Abstract
Background:
Compression neuropathy of the ulnar nerve at the Guyon canal is commonly seen by hand surgeons. Different anatomical variations of structures related to the Guyon canal have been reported in the literature. A thorough knowledge of the normal contents and possible variations is essential during surgery and exploration.
Objectives:
To review the recognized anatomical variations within and around the Guyon canal.
Methods:
This study is a narrative review in which relevant papers, clinical studies, and anatomical studies were selected by searching electronic databases (PubMed and EMBASE). Extensive manual review of references of the included studies was performed. We also describe a case report of an aberrant muscle crossing the Guyon canal.
Results:
This study identified several variations in the anatomical structures of the Guyon canal reported in the literature. Variations of the ulnar nerve involved its course, branching pattern, deep motor branch, superficial sensory branch, dorsal cutaneous branch, and the communication with the median nerve. Ulnar artery variations involved its course, branching pattern, the superficial ulnar artery, and the dorsal perforating artery. Aberrant muscles crossing the Guyon canal were found to originate from the antebrachial fascia, pisiform bone, flexor retinaculum, the tendon of palmaris longus, flexor carpi ulnaris, or flexor carpi radialis; these muscles usually fuse with the hypothenar group.
Conclusion:
The diverse variations of the contents of the Guyon canal were adequately described in the literature. Taking these variations into consideration is important in preventing clinical misinterpretation and avoiding potential surgical complications.
Keywords: Guyon canal, ulnar tunnel, anatomy, variations, ulnar nerve, ulnar artery, hypothenar
Abstract
Historique :
Les chirurgiens de la main observent souvent une neuropathie par compression du nerf ulnaire au niveau de la loge de Guyon. Les publications font état de diverses variations anatomiques des structures liées à la loge de Guyon. Il est essentiel d’avoir une connaissance approfondie des contenus normaux et des variations possibles pendant l’opération et l’exploration.
Objectifs :
Analyser les variations anatomiques connues dans la loge de Guyon et à proximité.
Méthodologie :
La présente étude est une analyse narrative pour laquelle les auteurs ont sélectionné les articles pertinents, les études cliniques et les études anatomiques après des recherches dans des bases de données électroniques (PubMed et EMBASE). Ils ont procédé à un dépouillement manuel approfondi des études retenues. Ils décrivent également le rapport de cas d’un muscle aberrant traversant la loge de Guyon.
Résultats :
La présente étude a permis de constater plusieurs variations des structures anatomiques de la loge de Guyon exposées dans les publications. Les variations du nerf ulnaire incluaient le trajet, le mode de ramification, la branche motrice profonde, la branche sensorielle superficielle, la branche cutanée dorsale et la communication avec le nerf médian. Les variations de l’artère ulnaire incluaient le trajet, le mode de ramification, l’artère ulnaire superficielle et l’artère perforante dorsale. Les muscles aberrants qui traversaient la loge de Guyon provenaient du fascia antébrachial, de l’os pisiforme, du rétinaculum des fléchisseurs, du tendon du fléchisseur radial du carpe, du fléchisseur ulnaire du carpe ou du fléchisseur radial du carpe. Ces muscles fusionnent habituellement avec le groupe de l’éminence hypothénar.
Conclusion :
Les diverses variations des contenus de la loge de Guyon étaient bien décrites dans les publications. Il est important d’en tenir compte pour prévenir les mauvaises interprétations cliniques et éviter les complications chirurgicales.
Introduction
The Guyon canal is the narrow space located in the wrist through which the ulnar nerve and artery pass. It is named after the French surgeon Jean Casimir Félix Guyon, who originally described it in 1861.1 The Guyon canal is recognized as a potential site of pathology leading to ulnar nerve compression. The compression of the ulnar nerve in the wrist was described in 3 different zones.2,3 Zone I compression occurs proximal to or within the Guyon canal, before the nerve bifurcation, and presents with combined motor and sensory deficits. Zone II compression, involving only the deep motor branch, occurs as the ulnar nerve exits the Guyon canal or at the hook of the hamate level. Zone III compression, with isolated superficial sensory branch involvement, may also occur as the nerve exits the Guyon canal or at the hook of the hamate distal to the bifurcation. Several anatomical variations in the Guyon canal and the surrounding compression zones were reported. A thorough knowledge of these variations is critical both during clinical assessment and surgical release of the nerve.
This study is a narrative review of relevant papers selected by searching electronic databases (PubMed and EMBASE). Extensive manual review of references of the included studies was also performed. We reviewed the recognized variations in the anatomical structures related to the Guyon canal including nerves, vessels, muscles, and tendons. In addition, we are reporting a case of an aberrant muscle crossing the Guyon canal. The patient granted full consent for photographic documentation and publication of clinical information in the present article.
Normal Anatomy
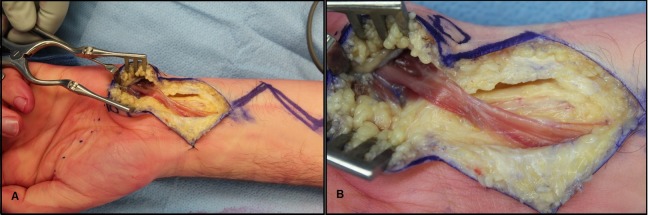
The Guyon canal is situated between the pisiform and the hook of the hamate in the proximal hypothenar region (Figure 1). Within the Guyon canal, the ulnar nerve usually lies slightly deep and ulnar to the ulnar artery. The canal also contains the vena comitans of the ulnar artery in addition to connective fatty tissue. It measures approximately 40 to 45 mm in length, extending from the proximal edge of the palmar carpal ligament to the fibrous arch of the hypothenar muscles at the level of the hook of the hamate distally.3–6 The boundaries of the Guyon canal are formed by several surrounding anatomical structures. The palmar carpal ligament, palmaris brevis, and hypothenar connective tissue form the roof of the canal. The structures forming the floor of the canal include the transverse carpal ligament, pisohamate ligament, pisometacarpal ligament, and the tendons of the flexor digitorum profundus and opponens digiti minimi. The medial wall is formed by the pisiform, the abductor digiti minimi, and the tendon of the flexor carpi ulnaris. The lateral wall boundaries of the canal are the hook of the hamate, the transverse carpal ligament, and the flexor tendons.3–8
Figure 1.
Anatomy of the Guyon canal. Reproduced with permission license (Polatsch 20074, Hand Clinic).
Variations of the Ulnar Nerve
Overview
The ulnar nerve typically divides into 2 terminal branches within the Guyon canal, the superficial sensory branch and the deep motor branch. The former runs distally over the hypothenar muscles and bifurcates into the common digital nerve of the ring finger and the ulnar proper digital nerve of the little finger. The deep branch passes through the canal and turns around the medial side of the hook of hamate and continues on a distal and radial course to reach the deep palmar space.3–6,9–11 Table 1 summarizes the ulnar nerve anomalies within and around the Guyon canal.
Table 1.
Anomalies of the Ulnar Nerve Within and Around the Guyon Canal.
| Ulnar Nerve Anomalies |
|---|
Branching pattern
|
Deep motor branch
|
Superficial sensory branch
|
Anomalous course
|
Communication with median nerve
|
Dorsal cutaneous branch
|
Variation in the Terminal Division of the Ulnar Nerve
In the literature, several ways in which the ulnar nerve divides in the Guyon canal were described. The most commonly described patterns are bifurcation, trifurcation, and anomalies of these divisions. These patterns were described radiologically by Niitsu et al,12 who reported that bifurcation occurs within the canal (distal to the mid-portion of the pisiform), just past the inlet of the canal (the proximal portion of the pisiform) and prior to entering the canal. Trifurcation pattern may occur by the division of the ulnar nerve into 2 branches, one of which further divides, resulting in 3 branches exiting the canal. Another reported trifurcation pattern of the ulnar nerve in the Guyon canal is the direct division into 3 branches at the proximal portion of the pisiform.
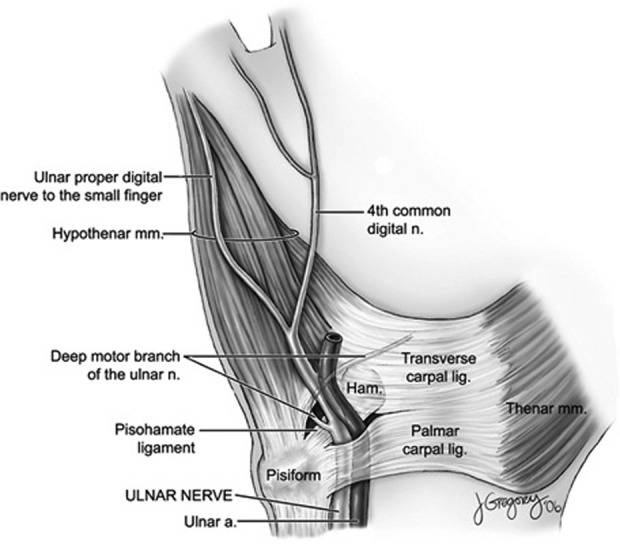
Murata et al10 explicitly classified the division patterns of the ulnar nerve (Figure 2). The most frequent pattern observed in the literature was bifurcation of the ulnar nerve into deep motor branch and superficial trunk distal to the distal border of pisiform. The superficial trunk further divides into the ring finger common digital nerve and the ulnar proper digital nerve of the little finger. This type has a frequency of occurrence that ranged from 66% to 86%.10–14 Moreover, the main ulnar trunk may trifurcate into a deep motor branch, the fourth common digital nerve and the ulnar proper palmar digital nerve of the little finger just past the distal border of pisiform. Trifurcation of the ulnar nerve has been fairly described in multiple anatomical studies, and it occurs in 13% to 22% of people. Cases with trifurcation proximal to the Guyon canal have been rarely reported, and in 1 case, 1 of 3 branches passed solely underneath the flexor retinaculum.9,11 In rare cases, the ulnar nerve bifurcates around the pisiform and reunites distal to the pisiform in an encircling pattern.15,16
Figure 2.
Variation of the branching pattern of the ulnar nerve in the Guyon canal. A, Bifurcation (66%-86%). B, Trifurcation (13%-22%). C, Trifurcation with communication between a proximal superficial branch and the ulnar proper palmar digital branch (<3%). D, High trifurcation (<3%). DB indicates deep branch; H, hamate; P, pisiform; SFB, superficial branch; UPDN, ulnar proper digital nerve; 4th CDN, fourth common digital nerve.
Few aberrant branches of the ulnar nerve have been reported. One branch was given off about 8 cm proximal to the pisiform and passed distally to join the superficial branch of the ulnar nerve distal to the distal edge of the pisiform.17 Another branch, arising 13 cm proximal to the pisiform, coursed distally along the ulnar artery and passed through the Guyon canal, then joined the common palmar digital nerves of the ring finger and middle finger.18
Variation of the Deep Motor Branch of the Ulnar Nerve
Various branching patterns of the deep motor branch to the hypothenar muscles have been described.13,19 Generally, muscles receive cross-innervation from the main branches, which range from a single main branch to 4 branches.10,13,19 The most common pattern of branching is 2 main branches to supply the hypothenar muscles.19 Murata et al10 described 4 arborization patterns of the deep branch of the ulnar nerve to the abductor digiti minimi.10 Type 1 is the most prevalent pattern, where the motor branch arises distal to the Guyon canal. In type 2, there are 2 motor branches; 1 branch arises within the Guyon canal and another branch arises distal to the canal. The ulnar nerve in some cases trifurcates within the Guyon canal into a superficial trunk, a deep branch, and a motor branch to the abductor digiti minimi (type 3). The motor branch to abductor digiti minimi (ADM) can also arise from the main trunk of the ulnar nerve within the Guyon canal (type 4).
Bifid deep motor branch of the ulnar nerve has been reported in different case reports with20,21 or without neural loop distal to the hook of the hamate.22 In an anatomical study of 77 cadavers, neural loop of the deep motor branch was noticed to pass around the hook of the hamate in 9% of dissected cadavers.23 The presence of anomalous neural communications might alter the classical clinical presentation, which can cause clinical confusion.
Variation of the Superficial Sensory Branch of the Ulnar Nerve
A number of variations involving the superficial sensory branch(es) of the ulnar nerve have been reported in the literature. In addition to having a single superficial branch of the ulnar nerve, 2 distinct sensory branches and a trifurcated sensory nerve were described.10,11 In 1 case, the superficial branch of the ulnar nerve continued as a common palmar digital nerve to the ring finger.24
Unusual Course of the Ulnar Nerve
The presence of the ulnar nerve within the carpal tunnel has been rarely encountered in the literature. This atypical course was first described in a case report by Eskesen et al25 and was then followed by 2 other reports.26,27 In addition to signs and symptoms of carpal tunnel syndrome, these patients express numbness and paraesthesias of the ulnar digits and hypothenar muscle wasting. In both reports, the Guyon canal contained only a small ulnar artery.26,27 Galzio et al found that the ulnar nerve was atrophic distally, where it bifurcated into superficial and deep branches.26
Communication With the Median Nerve
Several types of unusual communications between ulnar and median nerves were described in the literature.28 These anomalies result in atypical sensory and motor symptoms, which might confuse the treating surgeon.29 In the forearm, the Martin-Gruber anastomosis is a well-described anomalous connection in which a communicating branch originates from the median nerve to the ulnar nerve.29–31 The incidence of this is reported to be 11% to 24% in anatomic studies, whereas electrophysiological studies revealed a slightly higher range of 15% to 39%.29,32–35 Isolated ulnar nerve lesions at a level higher to the anastomosis may result in an atypical presentation of intrinsic muscle denervation.28 Marinacci communications are a very uncommon connection in the forearm, which describe an ulnar-to-median communication.36,37 Hence, it is also called a reverse Martin-Gruber anastomosis. Its reported incidence ranged from 1.3% to 16.7%.38–40
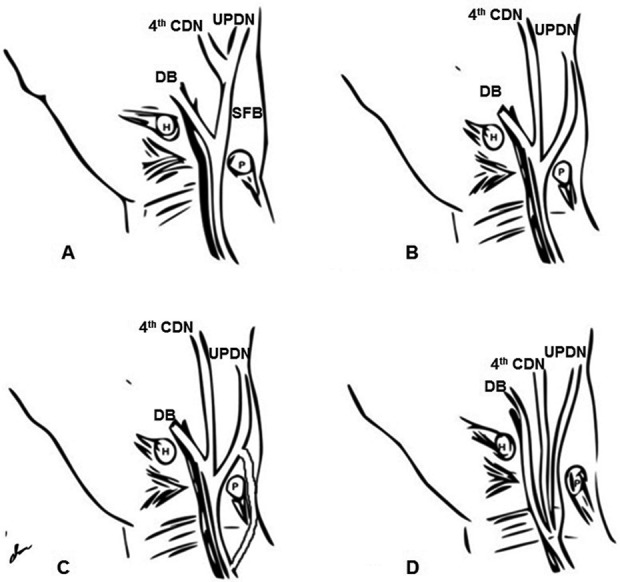
In the hand, the Riche-Cannieu anastomosis is a connection between the deep branch of the ulnar nerve and the recurrent branch of the median nerve in the palm (Figure 3). It has a high incidence reaching up to 83.3%.38 Riche-Cannieu anastomosis can present as an all ulnar hand, a condition that motor and sensory are supplied solely by the ulnar nerve,41 or an ulnar innervation of all thenar muscles.42 Berrettini anastomosis, or superficial palmar anastomosis, is a branch that communicates common digital nerves arising from the ulnar and median nerves in the palm, resulting in changes in sensation of the third and fourth digits.43,44 Incidence of this branch was found to be about 81% (Figure 3).45 Ramus communicans is a sensory deep communication branch between the fourth palmar common digital nerve that arises from the ulnar nerve and the third palmar common digital nerve that arises from the median nerve.45 It has a high incidence reaching up to 90%, and hence, it was considered to be a normal structure rather than an anomaly.28,45,46
Figure 3.
Communication between the ulnar nerve and median nerve in the hand. CDN indicates common digital nerve; MN, median nerve; UN, ulnar nerve.
Other reported variations included an anastomosis between the palmar cutaneous branch of the ulnar nerve and the third common digital nerve, a superficial anastomosis in the palm between the ulnar and median nerve9,47 or a deep anastomosis between the deep branch of the ulnar nerve and median nerve.48
Variation of the Dorsal Cutaneous Branch of the Ulnar Nerve
Kaplan49 described an accessory atypical branch arising from the dorsal cutaneous branch of the ulnar nerve directly to the superficial terminal branch, traversing to the palmar side, and passing the ulnar head on the medial side of the pisiform. This branch joins the palmar sensory branch of the ulnar nerve after passing the pisiform. This nerve was named “Kaplan’s accessory branch,” and several variations of this branch were eventually reported.50 These variations were described as having a terminal connection to the main trunk of the ulnar nerve in the Guyon canal,50 to the sensory branch of the ulnar nerve, to the proximal motor branch of the ulnar nerve,51 to the ulnar digital nerve of the little finger midway at the hypothenar eminence,24 or at the proximal interphalangeal joint of the little finger. It was also found as a continuing separate branch into the little finger.9,52
Variations of the Ulnar Artery
Overview
The ulnar artery passes along the ulnar nerve through the Guyon canal and then divides into superficial and deep branches, forming the superficial palmar arch and deep palmar arch, respectively.9,53 Table 2 summarizes the ulnar artery anomalies within and around the Guyon canal.
Table 2.
Anomalies of the Ulnar Artery Within and Around the Guyon Canal.
| Ulnar Artery Anomalies |
|---|
|
Branching Patterns of the Ulnar Artery
The majority of anatomical variations of the ulnar artery in the Guyon canal are related to the branching pattern. The main trunk of the ulnar artery typically divides into superficial and deep branches, which occurs in the Guyon canal. Variations of the arterial branches that accompany the deep branch of the ulnar nerve and the branch that supply the hypothenar muscles were described in different studies. In the majority of the reports, the most common pattern is finding the deep branch of the ulnar nerve accompanied with an arterial branch arising from the main trunk of the ulnar artery in the Guyon canal. Although the deep branch of the ulnar artery originates distally within the canal, it passes between the flexor tendon sheath of the little finger and the flexor digiti minimi, joining the deep branch of the ulnar nerve in the mid-palmar space.8,9,13,54,55 However, a different study reported that the most common pattern was observing the deep branch of the ulnar nerve accompanied with an arterial branch (the deep branch) originating from the ulnar artery, which then leaves the canal to reach the mid-palmar space.54 Moreover, cases with no arterial branch that accompanies the deep branch of the ulnar nerve in the canal have been observed. This pattern may include another arterial branch that joins the deep branch of the ulnar nerve distally in the mid-palmer space.9
The deep palmar arch is commonly formed by the anastomosis of the deep volar branch of the radial artery and the deep branch of the ulnar artery which is given off distally and enters the mid-palmar space.54,56 The deep palmar arch was also found to be formed by an anastomosis of the deep volar branch of the radial artery and the arterial branch accompanying the deep branch of the ulnar nerve in the Guyon canal.56 Less commonly, an anastomosis of the deep volar branch of the radial artery with both the arterial branch accompanying the deep branch of the ulnar nerve and the deep branches of the ulnar artery forms the deep palmar arch.54,56 In 1 case, no deep palmar arch was found in the hand.54
The Dorsal Perforating Artery
This variant branch has been rarely described in the literature. It is given off from the arterial branch of the ulnar artery that accompanies the deep branch of the ulnar nerve distally in the Guyon canal and contributes to the dorsal carpal arterial arch.54,57 Knowing this variant branch is particularly important because it passes along with the arterial branch that accompanies the deep branch of the ulnar nerve in the canal where injury may occur.
The Superficial Ulnar Artery
The superficial ulnar artery is a well-described anomaly and has been reported to occur approximately between 0.7% and 9.4%.53,58 The superficial ulnar artery arises from the brachial artery and passes in the forearm superficial to the pronator teres and flexor muscles and deep to the antebrachial fascia. In the hand, this artery and the superficial branch of the radial artery form a superficial palmar arch. High origin of the superficial ulnar artery from the brachial artery has also been described, with a prevalence ranging from 0.67% to 9.38%.59 Less commonly, the superficial ulnar artery originates from the axillary artery or as a continuity of a superficial brachial artery.53,60
Unusual Course of Ulnar Artery
In an isolated anomaly, the ulnar artery passes superficial to the palmaris brevis at the level of the Guyon canal and divides distally in a normal pattern.61
Muscle Anatomical Variations
Case Report
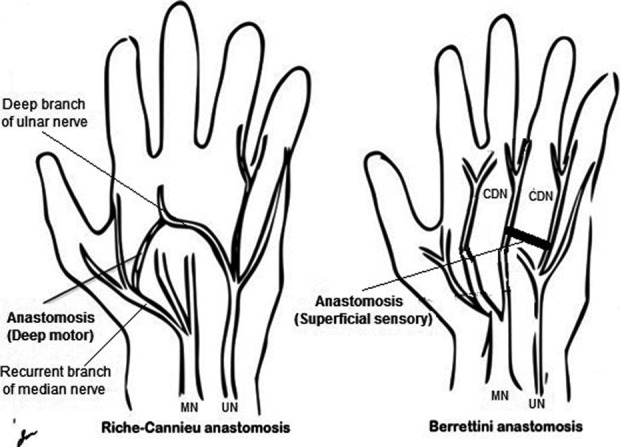
A 46-year-old right-hand-dominant male labourer presents with a 3-month history of constant numbness and progressive weakness in the small and ring fingers of his left hand. He describes clumsiness and a loss of manual dexterity. On physical examination, he has severe intrinsic muscle atrophy and weakness. He also has reduced light touch sensation and prolonged 2-point discrimination over the left ulnar nerve distribution. He has a clearly positive Tinel sign at the left elbow and wrist, as well as a positive elbow flexion test. Scratch collapse test is positive at both cubital tunnel and Guyon canal. Electrodiagnostic studies confirm these clinical findings. The patient underwent a left Guyon canal, cubital tunnel, and carpal tunnel release surgery, in addition to a left distal anterior interosseous nerve to ulnar motor nerve transfer. During the release of the Guyon canal, an anomalous muscle was identified at the volar surface of the forearm entering the Guyon canal over the site of compression. The muscle had an origin from the tendon of the palmaris longus and inserted into the hypothenar muscles (Figure 4). The anomalous muscle was resected and the procedure was completed successfully with no complications. Upon follow-up, signs of sensory recovery were seen in the ulnar nerve distribution within 2 months.
Figure 4.
Aberrant muscle in the forearm overlying the Guyon canal. A and B, Aberrant muscle in the volar surface of the left forearm, extending from the palmaris longus to the hypothenar muscles over the site of ulnar nerve compression in the Guyon canal.
Aberrant Muscles Related to the Guyon Canal
Different variations in the muscles around the Guyon canal were described in the literature. Several authors reported variations related to the origin, insertion, fusion, or absence of any of the hypothenar muscles, most frequently the abductor digiti minimi.10 However, aberrant muscles are the most clinically relevant variations. Aberrant muscles related to the Guyon canal are identified in about 22% to 35% of the population.10,17,62,63
Dodds et al17 reported a series of dissections of 58 paired cadaver wrists. Thirteen anomalous muscles were found. Six of the 13 muscles were bilaterally paired. Ten muscles had their origin from the antebrachial fascia, most of which originated just proximal to the wrist. Three had their origin from the lateral side of the pisiform and the palmar carpal ligament. All 13 muscles followed the abductor digiti minimi and inserted on the ulnar side, base of the proximal phalanx of the small finger.
Zeiss et al62 analyzed the wrists of 42 asymptomatic individuals by magnetic resonance imaging and noted the prevalence of muscular anomalies in the volar aspect of the wrist. Ten of the 42 wrists demonstrated anomalous muscles along the ulnar side of the wrist, with a length ranging from 12 mm to 8 cm. They originated along the distal half of the forearm to the wrist area, from the antebrachial fascia or palmar carpal ligament between the flexor carpi ulnaris and palmaris longus. Two muscles were attached to the palmaris longus tendon at their origin. All of the muscles traveled into the Guyon canal and inserted with the abductor or flexor digiti minimi muscle.
The study by Harvie et al63 reported a series of 58 volunteers (116 wrists) examined by ultrasound to identify anomalous muscles in the Guyon canal. Anomalous muscles were identified in 41 wrists, with a higher prevalence in males. Bilateral muscles were present in 50% of cases in both sexes. All anomalous muscles were described as variants of abductor digiti minimi. The origin could not be accurately defined in all cases. However, the findings from most cases were suggestive of an origin either from the pisiform bone or the antebrachial fascia.
Murata et al10 dissected the hypothenar region of 35 hands from 20 cadavers. An aberrant muscle was identified in 9 hands. The authors classified these aberrant muscles into 4 types. In variation 1 (5 hands), the aberrant muscle originated from the flexor retinaculum. In variation 2 (2 hands), the muscle originated from the antebrachial fascia. These 7 muscles lied volar to the neurovascular bundle in the Guyon canal and fused into the ADM distally. In variation 3 (1 hand), a short aberrant muscle originated from the pisiform and inserted into the flexor retinaculum, lying over the ulnar nerve and separating it from the ulnar artery. In variation 4 (1 hand), the aberrant muscle originated from the pisiform and inserted onto the volar aspect of the fifth metacarpal head.
Several case studies reported similar aberrant muscles related to the Guyon canal.16,64–66 In addition, muscles originating from the tendon of the palmaris longus67–70 and less frequently from the flexor carpi ulnaris71,72 or flexor carpi radialis were reported.73 The reported aberrant muscles are summarized in Table 3.
Table 3.
Aberrant Muscles Related to the Guyon Canal.
| Aberrant muscles | |
|---|---|
| Origin | Insertion |
|
|
Discussion
This study identified several variations in the anatomical structures of the Guyon canal reported in the literature. Variations of the ulnar nerve involved its course, branching pattern, deep motor branch, superficial sensory branch, dorsal cutaneous branch, and the communication with the median nerve. Understanding these variations is critical to the hand surgeon.45 For example, patients with a median–ulnar nerve communication who sustain trauma or compression neuropathies may present with atypical functional (motor or sensory) deficits.10,45 Moreover, care must be taken to avoid iatrogenic injury to nerves when surgically exploring the Guyon canal or the area surrounding it. Avoiding nerve damage is particularly important in case of nerve communication, thus decreasing the likelihood of post-operative neuropathic pain.74
Ulnar artery variations involved its course, branching pattern, the superficial ulnar artery, and the dorsal perforating artery. Palpable arterial pulses in unusual regions, absence of pulses in usual regions, or uncontrolled bleeding after superficial incisions may raise suspicion of superficial arterial anomalies (eg, superficial ulnar artery).60 Knowledge of the precise course and branching pattern of the ulnar artery is critical to avoid unexpected complications during hand or wrist surgery.
Aberrant muscles crossing the Guyon canal were found to originate from the antebrachial fascia, pisiform bone, flexor retinaculum, the tendon of palmaris longus, flexor carpi ulnaris, or flexor carpi radialis; these muscles may insert into 1 or more of the hypothenar muscles, flexor retinaculum, or the head of fifth metacarpal. In most cases, the aberrant muscle fuses with abductor digiti minimi, thus earning the description of an accessory abductor digiti minimi by many authors.10,17,62 Our case represents a good example of these aberrant muscles that could potentially represent a source of ulnar nerve compression causing significant symptoms.
The association of the anatomical variations of the Guyon canal with different clinical conditions was described in the literature. Several papers reported compression neuropathy due to an aberrant hypothenar muscle.16,65,75–77 Additionally, an aberrant muscle may also be associated with thrombosis of the ulnar artery.71,78 Thus, appropriate recognition of the previously described variations by hand surgeons is important to avoid clinical misinterpretation and potential surgical complications.
Footnotes
Authors’ Note: Z. T. Fadel is the primary reviewer of this study. He contributed to search strategy, data extraction, and interpretation and was the principal contributor to the manuscript development. O. A. Samargandi is the second reviewer of this study. He contributed to search strategy, data extraction, and interpretation and largely contributed to the manuscript development. D. T. Tang is the senior author of this study. He is primarily responsible for reviewing the paper for oversights and provides a comprehensive revision to the manuscript. This work was presented at the 69th Annual Meeting of the Canadian Society of Plastic Surgeons, Victoria, British Columbia, on June 2015
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Guyon F. Note sure une disposition anatomique prope a la face antericure de la region du poignet et non encore decrite par le docteur. Bulletin de la Societe de Anatomique de Paris. 1861;6:184–186. [Google Scholar]
- 2. Shea JD, McClain EJ. Ulnar-nerve compression syndromes at and below the wrist. J Bone Joint Surg Am. 1969;51(6):1095–1103. [PubMed] [Google Scholar]
- 3. Gross MS, Gelberman RH. The anatomy of the distal ulnar tunnel. Clin Orthop Relat Res. 1985(196):238–247. [PubMed] [Google Scholar]
- 4. Polatsch DB, Melone CP, Jr, Beldner S, Incorvaia A. Ulnar nerve anatomy. Hand Clin. 2007;23(3):283–289, v. [DOI] [PubMed] [Google Scholar]
- 5. Bachoura A, Jacoby SM. Ulnar tunnel syndrome. Orthop Clin North Am. 2012;43(4):467–474. [DOI] [PubMed] [Google Scholar]
- 6. Ombaba J, Kuo M, Rayan G. Anatomy of the ulnar tunnel and the influence of wrist motion on its morphology. J Hand Surg Am. 2010;35(5):760–768. [DOI] [PubMed] [Google Scholar]
- 7. Pierre-Jerome C, Moncayo V, Terk MR. The Guyon’s canal in perspective: 3-T MRI assessment of the normal anatomy, the anatomical variations and the Guyon’s canal syndrome. Surg Radiol Anat. 2011;33(10):897–903. [DOI] [PubMed] [Google Scholar]
- 8. Zeiss J, Jakab E, Khimji T, Imbriglia J. The ulnar tunnel at the wrist (Guyon’s canal): normal MR anatomy and variants. AJR Am J Roentgenol. 1992;158(5):1081–1085. [DOI] [PubMed] [Google Scholar]
- 9. König PS, Hage JJ, Bloem JJ, Prosé LP. Variations of the ulnar nerve and ulnar artery in Guyon’s canal: a cadaveric study. J Hand Surg. 1994;19(4):617–622. [DOI] [PubMed] [Google Scholar]
- 10. Murata K, Tamai M, Gupta A. Anatomic study of variations of hypothenar muscles and arborization patterns of the ulnar nerve in the hand. J Hand Surg. 2004;29(3):500–509. [DOI] [PubMed] [Google Scholar]
- 11. Bonnel F, Vila RM. Anatomical study of the ulnar nerve in the hand. J Hand Surg Br. 1985;10(2):165–168. [DOI] [PubMed] [Google Scholar]
- 12. Niitsu M, Kokubo N, Nojima S. Variations of the ulnar nerve in Guyon’s canal: in vivo demonstration using ultrasound and 3T MRI. Acta Radiol. 2010;51(8):939–946. [DOI] [PubMed] [Google Scholar]
- 13. Lindsey JT, Watumull D. Anatomic study of the ulnar nerve and related vascular anatomy at Guyon’s canal: a practical classification system. J Hand Surg. 1996;21(4):626–633. [DOI] [PubMed] [Google Scholar]
- 14. Gotani H, Yamano Y, Gilbert A. Anatomy of the ulnar nerve in the hand: study of anomalous sensory branches. J Jpn Soc Surg Hand. 2001;18:670–674. [Google Scholar]
- 15. Mannerfelt L. Studies on the hand in ulnar nerve paralysis. A clinical-experimental investigation in normal and anomalous innervation. Acta Orthop Scand. 1965;Suppl 87:1+. [DOI] [PubMed] [Google Scholar]
- 16. Greenberg JA, Mosher JF., Jr Distal ulnar neuropathy: coexisting anatomic variants. J Hand Surg. 1992;17(2):303–305. [DOI] [PubMed] [Google Scholar]
- 17. Dodds GA, III, Hale D, Jackson WT. Incidence of anatomic variants in Guyon’s canal. J Hand Surg Am. 1990;15(2):352–355. [DOI] [PubMed] [Google Scholar]
- 18. Bozkurt MC, Tagil SM, Ersoy M, Tekdemir I. Muscle variations and abnormal branching and course of the ulnar nerve in the forearm and hand. Clin Anat. 2004;17(1):64–66. [DOI] [PubMed] [Google Scholar]
- 19. Blair WF, Percival KJ, Morecraft R. Distribution pattern of the deep branch of the ulnar nerve in the hypothenar eminence. Clin Orthop Relat Res. 1988;(229):294–301. [PubMed] [Google Scholar]
- 20. Lassa R, Shrewsbury MM. A variation in the path of the deep motor branch of the ulnar nerve at the wrist. J Bone Joint Surg. 1975;57(7):990–991. [PubMed] [Google Scholar]
- 21. Fenning JB. Deep ulnar-nerve paralysis resulting from an anatomical abnormality. A case report. J Bone Joint Surg Am. 1965;47(7):1381–1382. [PubMed] [Google Scholar]
- 22. Bergfield TG, Aulicino PL. Variation of the deep motor branch of the ulnar nerve at the wrist. J Hand Surg. 1988;13(3):368–369. [DOI] [PubMed] [Google Scholar]
- 23. Rogers MR, Bergfield TG, Aulicino PL. A neural loop of the deep motor branch of the ulnar nerve: an anatomic study. J Hand Surg. 1991;16(2):269–271. [DOI] [PubMed] [Google Scholar]
- 24. Bozkurt MC, Cezayirli E, Tagil SM. An unusual termination of the ulnar nerve in the palm. Ann Anat. 2002;184(3):271–273. [DOI] [PubMed] [Google Scholar]
- 25. Eskesen V, Rosenørn J, Osgaard O. Atypical carpal tunnel syndrome with compression of the ulnar and median nerves: case report. J Neurosurg. 1981;54(5):668–669. [DOI] [PubMed] [Google Scholar]
- 26. Galzio RJ, Magliani V, Lucantoni D, D’Arrigo C. Bilateral anomalous course of the ulnar nerve at the wrist causing ulnar and median nerve compression syndrome: case report. J Neurosurg. 1987;67(5):754–756. [DOI] [PubMed] [Google Scholar]
- 27. Papanastasiou S, Sood M. Aberrant position of the ulnar nerve within the carpal canal. Microsurgery. 2004;24(1):24–25. [DOI] [PubMed] [Google Scholar]
- 28. Dogan NU, Uysal II, Seker M. The communications between the ulnar and median nerves in upper limb. Neuroanatomy. 2009;8:15–19. [Google Scholar]
- 29. Lee KS, Oh CS, Chung IH, Sunwoo IN. An anatomic study of the Martin–Gruber anastomosis: electrodiagnostic implications. Muscle Nerve. 2005;31(1):95–97. [DOI] [PubMed] [Google Scholar]
- 30. Uchida Y, Sugioka Y. Electrodiagnosis of Martin-Gruber connection and its clinical importance in peripheral nerve surgery. J Hand Surg. 1992;17(1):54–59. [DOI] [PubMed] [Google Scholar]
- 31. Shu HS, Chantelot C, Oberlin C, Alnot JY, Shao H. Martin-Gruber communicating branch: anatomical and histological study. Surg Radiol Anat. 1999;21(2):115–118. [DOI] [PubMed] [Google Scholar]
- 32. Amoiridis G. Median–ulnar nerve communications and anomalous innervation of the intrinsic hand muscles: an electrophysiological study. Muscle Nerve. 1992;15(5):576–579. [DOI] [PubMed] [Google Scholar]
- 33. Lee SA, Kim KK, Lee MC, Sunwoo IN, Kim KW. The electrodiagnostic findings in Martin-Gruber anastomosis. J Korean Neurol Assoc. 1994;12(1):87–91. [Google Scholar]
- 34. Rodriguez-Niedenführ M, Vazquez T, Parkin I, Logan B, Sañudo JR. Martin-Gruber anastomosis revisited. Clin Anat. 2002;15(2):129–134. [DOI] [PubMed] [Google Scholar]
- 35. Nakashima T. An anatomic study on the Martin-Gruber anastomosis. Surg Radiol Anat. 1993;15(3):193–195. [DOI] [PubMed] [Google Scholar]
- 36. Stancić MF, Burgić N, Mićović V. Marinacci communication: case report. J Neurosurg. 2000;92(5):860–862. [DOI] [PubMed] [Google Scholar]
- 37. Marinacci A. The problem of unusual anomalous innervation of hand muscles. The value of electrodiagnosis in its evaluation. Bull Los Angel Neuro Soc. 1964;29:133–142. [PubMed] [Google Scholar]
- 38. Kimura I, Ayyar DR, Lippmann SM. Electrophysiological verification of the ulnar to median nerve communications in the hand and forearm. Tohoku J Exp Med. 1983;141(3):269–274. [DOI] [PubMed] [Google Scholar]
- 39. Meenakshi-Sundaram S, Sundar B, Arunkumar MJ. Marinacci communication: an electrophysiological study. Clin Neurophysiol. 2003;114(12):2334–2337. [DOI] [PubMed] [Google Scholar]
- 40. Hopf HC. Forearm ulnar-to-median nerve anastomosis of sensory axons. Muscle Nerve. 1990;13(7):654–656. [DOI] [PubMed] [Google Scholar]
- 41. Kim BJ, Date ES, Lee SH, Lau EW, Park MK. Unilateral all ulnar hand including sensory without forearm communication. Am J Phys Med Rehabil. 2004;83(7):569–573. [DOI] [PubMed] [Google Scholar]
- 42. Ganes T. Complete ulnar innervation of the thenar muscles combined with normal sensory fibres in a subject with no peripheral nerve lesion. Electromyogr Clin Neurophysiol. 1991;32(10-11):559–563. [PubMed] [Google Scholar]
- 43. Stancić MF, Mićović V, Potocnjak M. The anatomy of the Berrettini branch: implications for carpal tunnel release. J Neurosurg. 1999;91(6):1027–1030. [DOI] [PubMed] [Google Scholar]
- 44. May JW, Jr, Rosen H. Division of the sensory ramus communicans between the ulnar and median nerves: a complication following carpal tunnel release. A case report. J Bone Joint Surg Am. 1981;63(5):836–838. [PubMed] [Google Scholar]
- 45. Loukas M, Abel N, Tubbs RS, Matusz P, Zurada A, Cohen-Gadol AA. Neural interconnections between the nerves of the upper limb and surgical implications: a review. J Neurosurg. 2011;114(1):225–235. [DOI] [PubMed] [Google Scholar]
- 46. Don Griot JP, Zuidam JM, van Kooten EO, Prosé LP, Hage JJ. Anatomic study of the ramus communicans between the ulnar and median nerves. J Hand Surg. 2000;25(5):948–954. [DOI] [PubMed] [Google Scholar]
- 47. Ferrari GP, Gilbert A. The superficial anastomosis on the palm of the hand between the ulnar and median nerves. J Hand Surg. 1991;16(5):511–514. [DOI] [PubMed] [Google Scholar]
- 48. Loukas M, Bellary SS, Tubbs RS, Shoja MM, Cohen Gadol AA. Deep palmar communications between the ulnar and median nerves. Clin Anat. 2011;24(2):197–201. [DOI] [PubMed] [Google Scholar]
- 49. Kaplan EB. Variation of the ulnar nerve at the wrist. Bull Hosp Joint Dis. 1963;24:85. [PubMed] [Google Scholar]
- 50. Hankins CL, Flemming S. A variant of Kaplan’s accessory branch of the dorsal cutaneous branch of the ulnar nerve: a case report and review of the literature. J Hand Surg. 2005;30(6):1231–1235. [DOI] [PubMed] [Google Scholar]
- 51. Hoogbergen MM, Kauer JM. An unusual ulnar nerve-median nerve communicating branch. J Anat. 1992;181(pt 3):513. [PMC free article] [PubMed] [Google Scholar]
- 52. McCarthy RE, Nalebuff EA. Anomalous volar branch of the dorsal cutaneous ulnar nerve: a case report. J Hand Surg. 1980;5(1):19–20. [DOI] [PubMed] [Google Scholar]
- 53. Sieg P, Jacobsen HC, Hakim SG, Hermes D. Superficial ulnar artery: curse or blessing in harvesting fasciocutaneous forearm flaps. Head Neck. 2006;28(5):447–452. [DOI] [PubMed] [Google Scholar]
- 54. Murata K, Tamai M, Gupta A. Anatomic study of arborization patterns of the ulnar artery in Guyon’s canal. J Hand Surg. 2006;31(2):258–263. [DOI] [PubMed] [Google Scholar]
- 55. Coleman SS, Anson BJ. Arterial patterns in the hand based upon a study of 650 specimens. Surg Gynecol Obstet. 1961;113:409. [PubMed] [Google Scholar]
- 56. Gellman H, Botte MJ, Shankwiler J, Gelberman RH. Arterial patterns of the deep and superficial palmar arches. Clin Orthop Relat Res. 2001;(383):41–46. [DOI] [PubMed] [Google Scholar]
- 57. Gelberman RH, Panagis JS, Taleisnik J, Baumgaertner M. The arterial anatomy of the human carpus. Part I: the extraosseous vascularity. J Hand Surg. 1983;8(4):367–375. [DOI] [PubMed] [Google Scholar]
- 58. Thoma A, Young JE. The superficial ulnar artery” trap” and the free forearm flap. Ann Plast Surg. 1992;28(4):370–372. [DOI] [PubMed] [Google Scholar]
- 59. Solan S. Accessory superficial ulnar artery: a case report. J Clin Diagn Res. 2013;7(12):2943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Troupis TG, Tsakotos G, Michalinos A, et al. Uncommon course of the ulnar artery. Am Surg. 2011;77(12):1717–1719. [PubMed] [Google Scholar]
- 61. Richards RS, Dowdy P, Roth JH. Ulnar artery palmar to palmaris brevis: cadaveric study and three case reports. J Hand Surg. 1993;18(5):888–892. [DOI] [PubMed] [Google Scholar]
- 62. Zeiss J, Guilliam-Haidet L. MR demonstration of anomalous muscles about the volar aspect of the wrist and forearm. Clin Imaging. 1996;20(3):219–221. [DOI] [PubMed] [Google Scholar]
- 63. Harvie P, Patel N, Ostlere SJ. Prevalence and epidemiological variation of anomalous muscles at Guyon’s canal. J Hand Surg Br. 2004;29(1):26–29. [DOI] [PubMed] [Google Scholar]
- 64. Depukat P, Mizia E, Walocha J. An anomalous bilateral muscle in Guyon’s canal found during cadaver study. Folia Morphol (Warsz). 2010;69(1):65–67. [PubMed] [Google Scholar]
- 65. Fong EP, Mahaffey PJ. Ulnar tunnel syndrome—an unusual cause. Hand Surg. 2000;5(1):77–79. [DOI] [PubMed] [Google Scholar]
- 66. Ogun TC, Karalezli N, Ogun CO. The concomitant presence of two anomalous muscles in the forearm. Hand. 2007;2(3):120–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Zeiss J, Jakab E. MR demonstration of an anomalous muscle in a patient with coexistent carpal and ulnar tunnel syndrome. Case report and literature summary. Clin Imaging. 1995;19(2):102–105. [DOI] [PubMed] [Google Scholar]
- 68. Curry B, Kuz J. A new variation of abductor digiti minimi accessorius. J Hand Surg Am. 2000;25(3):585–587. [DOI] [PubMed] [Google Scholar]
- 69. Soldado-Carrera F, Vilar-Coromina N, Rodríguez-Baeza A. An accessory belly of the abductor digiti minimi muscle: a case report and embryologic aspects. Surg Radiol Anat. 2000;22(1):51–54. [DOI] [PubMed] [Google Scholar]
- 70. Lokanathan TH, Surendra M, Ajay N, Rajendra RR. Unusual co-existence of biaponeurotic palmaris longus and accessory abductor digiti minimi in man. J Clin Diagn Res. 2014;8(1):146–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Pribyl CR, Moneim MS. Anomalous hand muscle found in the Guyon’s canal at exploration for ulnar artery thrombosis. A case report. Clin Orthop Relat Res. 1994(306):120–123. [PubMed] [Google Scholar]
- 72. Hill ML, Shoja MM, Salter EG, Tubbs RS. An unusual muscle of the wrist with potential compression of the ulnar nerve. Folia Morphol (Warsz). 2006;65(2):178–180. [PubMed] [Google Scholar]
- 73. Paraskevas GK, Ioannidis O, Economou DS. Anomalous muscle causing ulnar nerve compression at Guyon’s canal. J Plast Surg Hand Surg. 2012;46(3-4):288–290. [DOI] [PubMed] [Google Scholar]
- 74. Lourie GM, King J, Kleinman WB. The transverse radioulnar branch from the dorsal sensory ulnar nerve: its clinical and anatomical significance further defined. J Hand Surg. 1994;19(2):241–245. [DOI] [PubMed] [Google Scholar]
- 75. Fahrer M, Millroy PJ. Ulnar compression neuropathy due to an anomalous abductor digiti minimi-clinical and anatomic study. J Hand Surg Am. 1981;6(3):266–268. [DOI] [PubMed] [Google Scholar]
- 76. Luethke R, Dellon AL. Accessory abductor digiti minimi muscle originating proximal to the wrist causing symptomatic ulnar nerve compression. Ann Plast Surg. 1992;28(3):307–308. [DOI] [PubMed] [Google Scholar]
- 77. Netscher D, Cohen V. Ulnar nerve compression at the wrist secondary to anomalous muscles: a patient with a variant of abductor digiti minimi. Ann Plast Surg. 1997;39(6):647–651. [DOI] [PubMed] [Google Scholar]
- 78. Moss DP, Forthman CL. Ulnar artery thrombosis associated with anomalous hypothenar muscle. J Surg Orthop Adv. 2008;17(2):85–88. [PubMed] [Google Scholar]