Abstract
Background
Whole-lesion apparent diffusion coefficient (ADC) histogram analysis has been introduced and proved effective in assessment of multiple tumors. However, the application of whole-volume ADC histogram analysis in gastrointestinal tumors has just started and never been reported in T and N staging of gastric cancers.
Methods
Eighty patients with pathologically confirmed gastric carcinomas underwent diffusion weighted (DW) magnetic resonance imaging before surgery prospectively. Whole-lesion ADC histogram analysis was performed by two radiologists independently. The differences of ADC histogram parameters among different T and N stages were compared with independent-samples Kruskal-Wallis test. Receiver operating characteristic (ROC) analysis was performed to evaluate the performance of ADC histogram parameters in differentiating particular T or N stages of gastric cancers.
Results
There were significant differences of all the ADC histogram parameters for gastric cancers at different T (except ADCmin and ADCmax) and N (except ADCmax) stages. Most ADC histogram parameters differed significantly between T1 vs T3, T1 vs T4, T2 vs T4, N0 vs N1, N0 vs N3, and some parameters (ADC5%, ADC10%, ADCmin) differed significantly between N0 vs N2, N2 vs N3 (all P < 0.05). Most parameters except ADCmax performed well in differentiating different T and N stages of gastric cancers. Especially for identifying patients with and without lymph node metastasis, the ADC10% yielded the largest area under the ROC curve of 0.794 (95% confidence interval, 0.677–0.911). All the parameters except ADCmax showed excellent inter-observer agreement with intra-class correlation coefficients higher than 0.800.
Conclusion
Whole-volume ADC histogram parameters held great potential in differentiating different T and N stages of gastric cancers preoperatively.
Electronic supplementary material
The online version of this article (10.1186/s12885-017-3622-9) contains supplementary material, which is available to authorized users.
Keywords: Diffusion weighted magnetic resonance imaging, Stomach neoplasm, Histogram, Staging
Background
Gastric cancer is a common gastrointestinal malignancy, especially in eastern Asia [1]. Accurate preoperative staging is critical for treatment strategy optimization and prognosis prediction in patients with gastric cancers [2]. Since the performance of endoscopic ultrasonography (EUS), computed tomography (CT) or magnetic resonance (MR) imaging in T staging was fairly well, accurate preoperative N staging of gastric cancers appeared more challenging [3, 4].
Preoperative judgment of the nodular status is mainly based on the information obtained from the lymph nodes themselves, such as their size (longest or shortest diameter), shape, enhancement features, and the standard uptake values [5, 6]. And recent studies reported the value of diffusion weighted (DW) imaging in the assessment of lymph node metastasis [7, 8]. However, their diagnostic performance was usually unsatisfactory, especially for those lymph nodes too small to contain the region of interest (ROI) or even undetectable by imaging modalities.
Fortunately, the nodular status is closely involved with the intrinsic features of primary tumor lesions [9, 10]. For instance, tumors with poor differentiation degree or high T stage were at a higher risk of lymph nodes metastasis [9], but most of those features could only be obtained postoperatively. In recent years, some studies have reported that lymph nodes metastasis also correlated with the radiological characteristics of the primary tumors [11, 12]. For example, both Zhang XP et al. and Zhou ZG et al. demonstrated that models based on image indicators (such as tumor enhancement pattern, tumor maximum diameter and so on) from multi-detector CT imaging could help to diagnose lymph node metastasis in gastric cancers [11, 12]. In addition, our previous study found that a lower apparent diffusion coefficient (ADC) value of primary gastric cancer lesion tended to be complicated with lymph node metastasis [13]. However, only several parameters (ADCmean and ADCmin) obtained from one ROI at one slice of the lesion were used in most previous studies, which neglected the whole information as well as the heterogeneity of the tumors.
Recently, whole-lesion ADC histogram analysis has been introduced and proved effective in assessment of multiple tumors, such as prostate cancer, glioma, cervical cancer, et al. [14–18]. For instance, Donati OF et al. stated that whole-lesion ADC histogram parameters were significantly related to Gleason score of prostate cancer and the ADC10% performed better than ADCmean [14]. Suo ST et al. also reported that ADCmean and kurtosis derived from whole-volume ADC histogram analysis showed significant associations with pathologic T stage of bladder cancer [18].
The application of whole-volume ADC histogram analysis in gastrointestinal tumors has just started. For instance, our pilot study has demonstrated a significant association between whole-volume ADC histogram parameters and differentiation degree of gastric cancers [19]. To the best of our knowledge, the role of those parameters in T and N staging of gastric cancers has never been reported.
So, the purpose of this study was to explore the correlation between whole-volume ADC histogram parameters and T/N staging, and to establish their role in preoperative T and N staging of gastric cancers.
Methods
Patients
This prospective study was approved by the ethics committee of the Institutional Review Board of Nanjing Drum Tower Hospital, and written informed consent was obtained from all the patients.
From January 2012 to May 2015 patients with gastric cancers were consecutively included in this study. The inclusion criteria were: (1) with a diagnosis of gastric cancer confirmed by endoscopic biopsy; (2) willing to undergo MR examination for preoperative assessment; (3) without any local or systematic treatment before MR examination or surgery; (4) with definite information of postoperative pathologic T and N staging. The exclusion criteria were: (1) with absolute contraindications to MR examination, such as cardiac pacemaker or defibrillator, nerve stimulator, insulin pump, aneurysm clip, cochlear implant; (2) with a minimum diameter of tumor less than 5 mm insufficient to contain a ROI; (3) poor MR image quality for postprocessing due to motion or magnetic susceptibility artifacts. The flowchart of patient selection is shown in Fig. 1. A total of 80 patients were prospectively enrolled in this study. And the clinicopathological information of the cohort is shown in Table 1.
Fig. 1.
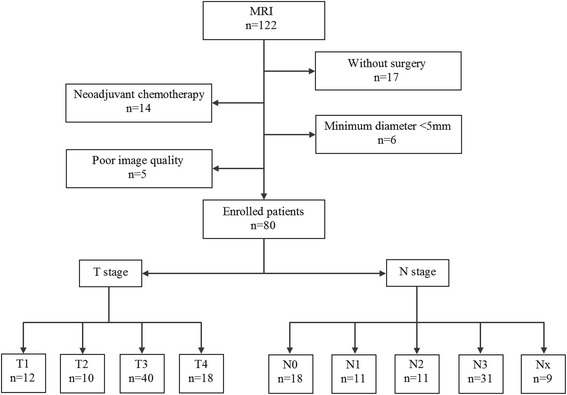
The flowchart of patient selection. Nx: 9 patients were categorized as Nx because they underwent palliative surgeries which could not completely meet the requirements for N staging
Table 1.
Clinicopathological information of the patient cohort
| Characteristics | No. of patients | Percentages (%) | |
|---|---|---|---|
| Gender | Male | 49 | 61.25 |
| Female | 31 | 38.75 | |
| Age | ≤60 | 38 | 47.50 |
| >60 | 42 | 52.50 | |
| Pathological types | Ade | 57 | 71.25 |
| Sig | 10 | 12.50 | |
| Mus | 1 | 1.25 | |
| Ade + sig | 6 | 7.50 | |
| Ade + mus | 3 | 3.75 | |
| Mus + sig | 2 | 2.50 | |
| Ade + sig + mus | 1 | 1.25 | |
| Location | Cardia | 26 | 32.50 |
| Body | 20 | 25.00 | |
| Antrum | 23 | 28.75 | |
| Cardia + body | 8 | 10.00 | |
| Body + antrum | 3 | 3.75 | |
ade adenocarcinoma, sig signet-ring cell carcinoma, mus mucinous adenocarcinoma
MR examination
Patients fasted for at least eight hours before MR examination to empty the gastrointestinal tract. To reduce gastrointestinal motility, 20 mg of scopolamine butyl bromide (1 ml: 20 mg; Chengdu NO.1 Drug Research Institute Company Limited, Chengdu, China) was injected intramuscularly 10 min before MR imaging for patients without contraindications, such as a history of glaucoma, prostate hypertrophy and severe heart disease. Sixty-one (76.3%) of 80 patients received scopolamine butylbromide (no side effects occurred during or after MR examination), and the remaining 19 (23.8%) patients had contraindications to the drug regime (15 patients) or rejected the drug (4 patients).Warm water (800–1000 mL) was orally administered within 5 min before MR imaging to fill the gastric cavity. And the patients were instructed to breathe normally before the MR examination.
MR examination was performed using a whole body 3.0 T scanner (Philips Medical Systems, Best, the Netherlands) with a phased-array 16-channel abdominal coil. The scan range was set from the diaphragmatic dome to the level of the renal hilum. Axial T2 weighted (T2 W) images were obtained with respiratory-triggered turbo spin-echo sequence without fat-saturation (repetition time msec/echo time msec, 1210–1220/70; matrix, 256 × 198; section thickness, 4 mm; gap, 1 mm; number of sections, 32–36; field of view, 36 cm; sensitivity encoding factor, 3.0; number of signal averaged, 1). Scan time of T2 W imaging was 1 min 36 s to 1 min 48 s.
T1 high resolution isotropic volume excitation (THRIVE) with spectral attenuated inversion recovery (SPAIR) techniques (repetition time msec/echo time msec, shortest/shortest; matrix, 256 × 198; section thickness, 4 mm; gap, 1 mm; number of sections, 32–36; field of view, 36 cm; number of signal averaged, 1) were utilized before and 30, 60, 90, and 180 s after administration of 0.2 mL per kilogram of body weight gadodiamide (Omniscan 0.5 mmol/mL; GE Healthcare, Ireland) using an automatic power injector (Medrad Spectris Solaris EP MR Injector System; One Medrad Drive Indianola, PA, US). Acquisition time of dynamic contrast enhancement MR imaging was 3 min 15 s to 3 min 17 s.
The parameters for DW imaging (a respiratory-triggered single-shot spin-echo echo-planar sequence) were as follows: b values, 0 and 1000 s/mm2; repetition time msec/echo time msec, 2280–3600/40–50; matrix, 236 × 186; section thickness, 4 mm; gap, 1 mm; direction of the motion-probing gradient, three orthogonal axes; field of view, 38 cm; number of sections, 32–36; number of signals averaged, 3; and scan time, 3 min 45 s to 4 min 24 s. All patients underwent MR scanning successfully without any side effects or discomfort.
Post processing
The DW images were transferred to a clinical workstation (Extended MR WorkSpace 2.6.3.4; Philips Medical Systems, Best, the Netherlands) and the corresponding ADC maps were generated automatically. Then two radiologists (X.X., X.X.) with 7 and 10 years’ experience in abdominal imaging, performed the whole-lesion ADC histogram analysis using our in-house software (Image analyzer 1.0, China) independently. Both of them were blinded to the pathologic staging information of the patients.
Before analysis, both DW images and the corresponding ADC maps were imported into our in-house software. The two radiologists were informed of the endoscopic findings including the general location of the lesion (such as the cardia, body and antrum). Gastric cancers presented as thickening of the gastric wall or a mass lesion with hyperintensity on the DW and T2 W images, as well as enhancement on the contrast enhanced T1 weighted images. ROIs were manually drawn on the DW images by the two radiologists independently with other MR sequences as references. The ROIs were drawn around the edge of the lesion including necrosis and hemorrhage within the tumor, carefully excluding adjacent water, air and motion artifacts, on each DW slice that showed the tumor lesion. Besides, the top and bottom slices were excluded to avoid the partial volume effects. The number of slices for drawing ROIs was 19 ± 10 (range, 2–26). And the tumor volume was 34,800.48 ± 28,636.28 mm3 (range, 362.55–130,552 mm3).
The ROIs drawn on DW images were automatically copied to exactly the same location of the corresponding ADC maps in real time.
After drawing all the ROIs covering the entire gastric lesion, the volume of interest (VOI) of the whole lesion was obtained, and then the ADC histogram with a set of parameters were calculated automatically. An example of DW image, ADC map and corresponding ADC histogram was shown in Fig. 2. A total of 9 parameters were generated: (1) ADCmean; (2) ADCmin; (3) ADCmax; (4–9) the 5th, 10th, 25th, 50th, 75th and 90th percentiles.
Fig. 2.
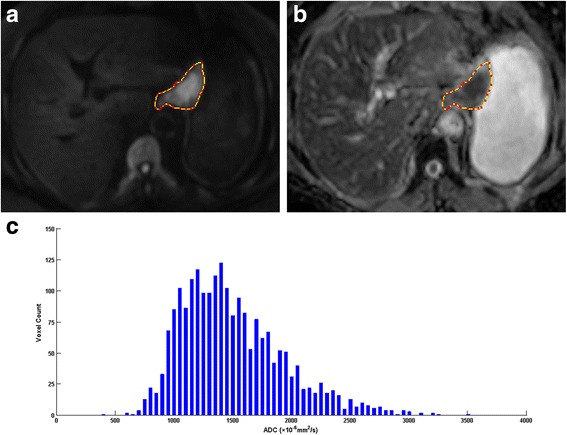
A 74-year-old woman with gastric carcinoma pathologically staged as T3N1cM0. a Axial diffusion weighted image (b = 1000 s/mm2) showed the lesion with high signal intensity in the lesser curvature of stomach; (b) The outline of the lesion was automatically copied to the same location of the apparent diffusion coefficient (ADC) map at the same level as (a); (c) The histogram of ADC map, with a bin size of 50 × 10−6 mm2/s: ADCmean* = 1520.76, ADCmin* = 437, ADCmax* = 3502, ADC5%* = 957, ADC10%* = 1025, ADC25%* = 1194, ADC50%* = 1443, ADC75%* = 1777, ADC90%* = 2110 (note: * The unit for ADC value is ×10−6 mm2/s)
Pathological T and N staging
Histopathological analysis of the resected specimens was performed by the pathologist (X. X.) with 6 years’ experience in gastrointestinal pathology, who was blinded to the MR findings. The T and N staging was diagnosed according to the seventh AJCC TNM classification (T1: Tumor invades lamina propria, muscularis mucosae, or submucosa; T2: Tumor invades muscularis propria; T3: Tumor penetrates subserosal connective tissue without invasion of visceral peritoneum or adjacent structures; T4: Tumor invades serosa (visceral peritoneum) or adjacent structures; N0: No regional lymph node metastasis; N1: Metastasis in 1 to 2 regional lymph nodes; N2: Metastasis in 3 to 6 regional lymph nodes; N3: Metastasis in 7 or more regional lymph nodes) [20]. Nine specimens from the palliative surgeries that did not completely meet the requirements for accurate N staging were only recorded as N+ or N- pathologically.
Statistical analyses
Shapiro-Wilk tests were used to check the normality assumption for all parameters in all groups. As some groups did not verify the normality assumption, quantitative data were presented as median (interquartile range), and the Kruskal-Wallis test was used to detect the difference of ADC histogram parameter distributions among different T and N stages. A full pairwise comparison of ADC histogram parameters using Mann-Whitney U test at each individual T and N level was performed. Receiver operating characteristic (ROC) analysis was performed to evaluate the performance of ADC histogram parameters in differentiating certain T or N stages of gastric cancers. The intra-class correlation coefficient (ICC) was calculated to evaluate the inter-observer agreement in the measurement of ADC histogram parameters (0.000–0.200 poor, 0.201–0.400 fair, 0.401–0.600 moderate, 0.601–0.800 good, 0.801–1.000 excellent). Statistical analyses were performed with SPSS (version 22.0 for Microsoft Windows ×64, SPSS, Chicago, US). A two-tailed P value less than 0.05 was considered statistically significant.
Results
Independent-samples Kruskal-Wallis test
The results of Shapiro-Wilk tests of normality for all the parameters in every group are shown in Additional file 1: Table S1. The parameters ADCmax in T3 group, ADCmin in N0 group, ADC5% and ADC10% in N2 group did not verify normality assumption, so we chose to present all the parameters as median (interquartile range) and use the independent-samples Kruskal-Wallis test for evaluating differences of all the parameters among different T and N stages. According to independent-samples Kruskal-Wallis test, parameters ADCmean, ADC5%, ADC10%, ADC25%, ADC50%, ADC75% and ADC90% showed significant differences in gastric cancers with different T stages (P = 0.001, 0.008, 0.002, <0.001, <0.001, 0.002 and 0.010, respectively) while parameters ADCmean, ADCmin, ADC5%, ADC10%, ADC25%, ADC50%, ADC75% and ADC90% showed significant differences in gastric cancers with different N stages (P = 0.007, 0.005, 0.006, 0.004, 0.004, 0.005, 0.013 and 0.023, respectively) (Table 2).
Table 2.
ADC histogram parameters for differentiating different T and N stages of gastric cancers
| n | ADCmean | ADCmin | ADCmax | ADC5% | ADC10% | ADC25% | ADC50% | ADC75% | ADC90% | |
|---|---|---|---|---|---|---|---|---|---|---|
| T1 | 12 | 1804.56 (331.03) | 804.00 (541.00) | 3291.00 (976.00) | 1309.50 (337.25) | 1428.00 (405.00) | 1586.50 (397.50) | 1769.50 (376.50) | 1985.50 (375.50) | 2297.00 (352.25) |
| T2 | 10 | 1736.87 (334.60) | 545.00 (492.00) | 3198.50 (328.00) | 1086.50 (468.25) | 1285.00 (355.50) | 1527.00 (286.00) | 1735.00 (374.50) | 1970.00 (380.00) | 2179.50 (363.25) |
| T3 | 40 | 1569.38 (445.54) | 451.00 (386.75) | 3514.50 (553.75) | 1038.00 (315.50) | 1123.00 (365.25) | 1307.00 (409.25) | 1549.50 (467.50) | 1775.00 (478.00) | 2053.00 (561.75) |
| T4 | 18 | 1486.67 (206.90) | 493.00 (239.50) | 3505.50 (857.50) | 998.00 (221.00) | 1061.50 (219.00) | 1199.50 (178.25) | 1389.00 (176.50) | 1657.50 (248.75) | 2027.50 (286.75) |
| P | 0.001* | 0.069 | 0.466 | 0.008* | 0.002* | <0.001* | <0.001* | 0.002* | 0.010* | |
| N0 | 18 | 1856.23 (312.81) | 750.00 (396.75) | 3195.00 (536.75) | 1301.50 (308.25) | 1428.50 (290.00) | 1620.50 (285.75) | 1818.50 (347.75) | 2060.50 (354.50) | 2261.50 (328.00) |
| N1 | 11 | 1566.30 (483.09) | 512.00 (275.00) | 3502.00 (762.00) | 957.00 (488.00) | 1028.00 (554.00) | 1257.00 (592.00) | 1596.00 (566.00) | 1823.00 (488.00) | 2066.00 (446.00) |
| N2 | 11 | 1660.12 (346.68) | 568.00 (353.00) | 3609.00 (815.00) | 1018.00 (160.00) | 1142.00 (177.00) | 1366.00 (174.00) | 1605.00 (375.00) | 1947.00 (470.00) | 2141.00 (542.00) |
| N3 | 31 | 1552.96 (326.16) | 382.00 (425.00) | 3463.00 (449.00) | 1026.00 (308.00) | 1117.00 (328.00) | 1271.00 (313.00) | 1494.00 (321.00) | 1759.00 (378.00) | 2074.00 (430.00) |
| Nx | 9 | 1489.73 (216.96) | 391.00 (336.50) | 3548.00 (932.00) | 991.00 (233.00) | 1054.00 (223.50) | 1179.00 (189.50) | 1379.00 (219.50) | 1652.00 (227.00) | 2017.00 (246.00) |
| P† | 0.007* | 0.005* | 0.277 | 0.006* | 0.004* | 0.004* | 0.005* | 0.013* | 0.023* |
ADC apparent diffusion coefficient; Nx: 9 patients were categorized as Nx because they underwent palliative surgeries which could not completely meet the requirements for N staging
The values of the ADC parameters were presented as median (interquartile range)
*: P < 0.05 (independent-samples Kruskal-Wallis test)
†: The independent-samples Kruskal-Wallis test for N staging didn’t include those 9 patients who were categorized as Nx
Pairwise comparison
Most ADC histogram parameters differed significantly between T1 vs T3, T1 vs T4, T2 vs T4, N0 vs N1, N0 vs N3 (all P < 0.05), and some parameters (ADC5%, ADC10%, ADCmin) differed significantly between N0 vs N2, N2 vs N3 (Table 3).
Table 3.
Pairwise comparison of ADC histogram parameters at each individual T and N level
| Parameters | T1 vs T2 | T1 vs T3 | T1 vs T4 | T2 vs T3 | T2 vs T4 | T3 vs T4 | N0 vs N1 | N0 vs N2 | N0 vs N3 | N1 vs N2 | N1 vs N3 | N2 vs N3 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ADCmean | 0.821 | 0.021* | < 0.001* | 0.097 | 0.001* | 0.107 | 0.035* | 0.112 | 0.001* | 0.478 | 0.822 | 0.110 |
| ADCmin | 0.314 | 0.015* | 0.017* | 0.369 | 0.436 | 0.960 | 0.068 | 0.674 | 0.001* | 0.332 | 0.211 | 0.024* |
| ADCmax | 0.872 | 0.385 | 0.267 | 0.264 | 0.245 | 0.579 | 0.412 | 0.159 | 0.054 | 0.652 | 0.866 | 0.714 |
| ADC5% | 0.314 | 0.007* | < 0.001* | 0.369 | 0.121 | 0.257 | 0.035* | 0.012* | 0.001* | 0.519 | 0.844 | 0.429 |
| ADC10% | 0.456 | 0.007* | < 0.001* | 0.102 | 0.014* | 0.171 | 0.016* | 0.014* | 0.001* | 0.243 | 1.000 | 0.445 |
| ADC25% | 0.722 | 0.010* | < 0.001* | 0.063 | 0.001* | 0.088 | 0.016* | 0.055 | 0.001* | 0.365 | 0.955 | 0.163 |
| ADC50% | 0.974 | 0.019* | < 0.001* | 0.059 | 0.001* | 0.053 | 0.024* | 0.146 | 0.001* | 0.438 | 0.866 | 0.081 |
| ADC75% | 1.000 | 0.039* | < 0.001* | 0.092 | 0.001* | 0.118 | 0.035* | 0.387 | 0.002* | 0.332 | 0.672 | 0.104 |
| ADC90% | 0.456 | 0.035* | 0.001* | 0.138 | 0.010* | 0.290 | 0.028* | 0.438 | 0.004* | 0.270 | 0.955 | 0.172 |
ADC apparent diffusion coefficient; *: P < 0.05 with Mann-Whitney U test
ROC curve analysis
Most ADC histogram parameters except ADCmax performed well in differentiating different T and N stages of gastric cancers (Table 4).
Table 4.
The performance of histogram parameters for differentiating different T and N stages of gastric cancers
| Parameters | T1 vs T2 + 3 + 4 | T1 + 2 vs T3 + 4 | T1 + 2 + 3 vs T4 | N0 vs N1 + 2 + 3 | N0 + 1 vs N2 + 3 | N0 + 1 + 2 vs N3 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AUC | 95% CI | AUC | 95% CI | AUC | 95% CI | AUC | 95% CI | AUC | 95% CI | AUC | 95% CI | |
| ADCmean | 0.740 | 0.608–0.872 | 0.755 | 0.642–0.869 | 0.721 | 0.610–0.833 | 0.752 | 0.626–0.877 | 0.656 | 0.522–0.790 | 0.679 | 0.551–0.807 |
| ADCmin | 0.725 | 0.564–0.887 | 0.674 | 0.535–0.814 | 0.568 | 0.430–0.706 | 0.716 | 0.591–0.842 | 0.660 | 0.533–0.787 | 0.725 | 0.602–0.848 |
| ADCmax | 0.578 | 0.374–0.783 | 0.609 | 0.466–0.752 | 0.576 | 0.415–0.737 | 0.349 | 0.512–0.790 | 0.614 | 0.478–0.749 | 0.569 | 0.435–0.704 |
| ADC5% | 0.769 | 0.622–0.916 | 0.715 | 0.582–0.848 | 0.661 | 0.538–0.784 | 0.773 | 0.649–0.897 | 0.673 | 0.539–0.808 | 0.657 | 0.527–0.786 |
| ADC10% | 0.771 | 0.636–0.906 | 0.757 | 0.639–0.876 | 0.694 | 0.577–0.811 | 0.781 | 0.660–0.902 | 0.662 | 0.526–0.798 | 0.652 | 0.524–0.781 |
| ADC25% | 0.765 | 0.637–0.892 | 0.776 | 0.665–0.887 | 0.731 | 0.620–0.841 | 0.773 | 0.648–0.897 | 0.656 | 0.520–0.793 | 0.671 | 0.544–0.797 |
| ADC50% | 0.747 | 0.625–0.869 | 0.771 | 0.662–0.881 | 0.746 | 0.639–0.854 | 0.755 | 0.633–0.877 | 0.654 | 0.520–0.788 | 0.684 | 0.556–0.812 |
| ADC75% | 0.719 | 0.586–0.853 | 0.747 | 0.634–0.860 | 0.718 | 0.604–0.831 | 0.725 | 0.598–0.852 | 0.638 | 0.505–0.771 | 0.678 | 0.550–0.806 |
| ADC90% | 0.724 | 0.585–0.863 | 0.724 | 0.609–0.840 | 0.670 | 0.548–0.793 | 0.715 | 0.586–0.844 | 0.616 | 0.482–0.749 | 0.652 | 0.522–0.783 |
ADC apparent diffusion coefficient, AUC area under the receiver operating characteristic curve, CI confidence interval
Especially for differentiating patients with and without lymph node metastasis, the ADC10% yielded the largest area under the curve (AUC) value of 0.794 (Table 5 and Fig. 3, panels a, b and c).
Table 5.
The performance of ADC histogram parameters for differentiating patients with and without lymph node metastasis
| Parameters | Cutoff valuea | Sensitivity | Specificity | Accuracy | AUC | 95% CI |
|---|---|---|---|---|---|---|
| ADCmean | 1666.25 | 0.778 | 0.710 | 0.763 | 0.772 | 0.652–0.891 |
| ADCmin | 649.50 | 0.667 | 0.742 | 0.684 | 0.737 | 0.618–0.856 |
| ADCmax | 3531.00 | 0.484 | 0.833 | 0.563 | 0.656 | 0.523–0.789 |
| ADC5% | 1213.50 | 0.722 | 0.839 | 0.748 | 0.785 | 0.663–0.907 |
| ADC10% | 1293.00 | 0.722 | 0.806 | 0.741 | 0.794 | 0.677–0.911 |
| ADC25% | 1424.50 | 0.778 | 0.258 | 0.661 | 0.791 | 0.673–0.909 |
| ADC50% | 1539.00 | 0.889 | 0.597 | 0.823 | 0.776 | 0.662–0.891 |
| ADC75% | 1842.50 | 0.778 | 0.661 | 0.752 | 0.747 | 0.627–0.867 |
| ADC90% | 2171.50 | 0.778 | 0.710 | 0.763 | 0.732 | 0.606–0.858 |
ADC apparent diffusion coefficient, AUC area under the receiver operating characteristic curve
athe cutoff values of the ADC histogram parameters were calculated by using the Youden index; CI, confidence interval
Fig. 3.
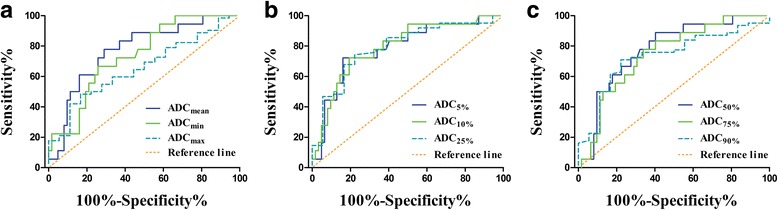
Receiver operating characteristic curves of histogram parameters for differentiating patients with and without lymph node metastasis. a The area under the curve (AUC) values of the parameters ADCmean, ADCmin and ADCmax were 0.772, 0.737 and 0.656, respectively; (b) The AUC values of the parameters ADC5%, ADC10% and ADC25% were 0.785, 0.794 and 0.791, respectively; (c) The AUC values of the parameters ADC50%, ADC75% and ADC90% were 0.776, 0.747 and 0.732, respectively
Inter-observer agreement
All the ADC histogram parameters except ADCmax showed excellent inter-observer agreement with ICCs higher than 0.800 (Table 6).
Table 6.
The inter-observer variability for the measurement of ADC histogram parameters
| Parameters | ICC (95% CI) |
|---|---|
| ADCmean | 0.980 (0.970–0.987) |
| ADCmin | 0.820 (0.733–0.881) |
| ADCmax | 0.641 (0.491–0.754) |
| ADC5% | 0.971 (0.955–0.981) |
| ADC10% | 0.989 (0.982–0.993) |
| ADC25% | 0.990 (0.985–0.994) |
| ADC50% | 0.990 (0.984–0.993) |
| ADC75% | 0.976 (0.962–0.984) |
| ADC90% | 0.929 (0.891–0.954) |
ADC apparent diffusion coefficient, ICC intra-class correlation coefficient, CI confidence interval
Discussion
Our study demonstrated that multiple whole-volume ADC histogram parameters differed significantly among gastric cancers at different T or N stages, which has never been reported previously.
The ADC histogram parameters in this study were derived from the whole volume of the lesion, which avoided the sampling error of drawing an ROI within the tumor. All the parameters showed significant differences in different T stages of gastric cancers except ADCmin and ADCmax, which was susceptible to extreme values caused by certain components (such as hemorrhage) or invisible artifacts within the tumor.
Different percentiles reflected certain features of different components of the whole lesion. Generally speaking, lower percentiles corresponded to the most solid, condense and malignant components, while higher percentiles represented as somewhat loose, cystic or necrotic tissues. As the tumor progresses in terms of T staging, it appears more malignant with higher cellular density, larger nucleus and more disordered arrangement, leading to greater limitation to the water molecular diffusion and resulting in lower ADC values. Therefore, gastric cancers at higher T stages showed lower values of ADC percentiles than those at lower T stages. Unsurprisingly, lower percentiles (such as 25th) showed more significant differences among different T stages of gastric cancers compared with ADCmean and higher percentiles. Nevertheless, other pathologic features including histological types, differentiation degrees and Lauren classification might have some influence on the results, which required more investigation.
Gastric cancers with different T stages need different treatment methods [21, 22]. However, it was extremely difficult for conventional CT or MR imaging to distinguish gastric cancers with or without muscular invasion (T1 vs. ≥ T2) [3, 7]. Fortunately, we found that all the ADC histogram parameters except ADCmax performed well in differentiating T1 from ≥ T2 (AUC, 0.719–0.771) especially ADC10% (AUC = 0.771), and differentiating ≤ T2 from ≥ T3 (AUC, 0.674–0.776) especially ADC25% (AUC = 0.776).
Furthermore, multiple ADC histogram parameters differed significantly between N0 vs N1, N0 vs N2, N0 vs N3, N2 vs N3, which suggested a negative relationship between ADC histogram parameters and N stage. Lymph node metastasis is a complex biological process involving multiple factors, among which the features of primary tumor undoubtedly play a critical role in this event [9, 23]. Different components within the primary tumor hold different metastatic potentials to lymph nodes. Based on our findings, the lower ADC percentiles, which corresponded to more malignant components, showed closer correlations with N staging compared with higher percentiles.
The lower ADC percentiles performed well in differentiating gastric cancer patients with and without lymph node metastasis. Especially the parameter ADC10% showed a sensitivity of 72.2% and a specificity of 80.6%, which was even higher than multiple indexes from lymph node itself in previous studies. For instance, Fairweather M. et al. reported an accuracy of 42.9% and 56.0% with endoscopic ultrasonography and CT for evaluating the nodal status in gastric cancers, respectively [24]. Maccioni F. et al. reported an accuracy of 68% with MR imaging in N staging of gastric cancers [3]. Nevertheless, lymph node metastasis is a complicated process influenced by multiple factors, so we will integrate more comprehensive factors in order to make a more accurate prediction in our future work.
Our study had several limitations. Firstly, the ROIs were manually drawn by the radiologists without rigorous reference to pathologic findings. However, consistency analysis showed that all the parameters, except ADCmax (ICC = 0.641), had excellent inter-observer repeatability with ICCs ranging from 0.820 to 0.990 and up to 7 parameters achieved ICCs over 0.900. Secondly, we did not perform DW imaging scan-rescan reproducibility analysis on histogram parameters due to some practical difficulties. Thirdly, we did not explore the correlation between histogram parameters with M staging, because this study took postoperative pathologic findings as the reference while most patients at M1 stage had lost the opportunity of surgery. All those issues required further research.
Conclusions
In conclusion, we successfully detected significant differences of whole-volume ADC histogram parameters among gastric cancers at different T or N stages and explored their potential in differentiating specific T and N stages of gastric cancers, which might improve preoperative assessment and optimize treatment planning for those patients.
Additional files
The P values of ADC parameters in every group for Shapiro-Wilk tests of normality. (DOC 35 kb)
The values of ADC parameters and T/N stages of each patient. (XLS 25 kb)
Acknowledgements
Not applicable.
Funding
National Health and Family Planning Commission of China (W201306), National Natural Science Foundation of China (81,371,516, 81,501,441 and 81,601,463), Natural Science Foundation of Jiangsu Province (BK20150109), Research Project of Health and Family Planning Commission of Jiangsu Province (Q201508), Key Project supported by Medical Science and technology development Foundation, Nanjing Department of Health (YKK15067) and Six Talent Peaks Project of Jiangsu Province (2015-WSN-079). The funding sources had no role in the study design, data collection, data analysis, or interpretation of the findings.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its Additional file 2: Supplementary Data].
Abbreviations
- ADC
Apparent diffusion coefficient
- AUC
Area under the curve
- CT
Computed tomography
- DW
Diffusion weighted
- EUS
Endoscopic ultrasonography
- ICC
Intra-class correlation coefficient
- MR
Magnetic resonance
- ROC
Receiver operating characteristic
- ROI
Region of interest
- SPAIR
Spectral attenuated inversion recovery
- T2 W
T2 weighted
- THRIVE
T1 high resolution isotropic volume excitation
Authors’ contributions
SL, YJZ, YunG, ZYZ and JH made substantial contributions to conception and design; SL, YJZ, YueG, WXG and LC made substantial contributions to acquisition of data; LC was the histopathologist responsible for all histopathological support; ZYZ and JH made substantial contributions to analysis and interpretation of data; SL and YJZ drafted the manuscript; YueG, LC, WXG, YunG, ZYZ and JH revised it critically for important intellectual content. All authors read and approved the final manuscript to be published. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics approval and consent to participate
This prospective study was approved by the ethics committee of the Institutional Review Board of Nanjing Drum Tower Hospital, and all the patients offered the written informed consents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12885-017-3622-9) contains supplementary material, which is available to authorized users.
Contributor Information
Song Liu, Email: liusongnj@126.com.
Yujuan Zhang, Email: shujuankathy@163.com.
Ling Chen, Email: lingpathol@126.com.
Wenxian Guan, Email: wenxianguan123@126.com.
Yue Guan, Email: gyuenju@126.com.
Yun Ge, Email: geyun@nju.edu.cn.
Jian He, Email: hjxueren@126.com.
Zhengyang Zhou, Email: zyzhou@nju.edu.cn.
References
- 1.Hartgrink HH, Jansen EP, van Grieken NC, van de Velde CJ. Gastric cancer. Lancet (London, England) 2009;374(9688):477–490. doi: 10.1016/S0140-6736(09)60617-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rocken C, Behrens HM. Validating the prognostic and discriminating value of the TNM-classification for gastric cancer - a critical appraisal. Eur J Cancer. 2015;51(5):577–586. doi: 10.1016/j.ejca.2015.01.055. [DOI] [PubMed] [Google Scholar]
- 3.Maccioni F, Marcelli G, Al Ansari N, Zippi M, De Marco V, Kagarmanova A, Vestri A, Marcheggiano-Clarke L, Marini M. Preoperative T and N staging of gastric cancer: magnetic resonance imaging (MRI) versus multi detector computed tomography (MDCT) Clin Ter. 2010;161(2):e57–e62. [PubMed] [Google Scholar]
- 4.Cardoso R, Coburn N, Seevaratnam R, Sutradhar R, Lourenco LG, Mahar A, Law C, Yong E, Tinmouth J. A systematic review and meta-analysis of the utility of EUS for preoperative staging for gastric cancer. Gastric Cancer. 2012;15(Suppl 1):S19–S26. doi: 10.1007/s10120-011-0115-4. [DOI] [PubMed] [Google Scholar]
- 5.Monig SP, Schroder W, Baldus SE, Holscher AH. Preoperative lymph-node staging in gastrointestinal cancer--correlation between size and tumor stage. Onkologie. 2002;25(4):342–344. doi: 10.1159/000066051. [DOI] [PubMed] [Google Scholar]
- 6.Saito T, Kurokawa Y, Takiguchi S, Miyazaki Y, Takahashi T, Yamasaki M, Miyata H, Nakajima K, Mori M, Doki Y. Accuracy of multidetector-row CT in diagnosing lymph node metastasis in patients with gastric cancer. Eur Radiol. 2015;25(2):368–374. doi: 10.1007/s00330-014-3373-9. [DOI] [PubMed] [Google Scholar]
- 7.Joo I, Lee JM, Kim JH, Shin CI, Han JK, Choi BI. Prospective comparison of 3T MRI with diffusion-weighted imaging and MDCT for the preoperative TNM staging of gastric cancer. J Magn Reson Imaging. 2015;41(3):814–821. doi: 10.1002/jmri.24586. [DOI] [PubMed] [Google Scholar]
- 8.Mizukami Y, Ueda S, Mizumoto A, Sasada T, Okumura R, Kohno S, Takabayashi A. Diffusion-weighted magnetic resonance imaging for detecting lymph node metastasis of rectal cancer. World J Surg. 2011;35(4):895–899. doi: 10.1007/s00268-011-0986-x. [DOI] [PubMed] [Google Scholar]
- 9.Xu YY, Huang BJ, Sun Z, Lu C, Liu YP. Risk factors for lymph node metastasis and evaluation of reasonable surgery for early gastric cancer. World J Gastroenterol. 2007;13(38):5133–5138. doi: 10.3748/wjg.v13.i38.5133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merkow RP, Bilimoria KY, Keswani RN, Chung J, Sherman KL, Knab LM, Posner MC, Bentrem DJ: Treatment trends, risk of lymph node metastasis, and outcomes for localized esophageal cancer. J Natl Cancer Inst. 2014;106(7):dju133. [DOI] [PubMed]
- 11.Zhou ZG, Liu F, Jiao LC, Wang ZL, Zhang XP, Wang XD, Luo XZ. An evidential reasoning based model for diagnosis of lymph node metastasis in gastric cancer. BMC Med Inform Decis Mak. 2013;13:123. doi: 10.1186/1472-6947-13-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang XP, Wang ZL, Tang L, Sun YS, Cao K, Gao Y. Support vector machine model for diagnosis of lymph node metastasis in gastric cancer with multidetector computed tomography: a preliminary study. BMC Cancer. 2011;11:10. doi: 10.1186/1471-2407-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu S, Wang H, Guan W, Pan L, Zhou Z, Yu H, Liu T, Yang X, He J, Zhou Z. Preoperative apparent diffusion coefficient value of gastric cancer by diffusion-weighted imaging: correlations with postoperative TNM staging. J Magn Reson Imaging. 2015;42(3):837–843. doi: 10.1002/jmri.24841. [DOI] [PubMed] [Google Scholar]
- 14.Donati OF, Mazaheri Y, Afaq A, Vargas HA, Zheng J, Moskowitz CS, Hricak H, Akin O. Prostate cancer aggressiveness: assessment with whole-lesion histogram analysis of the apparent diffusion coefficient. Radiology. 2014;271(1):143–152. doi: 10.1148/radiol.13130973. [DOI] [PubMed] [Google Scholar]
- 15.Wu CJ, Wang Q, Li H, Wang XN, Liu XS, Shi HB, Zhang YD. DWI-associated entire-tumor histogram analysis for the differentiation of low-grade prostate cancer from intermediate-high-grade prostate cancer. Abdom Imaging. 2015;40(8):3214–3221. doi: 10.1007/s00261-015-0499-4. [DOI] [PubMed] [Google Scholar]
- 16.Ryu YJ, Choi SH, Park SJ, Yun TJ, Kim JH, Sohn CH. Glioma: application of whole-tumor texture analysis of diffusion-weighted imaging for the evaluation of tumor heterogeneity. PLoS One. 2014;9(9):e108335. doi: 10.1371/journal.pone.0108335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Downey K, Riches SF, Morgan VA, Giles SL, Attygalle AD, Ind TE, Barton DP, Shepherd JH, deSouza NM. Relationship between imaging biomarkers of stage I cervical cancer and poor-prognosis histologic features: quantitative histogram analysis of diffusion-weighted MR images. AJR Am J Roentgenol. 2013;200(2):314–320. doi: 10.2214/AJR.12.9545. [DOI] [PubMed] [Google Scholar]
- 18.Suo ST, Chen XX, Fan Y, Wu LM, Yao QY, Cao MQ, Liu Q, Xu JR. Histogram analysis of apparent diffusion coefficient at 3.0 T in urinary bladder lesions: correlation with pathologic findings. Acad Radiol. 2014;21(8):1027–1034. doi: 10.1016/j.acra.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 19.Zhang Y, Chen J, Liu S, Shi H, Guan W, Ji C, Guo T, Zheng H, Guan Y, Ge Y et al: Assessment of histological differentiation in gastric cancers using whole-volume histogram analysis of apparent diffusion coefficient maps. J Magn Reson Imaging. 2017;45(2):440–9. [DOI] [PubMed]
- 20.Jung H, Lee HH, Song KY, Jeon HM, Park CH. Validation of the seventh edition of the American joint committee on cancer TNM staging system for gastric cancer. Cancer. 2011;117(11):2371–2378. doi: 10.1002/cncr.25778. [DOI] [PubMed] [Google Scholar]
- 21.Zali H, Rezaei-Tavirani M, Azodi M. Gastric cancer: prevention, risk factors and treatment. Gastroenterol Hepatol From Bed Bench. 2011;4(4):175–185. [PMC free article] [PubMed] [Google Scholar]
- 22.Digklia A, Wagner AD. Advanced gastric cancer: current treatment landscape and future perspectives. World J Gastroenterol. 2016;22(8):2403–2414. doi: 10.3748/wjg.v22.i8.2403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jin EH, Lee DH, Jung SA, Shim KN, Seo JY, Kim N, Shin CM, Yoon H, Jung HC. Clinicopathologic factors and molecular markers related to lymph node metastasis in early gastric cancer. World J Gastroenterol. 2015;21(2):571–577. doi: 10.3748/wjg.v21.i2.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fairweather M, Jajoo K, Sainani N, Bertagnolli MM, Wang J. Accuracy of EUS and CT imaging in preoperative gastric cancer staging. J Surg Oncol. 2015;111(8):1016–1020. doi: 10.1002/jso.23919. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The P values of ADC parameters in every group for Shapiro-Wilk tests of normality. (DOC 35 kb)
The values of ADC parameters and T/N stages of each patient. (XLS 25 kb)
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its Additional file 2: Supplementary Data].


