. The quality of fracture reduction was evaluated according to the Matta radiological scoring system.16,17
On the CT image of the fractured side, we selected the section that demonstrated the largest amount of fractured posterior acetabulum (i.e., the smallest intact remaining posterior acetabulum). In our patients, the selected section was sometimes at the level of the central acetabular fossa. A contralateral section was selected and matched by comparing the sizes of the femoral heads and the configuration of the femoral fovea, acetabular fossa, and pelvis. These sections were used for measurements.
AFI measurement
The AFI was defined as the percentage of remaining intact posterior acetabular arc (A).12 It is described by the following relationship:
Furthermore,
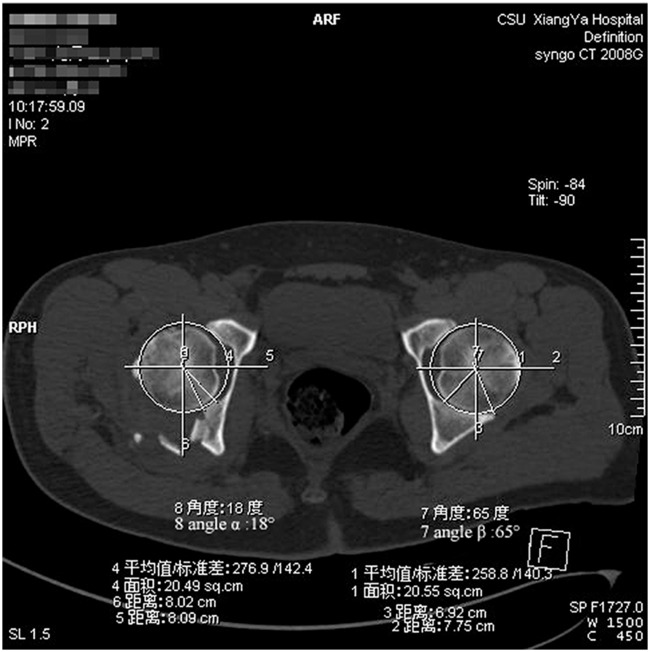
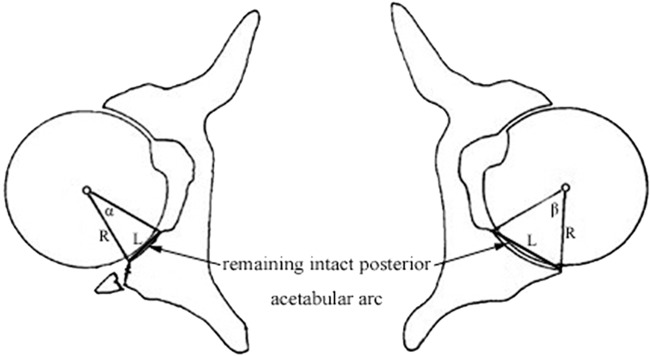
where A is the acetabular arc, R is the radius, α is the angle formed by the arc line to the remaining intact posterior acetabular margin on the fractured side, and β is the angle formed by the arc line to the posterior acetabular margin on the contralateral normal side (Figure 1).
Figure 1.
The center of the acetabular arc is marked, and the angles (α/β) were created from the remaining intact posterior acetabulum on the fractured side and contralateral side.
Two methods were used to measure α and β: (1) For most patients whose CT scans (Definition Syngo Somatom CT 2008G; Siemens, Munich, Germany) were performed in our hospital, we made direct measurements with a CT picture archiving and communication system (PACS) (DHC Software Co., Ltd., Beijing, China). (2) For two patients whose CT scans were performed in other hospitals, we performed calculations using the cosine theorem on their CT films:
where L is the straight line created by the margins of the remaining intact posterior acetabulum on the fractured side and contralateral normal side (Figure 2).
Figure 2.
Straight lines created by the margins of the remaining intact posterior acetabulum on the fractured and normal sides were used to calculate the acetabular fracture index by the cosine theorem.
For every patient, we repeated the measurement using multiple CT image section levels to ensure that the greatest percentage of posterior wall fracture involvement was identified. All measurements were repeated three times by the same radiologic professor and orthopedic professor to minimize errors. The mean AFI for all patients was 40.96 ± 22.82 (range, 0.00–85.90).
Grouping
The 48 patients were classified into the following groups according to the AFI: Group A (AFI ≤ 25%, 11 patients), Group B (25% < AFI ≤ 50%, 23 patients), Group C (50% < AFI ≤ 75%, 7 patients), and Group D (75% < AFI ≤ 100%, 7 patients). The data regarding this subgroup classification are shown in Table 1.
Table 1.
Demographic and fracture-related data in each group.
| Group | A | B | C | D |
|---|---|---|---|---|
| Patients (n) | 11 | 23 | 7 | 7 |
| Mean AFI (%) | 14.3 | 35.9 | 59.5 | 81.2 |
| Age (y) | 44.7 | 42.7 | 44.6 | 48.4 |
| Sex (male/female) | 10/1 | 18/5 | 7/0 | 6/1 |
| Fracture etiology | ||||
| Fall from height | 2 | 3 | 2 | 0 |
| Crush injury | 2 | 2 | 0 | 2 |
| Traffic accident | 7 | 18 | 5 | 5 |
| Hip dislocation | 9 | 16 | 2 | 4 |
| Primary sciatic nerve injury | 3 | 6 | 1 | 1 |
| Lower limb fracture | 3 | 6 | 3 | 5 |
| Brain injury | 1 | 4 | 0 | 0 |
| Trauma-to-surgery time (d) | 11.1 | 16.3 | 11.1 | 9.7 |
| Surgical duration (min) | 163.7 | 143.3 | 189.3 | 172.1 |
| Blood loss (ml) | 872.7 | 704.3 | 1221.4 | 855.7 |
| Operative complications | ||||
| Iatrogenic sciatic nerve injury | 0 | 1 | 0 | 0 |
| Infection | 0 | 0 | 0 | 0 |
| Reduction quality | ||||
| Anatomical | 4 | 16 | 4 | 5 |
| Good | 6 | 4 | 3 | 2 |
| Poor | 1 | 3 | 0 | 0 |
| Radiological evaluation | ||||
| Traumatic arthritis | 2 | 0 | 0 | 0 |
| Heterotopic ossification | 6 | 7 | 3 | 1 |
| Avascular necrosis of the femoral head | 0 | 0 | 1 | 0 |
| Physical therapy duration (months) | 36.0 | 23.7 | 22.9 | 22.6 |
| Merle’d Aubigne and Postel functional hip score | ||||
| Excellent | 2 | 10 | 4 | 4 |
| Good | 5 | 9 | 2 | 3 |
| Fair | 1 | 4 | 0 | 0 |
| Poor | 3 | 0 | 1 | 0 |
Data are presented as number of patients unless otherwise indicated.
AFI, acetabular fracture index
Implant selection
Different implants were used according to the AFI and other factors of posterior wall acetabular fracture. For an AFI of 25% to 75%, lag screws, neutralization plates, and spring plates were used. For an AFI of >75% or the presence of a large articular defect in the posterior wall, a gluteus medius pedicled greater trochanter bone flap plus lag screws and neutralization plates were used. Lag screws and neutralization plates were used in 24 patients (50.0%); lag screws, neutralization plates, and spring plates were used in 14 patients (29.2%); and a gluteus medius pedicled greater trochanter bone flap plus lag screws and neutralization plates were used in 4 patients (8.3%) to reconstruct the posterior wall.18
Statistical analysis
EpiData 3.0 was used to establish a database, and statistical analysis was performed using SPSS 17.0 for Windows (SPSS Inc., Chicago, IL, USA). Measurement data are presented as mean ± standard deviation, median, semi-interquartile range, lower (25th) quartile, and upper (75th) quartile. Enumeration data are presented as percentages or proportions. Two-sample t-tests and rank-sum tests were used for comparisons among the groups. Single-factor analysis was performed using two independent-sample nonparametric tests or multiple independent-sample nonparametric tests. Because a variety of factors had mutual interference and it was difficult to assess the influence of each factor on the functional outcome using single-factor analysis, multiple-factor analyses were also used. Multiple-factor analysis was performed using ordinal regression. All data were analyzed at a significance level of P < 0.05. Complete statistical analysis was performed by a biostatistician consultant.
Results
All patients underwent follow-up evaluations at every time point. No serious perioperative complications were observed. Only one patient had an iatrogenic sciatic nerve injury. This patient was treated with neurotrophic drugs for 3 months, and the muscle strength and sensation were finally completely restored to normal at the 1-year follow-up visit. All fractures were completely united at the 4-month follow-up visit, which was confirmed by radiologic examination.
Twenty-nine (60.4%) patients achieved anatomical reduction, 15 (31.3%) achieved good reduction, and 4 (8.3%) achieved poor reduction. Heterotopic ossification according to the Brooker grading system was observed in 11 (22.9%) patients with grade I ossification, 5 (10.4%) with grade II, and 1 (2.1%) with grade III; 31 (64.6%) patients had no heterotopic ossification. Two (4.2%) patients had traumatic arthritis, and one (2.1%) had necrosis of the femoral head. The functional outcome according to the modified Merle’d Aubigne and Postel hip scoring system was excellent in 20 cases (41.7%), good in 19 (39.6%), fair in 5 (10.4%), and poor in 4 (8.3%). The demographic and fracture-related data are shown in Table 1.
Comparison among groups
No significant differences in demographic and fracture-related data were observed among the groups, including sex, age, combinations with dislocation, primary and iatrogenic sciatic nerve injury, lower limb fracture, brain injury, trauma-to-surgery time, operation duration, blood loss, reduction quality, heterotopic ossification, traumatic arthritis, avascular necrosis of the femoral head, and physical therapy duration.
Single-factor analysis
Two independent-sample and multiple independent-sample nonparametric tests showed that the factors affecting functional outcome were blood loss (P = 0.024), physical therapy duration (P = 0.035), reduction quality (P = 0.001), and heterotopic ossification (P = 0.042). Blood loss of >1000 ml, physical therapy duration of <1 year, poor reduction quality, and heterotopic ossification were most likely to impair the functional outcome. The results of the single-factor analysis are shown in Table 2.
Table 2.
Results of single-factor analysis.
| Variable | Functional score (%) |
Mean rank | Z/χ2 | P | ||||
|---|---|---|---|---|---|---|---|---|
| Poor | Fair | Good | Excellent | Total | ||||
| Sex | ||||||||
| Male | 4 (9.8) | 5 (12.2) | 16 (39.0) | 16 (39.0) | 41 (100.0) | 23.54 | −1.241 | 0.215 |
| Female | 0 (0.0) | 0 (0.0) | 3 (42.9) | 4 (57.1) | 7 (100.0) | 30.14 | ||
| Age (y) | ||||||||
| <20 | 0 (0.0) | 0 (0.0) | 1 (100.0) | 0 (0.0) | 1 (100.0) | 19.00 | 0.705 | 0.872 |
| 20–40 | 1 (7.7) | 0 (0.0) | 6 (46.2) | 6 (46.2) | 13 (100.0) | 26.73 | ||
| 40–60 | 2 (6.9) | 4 (13.8) | 12 (41.4) | 11 (37.9) | 29 (100.0) | 23.60 | ||
| ≥60 | 1 (20.0) | 1 (20.0) | 0 (0.0) | 3 (60.0) | 5 (100.0) | 25.00 | ||
| AFI | ||||||||
| <25.0% | 3 (27.3) | 1 (9.1) | 5 (45.5) | 2 (18.2) | 11 (100.0) | 16.95 | 5.567 | 0.135 |
| 25.0%–50.0% | 0 (0.0) | 4 (17.4) | 9 (39.1) | 10 (43.5) | 23 (100.0) | 25.39 | ||
| 50.0%–75.0% | 1 (14.3) | 0 (0.0) | 2 (28.6) | 4 (57.1) | 7 (100.0) | 27.79 | ||
| ≥75.0% | 0 (0.0) | 0 (0.0) | 3 (42.9) | 4 (57.1) | 7 (100.0) | 30.14 | ||
| Trauma etiology | ||||||||
| Fall from height | 0 (0.0) | 2 (28.6) | 3 (42.9) | 2 (28.6) | 7 (100.0) | 21.14 | 0.769 | 0.681 |
| Crush injury | 1 (16.7) | 0 (0.0) | 3 (50.0) | 2 (33.3) | 6 (10.0) | 22.75 | ||
| Traffic accident | 3 (8.6) | 3 (8.6) | 13 (37.1) | 16 (45.7) | 35 (100.0) | 25.47 | ||
| Hip dislocation | ||||||||
| Yes | 2 (6.5) | 4 (12.9) | 10 (32.3) | 15 (48.4) | 31 (100.0) | 25.82 | −0.951 | 0.342 |
| No | 2 (11.8) | 1 (5.9) | 9 (52.9) | 5 (29.4) | 17 (100.0) | 22.09 | ||
| Primary sciatic nerve injury | ||||||||
| Yes | 2 (18.2) | 2 (18.2) | 4 (36.4) | 3 (27.3) | 11 (100.0) | 19.14 | −1.557 | 0.120 |
| No | 2 (5.4) | 3 (8.1) | 15 (40.5) | 17 (45.9) | 37 (100.0) | 26.09 | ||
| Lower limb fracture | ||||||||
| Yes | 3 (17.6) | 1 (5.9) | 7 (41.2) | 6 (35.3) | 17 (100.0) | 22.26 | −0.881 | 0.378 |
| No | 1 (3.2) | 4 (12.9) | 12 (38.7) | 14 (45.2) | 31 (100.0) | 25.73 | ||
| Thoracic and abdominal injury | ||||||||
| Yes | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| No | 4 (8.3) | 5 (10.4) | 19 (39.6) | 20 (41.7) | 48 (100.0) | |||
| Brain injury | ||||||||
| Yes | 0 (0.0) | 2 (40.0) | 2 (40.0) | 1 (20.0) | 5 (100.0) | 18.10 | −1.162 | 0.245 |
| No | 4 (9.3) | 3 (7.0) | 17 (39.5) | 19 (44.2) | 43 (100.0) | 25.24 | ||
| Iatrogenic sciatic nerve injury | ||||||||
| Yes | 0 (0.0) | 0 (0.0) | 1 (100.0) | 0 (0.0) | 1 (100.0) | 19.00 | −0.427 | 0.669 |
| No | 4 (8.5) | 5 (10.6) | 18 (38.3) | 20 (42.6) | 47 (100.0) | 24.62 | ||
| Trauma-to-surgery time (d) | ||||||||
| ≤14 | 3 (7.9) | 2 (5.3) | 18 (47.4) | 15 (39.5) | 38 (100.0) | 24.76 | −0.273 | 0.785 |
| >14 | 1 (10.0) | 3 (30.0) | 1 (10.0) | 5 (50.0) | 10 (100.0) | 23.50 | ||
| Surgical duration (min) | ||||||||
| ≤120 | 1 (6.7) | 0 (0.0) | 5 (33.3) | 9 (60.0) | 15 (100.0) | 29.60 | −1.830 | 0.067 |
| >120 | 3 (9.1) | 5 (15.2) | 14 (42.4) | 11 (33.3) | 33 (100.0) | 22.18 | ||
| Blood loss (ml) | ||||||||
| ≤1000 | 2 (5.1) | 2 (5.1) | 17 (43.6) | 18 (46.2) | 39 (100.0) | 26.54 | −2.259 | 0.024 |
| >1000 | 2 (22.2) | 3 (33.3) | 2 (22.2) | 2 (22.2) | 9 (100.0) | 15.67 | ||
| Physical therapy duration (m) | ||||||||
| ≤12 | 1 (14.3) | 1 (14.3) | 5 (71.4) | 0 (0.0) | 7 (100.0) | 14.93 | −2.105 | 0.035 |
| >12 | 3 (7.3) | 4 (9.8) | 14 (34.1) | 20 (48.8) | 41 (100.0) | 26.13 | ||
| Reduction quality | ||||||||
| Anatomical | 0 (0.0) | 2 (6.9) | 9 (31.0) | 18 (62.1) | 29 (100.0) | 30.28 | 14.862 | 0.001 |
| Good | 3 (20.0) | 2 (13.3) | 8 (53.3) | 2 (13.3) | 15 (100.0) | 16.70 | ||
| Poor | 1 (25.0) | 1 (25.0) | 2 (50.0) | 0 (0.0) | 4 (100.0) | 11.88 | ||
| Heterotopic ossification | ||||||||
| No | 1 (3.2) | 1 (3.2) | 13 (41.9) | 16 (51.6) | 31 (100.0) | 28.15 | 8.202 | 0.042 |
| Grade I | 2 (18.2) | 1 (9.1) | 5 (45.5) | 3 (27.3) | 11 (100.0) | 20.23 | ||
| Grade II | 1 (20.0) | 2 (40.0) | 1 (20.0) | 1 (20.0) | 5 (100.0) | 14.80 | ||
| Grade III | 0 (0.0) | 1 (100.0) | 0 (0.0) | 0 (0.0) | 1 (100.0) | 7.00 | ||
| Traumatic arthritis | ||||||||
| Yes | 0 (0.0) | 1 (50.0) | 1 (50.0) | 0 (0.0) | 2 (100.0) | 13.00 | −1.276 | 0.202 |
| No | 4 (8.7) | 4 (8.7) | 18 (39.1) | 20 (43.5) | 46 (100.0) | 25.00 | ||
| Avascular necrosis of the femoral head | ||||||||
| Yes | 1 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (100.0) | 2.50 | −1.708 | 0.088 |
| No | 3 (6.4) | 5 (10.6) | 19 (39.6) | 20 (41.7) | 47 (100.0) | 24.97 | ||
AFI, acetabular fracture index
Multiple-factor analysis
Ordinal regression showed that five factors (AFI, reduction quality, association with a lower limb fracture, physical therapy duration, and avascular necrosis of the femoral head) were associated with the final functional outcome after surgery (Table 3). A better reduction quality (odds ratio [OR] = 4.21, 95% confidence interval [CI] = 1.42 – 12.43, χ2 = 6.781, P = 0.009) and a larger AFI (OR = 2.56, 95% CI = 1.18 – 5.55, χ2 = 5.648, P = 0.017) resulted in a higher functional score. The functional outcome associated with a physical therapy duration of >12 months (OR = 0.15, 95% CI = 0.02 – 0.90, χ2 = 4.324, P = 0.038) was better than that associated with a physical therapy duration of <12 months. Lower limb fracture (OR = 0.13, 95% CI = 0.02 – 0.74, χ2 = 5.235, P = 0.022) and avascular necrosis of the femoral head (OR = 0.02, 95% CI = 0.00 – 0.87, χ2 = 4.127, P = 0.042) were correlated with a lower functional score.
Table 3.
Multiple-factor ordinal regression analysis.
| Variable | Estimated value | Standard error | Wald χ2 | OR | 95% CI |
P | |
|---|---|---|---|---|---|---|---|
| Lower limit | Upper limit | ||||||
| AFI | 0.939 | 0.395 | 5.648 | 2.56 | 1.18 | 5.55 | 0.017 |
| Lower limb fracture | |||||||
| Yes | −2.056 | 0.899 | 5.235 | 0.13 | 0.02 | 0.74 | 0.022 |
| No | 0.000 | 1.00 | 1.00 | 1.00 | |||
| Physical therapy duration (m) | |||||||
| ≤12 | −1.905 | 0.916 | 4.324 | 0.15 | 0.02 | 0.90 | 0.038 |
| >12 | 0.000 | 1.00 | 1.00 | 1.00 | |||
| Reduction quality | 1.438 | 0.552 | 6.781 | 4.21 | 1.43 | 12.43 | 0.009 |
| Avascular necrosis of the femoral head | |||||||
| Yes | −4.090 | 2.013 | 4.127 | 0.02 | 0.00 | 0.87 | 0.042 |
| No | 0.000 | 1.00 | 1.00 | 1.00 | |||
AFI, acetabular fracture index; OR, odds ratio; CI, confidence interval
Discussion
Several methods can be used to measure the size of posterior wall acetabular fracture fragments. Keith et al.19 used CT scans to measure the size of the remaining acetabular depths at the level of the transverse slice compared with the normal contralateral side through the fovea of the femoral head in adult cadavers. Moed et al.14 and Reagan and Moed15 used the level of the transverse slice through the greatest percentage of posterior wall fracture involvement on CT scans. Calkins et al.12 selected the section containing the largest amount of fractured posterior acetabulum on the CT scan using a plastic template to mark the center of the acetabular arc and a goniometer to measure the acetabular arc angle. The straight line of the posterior acetabulum was measured to calculate the approximate AFI, which closely approximates the real AFI. In the present study, this measurement was similar to that described by Calkins et al.12 Several modifications were performed to collect higher-quality data. First, we used CT PACS software to confirm the center of the acetabular arc, draw the acetabular arc, and measure the acetabular arc angle, which was more convenient and precise than using a plastic template and goniometer. Second, we used the cosine theorem to calculate the acetabular arc angle and the real AFI instead of the approximate AFI.
With respect to the influence of the size of the posterior wall acetabular fracture fragment, some studies have focused on the stability, articular contact area, and contact stress of the hip, but few have disclosed the relationship between the fragment size and the functional outcome of the hip. Keith et al.19 performed a progressive osteotomy from the acetabular posterior wall in 16 cadaveric hips and tested the stability. They found that all hips with removal of <20% of the posterior part of the acetabular wall were stable, while those with removal of >40% were unstable. Vailas et al.20 reported that fragments involving ≤25% of the acetabulum do not affect joint stability, while fragments involving ≥50% can affect joint stability. The stability of fragments involving 25% to 50% is determined by the posterior capsule. Calkins et al.12 found that all hips with <34% of the remaining posterior acetabulum were unstable and that hips with >55% were stable. Hips were either stable or unstable between these values. In the present study, we found that the size of the posterior wall acetabular fracture fragment could affect the hip joint functional outcome. The functional outcome score was better with a greater AFI. Many factors other than the fracture fragment size of the posterior wall affect the hip joint functional outcome, including hip dislocation, sciatic nerve injury, femoral head injury or necrosis, reduction quality, traumatic arthritis, heterotopic ossification, physical therapy, and others. Reduction quality is considered to be an important factor.21,22 Mears et al.23 showed that stable anatomic reduction of most displaced acetabular fractures affords an optimal prognosis, especially in younger patients. In the present study, we also found that the reduction quality significantly influenced the functional outcome. Our study also showed that the functional outcome was better with a physical therapy duration of >12 than <12 months. This result may be attributed to the different medical conditions among the 48 patients studied. Some patients came from rural areas without any medical insurance or access to a nearby physical therapy center. The patient’s economic capability is another factor affecting systemic or long-term postoperative physical therapy. Thus, poor physical therapy conditions may result in a poor functional outcome. Heterotopic ossification is a very common postoperative complication of acetabular fractures.24 A significant amount of ectopic bone could result in a ≥20% loss of hip motion. The iliofemoral surgical approach was found to be highly correlated with ectopic bone formation.25 Whether prophylactic indomethacin prevents heterotopic ossification is still debated.26–28 In the present study, prophylactic indomethacin was not used for all patients. The incidence of heterotopic ossification was 27.1% without severe heterotopic ossification that impaired hip function.
The present study has some limitations. The first is the relatively small sample size of each group. The study included only one patient with avascular necrosis of the femoral head and two with traumatic arthritis; therefore, valuable statistical results were difficult to obtain. We plan to enlarge the sample size in future research. Second, little consideration was given to the effects of the number, configuration, displacement, and distribution of fracture fragments; multi-fragmentary fracture pattern; marginal impaction; intra-articular fragments; and extension of the fracture into the weight-bearing dome, all of which may affect the stability of the weight-bearing area and the clinical outcome.
In conclusion, a higher AFI is associated with a better functional outcome score. Other factors, including reduction quality, physical therapy duration, association with a lower limb fracture, and avascular necrosis of the femoral head, are also likely to affect hip functional recovery.
Declaration of conflicting interest
The authors declare that there are no conflicts of interest.
Funding
This work was supported by the China Scholarship Council (student ID: 201606370164), the Open-End Fund for the Valuable and Precision Instruments of Central South University (CSUZC201733), and the Hunan Provincial Innovation Foundation for Postgraduate Students (CX2016B060).
References
- 1.Sen RK, Tripathy SK, Aggarwal S, et al. Posterior wall reconstruction using iliac crest strut graft in severely comminuted posterior acetabular wall fracture. Int Orthop 2011; 35: 1223–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Letournel E, Judet R. Fractures of the acetabulum, New York: Springer-Verlag, 1993. [Google Scholar]
- 3.Giannoudis PV, Nikolaou VS. Surgical techniques-how do I do it? Open reduction and internal fixation of posterior wall fractures of the acetabulum. Injury 2008; 39: 1113–1118. [DOI] [PubMed] [Google Scholar]
- 4.Borg T, Hailer NP. Outcome 5 years after surgical treatment of acetabular fractures: a prospective clinical and radiographic follow-up of 101 patients. Arch Orthop Trauma Surg 2015; 135: 227–233. [DOI] [PubMed] [Google Scholar]
- 5.Li YL, Tang YY. Displaced acetabular fractures in the elderly: results after open reduction and internal fixation. Injury 2014; 45: 1908–1913. [DOI] [PubMed] [Google Scholar]
- 6.Meena UK, Tripathy SK, Sen RK, et al. Predictors of postoperative outcome for acetabular fractures. Orthop Traumatol Surg Res 2013; 99: 929–935. [DOI] [PubMed] [Google Scholar]
- 7.Moed BR, Kregor PJ, Reilly MC, et al. Current management of posterior wall fractures of the acetabulum. Instr Course Lect 2015; 64: 139–159. [PubMed] [Google Scholar]
- 8.Sinatra PM, Moed BR. CT-generated radiographs in obese patients with acetabular fractures: can they be used in lieu of plain radiographs? Clin Orthop Relat Res 2014; 472: 3362–3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rehman H, Clement RG, Perks F, et al. Imaging of occult hip fractures: CT or MRI? Injury 2016; 47: 1297–1301. [DOI] [PubMed] [Google Scholar]
- 10.Shah SB, Manson TT, Nascone JW, et al. Radiographic determinants of early failure after posterior wall acetabular fracture fixation. Orthopedics 2016; 39: e1104–e1111. [DOI] [PubMed] [Google Scholar]
- 11.Harnroongroj T, Suangyanon P, Tharmviboonsri T, et al. Posterior acetabular arc angle of the femoral head assesses instability of posterior fracture-dislocation of the hip. Int Orthop 2013; 37: 1141–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Calkins MS, Zych G, Latta L, et al. Computed tomography evaluation of stability in posterior fracture dislocation of the hip. Clin Orthop Relat Res 1988; 227: 152–163. [PubMed] [Google Scholar]
- 13.Sauser DD, Billimoria PE, Rouse GA, et al. CT evaluation of hip trauma. AJR Am J Roentgenol 1980; 135: 269–274. [DOI] [PubMed] [Google Scholar]
- 14.Moed BR, Ajibade DA, Israel H. Computed tomography as a predictor of hip stability status in posterior wall fractures of the acetabulum. J Orthop Trauma 2009; 23: 7–15. [DOI] [PubMed] [Google Scholar]
- 15.Reagan JM, Moed BR. Can computed tomography predict hip stability in posterior wall acetabular fractures? Clin Orthop Relat Res 2011; 469: 2035–2041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferguson TA, Patel R, Bhandari M, et al. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br 2010; 92: 250–257. [DOI] [PubMed] [Google Scholar]
- 17.Bhandari M, Matta J, Ferguson T, et al. Predictors of clinical and radiological outcome in patients with fractures of the acetabulum and concomitant posterior dislocation of the hip. J Bone Joint Surg Br 2006; 88: 1618–1624. [DOI] [PubMed] [Google Scholar]
- 18.Sun B, Li K, Zhu Y, et al. Posterior wall reconstruction using intertrochanteric crest strut graft in comminuted posterior acetabular wall fractures. Hip Int 2013; 23: 199–203. [DOI] [PubMed] [Google Scholar]
- 19.Keith JJ, Jr, Brashear HJ, Jr, Guilford WB. Stability of posterior fracture-dislocations of the hip. Quantitative assessment using computed tomography. J Bone Joint Surg Am 1988; 70: 711–714. [PubMed] [Google Scholar]
- 20.Vailas JC, Hurwitz S, Wiesel SW. Posterior acetabular fracture-dislocations: fragment size, joint capsule, and stability. J Trauma 1989; 29: 1494–1496. [PubMed] [Google Scholar]
- 21.Shazar N, Eshed I, Ackshota N, et al. Comparison of acetabular fracture reduction quality by the ilioinguinal or the anterior intrapelvic (modified Rives-Stoppa) surgical approaches. J Orthop Trauma 2014; 28: 313–319. [DOI] [PubMed] [Google Scholar]
- 22.Boudissa M, Ruatti S, Kerschbaumer G, et al. Part 2: outcome of acetabular fractures and associated prognostic factors-a ten-year retrospective study of one hundred and fifty six operated cases with open reduction and internal fixation. Int Orthop 2016; 40: 2151–2156. [DOI] [PubMed] [Google Scholar]
- 23.Mears DC, Velyvis JH, Chang CP. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res 2003; 407: 173–186. [DOI] [PubMed] [Google Scholar]
- 24.Daum WJ, Scarborough MT, Gordon W, Jr, et al. Heterotopic ossification and other perioperative complications of acetabular fractures. J Orthop Trauma 1992; 6: 427–432. [DOI] [PubMed] [Google Scholar]
- 25.Ghalambor N, Matta JM and Bernstein L. Heterotopic ossification following operative treatment of acetabular fracture. An analysis of risk factors. Clin Orthop Relat Res 1994; 305: 96–105. [PubMed]
- 26.Griffin SM, Sims SH, Karunakar MA, et al. Heterotopic ossification rates after acetabular fracture surgery are unchanged without indomethacin prophylaxis. Clin Orthop Relat Res 2013; 471: 2776–2782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sagi HC, Jordan CJ, Barei DP, et al. Indomethacin prophylaxis for heterotopic ossification after acetabular fracture surgery increases the risk for nonunion of the posterior wall. J Orthop Trauma 2014; 28: 377–383. [DOI] [PubMed] [Google Scholar]
- 28.Firoozabadi R, O’Mara TJ, Swenson A, et al. Risk factors for the development of heterotopic ossification after acetabular fracture fixation. Clin Orthop Relat Res 2014; 472: 3383–3388. [DOI] [PMC free article] [PubMed] [Google Scholar]