Abstract
Adolescents with ADHD demonstrate notoriously poor treatment utilization. Barriers to access have been partially addressed through tailored therapy content and therapist delivery style; yet, additional challenges to engaging this population remain. To leverage modern technology in support of this aim, the current study investigates parent-teen therapy for ADHD delivered over a videoconferencing format. In this preliminary feasibility study, teens and parents (N=20) received an empirically supported dyadic therapy that incorporates skills-based modules with motivational interviewing. The videoconferencing interface was deemed feasible with nearly all families completing treatment. Acceptable therapeutic alliance was reported and key mechanisms of change were engaged (i.e., adolescent motivation to meet goals, parent strategy implementation). Families reported high satisfaction, despite minor disturbances associated with delivering therapy via videoconferencing. Treatment integrity and fidelity were acceptable, though slightly reduced compared to clinic-based trials of the same protocol. Therapists perceived that videoconferencing enhanced treatment for 50% of families. Reductions in participant ADHD symptoms and organization, time management, and planning problems from baseline to post-treatment were noted by parents and teachers. However, open trial results of this study should be interpreted with caution due to their uncontrolled and preliminary nature.
Keywords: ADHD, Adolescence, Family Therapy, Technology Interventions
Attention Deficit/Hyperactivity Disorder (ADHD) is a psychiatric disorder characterized by impairing levels of inattention, overactivity, and poor impulse control, and it affects 5–10% of individuals (Centers for Disease Control and Prevention, 2013). Though historically characterized as a childhood disorder, it is now accepted that ADHD continues to afflict adolescents and adults (Molina et al., 2009) and is associated with very negative outcomes by adulthood (e.g., high school dropout, lower rates of college matriculation, interpersonal difficulties, drug abuse, vocational underachievement; Barkley, Murphy, & Fischer, 2008; Kuriyan et al., 2013). Among these concerns, secondary school academic impairment is particularly troubling because it often catalyzes additional risks (Kuriyan et al., 2013; Molina et al., 2012) and creates a high societal burden (Robb et al., 2012), making it a key target for treatment. For example, compared to typically developing peers, adolescents with ADHD perform more poorly on standardized achievement tests (Barkley, Anastopoulos, Guevremont, & Fletcher, 1991; Fischer, Barkley, Edelbrock, & Smallish, 1990), complete fewer assignments (Barkley et al., 1991; Kent et al., 2011; Weiss & Hechtman, 1993), and receive poorer course grades (Barkley, Fischer, Smallish, & Fletcher, 2006; Kent et al., 2011). Such findings highlight the critical need for effective and accessible ADHD treatments to ameliorate the disorder’s negative impacts on adolescents and their families.
Treating ADHD in Adolescence
Central nervous system stimulant medications, behavioral interventions, and their combination are the most efficacious and recommended treatments for ADHD in childhood (American Academy of Pediatrics, 2011). However, longitudinal data indicate that receiving treatment for ADHD in childhood does not prevent long-term negative outcomes in late adolescence and adulthood (Biederman et al., 2008; Molina et al., 2009; Mannuzza, Klein, & Moulton, 2008). Poor long-term efficacy of child ADHD treatments underscores the need for continued ADHD treatment into adolescence (Molina et al., 2009; Wolraich et al., 2005) as well as empirically supported treatments that target mechanisms of long-term success (i.e., academic performance, family functioning). Yet, a majority of teens with ADHD do not receive interventions for their symptoms. For example, in the Pittsburgh ADHD Longitudinal Study, most participants with childhood ADHD (80%) did not receive treatment for ADHD past age twelve, even though most displayed substantial impairment across several domains (Kent et al., 2011; Molina et al., 2009; Wolraich et al., 2005). Similarly longitudinal work by Bussing et al. (2011) indicated that a majority of impaired adolescents with ADHD (58%) had not received mental health services in the past year.
There are several reasons for poor treatment utilization in this population. With respect to medication, most teens who were medicated in childhood eventually ask to desist—disliking side effects or perceiving themselves as insufficiently impaired to warrant medication (Biswas, Gnagy, Molina, & Pelham, 2009). Psychosocial interventions for teens with ADHD have been developed for delivery in schools and clinics (Sibley, Kuriyan, Evans, Waxmonsky, & Smith, 2014). However, these services are not widely offered in public schools due to resource barriers (Fabiano et al., 2002) and are poorly accessed in community clinics due to engagement problems (Bussing et al., 2011). These engagement problems may be a result of several factors. First, some parents possess an interfering belief that forcing uninterested teens to come to treatment at a clinic could become a source of arguments (Weisz & Hawley, 2002). Second, based on past experiences with childhood interventions, families may believe that behavioral techniques work only for a short while (Molina et al., 2009). Third, disorganization and time management problems possess a genetic component—therefore parents of teens with ADHD may struggle to keep therapy appointments and remember to practice skills at home (Nigg et al., 2004). Finally, anxiety-driven micromanagement of teen academics is prevalent among a subset of these parents (Sibley, Campez, et al., 2016). When these parents are asked to reduce organizational assistance to promote teen autonomy building, they may be unprepared to do so without therapeutic support.
Engagement-Oriented Intervention
Given that psychosocial interventions for teens with ADHD are acutely efficacious (Chan, Fogler, & Hammerness, 2016; Sibley et al., 2014) but face engagement challenges, our team developed a treatment that directly addresses the problems noted above. Supporting Teens’ Autonomy Daily (STAND)1 is a skills-based therapy (BLINDED) that targets key adolescent functional domains (i.e., academic and family impairment; Wolraich et al., 2005) through engagement of empirically identified mechanisms of ADHD-related risk in adolescence (i.e., organization, time management, and planning problems, motivation deficits; Langberg, Dvorsky, & Evans, 2013; Sibley, Altszuler, Morrow, & Merrill, 2014; Toplak, Jain, & Tannock, 2005). A parent-teen collaborative model was chosen given the importance of parent involvement in adolescent mental health treatment (Henggeler & Lee, 2003; Le Grange, Lock, Loeb, & Nicholls, 2010), the potential for parents to supervise and reinforce skill practice, and the need to remediate maladaptive parenting practices in this population (Sibley, Campez, et al., 2016). To overcome previously documented difficulties engaging parents and teens with ADHD in treatment (Barkley, Edwards, Laneri, Fletcher, & Metevia, 2001), we blended behavioral skill modules (Barkley et al., 2001; Evans, Schultz, DeMars, & Davis, 2011; Patterson & Forgatch, 1987) with Motivational Interviewing (MI; Miller & Rollnick, 2013) to support parents in considering changes to parenting practices and to increase adolescent openness to new skills. For teens, STAND’s MI components are designed to promote identification of personal goals, increase openness to skill learning and practice, and contribute to the reduction of motivation problems (i.e., helping the teen clearly conceptualize personal reasons to complete work in spite of boredom and task aversiveness). MI components also are designed to help parents articulate their parenting goals and values, explore the extent to which their current practices support these desires, and empower parents to correct maladaptive parenting habits that inhibit teen improvements. To personalize treatment, we also designed a flexible protocol that offers families autonomy in choosing skills that feel most relevant. Therapists work with families to apply these skills to their households in a personalized manner. Therapists begin treatment with engagement modules designed to overcome common psychological and behavioral barriers to treatment in this population. Treatment concludes with mobilizing modules designed to empower independent skill use and healthy habit formation after termination.
Two randomized trials evaluating STAND (N=36; N=128; BLINDED) indicated strong treatment completion (85–100%) and family engagement using the skills-based blended MI model. Families in these trials reported high satisfaction and face validity for STAND, while therapists implemented skills-based components with fidelity and MI with integrity. Compared to untreated control participants, both trials indicated that STAND produced a range of medium to large acute effects on ADHD symptoms, organization time management, and planning (OTP) skills, homework behavior, parent-teen contracting, implementation of home privileges, parenting stress, and daily homework recording. Six months after treatment ceased, effects on ADHD symptom severity, OTP skills, and parenting stress maintained over time.
Rationale for an Internet-Based Approach
Although the content and therapeutic style of STAND were chosen to target population-specific treatment engagement, there are additional structural barriers that impede treatment delivery—consequently, some may not even make it to the first session to reap the benefits of STAND’s population-specific approach. The most common treatment barriers for youth with ADHD are distance to services, transportation access, scheduling conflicts, inconvenience of services, and disliking time in a waiting room (Bussing et al., 2012). On a public health scale, many families live in sparsely populated geographic locations that lack quality care options.
Internet-delivered treatment formats can offer transformative opportunities to overcome these systematic barriers to care (Comer, 2015; Comer & Myers, 2016). Recent estimates suggest over 75% of households in the U.S. possess Internet access (United States Census Bureau, 2012). Across the field of mental health, Internet-based therapy is an emerging treatment delivery strategy with documented benefits that include: (1) increasing access to geographic regions without available specialty services, (2) improving the convenience of supported services in ways that may overcome barriers related to transportation, work schedules, and scheduling competing child activities, (3) consolidating specialty services across geographic regions, (4) improving the ecological validity of care by delivering treatment directly in settings of impairment, and (5) reducing treatment barriers related to distance to the clinic, transportation costs and access, child care needs, and scheduling conflicts (Comer & Barlow, 2014; O’Donohue & Draper, 2011). Thus, Internet-based therapy has the potential to increase access to population-specific treatments. Pairing an Internet-based therapy modality with a population-specific treatment package (e.g., STAND) may be a strategic way to meaningfully expand access to quality care. Internet-based therapy formats are supported in the treatment of a range of mental health needs including adult depression (Broten, Naugle, Kalata, & Gaynor, 2011), pediatric obesity (Moore & O’Donohue, 2011), childhood OCD (Comer et al., 2014), and early childhood behavior problems (Comer et al., 2015). Research supports the role of Internet-delivered treatment for the medication management of childhood ADHD (Myers et al., 2015), but investigations are yet to evaluate Internet methods for the psychosocial treatment of adolescent ADHD.
In this uncontrolled feasibility study, we adapted STAND’s family-based therapy model for real-time delivery by a therapist over secure videoconferencing (Cisco WebEx), using an identical treatment manual to clinic-based trials of this approach (BLINDED). Families receive the same quantity of therapist contact as in traditional clinic-based STAND. Delivery adaptations included: (1) completing all client interactions via real-time videoconferencing, (2) mailing the family’s therapy workbook to clients, and (3) using the videoconferencing platform’s shared desktop feature (whereby families and therapists can simultaneously view the same screen) to complete certain in-session therapy activities. Full details on technological considerations and logistical details for the secure delivery of real-time psychological treatment over the Internet can be found elsewhere (Chou, Comer, Turvey, Karr, & Spargo, 2016).
The present study
The present study is an uncontrolled pilot evaluation of STAND delivered via videoconferencing to 20 adolescents with ADHD and their parents. Our aims were to: (1) evaluate the fidelity, implementation integrity, and feasibility of STAND delivered via videoconferencing, (2) characterize the engagement of families receiving STAND via videoconferencing, (3) evaluate the extent to which proposed mechanisms of therapeutic change (i.e., parent and teen motivation, parent coordination of home behavioral interventions) were engaged, and (4) assess the extent to which participating families experienced improvements in functioning that were similar in magnitude to those reported in face-to-face STAND trials. We hypothesized that STAND delivered through videoconferencing would demonstrate adequate fidelity, integrity and feasibility, that a majority of families would complete and participate actively in treatment, and that parents and adolescents would show increases in motivation and strategy use throughout the weeks of treatment. We also hypothesized that parent and teen satisfaction and therapeutic alliance would be strong. Based on data from face to face STAND trials, we hypothesized that participating adolescents would demonstrate large improvements in ADHD symptoms and organization problems, and small improvements in grade point average from baseline to post-treatment (BLINDED).
Method
Participating Families
Participants were 20 adolescents with ADHD between the ages of 11 and 16 who resided in a southeastern state. Participants attended 16 different schools: 70% attended public school and 30% private school. Participants were required to: (a) meet DSM-5 criteria for any presentation of ADHD (American Psychiatric Association, 2013), (b) be enrolled in sixth through twelfth grade, (c) display significant academic impairment, (d) have an estimated IQ > 75, and (e) have no history of an autism spectrum disorder. Significant academic impairment was assessed by examining parent and teacher impairment ratings and official school grades. Academic impairment was determined to be present if two of the three following criteria were met: (a) teacher endorsement of academic impairment on the Impairment Rating Scale (“3” or higher on 7-point scale, Fabiano et al., 2006), (b) academic impairment present in assignment-level school grades (i.e., failing to turn-in greater than 20% of assignments during the last month in at least one class or possessing a grade of D or F during the last month in at least one class), or (c) clinically elevated academic problems on the teacher academic problems checklist (4 items endorsed as “pretty much” or “very much;” Sibley et al., 2014). For generalizability to the larger adolescent ADHD population seeking care, youth with comorbidities and youth on psychotropic medications were permitted to remain in the study (see Table 1). Participants lived an average of 53.66 miles from the university clinic (SD=57.66, Range: 5.96–208.03). This study was conducted during the 2014–2015 school year.
Table 1.
Demographic and Clinical Characteristics of the Sample
| Adolescent Demographic | |
| Age M (SD) | 13.90 (1.55) |
| Male (%) | 75.0 |
| Race/Ethnicity (%) | |
| White Non-Hispanic | 50.0 |
| African American | 15.0 |
| Hispanic Any Race | 30.0 |
| Other | 5.0 |
| Parent Demographic | |
| Relationship to Teen | |
| Mother (%) | 95.0 |
| Father (%) | 5.0 |
| Parent Education Level (%) | |
| Some college or less | 5.0 |
| Bachelor’s degree | 40.0 |
| Master’s degree or higher | 55.0 |
| Single Parent (%) | 20.0 |
| Clinical | |
| Estimated Full Scale IQ M (SD) | 104.45 (13.21) |
| ADHD Diagnosis (%) | |
| ADHD-Predominantly Inattentive Type | 50.0 |
| ADHD-Combined Type | 50.0 |
| Oppositional Defiant Disorder (%) | 35.0 |
| Conduct Disorder (%) | 10.0 |
| Current ADHD Medication (%) | 60.0 |
| School Accommodations (%) | |
| Individualized Education Plan | 50.0 |
| Section 504 Plan | 20.0 |
| None | 30.0 |
All families possessed Internet access and a computing device equipped with a webcam and microphone at the outset of the study. However, webcams and microphones were available for loan, as needed. Prior to treatment, families were surveyed regarding their typical use of Internet technology. Overall, all parents reported at least daily use of smart phones or tablets and at least daily Internet or social media browsing. Ninety percent of parents reported at least daily use of email. In addition, 90% of parents reported previous experience with videoconferencing and 50% used videoconferencing technology at least monthly. Overall, 85% of adolescents reported at least daily smart phone or tablet use and Internet or social media browsing. Twenty percent reported daily use of email. Ninety percent of adolescents reported previous experience with videoconferencing and 75% reported using videoconferencing at least monthly.
Assessment Procedures
All procedures were approved by the university’s institutional review board. Guidance counselors throughout the state were emailed information about an opportunity for students to receive STAND free of charge via videoconferencing as part of research. Parents were directed to complete an online application for the trial that included parent ratings of the adolescent’s ADHD symptoms and psychosocial functioning. This application included instructions to provide an academic teacher with a hyperlink to similar teacher symptom and impairment ratings. Families were invited to participate in an intake assessment conducted via videoconferencing if the parent and teacher reports indicated probable eligibility defined as: (1) four or more symptoms of either Inattention or Hyperactivity/Impulsivity using an “or” diagnostic rule and (2) clinically significant problems at home and school (at least a “3” on a “0 to 6” impairment scale).
Intake occurred via videoconference. Informed parental consent and youth assent were obtained by providing family members with electronic links to consent and assent forms and discussing these documents via videoconference. The primary caretaker participated in the assessment and treatment aspects of the project. During the intake, a predoctoral trainee administered the Computerized-Diagnostic Interview Schedule for Children (Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000) to the parent face to face via the videoconferencing platform. Information collected in the interview was integrated with web-collected teacher ratings to provide standard and recommend assessment for ADHD. Additionally, two orally administered subtests (Arithmetic and Similarities) of the Wechsler Intelligence Scale for Children-IV (WISC-IV; Wechsler, 2004) were delivered to the adolescent via videoconference to estimate adolescent IQ. The combination of these two subtests correlates highly (.87) with WISC-IV full scale IQ (Sattler & Dumont, 2004). A licensed clinical psychologist determined diagnosis and study eligibility. Symptom data were combined using an “or rule,” which identifies the presence of a symptom if endorsed by either informant (Bird, Gould, & Staghezza, 1992), and subjected to the age appropriate threshold outlined in the DSM-5 (six symptoms of either inattention or H/I for youth under seventeen). When applying the “or rule,” ADHD symptoms were required to be present in both the school and the home setting (at least three symptoms present in each); however, the adolescent need not meet full threshold in both settings. The psychologist used all available information to consider age of onset (i.e., parents were required to report that symptoms were present before age 12), chronicity (i.e., symptoms were required to be present for at least six months duration, including presence during the last four weeks), comorbid symptoms (i.e., symptoms could not occur exclusive to another mental health disorder), and severity of impairment when making ADHD diagnoses, adhering strictly to the requirements of the DSM-5. Families began treatment within one month of intake.
Complete baseline data was required for study entry. Participants provided bi-weekly data on motivational indices and parent implementation of home behavioral strategies through an online survey interface. Therapists kept standardized contact logs with information about treatment attendance, homework completion, technology disturbances, and session proceedings that were reviewed by the Ph.D. level clinical supervisor each week. At the end of treatment, therapists completed ratings of family engagement and experiences delivering treatment through videoconferencing. Parents and adolescents completed satisfaction ratings and reported on their experience with the videoconferencing interface. Teachers provided post-treatment ratings of the teen’s ADHD symptoms. Families received $90 at the end of the study if all study ratings were completed, regardless of treatment completion. Teachers received $20 for providing post-treatment symptom ratings. No incentives were given for treatment activities.
Treatment Description
Families were assigned to therapists based on scheduling availability. All therapists (N=7) participated in a three-day training that included a one-day basic MI workshop conducted by a member of the Motivational Interviewing Network of Trainers (MINT) and two days focused on the application of MI spirit and skills to parents and adolescents with ADHD, training in skill module content, and an orientation to study procedures. Therapists were required to demonstrate mastery of the STAND manual (skill based modules and MI delivery style) through a score of at least 80% on a written procedural test. Therapist training level included pre-doctoral trainee (71.4%), master’s level (14.3%), and doctoral level (14.3%). Study caseloads ranged from one to five per therapist. All STAND therapists received weekly supervision from the lead developer of the STAND protocol, who is a licensed clinical psychologist, a member of MINT, and has extensive experience with families of adolescents with ADHD.
STAND consists of ten 60-minute manualized family therapy sessions attended by the parent and teen. Full implementation procedures are provided in a manual (BLINDED) that includes suggested use of MI as well as skills-based components. In Session 1, therapists (a) provide an overview of STAND, (b) discuss case conceptualization and provide feedback on assessment results, (c) discuss parent and adolescent strengths and values, (d) discuss common behavior patterns among parents of teens with ADHD, and (e) explore discrepancies between parent values and current parenting patterns. In Session 2, therapists work with family members to (a) identify and prioritize parent and adolescent areas for change, (b) identify treatment goals, and (c) select modular skills-based components from a treatment menu. The STAND menu contains seven possible modular sessions, of which families select up to four: (a) recording homework daily, (b) creating a homework contract, (c) organizing school materials, (d) prioritizing and managing time out of school, (e) note-taking in class, (f) preparing for tests and quizzes, and (g) troubleshooting problems at home.
For each modular session, a skill is introduced, a plan for applying the skill is devised, and a parent-teen contract is created to detail contingencies associated with appropriate and consistent skill use during the upcoming week. During skills-based sessions, therapists use MI in a blended manner to increase the family’s openness to trying a new strategy and empower lasting changes at home. As part of each skill contract, parents detail a monitoring plan to reinforce consistent skill use by the teen. At each session, families review the past weeks’ skill use and contract implementation and the therapist engages the family in MI to consider whether they will continue skill use and monitoring. Four mobilizing sessions at the conclusion of treatment address how to engage the school, creating a lasting routine for the practice of new skills, using communication skills to modify home contracts, and reviewing progress and next steps. At the outset of treatment, parents and teens each identify up to three personal treatment goals. A qualitative coding procedure outlined in Merriam (1998) was used to identify common themes across individualized treatment goals in the present sample, which are summarized in Table 2.
Table 2.
Parent and Teen Self-Identified Treatment Goals across Families
| Parent Stated Treatment Goals (%) | |
| Reduce helping during homework | 65.0 |
| Learn how to motivate teen | 50.0 |
| Be more consistent with consequences | 50.0 |
| Find more time for self | 30.0 |
| Reduce emotional response to teen behavior (anger or anxiety) | 15.0 |
| Increase supervision of the adolescent | 10.0 |
| Improve communication with the school | 5.0 |
| Teen Stated Treatment Goals (%) | |
| Improve time management after school | 55.0 |
| Improve organization skills | 35.0 |
| Improve study skills | 35.0 |
| Reduce missing assignments | 30.0 |
| Keep track of homework assignments better | 25.0 |
| Become more motivated to do school work | 20.0 |
| Start and finish homework earlier | 20.0 |
| Improve planning skills | 15.0 |
| Get homework done more efficiently | 15.0 |
| Improve relationship with parent | 15.0 |
| Improve social life | 10.0 |
| Participate more in class | 10.0 |
| Improve relationships with teachers | 5.0 |
| Reduce anger toward parent | 5.0 |
| Complete morning routine without parental assistance | 5.0 |
Note. % represents the percentage of families that identified this goal. Each family member was encouraged to identify up to five goals for treatment.
Videoconference Interface
Technological, ethical, and administrative considerations for use of videoconferencing to deliver mental health interventions are discussed in greater detail elsewhere (American Telemedicine Association, 2009; Chou et al., 2016; Crum & Comer, 2016; Nelson, Davis & Velasquez, 2013; Spargo, Karr, & Turvey, 2013). Study decisions related to technology and administration were made in accordance with the American Telemedicine Association’s current practice guidelines for videoconference telemental health (American Telemedicine Association, 2009). Cisco Webex (www.webex.com) is a videoconferencing platform that was selected for STAND delivery. Cisco Webex can be accessed via webcam and microphone equipped computer, tablet, or smart phone. This technology allows therapists and families to communicate in real time and high speed Internet offers sufficient connection quality to support therapeutic interactions. Cisco Webex includes a desktop sharing function through which connected parties can simultaneously view one party’s screen, allowing therapists and families to share treatment forms with one another and jointly evaluate graphs depicting treatment responses. The platform’s interface includes a Secure Sockets Layer/Transport Layer Security encryption tunnel to ensure privacy and the platform does not store or retain session information on its network after sessions end, as required for HIPAA regulatory compliance. Prior to the first session, therapists held a 20-minute technology orientation with families to introduce the interface and troubleshoot issues related to platform connection. Each week, therapists invited families to the videoconferencing session via a link sent to the parent’s email address. Once families clicked this link, the Cisco Webex meeting automatically launched through their Internet browser or device application.
Measures
Treatment Fidelity
Therapists audiotaped each weekly family session. Trained bachelor’s level research assistants were trained to code audiotape sessions using a standard dichotomously coded treatment fidelity checklist for each session that was employed in previous trials of STAND (BLINDED). Twenty percent of sessions were randomly selected for fidelity coding. In the current study, half of coded sessions were double coded and inter-rater reliability was found to be 88.5%.
Therapist MI Adherence
The Motivational Interviewing Treatment Integrity (MITI) version 4.1 (Moyers, Manuel, & Ernst, 2014) was used to code therapy tapes for MI adherence. The MITI is a behavioral coding system that has been used to measure MI treatment integrity across numerous clinical trials and possesses strong reliability and predictive validity (Moyers, Martin, Manuel, Hendrickson, & Miller, 2005). MITI coding yields global scores of MI implementation quality on four dimensions rated from a minimum of “1” to a maximum of “5”: Cultivating Change Talk, Softening Sustain Talk, Partnership, and Empathy. MITI behavior counts were tallied for each therapist utterance using ten categorical behaviors representing MI adherent (e.g., affirm, seek collaboration, emphasize autonomy) and nonadherent (e.g., confront, persuade) behaviors. Technical skill indices (i.e., reflection to question ratio, % complex reflection) were also calculated. Twenty percent of sessions were randomly selected for each STAND case and twenty minutes of these sessions were randomly selected for coding. Two coders who attended formal training in MITI coding independently double coded sessions. Intraclass correlation coefficients (ICC) were calculated to measure inter-rater reliability. Two indices could not be evaluated with ICCs due to restriction of range (Cultivating Change Talk, Softening Sustain Talk); however, coding pairs were within one point of each other on these indices for 100% of tapes. Average ICC was .71 indicating “substantial” inter-rater agreement (Landis & Koch, 1977).
Attendance & Home Activity Completion
Weekly attendance and home activity completion for each family session was measured from therapist contact logs. For attendance, therapists coded families as (0=not present or 1= present) for each session. Therapists also coded each week’s home activity as (0=not completed, .5=partially completed, or 1=completed). The proportion of sessions attended (out of 10) was calculated. The proportion of home activities completed (out of the total number of sessions with assigned home activities attended) was also calculated.
Videoconferencing Feasibility
Parents and adolescents provided qualitative report of the most helpful and most problematic elements of receiving STAND via videoconference. Parents and adolescents also reported the type of device used (i.e., tablet, laptop computer, desktop computer, smartphone) and location of sessions (i.e., common room, private room, public location). Parents and adolescents reported the extent to which privacy was an issue on a 4-point scale (0=not at all to 3=very much). In addition, parents and adolescents completed the Telepresence in Video Conference Scale (Bouchard & Robillard, 2006) which is an eight-item measure of the sensation that therapist is in the same physical space as the family (telepresence). Respondents rate their agreement with statements about the therapist’s telepresence on a 5-point scale (1=strongly disagree to 5=strongly agree). Alpha for this scale ranged from .69 to .86.
Therapists logged all technological and contextual disturbances (due to delivering treatment in the home) that occurred during each session including the number and duration of disturbances and the specific nature of problems. At post-treatment, therapists also rated rapport with families and perceived treatment effectiveness on an 11-point Likert scale. Using a five point Likert scale, therapists offered global impressions of the extent to which delivering STAND via videoconferencing interfered with or enhanced treatment for each family (0=interfered with significantly to 4=enhanced significantly).
Therapeutic Alliance
After even numbered sessions, parents’ and adolescents’ perceptions of working alliance and emotional bond with their therapist was measured using the seven-item Therapist Bond Scale (Shirk & Saiz, 1992). The TBS items are rated by teens and parents on a 4-point Likert-type scale, ranging from 1 (not at all) to 4 (very much). Internal consistency and convergent validity are established for this measure (Shirk et al., 1992). Alpha ranged from .79 to .81.
Motivation to Change
Parents and teens were asked to consider the personal goals they set in session 2 (see Table 2) and rate their present motivation to make these changes on three dimensions (readiness, importance, and confidence) using an 11-point Likert Scale (0=not at all to 10=extremely). This scale was administered after even numbered sessions. The measure was based on the readiness ruler, which is a primary outcome variable in research on MI (Miller & Rollnick, 2013) and possesses established psychometric properties with adolescent populations (Aliotta, Vlasnik, & DeLor, 2004).
Implementation of Home Interventions
The Parent Academic Management Scale (PAMS) is a checklist developed to measure the frequency with which parents monitor (e.g., check to see if teen wrote in a daily planner), assist with (e.g., help teen organize school materials), and reinforce (e.g., use a home academic contract) a range of adolescent OTP skills. Parents indicated the number of days during the past school week (0 to 5) that they performed each activity. The PAMS possesses established psychometric properties (Sibley, Altszuler, et al., 2016). This scale was administered at baseline and after even numbered sessions. Behavioral strategies of interest in the current study were checking to see if the teen had completed homework and providing home privileges on a contingent basis based on practice of therapy skills.
ADHD Symptom Severity
Each participant’s level of inattention severity was measured using the parent and teacher versions of the DSM-5 Disruptive Behavior Disorder Rating Scale (DBD; Pelham, Gnagy, Greenslade, & Milich, 1992; Sibley & Yeguez, 2014; Sibley & Kuriyan, 2016). At baseline and post-treatment, respondents rated symptoms of ADHD as not at all present (0), just a little (1), pretty much (2), or very much (3). To calculate symptom severity, the average level (0–3) of each item on each subscale was calculated. The psychometric properties of the DSM-5 version of the DBD rating scale are well established, with empirical support for distinct, internally consistent subscales (Sibley & Yeguez, 2014, Sibley & Kuriyan, 2016). The DBD shows test-retest stability over time (Fabiano et al., 2006) and reliably detects treatment effects in samples of youth with ADHD (Pelham & Hoza, 1996). In the current study, alpha on the DSM-5 version of the DBD ranged from .92 to .94.
Organization, Time Management, and Planning Problems
The parent and teacher versions of the 24-item Adolescent Academic Problems Checklist (AAPC; Sibley et al., 2014) measure observable secondary-school specific organization, time management, and planning (OTP) problem behaviors and are validated for use in samples of adolescents with ADHD (Sibley et al., 2014). The parent and teacher AAPCs possess two distinct factors with strong internal reliability and concurrent validity (Sibley et al., 2014). Alphas for the AAPC were strong in the current study (.90–92).
Official School Grades
Electronic gradebook data were obtained directly from schools or parents. GPA for the three weeks prior to baseline and post-treatment was calculated by converting all academic grades (i.e., Language Arts, Math, Science, Social Studies, Foreign Language) to a 5-point scale (i.e., 4.0=A, 3.0=B, 2.0=C, 1.0=D, 0.0=F), averaging grades within class, and then averaging all core academic class grades during the three week period. Grades were not weighted for class level (e.g. Honors vs. Regular).
Treatment Satisfaction
Parents and adolescents provided ratings of treatment satisfaction at post-treatment using a standard satisfaction questionnaire developed for STAND (BLINDED). These surveys evaluate the respondent’s satisfaction with program performance across key domains of treatment. Parents indicated their degree of satisfaction for 20 aspects of treatment using a 5-point Likert Scale (1=Strongly Disagree to 5=Strongly Agree). The teen version of this scale possesses 15 items and is also evaluated using a 5-point Likert Scale (1=Strongly Disagree to 5=Strongly Agree). An average satisfaction index was calculated and examined for each rater. Alpha for this index ranged from .95 to .96.
Analytic Plan
In this uncontrolled preliminary feasibility study, descriptive data are presented for measures of feasibility and therapeutic process. With respect to therapeutic alliance, motivation to change, and parent use of behavioral strategies, linear mixed models (LMMs) with random effects were conducted in SPSS 22 using an intent-to-treat design (West, Welch, & Galecki, 2006). Separate LMMs were conducted for each outcome. For each model, a fixed effect of linear time and random intercepts were included. A robust Maximum Likelihood estimator was employed in all models. All outcome variables were measured at approximately two weeks apart at session numbers 2, 4, 6, 8, and 10, as well as a post-treatment measurement that occurred one week after the family’s final session. Time was coded as a continuous, subject-specific measure that reflected session number (which also corresponds with the number of weeks since baseline). The initial measurement time is coded 0; the intercept reflects the predicted outcome value at the first measurement point and the linear effect reflects the instantaneous linear change in the outcome at the first measurement point. To investigate preliminary baseline to post changes in parent and teacher rated inattention severity, as well as OTP problems and grade point average, a repeated measures general linear model (GLM) was conducted separately for each outcome (inattention, OTP problems, GPA). In these models, time (baseline vs. post treatment) was modeled as the independent variable.
Results
Attendance & Home Activities
Overall, 85.0% of families completed all ten sessions. Three families who did not complete ceased treatment after sessions 2, 3, and 4 respectively. Among completing families, home activity completion was typically high (M=70.3%, SD=16.2%; range: 44.4% to 100.0%).
Videoconferencing Feasibility
All families reported completing sessions in their homes, using a range of devices (see Table 3). Families used public rooms (e.g., kitchen, living room) at greater frequency than private rooms (e.g., bedroom, office). Privacy was at least a minor concern for most families. On average, only 2.40 sessions (SD=1.84) per family were interrupted by technological disturbances, requiring an average of 8.50 minutes (SD=5.64) to resolve. Almost four sessions (M=3.55; SD=3.21) per family were interrupted by disturbances specific to conducting treatment at home, requiring an average of 6.10 minutes (SD=6.04) to resolve. Technology disturbances stemmed from a range of sources (see Table 3), with the most common being full or partial Internet connection problems. Therapist reported a range of home disturbances (see Table 3), the most common being family members leaving the room and interruptions by nonparticipating family members. These disturbances were reported by therapists to be meaningful for 45% of the sample. In 50% sample, therapists believed that the videoconferencing format enhanced treatment. The perceived benefits of the videoconferencing interface included fewer cancellations, fitting better with the family’s schedule, overcoming distance from clinic, and beginning sessions on time.
Table 3.
Details of Each Family’s Videoconferencing Treatment Experience
| Device used (%) | |
|---|---|
| Tablet | 20.0 |
| Laptop computer | 65.0 |
| Desktop computer | 10.0 |
| Combination of devices | 5.0 |
| Session location (%) | |
| Public room in home | 75.0 |
| Private room in home | 25.0 |
| Privacy concerns (%) | |
| Major | 40.0 |
| Minor | 25.0 |
| None | 35.0 |
| Technological disturbances (% experiencing) | |
| Temporarily lost audio connection | 25.0 |
| Temporarily lost video connection | 20.0 |
| Temporarily dropped Internet connection | 20.0 |
| Slow connection | 10.0 |
| Full Internet outage | 5.0 |
| Inability for parent and teen to fit in camera frame | 5.0 |
| Parent difficulty finding invitation in email inbox | 5.0 |
| Home disturbances (% experiencing) | |
| Family member leaving the room | 30.0 |
| Interruptions by nonparticipating family member | 20.0 |
| Incoming phone calls | 15.0 |
| Sending phone messages | 15.0 |
| Playing games on the computer | 15.0 |
| Cooking or eating meals | 15.0 |
| Private conversations that excluded therapist | 10.0 |
| Answering the door | 10.0 |
| Watching television | 5.0 |
| Playing a musical instrument | 5.0 |
Treatment Fidelity & MI Adherence
Average STAND fidelity score for probed sessions was 81.9%. Using the MITI 4.1, all mean global scores converged at a value of 4 on the 5-point scale indicating strong integrity: Cultivating Change Talk (M=4.00, SD=.72), Softening Sustain Talk (M=3.94, SD=.35), Partnership (M=4.19, SD=.74), and Empathy (M=4.34, SD=.75). Technical benchmark means (Moyers et al., 2014) were mixed for the videoconferencing format. These indicated a higher reliance on questions than reflections (reflection to question ratio=.88:1), but an excellent level of complex reflections compared to simple reflections (48.9%) and appropriate levels of MI adherent statements (M= 2.25) and MI non-adherent statements (M=.03) per coded segment.
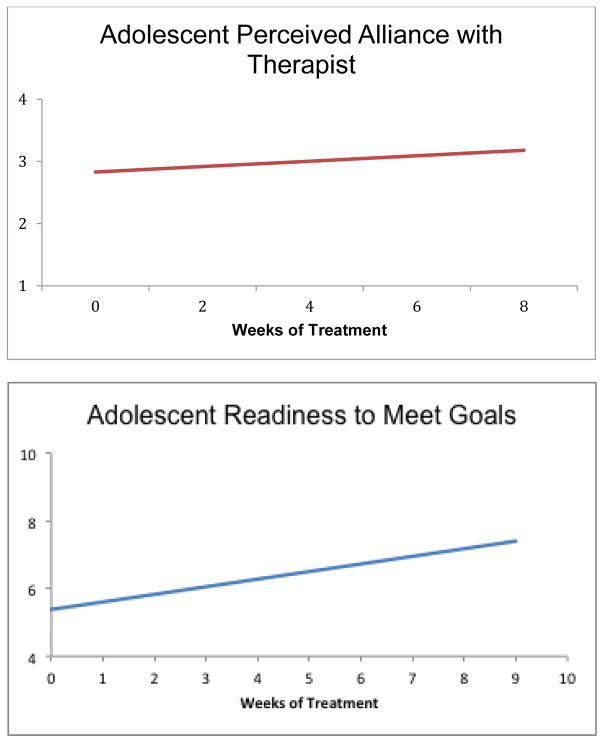
Therapeutic Alliance
Average therapist telepresence (1 to 5 scale) was rated as 3.58 (SD=.56) by parents and 3.11 (SD=.43) by adolescents. LMM results (see Figure 1) indicated a significant positive linear effect of time for adolescent perceived therapeutic alliance (b=.04, SE=.01, p=.003, d=.84), whereas parent perceived therapeutic alliance (1 to 4 scale) was strong at the outset of therapy (M=3.53, SD=.39) and did not change significantly over time. On a 0 to 10 scale, average therapist perceived rapport with families was 7.75 (SD=2.34) and therapists rated perceived therapy effectiveness as 6.40 (SD=2.52).
Figure 1. Changes over Videoconference-delivered Treatment in Adolescent Perceived Alliance with Therapist and Readiness to Meet Self-Selected Goals.
Note. Therapeutic Alliance is measured on an 4 point scale (from 1 to 4) with high values indicated stronger alliance. Readiness to meet goals is measured on an 11 point scale (from 0 to 10) with high values indicated stronger readiness. Data displays mean values during each week as derived from intercept and slopes of Linear Mixed Models.
Motivation to Change
LMM results (see Figure 1) indicated a significant positive linear effect of time for adolescent perceived readiness to achieve self-selected therapy goals (baseline M= 5.38, SD=1.82; b=.22, SE=.06, p<.001, d=1.11), whereas adolescent perceived importance of (M=7.26, SD=2.58) and confidence in (M=6.89, SD=2.40) meeting these goals were strong from the outset of goal setting (0 to 10 scale) and did not change significantly over time. Parent perceived importance (M=8.55, SD=1.91), confidence (M=8.95, SD=1.64), and readiness (M=7.90, SD=1.83) also were strong at the outset of goal setting and did not change significantly over time.
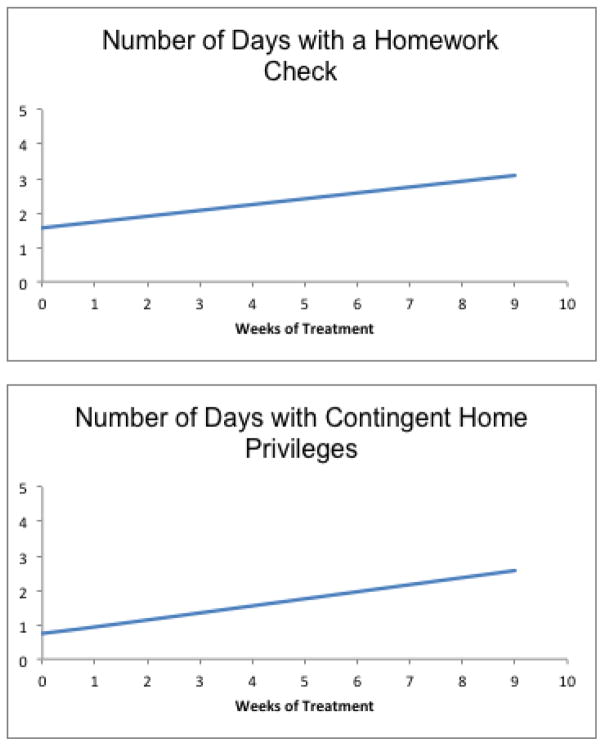
Implementation of Home Interventions
LMM results (see Figure 2) indicated a significant positive linear effect of time for frequency of parent homework checks per week (baseline M= 1.56, SD=1.31, b=.17, SE=.06, p=.008, d=.98) and contingent provision of home privileges (baseline M=.74, SD=.82, b=.22, SE=.06, p<.001, d=2.41).
Figure 2. Parent Implementation of Behavioral Strategies at Home across Videoconference-delivered Treatment for Adolescent ADHD.
Note. Data displays mean values during each week as derived from intercept and slopes of Linear Mixed Models.
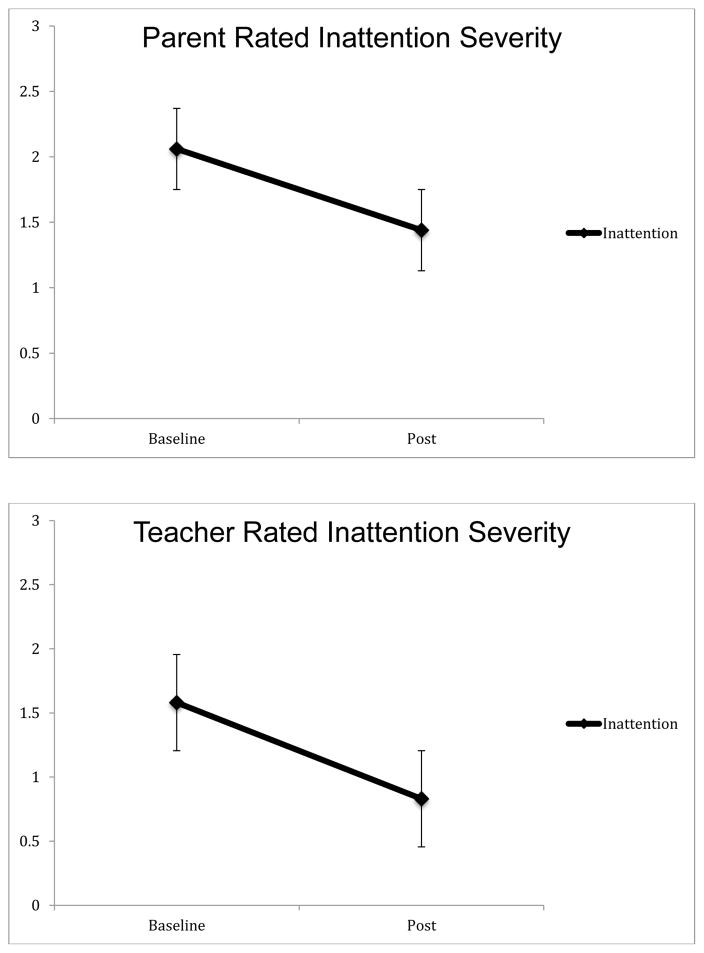
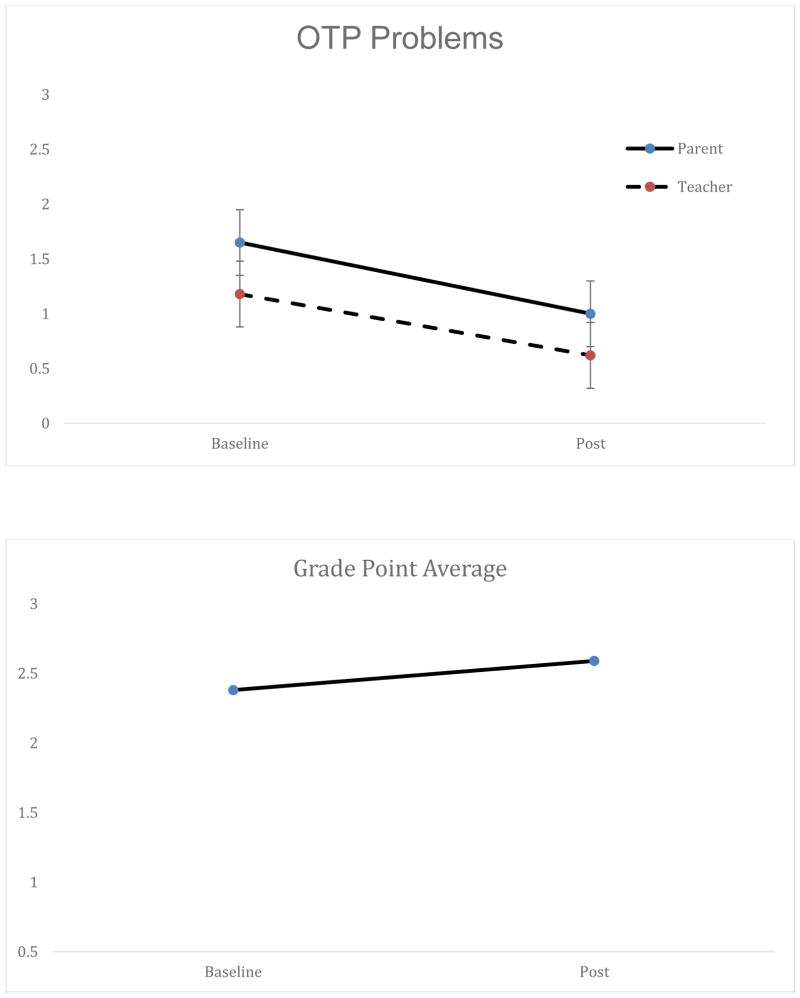
ADHD Symptom Severity & Academic Impairment
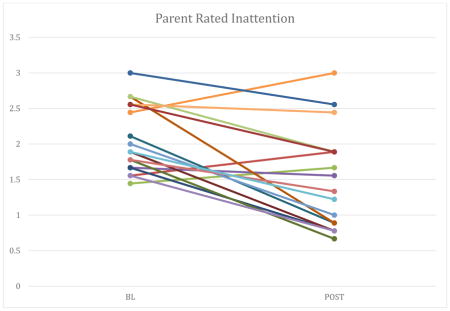
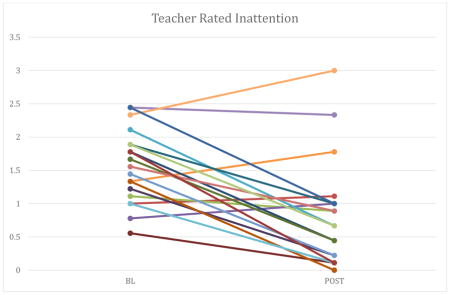
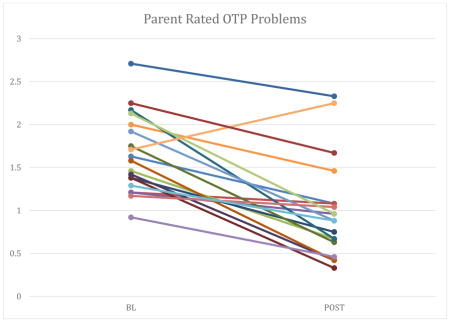
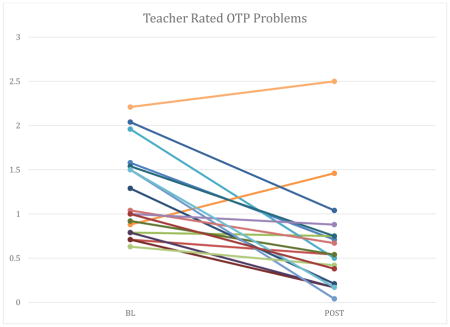
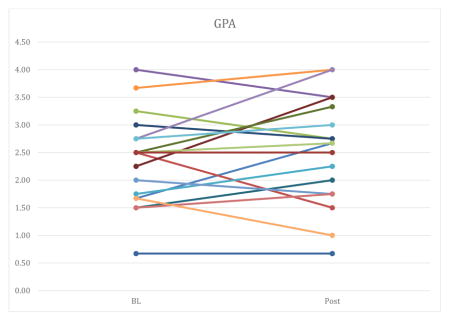
Compared to baseline (M=2.06, SD=.46), parents of participants observed inattention symptoms to be significantly less severe at post-treatment [see Figure 3; M=1.44, SD=.68, F(1, 18)=20.06, p<.001, d=1.35, SEM=.42]. Similarly, compared to baseline observations (M=1.58, SD=.54), teachers indicated inattention symptoms were significantly less severe at post-treatment [see Figure 3; M=.83, SD=.77, F(1, 19)=22.44, p<.001, d=.83, SEM=.50]. Compared to baseline (M=1.65, SD=.45), parents of participants also observed OTP problems to be significant less severe at post-treatment [see Figure 4; M=1.00, SD=.57, F(1, 18)=33.84, p<.001, d=1.44, SEM=.34]. Similarly, compared to baseline observations (M=1.18, SD=.49), teachers indicated OTP problems were significantly less severe at post-treatment [see Figure 4; M=.61, SD=.57, F(1, 19)=20.68, p<.001, d=1.16, SEM=.40]. Compared to baseline (M=2.38, SD=.81), the grade point average of participants was slightly higher at post-treatment [see Figure 4; M=2.56, SD=.94). However, this small effect was not statistically significant [F(1, 18)=1.55, p=.22, d=.22].
Figure 3.
ADHD symptom responses across videoconference-delivered treatment, as reported by parents and by teachers
Note. Error bars represent standard error of measurement values.
Figure 4.
OTP Problems and GPA across videoconference-delivered treatment, as reported by parents
Note. Error bars represent standard error of measurement values.
Treatment Satisfaction
Mean overall satisfaction (1 to 5 scale) for parents was 3.92 (SD=.68) and for adolescents was 3.84 (SD=.98) indicating that satisfaction was well above the neutral point of the scale.
Discussion
Although recent years witnessed gains in our understanding of efficacious psychological treatment for adolescent ADHD (Sibley et al., 2014), barriers to care continue. The present evaluation is a preliminary attempt to leverage videoconferencing to expand the accessibility of psychosocial treatment for adolescents with ADHD. Findings were that: (1) most families completed a full course of treatment and intervention fidelity and integrity were acceptable; (2) delivering STAND via videoconferencing was feasible, but subject to minor technological disruptions, which may have reduced therapeutic benefit for a subset of families; (3) therapeutic alliance was acceptable; (4) key mechanisms of change (adolescent motivation to meet goals, parent strategy implementation) appeared to be engaged during treatment; (5) ADHD symptoms, OTP problems, and GPA changed at a rate that was similar to those reported in face to face trials of STAND; and (6) families were satisfied with treatment.
Treatment completion in this trial (85%) was identical to that reported for a randomized controlled trial (RCT) of STAND delivered in the clinic (BLINDED). Thus, the videoconferencing interface appears to promote retention at a similarly high rate to clinic-based STAND. Fidelity for STAND delivered via videoconferencing was also high (81.9%), indicating that a majority of intervention components were appropriately delivered. This estimate is somewhat lower than those reported in clinic-based evaluations of STAND (approximately 95% fidelity; BLINDED), but still quite high. Overall, MI integrity was high in this trial, with the exception of an overreliance on questions, rather than therapeutic reflections by therapists, which was not the case for clinic-based versions of the intervention (BLINDED). Based on past trials of clinic-based STAND, instances of MI adherent statements were also fewer than expected (BLINDED). Thus, it appears that there was a slight reduction in fidelity and integrity for skills-based and MI components when delivering STAND via videoconferencing, but that overall, a majority of core components remained in tact.
Slightly reduced integrity and fidelity is not surprising given that approximately five minutes per session were lost to disturbances caused by technology problems or issues specific to conducting home-based treatment. In addition, parents and teens felt that their interactions and ability to bond with the therapist were acceptable but that naturalness of the therapeutic relationship (telepresence) was somewhat reduced by the videoconferencing interface. It is not clear whether problems with telepresence reduced efficacy. However, recent RCTs evaluating videoconferencing formats relative to clinic-based formats of other evidence-based treatments for youth find no indication of reduced efficacy associated with videoconferencing formats (Comer & Myers, 2016).
Despite slight reductions in integrity, fidelity, and therapeutic presence, evidence suggests that STAND’s theoretical mechanisms of change were engaged during treatment (see Figures 1 & 2). This included enhancing teen motivation to improve functioning and increased parent implementation of behavioral strategies. In addition, parents and teachers perceived reductions in inattention symptom severity from baseline to post-treatment that mirror effects reported in previous RCTs of STAND (BLINDED) and represents movement into the subclinical range of ADHD severity for a majority of participants. Reductions in OTP problems, the chief presenting concern of most adolescents in the study, also were similar in magnitude to those reported in face to face trials of STAND. Much like the face to face trials of STAND, there was a small effect for GPA (d=.22). It is important to note that in the current investigation, this effect was nonsignificant. Given evidence that GPA trajectories for adolescents with ADHD decline across the school year (Schultz, Evans, & Serpell, 2009), these data are difficult to fully interpret without a control group.
Given that parents perceived positive change in adolescents following participation in STAND via video conferencing, it is not surprising that therapists of 50% of families believed treatment response to be enhanced by videoconferencing. Likewise, despite some disruptions, both parents and teens were satisfied with treatment. These data suggest that in spite of a slight reduction in fidelity and integrity, videoconferencing is a promising method of engaging families who might not otherwise have attended clinic-based STAND. However, further research is needed that directly compares the therapeutic trajectory of families who received STAND via videoconferencing versus in a clinic. It is likely that for many families, clinic-based treatment remains preferable; however, for the large number of families dwelling in regions beset by poor mental health care accessibility, a quality videoconferencing format may yield better long-term outcomes.
This study is an uncontrolled preliminary investigation of STAND delivered via videoconferencing and therefore possesses many important limitations. First, the sample was highly educated, located relatively close to a major metropolitan region, motivated to participate in treatment, and computer literate; thus, findings may not generalize to families of lower socioeconomic status or with poorer familiarity with technology, or who are dwelling in rural or other underserved regions. This sample also was relatively motivated from the outset of therapy; thus, it is possible that treatment completion and efficacy may be weaker in a less engaged sample. In addition, parents and teachers were involved in aspects of the clinical assessment and treatment process and therefore could not be blinded to the adolescent’s participation in treatment. We did not include a control group in this preliminary study. Thus, some treatment effect sizes may be inflated because they do not account for normative changes in symptoms and functioning over time. Therefore, all conclusions about efficacy must be suspended until the completion of a randomized controlled trial of STAND delivered by videoconferencing. Because of our small sample size, we were unable to examine treatment moderators such as age or medication status. In addition, given our small sample size and the modular nature of the treatment, it is also possible that the modules selected by participants may not be representative of the modules that would be selected by the larger population of adolescents with ADHD, which could limit generalizability of findings. It is also possible that this study may have oversampled adolescents who received medication (60.0%) and attended private school (30.0%). Although medication status was held constant through the study weeks, receipt of medication likely influenced overall ADHD symptom severity at baseline and post-treatment. Future work focused on efficacy is needed to assess the full utility of Internet-delivered STAND. Since we did not directly compare videoconferencing therapy process and outcomes to those of clinic-based STAND, our present observations about the efficacy of the videoconferencing interface are tentative.
Despite the preliminary nature of our results, we offer several recommendations for the continued development of internet-delivered treatments for ADHD. First, the protocol might be modified to address disruptions associated with technology problems and delivering treatment in the home setting. For example, therapists may consider conducting a discussion with families at the outset of treatment about ways to reduce distractions that are specific to the videoconferencing interface. Therapists might also consider being mindful of the need to more fully cover STAND content and increase instances of therapeutic reflections and MI adherent statements when using videoconferencing. It may also be helpful for therapists to make added attempts to build rapport with families given that problems with telepresence are noted using videoconferencing interface. Future evaluations of STAND delivered through videoconferencing should also investigate whether medication influences treatment response and whether parents with a diagnosis of ADHD respond differently to STAND delivered through videoconferencing. There are also demographic factors, such as socioeconomic status and age, that may specifically influence response to treatment delivered through internet-based technology. Future research should evaluate the extent to which STAND delivered through videoconferencing is differentially beneficial to certain youth and families. Conducting a rate of change analysis could also provide useful information about how many sessions of STAND are needed to obtain meaningful reductions in ADHD symptoms and impairment.
The field of behavioral telehealth is still relatively nascent and clinical applications incorporating technology to expand mental health services are advancing at a pace more rapid than the development of logistical, regulatory, legal, and ethical guidelines and a supporting evidence-base (Comer & Barlow, 2014). As such, we must be appropriately cautious as we move forward to use videoconferencing to remotely deliver treatments, particularly with regard to issues of security, privacy, and liability. Fortunately, a guiding dialogue about these issues has begun to emerge in recent years (Chou et al., 2016; Kramer, Kinn, & Mishkind, 2015, Schwartz & Longborg, 2011), but much of the work is still ahead. The present findings add to this ongoing conversation, providing preliminary information about how videoconferencing may play a future role in making supported treatments for adolescent ADHD accessible to more teens in need, regardless of geography or local accessibility of quality services.
Acknowledgments
Funding. This work was made possible by grants from the American Psychological Foundation and Florida International University, Herbert Wertheim College of Medicine.
Appendix: Individual graphs for participants on pre-post outcomes
Footnotes
The STAND acronym originally stood for Supporting Teens’ Academic Needs Daily; however, the full name of the program was modified to Supporting Teens’ Autonomy Daily in 2016. This change was made to reflect the protocol’s breadth (academics is only one of several domains targeted) and central goal (building autonomy in teens with ADHD).
The authors report no conflicts of interest.
Compliance with Ethical Standards
Ethical Approval. All procedures were approved by the university Institutional Review Board. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent. Informed consent was obtained from all individual participants included in the study.
Conflicts of Interest. The authors report no conflicts of interest.
References
- Aliotta SL, Vlasnik JJ, DeLor B. Enhancing adherence to long-term medical therapy: a new approach to assessing and treating patients. Advances in therapy. 2004;21:214–231. doi: 10.1007/BF02850154. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. ADHD: Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128:1007–1022. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- American Telemedicine Association. Practice guidelines for videoconferencing-based telemental health: October 2009. 2009 doi: 10.1089/tmj.2010.0148. Retrieved June 25, 2013 from: http://www.americantelemed.org/docs/default-source/standards/practice-guidelines-for-videoconferencing-based-telemental-health.pdf. [DOI] [PubMed]
- Barkley R, Edwards G, Laneri M, Fletcher K, Metevia L. The efficacy of problem-solving communication training alone, behavior management training alone, and their combination for parent–adolescent conflict in teenagers with ADHD and ODD. Journal of Consulting and Clinical Psychology. 2001;69:926–941. [PubMed] [Google Scholar]
- Barkley R, Anastopoulos A, Guevremont D, Fletcher K. Adolescents with ADHD: Patterns of behavioral adjustment, academic functioning, and treatment utilization. Journal of the American Academy of Child & Adolescent Psychiatry. 1991;30:752–761. doi: 10.1016/s0890-8567(10)80010-3. [DOI] [PubMed] [Google Scholar]
- Barkley R, Fischer M, Smallish L, Fletcher K. Young adult outcome of hyperactive children: Adaptive functioning in major life activities. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:192–202. doi: 10.1097/01.chi.0000189134.97436.e2. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR, Fischer M. ADHD in Adults: What the Science Says. New York: Guilford; 2008. [Google Scholar]
- Biederman J, Monuteaux M, Spencer T, Wilens T, MacPherson H, Faraone S. Stimulant therapy and risk for subsequent substance use disorders in male adults with ADHD: a naturalistic controlled 10-year follow-up study. American Journal of Psychiatry. 2008;165:597–603. doi: 10.1176/appi.ajp.2007.07091486. [DOI] [PubMed] [Google Scholar]
- Bird HR, Gould MS, Staghezza B. Aggregating data from multiple informants in child psychiatry epidemiological research. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:78–85. doi: 10.1097/00004583-199201000-00012. [DOI] [PubMed] [Google Scholar]
- Biswas A, Gnagy E, Molina B, Pelham W. Association for Behavioral and Cognitive Therapies. New York, NY: 2009. Examining the decline of treatment use in adolescents with ADHD. Poster presented at the annual meeting of the. [Google Scholar]
- Bouchard S, Robillard G. Telepresence Scale–Validation results. Unpublished document. Available online at http://w3.uqo.ca/cyberpsy/en/index_en.htm, 2006; Mood induction procedures: A critical review. Encephale. 2006;34:233–239. [Google Scholar]
- Broten LA, Naugle AE, Kalata AH, Gaynor ST. Depression and a stepped care model. In: O’Donohue WT, Draper C, editors. Stepped-care and e-health: Practical applications to behavioral disorders. New York: Springer; 2011. [Google Scholar]
- Bussing R, Koro M, Noguchi K, Mason D, Mayerson G, Garvan C. Willingness to use ADHD treatments: a mixed methods study of perceptions by adolescents, parents, health professionals and teachers. Social Science and Medicine. 2012;74:92–100. doi: 10.1016/j.socscimed.2011.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussing R, Zima BT, Mason DM, Porter PC, Garvan CW. Receiving treatment for attention-deficit hyperactivity disorder: do the perspectives of adolescents matter? Journal of Adolescent Health. 2011;49:7–14. doi: 10.1016/j.jadohealth.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Mental health surveillance among children-United Sates, 2005–2011. MMWR. 2013;62(Suppl 2):1–35. [PubMed] [Google Scholar]
- Chou T, Comer JS, Turvey CL, Karr A, Spargo G. Technical consierations for the delivery of real-time child telemental health care. Journal of Child and Adolescent Psychopharmacology. 2016 doi: 10.1089/cap.2015.0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Barlow DH. The occasional case against broad dissemination and implementation: Retaining a role for specialty care in the delivery of psychological treatments. American Psychologist. 2014;69:1–18. doi: 10.1037/a0033582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Myers KM. Future directions in the use of telemental health to improve the accessibility and quality of children’s mental health services. Journal of Child and Adolescent Psychopharmacology. 2016 doi: 10.1089/cap.2015.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Cooper-Vince C, Madigan RJ, Chow C, Chan, et al. Rationale and considerations for the Internet-based delivery of Parent-Child Interaction Therapy. Cognitive and Behavioral Practice. 2015;22:302–316. doi: 10.1016/j.cbpra.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Cooper-Vince CE, Kerns CE, Chan PT, Edson AL, et al. Internet-Delivered, Family-Based Treatment for Early-Onset OCD: A Preliminary Case Series. Journal of Clinical Child and Adolescent Pscyhology. 2014 doi: 10.1080/15374416.2013.855127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS. Introduction to the special section: Applying new technologies to extend the scope and accessibility of mental health care. Cognitive and Behavioral Practice. 2015;22:253–257. [Google Scholar]
- Crum KI, Comer JS. Using synchronous videoconferencing to deliver family-based mental health care. Journal of Child and Adolescent Psychopharmacology. 2016 doi: 10.1089/cap.2015.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans S, Schultz B, DeMars C, Davis H. Effectiveness of the Challenging Horizons program for young adolescents with ADHD. Behavior Therapy. 2011;42:462–474. doi: 10.1016/j.beth.2010.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabiano GA, Pelham WE, Pisecco S, Evans SW, Manos MJ, Caserta D, et al. A Nationally Representative Survey of Classroom-based, Behavior Modification Treatment for ADHD. Poster presented at the Association for the Advancement of Behavior Therapy Conference; Reno, NV. 2002. [Google Scholar]
- Fabiano GA, Pelham WE, Jr, Waschbusch DA, Gnagy EM, Lahey BB, Chronis AM, … Burrows-MacLean L. A practical measure of impairment: psychometric properties of the impairment rating scale in samples of children with attention deficit hyperactivity disorder and two school-based samples. Journal of Clinical Child and Adolescent Psychology. 2006;35:369–385. doi: 10.1207/s15374424jccp3503_3. [DOI] [PubMed] [Google Scholar]
- Fischer M, Barkley RA, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: II. Academic, attentional, and neuropsychological status. Journal of Consulting and Clinical Psychology. 1990;58(5):580. doi: 10.1037//0022-006x.58.5.580. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Lee T. Multisystemic treatment of serious clinical problems. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. New York: Guilford; 2003. [Google Scholar]
- Horrigan JB. Home broadband adoption 2009. Pew Internet & American Life Project; 2009. Retrived from http://www.pewinternet.org/files/old-media/Files/Reports/2009/Home-Broadband-Adoption-2009.pdf on February 9, 2016. [Google Scholar]
- Kent KM, Pelham WE, Jr, Molina BS, Sibley MH, Waschbusch DA, Yu J, et al. The academic experience of male high school students with ADHD. Journal of Abnormal Child Psychology. 2011;39:451–62. doi: 10.1007/s10802-010-9472-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer GM, Kinn JT, Mishkind MC. Legal, regulatory, and risk management issues in the use of technology to deliver mental health care. Cognitive & Behavioral Practice. 2015;22:258–268. [Google Scholar]
- Kuriyan AB, Pelham WE, Jr, Molina BS, Waschbusch DA, Gnagy EM, Sibley MH, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. Journal of Abnormal Child Psychology. 2013;41:27–41. doi: 10.1007/s10802-012-9658-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977:159–174. [PubMed] [Google Scholar]
- Langberg JM, Dvorsky MR, Evans SW. What specific facets of executive function are associated with academic functioning in youth with attention-deficit/hyperactivity disorder? Journal of Abnormal Child Psychology. 2013;41:1145–1159. doi: 10.1007/s10802-013-9750-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Lock J, Loeb K, Nicholls D. Academy for eating disorders position paper: The role of the family in eating disorders. International Journal of Eating Disorders. 2010;43:1–5. doi: 10.1002/eat.20751. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Moulton J. Lifetime criminality among boys with attention deficit hyperactivity disorder: A prospective follow-up study into adulthood using official arrest records. Psychiatry Research. 2008;160:237–246. doi: 10.1016/j.psychres.2007.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merriam SB. Qualitative Research and Case Study Applications in Education. San Francisco, CA: Josey-Bass; 1998. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Helping people change. New York: Guilford Press; 2013. [Google Scholar]
- Molina B, Hinshaw S, Swanson J, Arnold L, Vitiello B, Jensen P, et al. The MTA at 8 years: Prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore BA, O’Donohue WT. In Stepped Care and e-Health. New York: Springer; 2011. Evaluating a web-based cognitive behavioral intervention for the prevention and treatment of pediatric obesity. [Google Scholar]
- Moyers T, Martin T, Manuel J, Hendrickson S, Miller W. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Manuel JK, Ernst D. Motivational Interviewing Treatment Integrity Coding Manual 4.1. 2014 doi: 10.1016/j.jsat.2016.01.001. Unpublished Manual. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers K, Vander Stoep A, Zhou C, McCarty CA, Katon W. Effectiveness of a telehealth service delivery model for treating attention-deficit/hyperactivity disorder: A community-based randomized controlled trial. Journal of the American Academic of Child and Adolescent Psychiatry. 2015;54:263–274. doi: 10.1016/j.jaac.2015.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson EL, Davis K, Velasquez S. Telemental Health: Clinical, Technical, and Administrative Foundations for Evidence-Based Practice. New york: Elsevier; 2013. Ethical considerations in providing mental health services over videoteleconferencing. [Google Scholar]
- Nigg JT, Blaskey LG, Stawicki JA, Sachek J. Evaluating the endophenotype model of ADHD neuropsychological deficit: results for parents and siblings of children with ADHD combined and inattentive subtypes. Journal of Abnormal Psychology. 2004;113:614–621. doi: 10.1037/0021-843X.113.4.614. [DOI] [PubMed] [Google Scholar]
- O’Donohue WT, Draper C. Stepped care and e-health: Practical applications to behavioral disorders. New York: Springer; 2011. [Google Scholar]
- Patterson GR, Forgatch M. Parents and adolescents living together: Part 1: The basics. Eugene, OR: Castalia; 1987. [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade K, Milich R. Teacher ratings of DSM-III--R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Sattler JM, Dumont R. Assessment of children: WISC-IV and WPPSI-III Supplement. San Diego: Jerome M. Sattler, Publisher; 2004. [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan M, Schwab-Stone M. NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from pervious versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Schultz BK, Evans SW, Serpell ZN. Preventing failure among middle school students with attention deficit hyperactivity disorder: A survival analysis. School Psychology Review. 2009;38:14–27. [Google Scholar]
- Shirk SR, Saiz CC. Clinical, empirical, and developmental perspectives on the therapeutic relationship in child psychotherapy. Developmental Psychopathology. 1992;4:713–728. [Google Scholar]
- Sibley MH, Campez M, Perez A, Morrow AS, Merrill BM, Altszuler AR, et al. Parent Management of Organization, Time Management, and Planning Deficits among Adolescents with ADHD. Journal of Psychopathology and Behavioral Assessment. 2016 doi: 10.1007/s10862-015-9515-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley MH, Altszuler AR, Morrow AS, Merrill BM. Mapping the academic problem behaviors of adolescents with ADHD. School Psychology Quarterly. 2014;29:422–437. doi: 10.1037/spq0000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley MH, Kuriyan AB, Evans SW, Waxmonsky JG, Smith BH. Pharmacological and psychosocial treatments for ADHD in adolescents: An updated systematic review of the literature. Clinical Psychology Review. 2014;34:218–232. doi: 10.1016/j.cpr.2014.02.001. [DOI] [PubMed] [Google Scholar]
- Spargo G, Karr A, Turvey CL. Telemental health: clinical, technical and administrative foundations for evidence-based practice. Waltham: Elsevier; 2013. Technology options for the provision of mental health care through videoteleconferencing; pp. 135–151. [Google Scholar]
- Toplak M, Jain U, Tannock R. Executive and motivational processes in adolescents with Attention-Deficit-Hyperactivity Disorder. Behavior and Brain Functioning. 2005;1:1–8. doi: 10.1186/1744-9081-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. Computer and Internet Use in the United States: 2010. 2012 http://www.census.gov/hhes/computer/publications/2010.html.
- Wechsler D. The Wechsler intelligence scale for children—fourth edition. London: Pearson Assessment; 2004. [Google Scholar]
- Weiss G, Hechtman L. Hyperactive Children Grown Up. 2. New York: Guilford; 1993. [Google Scholar]
- Weisz JR, Hawley KM. Developmental factors in the treatment on adolescents. Journal of Consulting and Clinical Psychology. 2002;70:21–28. doi: 10.1037//0022-006x.70.1.21. [DOI] [PubMed] [Google Scholar]
- West BT, Welch KB, Galecki AT. Linear mixed models: a practical guide using statistical software. CRC Press; 2006. [Google Scholar]
- Wolraich ML, Wibbelsman CJ, Brown TE, Evans SW, Gotlieb EM, Knight JR, et al. Attention-Deficit/Hyperactivity Disorder among adolescents: A review of the diagnosis, treatment, and clinical implications. Pediatrics. 2005;115:1734–1746. doi: 10.1542/peds.2004-1959. [DOI] [PubMed] [Google Scholar]