INTRODUCTION
The parathyroid glands are 4 small paired glands usually intimately associated with the thyroid gland that regulate calcium homeostasis in the body by the production of parathyroid hormone (PTH). PTH increases serum levels of ionic calcium in the body by indirectly stimulating osteoclasts and bone resorption of calcium, promoting the reabsorption of calcium from the renal tubules, decreasing the reabsorption of renal phosphate, and increasing the activation of vitamin D to reabsorb calcium from the gastrointestinal system.1 Inappropriate production of PTH can lead to elevated serum levels of calcium. Primary hyperparathyroidism is diagnosed when the patient has hypercalcemia and hypophosphatemia with elevated or inappropriately normal levels of PTH.1 The condition primarily affects women in the fifth through seventh decades of life and can be associated with symptoms of fatigue, weakness, hypertension, bone pain, myalgias, depression, and psychotic illnesses.2 The culprit in primary hyperparathyroidism is usually a single parathyroid adenoma (89%), although hyperplasia (6%), multiple adenomas (4%), and, rarely, parathyroid carcinoma are other causes.2 The standard treatment for hyperparathyroidism secondary to parathyroid adenoma is surgical excision. In the past, preoperative imaging was unnecessary, as a bilateral cervical dissection was used to identify all 4 of the parathyroid glands and remove the offending gland. Today, preoperative imaging techniques to localize the adenoma are standard of care to identify and localize the abnormal gland so that minimally invasive, targeted surgical approaches can be used.3
We present a case of primary hyperparathyroidism in an adult female to highlight the role of diagnostic imaging in the diagnosis and preoperative planning of definitive surgical treatment.
HISTORY
A 53-year-old female of European decent with a remote history of multinodular goiter presented to her physician's office for an annual checkup. Laboratory blood test revealed hypercalcemia. Further workup by endocrinology revealed an elevated PTH, and the patient was diagnosed with hyperparathyroidism. The patient denied a history of pathologic fractures and complaints of mood instability/irritability, sleep disturbances, memory problems, kidney stones, joint pain, or abdominal pain. She reported a maternal family history of hyperparathyroidism requiring surgery.
RADIOGRAPHIC APPEARANCE
Ultrasound of the neck (Figure 1) and sestamibi nuclear medicine scan (Figure 2) to identify the presumed parathyroid adenoma revealed the previously diagnosed multinodular goiter but did not identify a parathyroid adenoma. However, computed tomography (CT) with 4-dimensional (4D) imaging (Figure 3) revealed a soft tissue nodule posterior to the right thyroid lobe with the imaging characteristics of a parathyroid adenoma. The patient subsequently underwent a successful parathyroidectomy with resolution postoperatively of her hypercalcemia and elevated PTH.
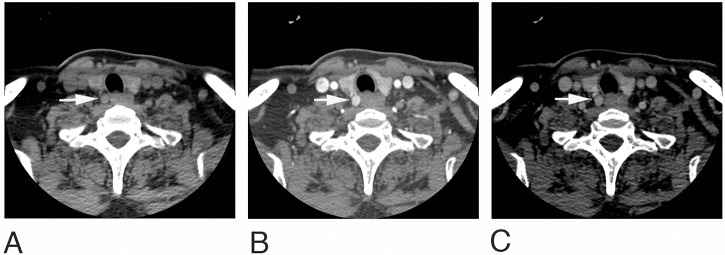
Figure 1.
Sonographic evaluation of the thyroid using grayscale and Doppler imaging demonstrates a heterogeneous solid nodule in the right lobe and a hypoechoic nodule in the left lobe but no evidence of a parathyroid adenoma in the neck.
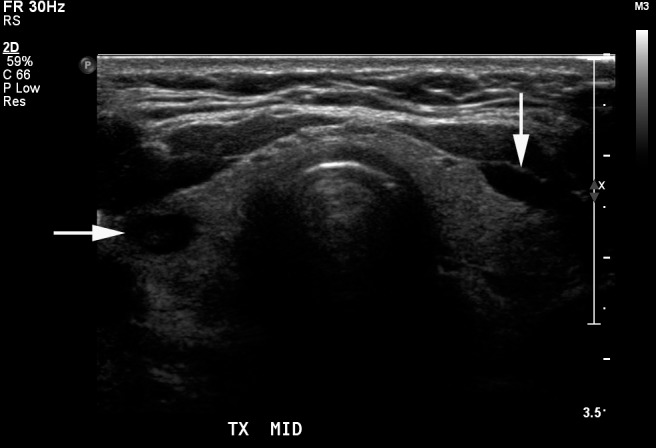
Figure 2.
Nuclear medicine sestamibi scan using 20.5 mCi of Technetium-99m sestamibi shows a heterogeneous distribution of the tracer within the thyroid gland compatible with multinodular goiter but no evidence of a parathyroid adenoma in the neck or mediastinum.
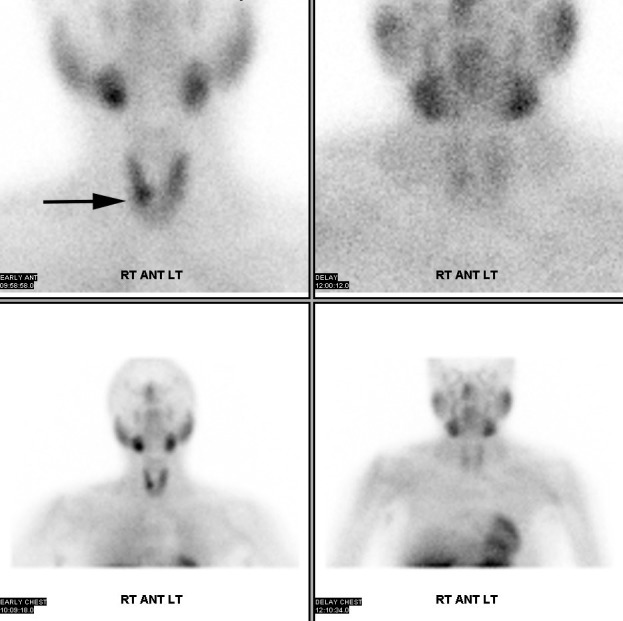
Figure 3.
Axial computed tomography scans of the neck before and after the administration of 75 cc Omnipaque 350 intravenous contrast show a subcentimeter soft tissue focus just posterior to the right lobe of the thyroid gland (arrow on all images). The nodule is of soft tissue attenuation on the noncontrast phase (A), is intensely hyperenhancing on the arterial phase (B), and washes out on the initial venous phase (C). These findings are compatible with a parathyroid adenoma.
DISCUSSION
In patients diagnosed with hyperparathyroidism, localization of a potential parathyroid adenoma or adenomas is important in preoperative planning because of the anatomy of the 2 pairs of parathyroid glands. The superior pair of glands is usually located in the mid-portion of the superior pole of the thyroid gland near the cricothyroid junction but can be found in the retroesophageal or retropharyngeal spaces or within the thyroid gland itself. The inferior pair of glands is usually located inferior, lateral, or posterior to the lower pole of the thyroid gland but can have a variable anatomy. The embryologic origin of the inferior glands from the third branchial cleft pouch allows the glands' position to vary widely from the mediastinum to even more cephalad than the superior pair of glands. This variant parathyroid anatomy stresses the importance of preoperative imaging in treating hyperparathyroidism.
Standard imaging performed prior to surgical treatment of hyperparathyroidism usually consists of ultrasound, sestamibi scan, or a combination of techniques with the goal of identifying a single adenoma to be removed. Multiple studies have reported the sensitivity for correctly identifying a single preoperative parathyroid adenoma with sonography to be 72%-89%, while the sensitivity of correctly identifying multinodular disease with sonography was 26%-40%.4-6 Preoperative scintigraphy with sestamibi Technetium-99m has yielded a similar range of sensitivity compared to preoperative ultrasound, ranging from 68%-95%, with similarly lower sensitivities for detecting multinodular disease.7 Combined preoperative ultrasound and sestamibi scans have demonstrated improved sensitivity compared to the individual techniques in correctly detecting single parathyroid adenomas from 79%-95% but still have low sensitivity for detecting multinodular disease.4 4D CT has emerged as an alternative preoperative imaging technique in the detection of parathyroid adenoma.
4D CT uses helical CT acquisition at 2.5-mm intervals from the base of the skull through the mediastinum to the level of the carina.8 The 4 phases of the examination include a noncontrast phase (Figure 3A), an arterial phase (Figure 3B), and 2 delayed phase venous images (Figure 3C) with coronal and sagittal reformatted images. Parathyroid adenomas typically demonstrate low attenuation on the noncontrast examination, peak enhancement on the initial arterial phase, and washout on progressive delayed phase imaging. Bahl et al have further characterized the enhancement characteristics, detailing 3 distinct parathyroid adenoma enhancement patterns relative to the thyroid on postcontrast 4D CT: hypoattenuating, hyperattenuating, or isoattenuating to the thyroid.9
Studies have demonstrated improved or equivalent sensitivity and specificity in diagnosing and localizing single parathyroid adenomas. Hunter et al found that 4D CT localized a single parathyroid adenoma to a particular side 96.5% of the time and to a particular quadrant in the neck 86.6% of the time.10 Chazen et al found that 4D CT localized single parathyroid adenomas with an accuracy of 93%11 but that sensitivity for multiglandular disease was significantly reduced with 4D CT to 44%, similar to findings for scintigraphy (30%)2 and ultrasound (40%).5 Multigland disease is presumed to be more difficult to detect on all imaging modalities, including 4D CT, as the size of the parathyroid adenomas is significantly smaller than in single-gland disease.11
As this case demonstrates, 4D CT is an effective tool for diagnosing and localizing single parathyroid adenomas for presurgical planning. Our discussion suggests that 4D CT is as effective, if not more effective, as other imaging modalities and has the potential to be the sole imaging modality for such purposes.
ACKNOWLEDGMENTS
The authors have no financial or proprietary interest in the subject matter of this article.
REFERENCES
- 1. Essig GF Jr Kramer S. . Parathyroid physiology. Medscape. http://emedicine.medscape.com/article/874690-overview#showall. Updated September 7, 2016. Accessed January 23, 2017.
- 2. Ruda JM, Hollenbeak CS, Stack BC Jr.. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg. 2005. March; 132 3: 359- 372. [DOI] [PubMed] [Google Scholar]
- 3. Gupta VK, Yeh KA, Burke GJ, Wei JP. . 99m-Technetium sestamibi localized solitary parathyroid adenoma as an indication for limited unilateral surgical exploration. Am J Surg. 1998. November; 176 5: 409- 412. [DOI] [PubMed] [Google Scholar]
- 4. Johnson NA, Tublin ME, Ogilvie JB. . Parathyroid imaging: technique and role in the preoperative evaluation of primary hyperparathyroidism. AJR Am J Roentgenol. 2007. June; 188 6: 1706- 1715. [DOI] [PubMed] [Google Scholar]
- 5. Haciyanli M, Lal G, Morita E, Duh QY, Kebebew E, Clark OH. . Accuracy of preoperative localization studies and intraoperative parathyroid hormone assay in patients with primary hyperparathyroidism and double adenoma. J Am Coll Surg. 2003. November; 197 5: 739- 746. [DOI] [PubMed] [Google Scholar]
- 6. Sugg SL, Krzywda EA, Demeure MJ, Wilson SD. . Detection of multiple gland primary hyperparathyroidism in the era of minimially invasive parathyroidectomy. Surgery. 2004. December; 136 6: 1303- 1309. [DOI] [PubMed] [Google Scholar]
- 7. Hunter GJ, Ginat DT, Kelly HR, Halpern EF, Hamberg LM. . Discriminating parathyroid adenoma from local mimics by using inherent tissue attenuation and vascular information obtained with four-dimensional CT: formulation of a multinomial logistic regression model. Radiology. 2014. January; 270 1: 168- 175. 10.1148/radiol.13122851. [DOI] [PubMed] [Google Scholar]
- 8. Hoang JK, Sung WK, Bahl M, Phillips CD. . How to perform parathyroid 4D CT: tips and traps for technique and interpretation. Radiology. 2014. January; 270 1: 15- 24. 10.1148/radiol.13122661. [DOI] [PubMed] [Google Scholar]
- 9. Bahl M, Sepahdari AR, Sosa JA, Hoang JK. . Parathyroid adenomas and hyperplasia on four-dimensional CT scans: three patterns of enhancement relative to the thyroid gland justify a three-phase protocol. Radiology. 2015. November; 277 2: 454- 462. 10.1148/radiol.2015142393. [DOI] [PubMed] [Google Scholar]
- 10. Hunter GJ, Schellingerhout D, Vu TH, Perrier ND, Hamberg LM. . Accuracy of four-dimensional CT for the localization of abnormal parathyroid glands in patients with primary hyperparathyroidism. Radiology. 2012. September; 264 3: 789- 795. 10.1148/radiol.12110852. [DOI] [PubMed] [Google Scholar]
- 11. Chazen JL, Gupta A, Dunning A, Phillips CD. . Diagnostic accuracy of 4D-CT for parathyroid adenomas and hyperplasia. AJNR Am J Neuroradiol. 2012. March; 33 3: 429- 433. 10.3174/ajnr.A2805. [DOI] [PMC free article] [PubMed] [Google Scholar]