Abstract
Rationale: Intraabdominal fibromatosis is a rare benign tumor that often affects the mesentery or retroperitoneum, and can infiltrate adjacent organs. However, it is rare for fibromatosis to arise from the small intestinal wall.
Patient concerns:
A 27-year-old female with a tangible abdominal tumor is described.
Diagnoses:
The computed tomography (CT) scan revealed a 7.5 cm, small intestine-associated tumor in the right abdomen.
Interventions:
The patient received tumor resection and intestinal anastomosis.
Outcomes:
Further pathological examination confirmed the tumor as a duodenal fibromatosis that infiltrated the intestinal wall. To the best of our knowledge, this is the first report of a duodenum-derived fibromatosis that invaded the muscular layer of the intestine.
Lessons:
Our study demonstrated that an unexplained abdominal mass should be noteworthy and properly treated.
Keywords: fibromatosis, small intestine
1. Introduction
Intraabdominal fibromatosis, also called abdominal desmoid, is a rare benign tumor.[1] It is prone to invading adjacent organs, but has a low tendency to induce distant metastasis.[1] Its detailed etiology remains unclear. Fibromatosis can be asymptomatic at the early stage; however, the symptoms caused by compression of nearby organs can occur as the tumor grows. Most studies have reported that intraabdominal fibromas arise from the small intestinal mesentery,[2,3] and other fibromas have been reported in abdominal ligands and the colon.[1] Moreover, they could arise from the small intestine wall directly. Currently, surgical resection remains the appropriate treatment for intraabdominal fibromatosis in most cases.[4]
As far as we know, the case presented in this study is the first report of duodenum-derived fibromatosis in which the tumor invaded the muscular layer of the intestinal wall.
2. Case report
This study was approved by the Ethics Committee and institutional review board of the second hospital of Jilin University, Changchun, China.
A 27-year-old woman attended our hospital with a tangible abdominal tumor for about 2 weeks. She denied any medical history, abdominal pain, abdominal distention, or abnormal stool. Physical examinations indicated a 7.0-cm hard mass, with poor activity. Laboratory tests revealed white blood cell count of 2.7 × 109 cells/L. Constant-enhanced computed tomography (CT) and 3-dimensional CT examinations showed a 7.5 × 5.8 × 5.4 cm oval mass with multiple vascular shadows in the right ascending colon area (Fig. 1A and B). In addition, the tumor mass was associated closely with the small intestine in the central abdomen. We considered that this might be a small intestine-derived mass, and fibromatosis could not be excluded.
Figure 1.
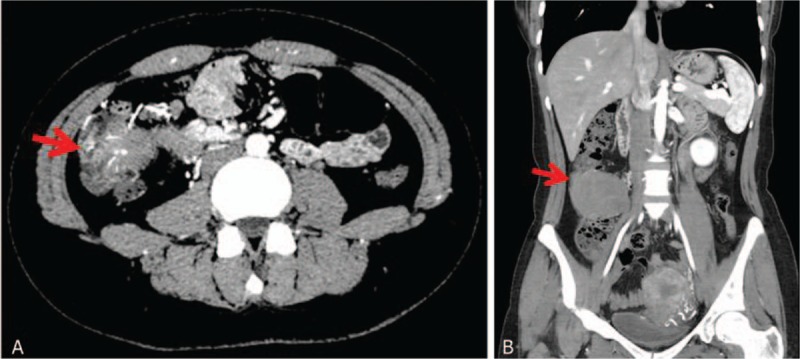
Contrast-enhanced computrd tomography (CT) (A) and three-dimensional CT (B) examinations of the abdominal fibromatosis. Red arrows indicate the abdominal fibromatosis.
On laparotomy, we found an 8-cm tumor in the horizontal section of the duodenum that was also connected to the ascending colon. The tumor was intact, and was not connected with intestinal mesenteries. Tumor mass resection, right colon resection, partial duodenum resection, and intestinal anastomosis were then performed. The gross pathology revealed that the tumor was intact, and almost the whole intestinal wall was invaded (Fig. 2A and B). Pathological examination confirmed intestinal fibromatosis, showing proliferation of spindle cells and large amounts of collagen in the intracellular space (Fig. 3). The muscular layer of the intestinal wall was totally infiltrated, whereas the mucosa layer remained intact. Immunohistological examination showed that the lesion was positive for actin and vimentin, but negative for CD34, CD117, S-100, and desmin. The patient recovered well and was discharged 1 week post-surgery. During 6 months of follow-up, the patient experienced no further complications.
Figure 2.
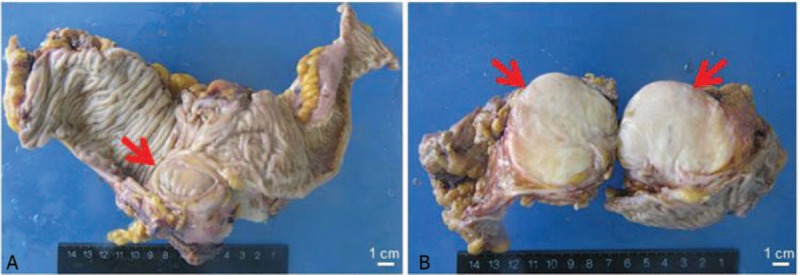
Gross pathology of the duodenum-derived fibromatosis. (A) The fibromatosis (red arrow) invaded almost the whole intestinal wall. (B) Transection of the fibromatosis (red arrows).
Figure 3.
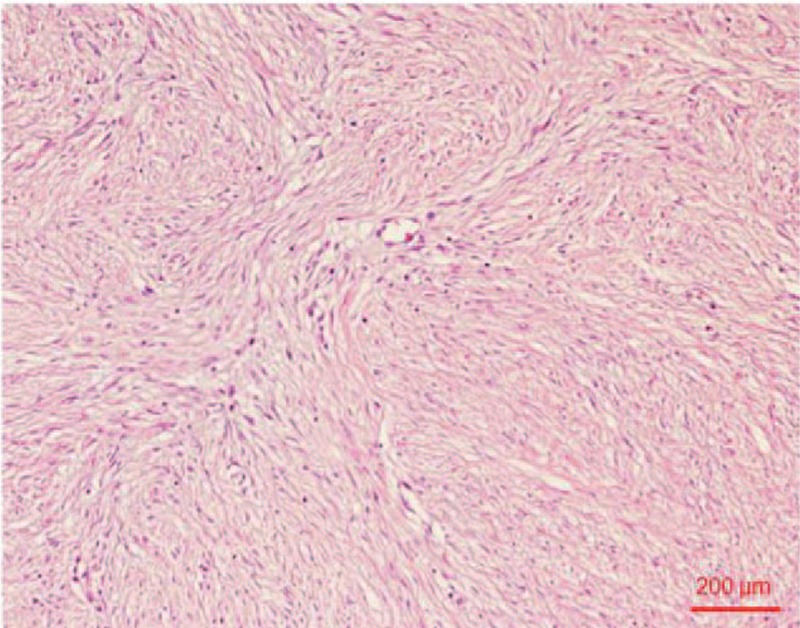
Histological examination (hematoxylin and eosin staining) of the fibromatosis.
3. Discussion
Fibromatosis, originated from the musculoaponeurotic structures of the body, includes a large group of nonneoplastic proliferative connective tissues. The etiology of fibromatosis is still unclear. However, it may be associated, for example, with Gardner syndrome, pregnancy, estrogen levels, and trauma.[1] Generally, intraabdominal fibromatosis originates mainly from the mesentery of the small intestine, the intestinal ligands, and the colon.[5] In rare cases, it can originate from the intestinal wall directly. Toydemir et al[5] reported a cecum-originated fibromatosis that caused acute appendicitis. In our study, the fibromatosis originated from the duodenum. To the best of our knowledge, this is the first case in which the duodenal-derived fibromatosis infiltrated almost the whole intestinal wall.
Aggression is a specific feature of fibromatosis; however, there are few reports of distant metastasis.[1] Usually, at the early stage of the intraabdominal fibromatosis, when the mass is small, patients remain clinically asymptomatic. As the volume of the fibromatosis enlarges, the tumor mass compresses and infiltrates adjacent organs, causing symptoms such as small bowel obstruction, intestinal perforation, acute peritonitis, hydronephrosis, and acute appendicitis. Misiak et al[1] reported a 36-year-old man with a mesenteric fibromatosis measuring 10 × 9 × 8 cm. The tumor caused abdominal pain, vomiting, nausea, and stoppage of bowel movements in this patient. However, even though the tumor can reach a large volume and compress the adjacent organs, the symptoms can be silent or vague. In a case reported by Gari et al,[6] a mesenteric fibromatosis reached 28 × 27 × 10 cm in size, and occupied almost the whole abdomen and pelvis. This patient only reported vague abdominal pain and the physical examination results were unremarkable. In our report, the fibromatosis mainly infiltrated the duodenum, and did not induce bowel obstruction or any other symptoms. The pathological examination indicated that the tumor infiltrated almost the whole intestine wall, only leaving the mucosal layer intact. We hypothesized that once the duodenum wall was totally invaded, intestinal perforation and acute peritonitis would be induced. As a result, as for other unexplained abdominal tumors, immediate diagnosis and appropriate treatment are important and necessary to avoid any secondary changes.
The presurgical diagnosis of intraabdominal fibromatosis depends mainly on imaging. On CT, a soft tissue mass with a slightly lower density is always indicated. In addition, an enhanced CT scan often shows uneven enhancement within the tumor.[7] However, the appearance of intraabdominal fibromatosis on a CT scan is untypical. On magnetic resonance imaging (MRI), especially the T1- and T2-weighted images, these tumors usually appear as having a low density, with plaque or star-like tissues inside. The enhanced scan might also reveal rich vessels within the tumors.[8] However, pathology is still the criterion standard to provide a concrete diagnosis of intraabdominal fibromatosis. Under microscopy, spindle cells arranged in bundles, surrounded by large amounts of collagen, could be seen. Immunohistological examination always indicates positive expression of vimentin and smooth muscle actin.[9]
Fibromatosis is highly aggressive and has a high local recurrence rate. For most intraabdominal fibromatosis, wide field surgical resection is the preferred treatment method. In our case, the tumor mass, right colon, and partial duodenum were resected to avoid any residual tumor and recurrence. No sign of tumor recurrence was noted during 6 moths of follow-up. Radiotherapy is also an important treatment method for fibromatosis, which can be used before surgery to shrink the tumor and make it operable.[10] For those patients who are not suitable for surgery or radiotherapy, systematic agents, such as antiproliferative and cytotoxic agents, can also be applied.
In the reported case, the fibromatosis started in the duodenum and invaded the muscular layer of the intestinal wall, which is very rare. Our study also demonstrated that an unexplained abdominal mass should be noted, diagnosed carefully, and treated appropriately to avoid any secondary changes.
Footnotes
Abbreviations: CT = computed tomography, MRI = magnetic resonance imaging.
The authors report no conflicts of interest.
References
- [1].Misiak P, Piskorz L, Wcislo S, et al. Giant mesentery fibromatosis presenting as acute abdomen—case report. Contemporary oncology (Poznan, Poland) 2013;17:468–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Faria SC, Iyer RB, Rashid A, et al. Desmoid tumor of the small bowel and the mesentery. AJR Am J Roentgenol 2004;183:118. [DOI] [PubMed] [Google Scholar]
- [3].Bethune R, Amin A. Mesenteric fibromatosis: a rare cause of acute abdominal pain. Ann Royal Coll Surg England 2006;88:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Levy AD, Rimola J, Mehrotra AK, et al. From the archives of the AFIP: benign fibrous tumors and tumorlike lesions of the mesentery: radiologic-pathologic correlation. Radiographics 2006;26:245–64. [DOI] [PubMed] [Google Scholar]
- [5].Toydemir T, Ertugrul G. Fibromatosis of the cecum presenting with acute appendicitis: a case report. Int J Gen Med 2012;5:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Gari MK, Guraya SY, Hussein AM, et al. Giant mesenteric fibromatosis: Report of a case and review of the literature. World J Gastrointest Surg 2012;4:79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Brooks AP, Reznek RH, Nugent K, et al. CT appearances of desmoid tumours in familial adenomatous polyposis: further observations. Clin Radiol 1994;49:601–7. [DOI] [PubMed] [Google Scholar]
- [8].Sheth PJ, Del Moral S, Wilky BA, et al. Desmoid fibromatosis: MRI features of response to systemic therapy. Skeletal Radiol 2016;45:1365–73. [DOI] [PubMed] [Google Scholar]
- [9].Rakha EA, Kandil MA, El-Santawe MG. Gigantic recurrent abdominal desmoid tumour: a case report. Hernia 2007;11:193–7. [DOI] [PubMed] [Google Scholar]
- [10].Nuyttens JJ, Rust PF, Thomas CR, Jr, et al. Surgery versus radiation therapy for patients with aggressive fibromatosis or desmoid tumors: A comparative review of 22 articles. Cancer 2000;88:1517–23. [PubMed] [Google Scholar]


