Abstract
Histoplasmosis is an infection caused by a fungus called Histoplasma. Diagnosis of histoplasmosis is based on the culture of biological samples and detection of fungus in tissues. Histoplasmosis can mimic malignant lesions. We report a 65-year-old, immunocompetent, male patient with back pain. We describe the main clinical and radiological characteristics in our patient who had vertebral histoplasmosis that mimicked cancer. A computed tomography scan showed lytic lesions of the right side of T4, T5, and T6 vertebral bodies. Magnetic resonance imaging displayed abnormal marrow signals in T4, T5, and T6 vertebral bodies (low signal on T1, high on T2 and short time inversion recovery (STIR)). Which was mimicking malignancy, such as haematological malignancy and metastatic bone cancer. Therefore, thoracic spinal surgery using the anterior approach was performed. An intraoperative frozen section examination and routine postoperative pathology showed thoracic histoplasmosis infection. Treatment of histoplasmosis was performed with oral itraconazole. The lesions did not progress and the patient symptomatically improved at a follow-up of 26 months.
Keywords: Histoplasmosis, spine, infection, cancer
Introduction
Histoplasmosis is caused by reproductive spores of the fungus Histoplasma capsulatum. Primary pulmonary infection is most commonly transmitted when these spores become airborne, often during clean-up or demolition projects. Air currents can carry the spores, which float in the air and expose unsuspecting individuals to contaminated sites.1 Histoplasmosis is not contagious, and thus cannot be spread from person to person. Disseminated histoplasmosis usually presents as a progressive disease, which can affect nearly any part of body and is considered as infiltration of macrophages into infected tissues.2 Histoplasmosis is classically described as an endemic mycosis, which often occurs in patients with an immunocompromised condition 3. Chronic, progressive, disseminated infection of histoplasmosis rarely occurs in older adults who do not have compromised immune systems 4. Many cases of histoplasmosis mimic malignancy.5,6,7 We report a 65-year-old immunocompetent male patient with back pain. We describe the main clinical and radiological characteristics of our patient who had vertebral histoplasmosis that mimicked cancer.
Case report
A 65-year-old man visited our hospital because of his gradually worsening back pain for 2 months. He was administered Nonsteroidal Antiinflammatory Drugs (NSAIDs) and paracetamol for pain relief, but these did not relieve the pain. He denied any persistent fevers, night sweats, chills, and respiratory symptoms. His past medical history and review of systems were unremarkable. A physical examination showed that the patient had a clear consciousness, upper thoracic (over the T4 and T6 vertebrae) percussion pain of the spine, myodynamia was V, and reflexes were all normal. The cervical and lumbosacral spine was clinically normal. Laboratory tests showed a white blood cell (WBC) count of 7.1 × 109/L and the percentage of neutrophilic granulocytes was 83.2%, the C-reactive protein (CRP) level was 63.0 mg/L, and a T-spot was negative. A bone marrow biopsy was normal.
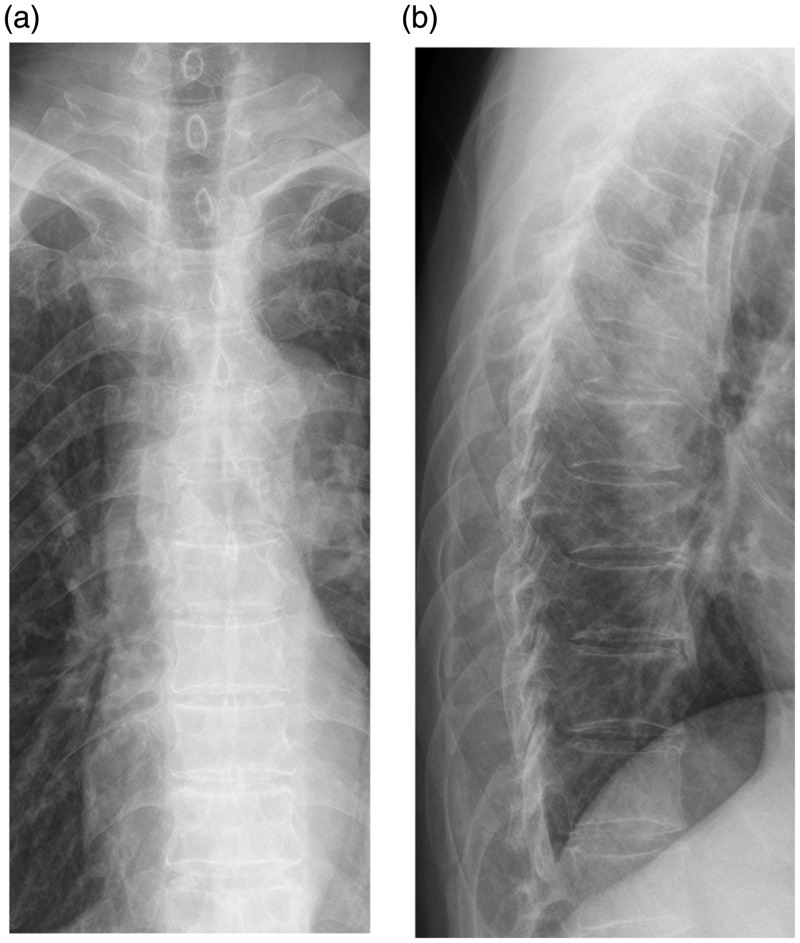
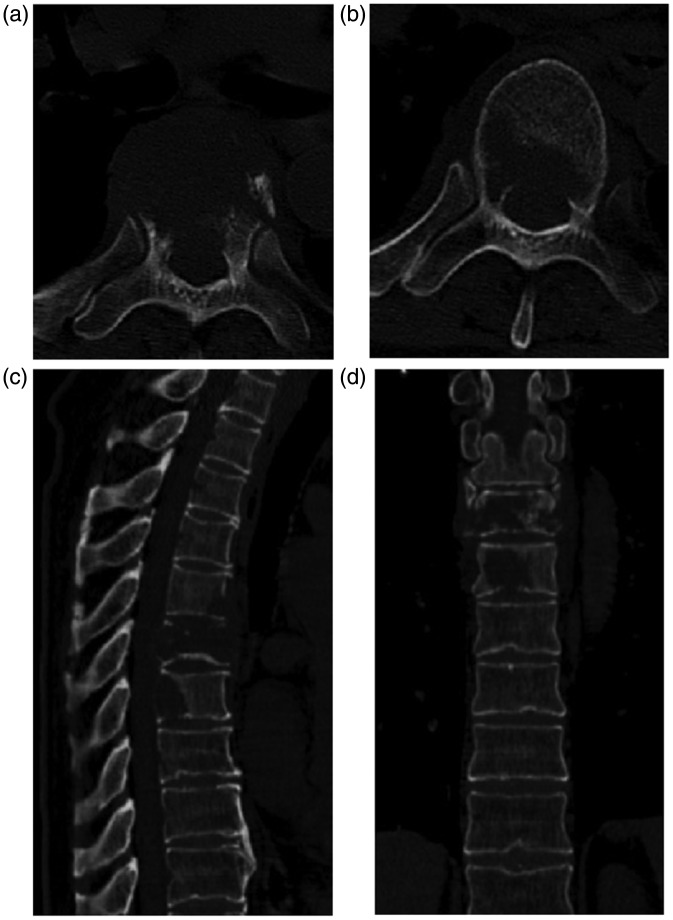
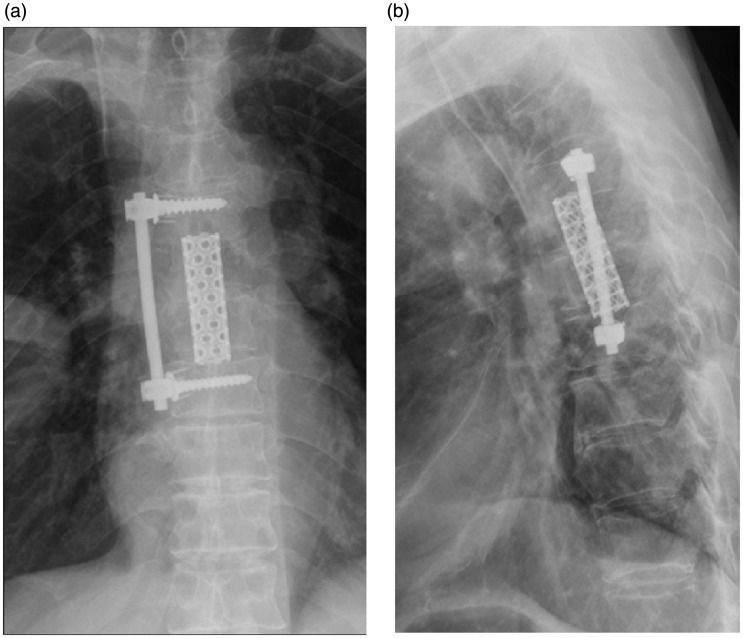
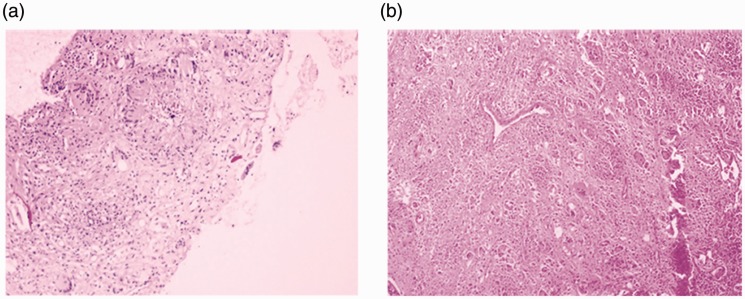
An X-ray of the thoracic spine showed slight compression of the body of T6 (Figure 1). Ultrasonic examination of the pelvis and abdomen was normal. A computed tomography (CT) scan showed lytic lesions of the right side of the T4, T5, and T6 vertebral bodies (Figure 2). Magnetic resonance imaging (MRI) displayed abnormal marrow signals in T4, T5, and T6 vertebral bodies (low signal on T1, high signal on T2 and short time inversion recovery), with some compressed fracture of the T5 body and the lesions partly extended into the right pedicle (Figure 3). Which is mimicking malignancy, such as haematological malignancy and metastatic bone cancer. The spinal cord was normal. There was no intra-spinal or extra-osseous component. A Positron Emission Computed Tomography (PET-CT) scan demonstrated increased uptake in T4, T5, and T6 vertebrae on late films. A CT-guided transpedicular biopsy of T6 showed a lesion (Figure 4). A histopathological examination showed granulomatous inflammation with necrosis, which was highly suggestive of tuberculosis. Therefore, the patient was administered isoniazid, rifampicin, pyrazinamide, and ethambutol for 2 weeks. The CRP level was 5.6 mg/L. Thoracic spinal surgery using the anterior approach was performed (Figure 5). An intraoperative frozen section examination showed thoracic histoplasmosis infection (Figure 6). Routine postoperative pathology, and specific mycological stains, such as Giemsa, PAS, and periodic acid-silver methenamine, also confirmed thoracic histoplasmosis infection (Figure 7). The patient’s back pain was relieved. He was treated with itraconazole for 12 months. At a 26-month follow-up, the lesions had not progressed. The patient was pain-free and asymptomatic, and was able to return to his active lifestyle.
Figure 1.
(a) Anteroposterior and (b) lateral plain radiographs showing an osteolytic lesion with a pathological fracture in T5
Figure 2.
T5 (a) and T6 (b), and spinal sagittal plane (c) and coronal plane (d) CT scans show lytic lesions of the right side of T4, T5, and T6 vertebral bodies
Figure 3.
T1-weighted (a) and T2-weighted (b) MRI findings
MRI shows abnormal marrow signals (low signal on T1, high on T2 and STIR) in T4, T5, and T6 vertebral bodies. There is some compression of the T5 body and extension into the right pedicle, which mimics malignancy.
Figure 4.
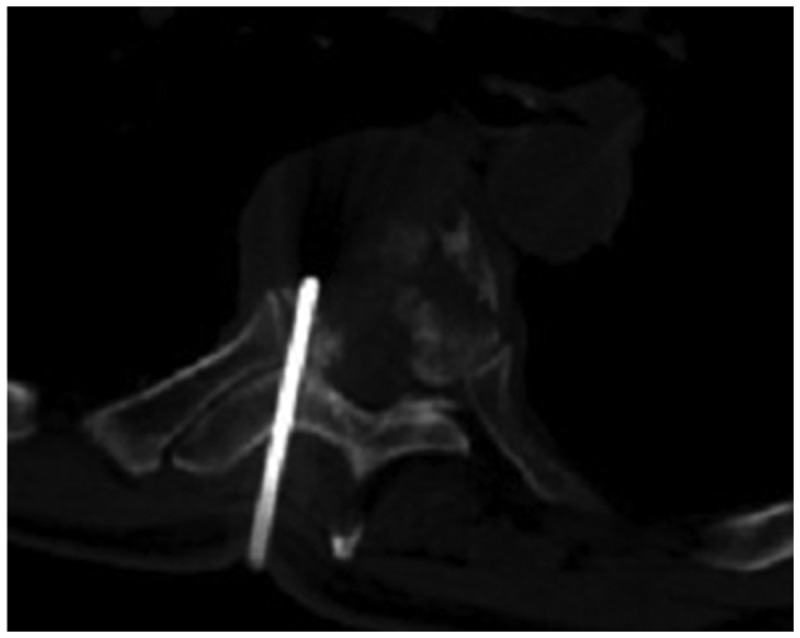
CT-guided transpedicular biopsy of T6
Figure 5.
(a) Anteroposterior and (b) lateral radiographs 26 months after surgery
The lesions have not progressed and the patient was asymptomatic.
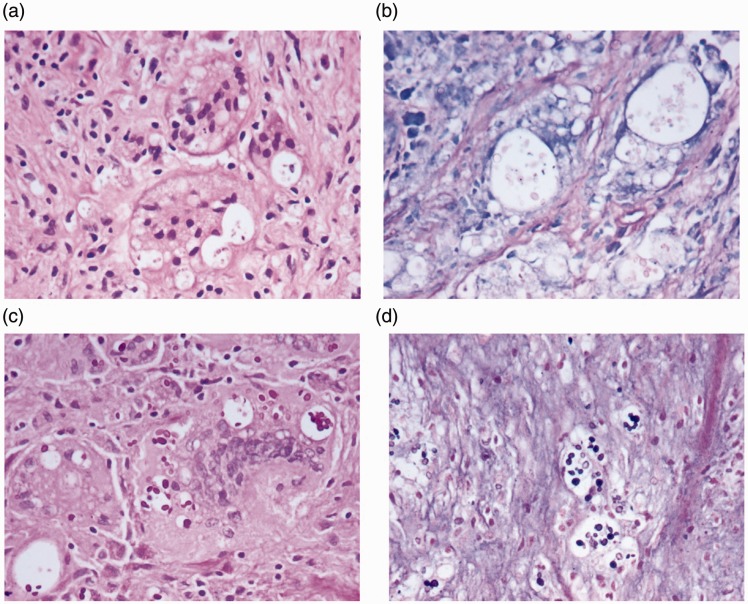
Figure 6.
(a) Histopathology from CT-guided transpedicular biopsy showing granulomatous inflammation with necrosis, tuberculosis. (b) An intraoperative frozen section examination and routine postoperative pathology show thoracic histoplasmosis infection.
Figure 7.
Mycological stains, including Giemsa, PAS, and periodic acid-silver methenamine, show thoracic histoplasmosis infection
Discussion
Histoplasmosis is caused by the reproductive spores of the fungus Histoplasma capsulatum, which is global, but is mainly concentrated in Central and North America. Immunocompetent infection with histoplasmosis is asymptomatic. Acute pulmonary histoplasmosis results in symptoms 8. Pulmonary infection is the main presentation of histoplasmosis 9. However, our case was a 65-year-old man who was immunocompetent and presented with no pulmonary disease. He had no symptoms of productive cough, weight loss, fever, or night sweats, but had spinal presentation of histoplasmosis mimicking a malignant tumour. His WBC count was normal, the CRP level was 63.0 mg/L, and a T-spot was negative. He was administered isoniazid, rifampicin, pyrazinamide, and ethambutol for 2 weeks, and then his CRP level was 5.6 mg/L.
Patients with histoplasmosis have been misdiagnosed as having a malignant tumour 10. On CT scans, as well as MRI or PET-CT, histoplasmosis can mimic malignant lesions. Our case appeared to have haematological malignancy, but a bone marrow biopsy was normal. We performed thoracic spinal surgery using the anterior approach because lesions appeared to be malignant. An intraoperative frozen section examination and routine postoperative pathology showed thoracic histoplasmosis infection. The infection did not progress and he had symptomatically improved at a follow-up of 26 months. Histoplasmosis was found to mimic tuberculosis spondylodiscitis in a patient with rheumatoid arthritis11, which can still simulate tuberculous spondylitis12. Therefore, histoplasmosis with tuberculosis and malignant lesions should be identified.
Diagnosis of histoplasmosis is based on culture of biological samples and detection of the fungus in lesions. Treatment of patients with histoplasmosis and severe acute/chronic respiratory or localized forms can be performed with intravenous or oral itraconazole 1.
In brief, histoplasmosis in the spine should be considered as a differential diagnosis of haematological malignancy and metastatic malignancy. Delaying treatment of this condition can result in severe manifestations.
Patient consent
The patient provided verbal consent.
Declaration of conflicting interest
The Authors declare that there is no conflict of interest.
Funding
The study was supported by a grant from the Medical Science and Technology Project of Zhejiang Province of China (2016KYA096 and 2017KY071) and Natural Science Funds of Zhejiang Province (Y17H160033).
References
- 1.Dall Bello AG, Severo CB, Guazzelli LS, et al. Histoplasmosis mimicking primary lung cancer or pulmonary metastases. J Bras Pneumol 2013; 39: 63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rimtepathip PP, Erickson A, Katner H, et al. Disseminated histoplasmosis presenting as pelvic inflammatory disease. Clin Case Rep 2015; 4: 76–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferreira MS, Borges AS. Histoplasmosis. Rev Soc Bras Med Trop 2009; 42: 192–198. [DOI] [PubMed] [Google Scholar]
- 4.Wheat LJ, Kauffman CA. Histoplasmosis. Infect Dis Clin North Am 2003; 17: 1–19. [DOI] [PubMed] [Google Scholar]
- 5.Mukhopadhyay S, Katzenstein AL. Biopsy findings in acute pulmonary histoplasmosis: unusual histologic features in 4 cases mimicking lymphomatoid granulomatosis. Am J Surg Pathol 2010; 34: 541–546. [DOI] [PubMed] [Google Scholar]
- 6.Paphitou NI, Barnett BJ. Solitary parietal lobe histoplasmoma mimicking a brain tumor. Scand J Infect Dis 2002; 34: 229–232. [DOI] [PubMed] [Google Scholar]
- 7.Rolston KV, Rodriguez S, Dholakia N, et al. Pulmonary infections mimicking cancer: a retrospective, three-year review. Support Care Cancer 1997; 5: 90–93. [DOI] [PubMed] [Google Scholar]
- 8.Goodwin RA, Jr, Shapiro JL, Thurman GH, et al. Disseminated histoplasmosis: clinical and pathologic correlations. Medicine (Baltimore) 1980; 59: 1–33. [PubMed] [Google Scholar]
- 9.Radhakrishnan S, Vanchilingam S, Subramaniam S, et al. Acute disseminated histoplasmosis with unusual features. An autopsy report. J Assoc Physicians India 1982; 30: 45–47. [PubMed] [Google Scholar]
- 10.McGraw EP, Kane JM, Kleiman MB, et al. Cervical abscess and mediastinal adenopathy: an unusual presentation of childhood histoplasmosis. Pediatr Radiol 2002; 32: 862–864. [DOI] [PubMed] [Google Scholar]
- 11.de Morais SS, Mafra Mde O, Canterle EM, et al. Histoplasmosis mimicking tuberculosis spondylodiscitis in a patient with rheumatoid arthritis. Acta Reumatol Port 2008; 33: 360–363. [PubMed] [Google Scholar]
- 12.Musoke F. Spinal African histoplasmosis simulating tuberculous spondylitis. Afr Health Sci 2001; 1: 28–29. [PMC free article] [PubMed] [Google Scholar]