Abstract
Background:
Five medical students traveled with 4 doctors and a medical photographer to Mayaya, La Victoire, Haiti, as part of a Medicine in Society rotation to provide medical care to the indigenous population.
Methods:
Preparation for the trip involved special study in identifying microbes and using blood analysis equipment; work in a clinic for underserved people in the New Orleans, LA, area; background reading; Haitian dialect classes; and development of ideas for streamlining clinic operations.
Results:
During the week in country, the healthcare team saw 472 patients and made more than 1,100 diagnoses. A shortage in almost all needed medications was one of the biggest challenges.
Conclusion:
Each aspect of the pretrip training was useful but did not prepare the students for the conditions in the poorest country in the Western Hemisphere. Overall, the clinic functioned smoothly, and each student had an important role to play each day. Medicine in Society-Haiti gave the medical students a completely new perspective on medicine as they experienced firsthand the ethical dilemma of resource scarcity.
Keywords: Developing countries, global health, health resources
INTRODUCTION
Christopher Columbus “discovered” Hispañola in 1492 and claimed it for the Spanish. Later, French buccaneers claimed parts of the island as well. The native Taínos were killed off by infectious disease epidemics brought by the colonizers. Hispañola was divided in 1697, with the French taking what today is called Haiti, and the Spanish receiving the Dominican Republic. Under the French, Haiti became a lucrative colony of sugar plantations and slaves imported from Africa. Subsequently, in 1804, it became the first independent former slave nation in the world after a revolt started by Toussaint L'Ouverture, a former slave, and completed by Jean-Jacques Dessalines, a former French army officer. Today, Haiti is a democratic nation.
Haiti has the worst health indicators in the Western Hemisphere. Less than half of the population has access to clean water, and vector-borne diseases such as dengue and chikungunya are persistent.1,2 Less than 3% of Haitians have healthcare coverage, and 72% of Haitians live on less than $2 per day.3,4 The United Nations (UN) Human Development Index (HDI) ranks countries on their achievement in key dimensions of human development and is based on life expectancy, education, and per capita income indicators. Haiti scores low on the HDI and is in the lowest quartile of development in the world (Figure 1).5
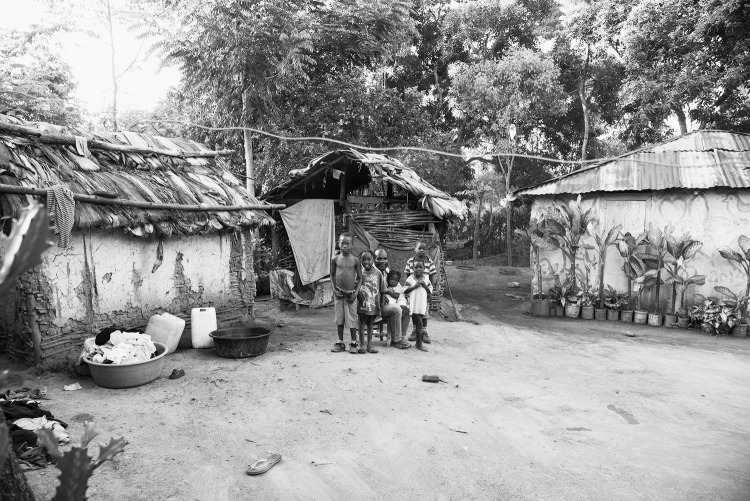
Figure 1.
The population of Mayaya, La Victoire, is extremely poor. Haiti is in the lowest quartile of development in the world as measured by the United Nations Human Development Index. (To see this image in color, click to https://education.ochsner.org/publishing-services/toc/laborde-16-0063-fig1.)
In 2010, a magnitude 7.0 earthquake hit the island, killing approximately 200,000 people, injuring more than 300,000 people, and displacing 1.5 million people. Thirty-seven of Haiti's 48 hospitals were out of service, including key universities and nursing schools in the capital of Port-au-Prince. Following the earthquake's devastation, a cholera outbreak, brought to the country by UN forces, started in the center of the country and spread nationwide within slightly more than a month. From October 2010 to December 2013, more than 697,000 cholera cases were reported to Haiti's National Cholera Surveillance System.6 Lack of access to safe drinking water and of proper sanitation practices increased the morbidity and mortality of cholera and other diarrheal diseases.7
After the earthquake, Dr Yvens Laborde, a native Haitian who is a medical director and physician at Ochsner Health System, established the Fondation de Dr Yvens Laborde de la Sante et l'Aide Humanitarian en Haiti (FONDYLSAHH). This foundation is focused on self-reliance and sustainability; is located in Mayaya, La Victoire; and supports the community with a clinic, school, housing for orphans, a well, and agricultural and community projects. The Ochsner Haitian Relief Fund works with FONDYLSAHH to help with ongoing relief efforts.
THE OCHSNER CLINICAL SCHOOL CONNECTION WITH HAITI
In November 2012, the government of Haiti and Ochsner Health System began a medical teaching partnership to enhance the healthcare delivery system in Haiti as the country continued to recover from the 2010 earthquake. This mutually beneficial relationship gives Ochsner the opportunity to pursue its mission to be a global leader in healthcare and provides an immersive experience for Ochsner medical students who are interested in international health. The elective Haiti experience is available to medical students as part of The University of Queensland-Ochsner Clinical School Medicine in Society rotation. The goal of the Medicine in Society rotation is to provide medical students the opportunity to understand and experience the benefits and challenges of clinical practice among population groups or in communities that face access and equity challenges associated with health service delivery. The rotation gives students a global view of clinical medicine that contextualizes how factors such as poverty, geographic isolation, socioeconomic status, religion, culture, ethnicity, and political events can adversely affect the health of individuals and populations.
Four Ochsner Clinical School students participated in the inaugural trip to Haiti in 2012. The authors of this article are the fourth group of medical students to visit the clinic in Mayaya for one week as a part of the Medicine in Society-Haiti rotation. We traveled to Haiti with 4 doctors and a medical photographer.
PRETRIP PREPARATION
The rotation started with intensive trip preparation. Our pretrip goals were to fundraise for medical supplies, become versed in Haitian history and public health, and plan a system that we could implement to streamline care at FONDYLSAHH. We were also provided with classes in the Creole dialect and clinical experiences to prepare us for our in-country experience.
The weeks leading up to our time in country prepared us for a variety of presentations and treatment options available in a country with limited resources. We each spent several clinic sessions with doctors working at the EXCELth clinic in New Orleans, LA. This urban clinic is government funded and serves low-income patients with primary care, obstetrics, behavioral management, dietary services, and pediatrics. Retrospectively, working in an underserved community helped us understand the similarities between New Orleans and the rural Haitian clinic that we previously had not realized existed.
In addition to our clinic time, we also spent time in a microbiology laboratory reviewing how to create and analyze smears and stains. We learned how to identify common microbes causing vaginitis, which resulted in a number of accurate diagnoses thanks to the addition of a microscope to the clinic this year. We were also trained to use i-STAT machines that, for the first time in the Haitian clinic's history, allowed us to analyze common and important laboratory values from our patients' blood.
Finally, we were given a reading list with books and articles that would introduce us to Haiti's current state of development. The literature focused on public health but included social, political, and economic aspects as well. The most influential and inspiring book we read was Mountains Beyond Mountains, an account of Dr Paul Farmer's aid work in one of the poorest regions in Haiti.
Obtaining the equipment and supplies for the clinic took significant effort. A large part of our rotation was holding events to support the Haitian Relief Fund and our week abroad. With the help of next year's group of students traveling to Haiti, we held several fundraisers: a movie screening, a silent auction, a Saints' football package raffle, Haitian art and fair-trade Haitian coffee sales, and a bar night. As a group, we raised more than $13,000.
PLANNING VS PRACTICE
One of our goals, which Dr Laborde emphasized, was to improve upon the contributions made by previous classes, and the process started months before the trip with meetings that focused on how to streamline clinic operations and data collection. As a group, we came up with 4 ideas that we believed would help the clinic run more efficiently and enable us to see more patients each day: issuing an identification (ID) card to each patient upon arrival at the clinic, giving each patient a pharmacy card with medication instructions, collecting data for a rudimentary electronic medical record (EMR) system, and conducting daily debriefings about the day's events.
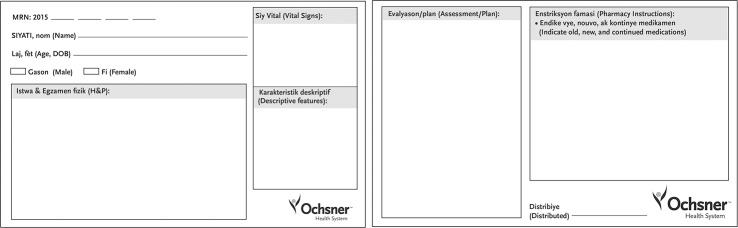
The ID card was originally envisioned as having a medical record number (MRN) for each patient and his/her photograph. We anticipated that patients would take their cards home after their clinic visit and bring them back for their next visit. This system would have enabled us to track their progress and progressively add to their documentation, developing information and history that would help us provide better patient care. However, because of logistics and time constraints, this plan did not work in practice. The clinic does not have internet access, so an EMR that could be updated continuously was not possible. Entering data into a computer from each encounter on a patient-by-patient basis would have been time consuming and would have led to fewer patients being seen per day. We were in the country for a short period and wanted to maximize the number of patients we treated. Therefore, we shifted gears slightly and developed a different ID card that combined what we believed to be the most important and feasible aspects of recordkeeping (Figure 2). Each patient did receive an MRN that was written at the top of the card along with the patient's name, age, and sex. One obstacle we discussed during the creation of this card was the fact that many of the people do not know their birthdays, so we decided to record age instead. The front of the card also includes boxes for noting vital signs, the history and physical examination findings, and descriptive characteristics of the patient. Because of budgetary constraints, we were not able to purchase a camera and film to take photos of each patient, so we opted to record descriptive characteristics as a compromise. The back of the card has space for the assessment and plan, as well as pharmacy instructions.
Figure 2.
The patient identification card includes spaces to record the patient's vitals, history and physical, descriptive characteristics, and treatment plan.
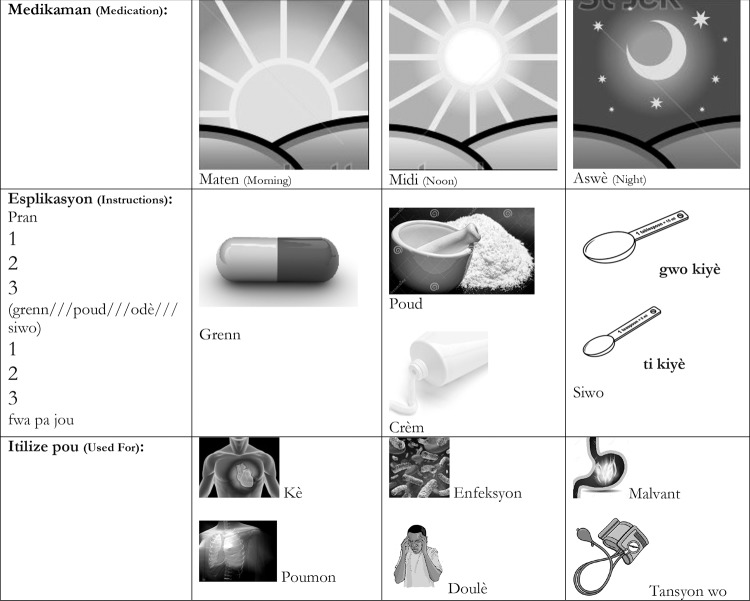
Another challenge was to design a pharmacy card that our patient population could easily understand and that the student in the pharmacy could complete quickly. During the previous year's rotation, the medical students simply wrote instructions on pieces of paper and gave the papers to the patients with their medications. This process resulted in backups at the pharmacy, and it was unclear whether the patients truly understood the instructions. To address this situation, we created a pharmacy card that included both pictures and written instructions (Figure 3). The pictures proved to be an essential aspect of the cards as not all people in the community were literate. We included pictures of the sun at 3 time points—morning, midday, and night—to indicate the time(s) of the day the medication should be taken. The card also includes pictures of a pill, powder, cream, syrup, tablespoon, and teaspoon; the dispensing student circled the appropriate medication type. All instructions included on the card were written in Creole, the dialect in Haiti. The next section showed what the medication was for, with depictions of the heart, lungs, an infection, pain, the gastrointestinal system, and high blood pressure. We selected these categories after talking to physicians who had previously been to the clinic and knew the most common complaints. The medical student in the pharmacy could quickly circle the applicable phrases and pictures on the card while giving the patient verbal instructions. This innovation improved pharmacy operations and enhanced patient understanding.
Figure 3.
The pictures on the pharmacy card facilitated patient understanding and increased the efficiency in the pharmacy as the dispensing student simply circled the applicable graphics. (To see this image in color, click to https://education.ochsner.org/publishing-services/toc/laborde-16-0063-fig3.)
CLINIC OPERATIONS
Just as previous students have done, we rotated through 5 stations. Each of us spent a day at triage, general practice, obstetrics and gynecology, laboratory, and pharmacy. By rotating through these 5 stations, we experienced the full range of patient care and health service delivery.
The first station in the clinic, the triage area, was the patio outside the clinic building, where throngs of patients were waiting to be seen and triaged (Figure 4). Vitals on each patient were taken by the attending physicians, students, or nurses, and then either the student or attending documented the patient's chief complaint. The primary attending physicians during our rotation were Dr Leise Knoepp of Ochsner and Dr Classaint Saint-Vil. Dr Saint-Vil is a Haitian physician who works primarily in the town of Cap-Haïtien but donates his time to help Dr Laborde in the clinic. Dr Saint-Vil's assistance was vital in translating the patients' chief complaints. Toward the end of the week, the clinic became extremely busy, and we noticed that most patients had straightforward and basic complaints. In response, we decided to start doing full clinic visits in the triage area. We conducted a full history and physical examination and wrote prescriptions that the patients took to the pharmacy. We estimate that this procedure change decreased the number of patients going to the clinic by 30%-40%, allowing the attending physicians in the clinic to focus on the patients with complicated presentations.
Figure 4.
In the busy triage area at the clinic, Ochsner medical student Aneesh Gupta (foreground) and Ochsner staff physician Dr Leise Knoepp assess patients. (To see this image in color, click to https://education.ochsner.org/publishing-services/toc/laborde-16-0063-fig4.)
After triage, the majority of patients went to one of two clinic rooms to see a physician, have their history taken, and undergo a physical examination. Patients with general complaints either saw Dr Obinna Nnedu, an infectious disease specialist at Ochsner, or Dr Laborde (Figure 5). In addition to the common ailments such as reflux, osteoarthritis, headaches, and fever, we saw a number of interesting and unusual cases such as trauma injuries, cerebrovascular accidents, undiagnosed growths, and probable myiasis (Figure 6). We performed minor procedures such as wound debridement, lipoma removal, and fracture splinting. We were assisted by the nurses who staffed the clinic, and they translated between patient and physician/student.
Figure 5.
Dr Yvens Laborde examines a patient at the FONDYLSAHH Clinic in Mayaya, La Victoire, Haiti. (To see this image in color, click to https://education.ochsner.org/publishing-services/toc/laborde-16-0063-fig5.)
Figure 6.
Among the cases seen in the clinic was a 54-year-old Haitian woman farmer with classic mucocutaneous signs and symptoms of what was clinically diagnosed as untreated systemic lupus erythematosus that led to her scarring and permanent alopecia. Because of the lack of access to laboratories and pathology at the clinic in Haiti, the clinicians must rely on their clinical and physical diagnosis skills. (To see this image in color, click to https://education.ochsner.org/publishing-services/toc/laborde-16-0063-fig6.)
All female patients with obstetric or gynecologic complaints saw Dr Shontell Thomas of Ochsner and Dr Phideline Jean. Dr Jean is a Haitian physician who completed her training in Cuba. She is fluent in Creole and translated what patients said. She is also fluent in Spanish and was thus able to communicate with Dr Thomas, who also speaks Spanish. Most of the patient complaints were vaginal discharge, itching, or pain. We also saw patients with amenorrhea related to pregnancy or menopause. We asked pregnant patients general questions about their pregnancy and measured their abdomens to determine if the size was appropriate for the dates. We had a few pregnancy tests we used for the first few days, but we ran out of them halfway through the week.
Patients who needed tests were sent to the laboratory. The laboratory contained all of the backup equipment for the clinic, as well as the tools needed to perform 3 main tests. If the patient had a urinary issue, we did a dipstick test on the urine; if the patient was suspected of having an infection, we used rapid test kits that analyzed blood for malaria, salmonella, or human immunodeficiency virus (HIV); if the patient needed a blood chemistry analysis, we used the i-STAT machine for a Chem 7 or Chem 8 blood test to obtain the patient's hemoglobin, hematocrit, sodium, potassium, anion gap, and bicarbonate levels, among others. The i-STAT machines were tricky to use because they have to be kept within a certain temperature range, and the clinic was quite hot. To keep the machines cool, we placed them in a cooler with ice packs or in a car with the air conditioning on at the maximum level. Once a patient's test results were available and written on his/her card, we walked the patient back to the clinic so that the physician could make the appropriate recommendations based on the laboratory results.
The last station was the pharmacy, a 2-room building situated between the house and the main clinic. We were fortunate to work with Miola, a tireless nurse, who worked 9-hour days without any breaks. Patients came to the front window with their patient card that contained prescriptions written by the physicians in the clinic. We dispensed the prescribed medications, putting each prescription into a separate resealable sandwich bag along with the pharmacy instruction card. Miola was fluent in Creole and French, and with her help, we instructed the patients in how to take their medications and answered their questions.
The medical student in the pharmacy collected the patient ID cards and stored them until the end of the day. At the end of each day, we compiled the data from all the patients into an Excel spreadsheet that served as our EMR. The EMR has various headings to enable easy extrapolation of the data for analysis and interpretation: all patient details (MRN, name, sex, age, vitals); diagnoses and corresponding treatments; laboratory values obtained from the i-STAT machines; infectious disease tests; and subcategories for urine pregnancy testing and urinalysis including leukocytes, nitrites, protein, glucose, and blood. Once all the data from the week were compiled, we could determine the average age of the people coming to the clinic, the most common diagnoses and treatments, and other important information such as whether we should be more selective about which patients receive various tests. This information is especially important in a setting where resources are very limited. This information can also be used by future classes to prepare for their trips and prevent obstacles to patient care, such as drug shortages.
In the spirit of always improving, we met on a nightly basis to discuss the day's events. No subject was off limits, and we took turns sharing what we thought worked well and what did not work well. These feedback sessions resulted in tangible process improvements. For example, on the first day of clinic, we worked until approximately 5:00 pm and saw approximately 75 patients. Toward the end of the week, we were finishing around 4:00 pm and were seeing approximately 120 patients per day. This communication forum enabled us to streamline certain aspects of the clinic process and to manage our time more efficiently. We also used our nightly debriefing sessions to share key Creole phrases we had learned. These tutorials facilitated better patient communication, and by the end of the week, we all had a diverse collection of useful phrases.
Throughout our 5 days of clinic we saw 472 patients, and more than 1,100 diagnoses were made (Figure 7). The patients had a wide variety of complaints, the most prevalent being gastroesophageal reflux disease (GERD). The prevalence of this diagnosis is hypothesized to be attributable to the chronic low-caloric intake of the people in this region, thus causing excess acid to accumulate in the stomach. The second most common diagnosis was hypertension. We were unable to determine whether the cases of hypertension were new or chronic. The third most common diagnosis was musculoskeletal pain, including conditions such as arthritis and low back pain. The fourth most common diagnosis was upper respiratory tract infection.
Figure 7.
Providing care during the Medicine in Society rotation at the FONDYLSAHH Clinic in Mayaya, La Victoire, Haiti were (back row from left) Ochsner medical students Timothy Ziethen and John Sisney and Ochsner staff physician Dr Obinna Nnedu; (middle row from left) Ochsner medical student Aneesh Gupta, Ochsner staff physicians Drs Leise Knoepp and Yvens Laborde, clinic nurse Enialikam Jean Francois, Ochsner medical student Marie Claire Lamb, medical photographer Shannon Caruso, Ochsner medical student Chantel Taylor, and clinic nurse Miola Elie; (front row from left) clinic nurse Widline Jean, Haitian physician Dr Phideline Jean, and Ochsner staff physician Dr Shontell Thomas. (To see this image in color, click to https://education.ochsner.org/publishing-services/toc/laborde-16-0063-fig7.)
Neuberger et al reported that the most common infectious diseases they saw in a primary care clinic in Haiti were respiratory tract infections, also our most common infectious disease, and suspected sexually transmitted infection.8 We treated a number of women for vaginitis, specifically bacterial and fungal vaginitis, hypothesized to occur because of the common practice for Haitian women to douche, thus disrupting the normal flora in their vaginas. We also treated two women for Trichomonas infection.
One difference between our rotation in Haiti and previous rotations was the lack of diarrhea complaints we encountered. This decrease is the direct result of the water well that was dug on the property next to the clinic (Figure 8). The well has virtually eliminated diarrheal diseases in the area of the clinic. People formerly captured dirty water from the nearby river or walked into the town center to try to get water from a well located there. The simple addition of a well has had a significant impact on the health of the people in Mayaya.
Figure 8.
The water well that was dug on the property next to the clinic has virtually eliminated diarrheal diseases in the area of the clinic. (To see this image in color, click to https://education.ochsner.org/publishing-services/toc/laborde-16-0063-fig8.)
We brought a wide variety of medications with us from the United States to treat the patients. Ranitidine was the most common GERD medication prescribed. The most common hypertension medication was lisinopril, but other options including hydrochlorothiazide, amlodipine, furosemide, and verapamil were used as well. For musculoskeletal pains, ibuprofen, acetaminophen, or aspirin was prescribed. The treatment for upper respiratory tract infections depended on whether a viral or bacterial infection was suspected. For suspected bacterial infections, either amoxicillin or doxycycline was prescribed. If viral infection was suspected, supportive treatment of ibuprofen, acetaminophen, dextromethorphan, or pseudoephedrine was prescribed.
The most common medication we dispensed during the week was multivitamins. We hoped to be able to give every patient some type of vitamin but because of our lack of resources, this was not possible. Following multivitamins, ranitidine was the second most common medication prescribed, followed by acetaminophen. While we were able to treat a wide range of medical complaints, we could not always follow first-line medication practices. We had limited medication resources, and our goal was to improve each patient's quality of life to some degree.
We could not treat some illnesses either because of low supplies or lack of access to treatment options. We referred a handful of patients to tertiary hospitals in Cap-Haïtien for diagnoses such as hernias, HIV, and tumors. We referred patients to specialists such as ophthalmologists and dentists. Such is the nature of a small free community clinic in a resource-poor area. We provided the best care we could with what we had available. We practiced a form of medical parsimony by using our resources wisely to ensure that they benefited the most people.
Overall, the clinic functioned smoothly, and each student had an important role each day. Students occasionally moved around to assist with an emergency or perform procedures such as lipoma removal, sutures, ganglion cyst aspiration, shave biopsies, speculum examinations, wound debridement and dressing, and orthopedic manipulation.
ADDITIONAL CHALLENGES
As explained earlier, the patient ID cards we designed have a space at the top of the card for the 8-digit patient MRN we needed for recordkeeping and the i-STAT machine. Each MRN began with the number 2015, followed by individual patient numbers that started with 0001. We numbered the first 200 cards, and the system functioned smoothly until we noticed that some of the cards were missing. After the second day, we saw that Mackenzie, the proprietor of the compound, had implemented a different numbering system, writing the numbers in highlighter on the bottom of the cards. However, some of the cards he gave to patients did not have MRNs, disrupting our data collection. Reconciling this problem was a great lesson in cultural differences and priorities. Our primary concern was organization, and Mackenzie's primary concern was fair distribution of ID cards to serve as entry passes into the clinic. After discussing what both parties were trying to accomplish, we reached a compromise that we all found suitable.
Another challenge was our miscalculation of the supplies we would need. We expected to see 500 patients during the week, so we printed 600 ID cards and 600 pharmacy instruction cards. We did not foresee that some patients would receive up to 4 prescriptions, each requiring a resealable plastic bag and individual pharmacy cards. Although we uncovered a stash of bags from previous trips, we completely ran out of pharmacy cards by the beginning of day 4. We addressed this situation by writing instructions on paper in the same format as the pharmacy cards had been printed. Although this manual process resulted in delays in the pharmacy, our patients benefited from having a record of their prescriptions and instructions on how to take them.
Our primary supply issue was the medication shortage. By the end of the first day, it was evident that we would need more antifungals to treat the high rates of tinea and yeast infections. We tried to stretch our supplies by splitting the bottles of ketoconazole shampoo and tubes of miconazole cream into smaller doses and giving them out in specimen cups. Despite these efforts, the ketoconazole shampoo, miconazole cream, and fluconazole were gone by the beginning of day 5. We had a low supply of nonsteroidal antiinflammatory drugs from the beginning, and we ran out of diclofenac on day 1. Dr Laborde produced a bottle each of acetaminophen and ibuprofen on day 2 from his luggage, but these bottles were empty before the end of the week. Other items we ran very low on or out of completely included diphenhydramine, metronidazole, doxycycline, ciprofloxacin, cephalexin, lisinopril, and amlodipine. Our other supply shortages were urine pregnancy tests, bluey pads for procedures, and rapid malaria cartridges. This information will be useful for future medical students going to Haiti as part of their Medicine in Society rotation to accurately estimate the amount of medications and supplies needed for this patient population.
CONCLUSION
Our efforts to streamline care through the use of patient ID cards and pharmacy cards at the FONDYLSAHH clinic in Mayaya, La Victoire, were successful. According to the staff physicians who have participated in the medical mission for the past few years, this trip was the most organized and efficient yet. Medical students were introduced to a socioeconomic situation they had never experienced before, along with a different language, culture, and political environment. Medicine in Society-Haiti gave 5 medical students a completely new perspective on medicine. We experienced firsthand the ethical dilemma of resource scarcity. We were also aware that many patients would not have follow-up, despite the fact the FONDYLSAHH clinic operates once a week. Resources are even more limited during these weekly openings. Finally, we experienced the practical application of our oath, “First, do no harm,” and let this adage guide us through our decisions from treatment commencement to minor procedures. The experience at the FONDYLSAHH clinic was the opportunity of a lifetime and will shape all of our careers as physicians.
The Medicine in Society-Haiti rotation is a tangible exposition of Ochsner's mission to serve, heal, lead, educate, and innovate on a global scale. The rotation gives fourth-year medical students an international health experience in an underdeveloped country with extremely limited resources. The students have the opportunity to provide primary care services to patients under safe and carefully supervised conditions. We look forward to the continual improvements and growth of this incredible organization in rural Haiti.
ACKNOWLEDGMENTS
The authors have no financial or proprietary interest in the subject matter of this article. Most photographs accompanying this article (and on this issue's cover) are by Ochsner medical photographer Shannon Caruso.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, Professionalism, and Systems-Based Practice.
REFERENCES
- 1. Hottinger DG, Patel BM, Frechette RL, Walent W, Augustin ME, Daly PJ. . Building surgical capacity in developing countries: lessons from Haiti and Honduras. J Health Care Poor Underserved. 2015. February; 26 1: 278- 286. 10.1353/hpu.2015.0011. [DOI] [PubMed] [Google Scholar]
- 2. World Bank. . Haiti, Honduras data repositories. Washington, DC: World Bank, 2011. https://databox.worldbank.org/. Accessed August 30, 2014.
- 3. Exantus J, Desrosiers F, Ternier A, Métayer A, Abel G, Buteau JH. . The need for dialysis in Haiti: dream or reality? Blood Purif. 2015; 39 1-3: 145- 150. 10.1159/000368979. [DOI] [PubMed] [Google Scholar]
- 4. Ministère de la santé publique et de la population. Country Planning Cycle Database Web site. http://www.nationalplanningcycles.org/sites/default/files/country_docs/Haiti/haiti_politique_national_de_sante_2012.pdf. Accessed August 30, 2014.
- 5. Human Development Index (HDI). Human Development Reports. United Nations Development Programme Web site. http://hdr.undp.org/en/content/human-development-index-hdi. Published 2015. Accessed August 30, 2014.
- 6. Lucien MA, Schaad N, Steenland MW, et al. Identifying the most sensitive and specific sign and symptom combinations for cholera: results from an analysis of laboratory-based surveillance data from Haiti, 2012-2013. Am J Trop Med Hyg. 2015. April; 92 4: 758- 764. 10.4269/ajtmh.14-0429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Watts J. . Haiti making good progress in health but challenges remain. Lancet. 2014. October 18; 384 9952: 1413- 1414. 10.1016/S0140-6736(14)61835-3. Erratum in: Lancet. 2014 Nov 8;384(9955):e56. [DOI] [PubMed] [Google Scholar]
- 8. Neuberger A, Tenenboim S, Golos M, et al. Infectious diseases seen in a primary care clinic in Leogane, Haiti. Am J Trop Med Hyg. 2012. January; 86 1: 11- 15. 10.4269/ajtmh.2012.11-0426. [DOI] [PMC free article] [PubMed] [Google Scholar]