Abstract
Purpose:
Canadian health care is often criticized for extended wait times, whereas the United States suffers from increased costs. The purpose of this pilot study was to determine the cost-utility of open carpal tunnel release in Canada versus the United States.
Methods:
A prospective cohort study evaluated patients undergoing open carpal tunnel release at an institution in Canada and the United States. All costs from a societal perspective were captured. Utility was measured using validated health-related quality of life (HRQOL) scales—the EuroQol-5D and the Michigan Hand Outcome Questionnaire.
Results:
Twenty-one patients at the Canadian site and 8 patients at the US site participated. Mean total costs were US $1581 ± $1965 and $2179 (range: $1421-$2741) at the Canadian and US sites, respectively. Health-related quality of life demonstrated significant improvements following surgery (P < .05). Patient utilities preoperatively and at 6 weeks and 3 months postoperatively were 0.72 ± 0.20, 0.86 ± 0.11, and 0.83 ± 0.16 at the Canadian site and 0.81 ± 0.09, 0.86 ± 0.10, and 0.86 ± 0.12 at the US site. Improvements in HRQOL directly related to surgery were not significantly different between patients in Canada and the United States. American patients, however, attained improved HRQOL sooner due to shorter wait times (27 ± 10 vs 214 ± 119 days; P < .001). The incremental cost-utility of the US system was $7758/quality-adjusted life year gained compared to the Canadian system. Sensitivity analyses confirmed that these results were robust.
Conclusion:
This pilot study suggests that carpal tunnel surgery is more cost-effective in the United States due to prolonged wait times in Canada.
Keywords: carpal tunnel syndrome, carpal tunnel surgery, cost-effectiveness, cost-utility, quality of life, decision analysis
Abstract
Objectif :
Le système de santé canadien est souvent critiqué pour ses temps d’attente prolongés, tandis qu’aux États-Unis, les coûts sont élevés. La présente étude pilote visait à déterminer le rapport coût-utilité de la libération ouverte du canal carpien au Canada par rapport aux États-Unis.
Méthodologie :
Les chercheurs ont réalisé une étude prospective de cohorte sur des patients qui subissaient une libération ouverte du canal carpien dans un établissement du Canada ou des États-Unis. Ils ont colligé tous les coûts sociétaux et ont mesuré l’utilité à l’aide d’échelles validées de la qualité de vie liée à la santé (QdVLS), soit l’EuroQol-5D et le questionnaire Michigan sur le résultat clinique de la main.
Résultats :
Vingt et un patients de l’établissement canadien et huit de l’établissement américain ont participé à l’étude. Les coûts totaux moyens s’élevaient à 1 581 $US ± 1 965 $ et à 2 179 $ (plage de 1 421 $ à 2 741 $) dans les établissements canadiens et américains, respectivement. La QdVLS s’est accrue de manière significative après l’opération (P<0,05). L’utilité des patients avant l’opération, puis six semaines et trois mois après l’opération, était de 0,72 ± 0,20, de 0,86 ± 0,11 et de 0,83 ± 0,16 dans l’établissement canadien et de 0,81 ± 0,09, de 0,86 ± 0,10 et de 0,86 ± 0,12 dans l’établissement américain. Les améliorations de la QdVLS découlant directement de l’opération ne différaient pas de manière significative entre le Canada et les États-Unis. Cependant, les patients américains voyaient leur QdVLS s’améliorer plus rapidement puisque les temps d’attente étaient moins longs (27 ± 10 jours par rapport à 214 ± 119 jours; P<0,001). Le coût-utilité incrémentiel du système américain s’établissait à 7 758 $/année de vie pondérée par la qualité par rapport au système canadien. Des analyses de sensibilité ont confirmé la solidité de ces résultats.
Conclusion :
D’après cette étude pilote, la libération du canal carpien présente un meilleur rapport coût-utilité aux États-Unis en raison des temps d’attente prolongés au Canada.
Introduction
In the present political and economic climate, there is an increasing scrutiny of health-care expenditures and an increasing pressure to attain value-for-money with respect to health-care practice. Canada, with its publicly funded, single-payer, universal health insurance, is often criticized for extended wait times. The United States, conversely, boasts reduced wait times but suffers from increased costs as a result of its multipayer public and private health-care systems.1 These increased health-care costs are difficult to justify with evidence that life expectancy and outcomes for some diseases are the same or better in Canada when compared to the United States.2–6
Appropriate comparison between health-care practices in Canada and the United States may be achieved through meticulous calculation of the costs and effectiveness. Although previous studies have examined either the costs or the effectiveness of surgical procedures (eg, total hip and knee replacements, cardiac surgery) between Canada and the United States, none provide a direct comparison of cost-effectiveness in the same population.1,2,6–10 This information is important to ensure the efficient delivery of surgical health-care services. Carpal tunnel surgery may facilitate this investigation given the high disease prevalence, availability of validated outcome scales, and relatively short follow-up times.
The goal of this pilot study was to determine the cost-utility of open carpal tunnel release in Canada versus the United States and to determine the feasibility of performing a large sample size cost-utility analysis study comparing the 2 health-care systems. This may ultimately identify factors that promote or limit the efficient delivery of services in hand/plastic surgery.
Methods
We performed a pilot prospective study to measure the costs and effectiveness of carpal tunnel surgery performed in Canada and the United States. Consecutive patients from 2 academic hospitals, 1 in Canada (St Joseph’s Healthcare, Hamilton, Ontario) and 1 in the United States (Southern Illinois Hand Center, Effingham, Illinois), were screened at the time of their initial consultation. Patients with a clinical and electromyogram/nerve conduction study (EMG/NCS) confirmed diagnosis of carpal tunnel syndrome undergoing unilateral open carpal tunnel release were considered for study participation. Patients were excluded for the following criteria—younger than 18 years of age, worker’s compensation, diabetes, generalized peripheral neuropathy, Raynaud’s, pregnancy, previous hand surgery including carpal tunnel release, medically unfit for surgery, and inability to complete surveys in English. All patients underwent open carpal tunnel release according to the investigators’ routine practice. Research ethics board approval was obtained at each institution.
Costs
All direct and indirect costs from a societal perspective were calculated as recommended by the Panel on Cost-Effectiveness in Health and Medicine.11 Direct costs included surgeon, hospital, anesthesia, and physiotherapy fees. Costs for Canadian patients were obtained from the Ontario Ministry of Health and Long-Term Care Physician Fee Schedule and the hospital’s finance department. Costs for US patients were based on the Medicare Physician Fee Schedule and reimbursement rates as reported by the hospital’s finance departments. Mean patient charges were also reported upon request. Indirect costs were collected through a modified case report form (CRF) designed to collect information on resource utilization specific to carpal tunnel syndrome.12 Patients recorded all out-of-pocket expenses such as postoperative medications, travel, general practitioner, physiotherapy and emergency department visits, and caregiver expenses. They also recorded time off work for themselves and their caregivers. Productivity losses were calculated using the Human Capital method.13 Duration of work loss for the patient or caregiver was multiplied by the average daily wage rate. All costs were converted to US$ using purchasing power parities.14 Costs were not discounted due to the short time frame of the study (less than 1 year).
Effectiveness
Effectiveness was measured from the patients’ perspective using quality-adjusted life years (QALYs). Quality-adjusted life years account for both patient quality of life and the time spent in the different health states. Quality of life was measured using 2 validated measures—(1) the Michigan Hand Outcomes Questionnaire (MHQ), a condition-specific scale, and (2) the EuroQOL-5D (EQ-5D), a utility measure from which QALYs can be calculated. Quality-adjusted life years are important components of cost-utility analyses.
Questionnaires were self-administered by all patients at 3 time points—preoperatively and at 6 weeks and 3 months postoperatively. A minimal clinically important difference in patient utility was assumed to be 0.03.15 The duration of time spent in each health states was measured by wait times, defined for both time from initial referral to initial consultation (wait 1) and time from decision to operate to the date of operation (wait 2). Wait times were collected through the modified CRF.
The MHQ is a 37-item questionnaire that measures 6 domains of interest. It is a specific and validated measure for assessing hand outcomes and quality of life in patients with carpal tunnel syndrome.16 The MHQ combines both functional and symptom scales of the right and left hand independently.
Utility values were obtained from the EQ-5D, a validated measure of health status used in the clinical and economic evaluation of health care. Using population values, each EQ-5D score can be translated via a regression equation to an equivalent utility score, derived from a general population using time trade-off techniques.17 Utilities measure relative patient preferences for a particular health state on a scale from 0 (representing death) to 1 (representing perfect health). Utility values were then multiplied by the time spent in each health state to determine the QALYs gained.
Sample Size Calculation
As this was a pilot study, a power analysis was not performed. We aimed to collect preliminary data on the outcomes of interest to adequately power a full-scale study.
Data Analysis
A descriptive analysis was performed. Categorical data were compared using χ2 or Fisher exact test. Continuous data were compared using a student t test or Wilcoxon rank test (when not normally distributed). Mean changes in MHQ and EQ-5D scores were calculated from baseline to each follow-up time point. Multiple regression analysis was used to control for differences in baseline utility between Canadian and US patients.18 An incremental cost-utility ratio (ICUR) was calculated as the difference in total costs between the Canadian and US system divided by the difference in QALYs. A threshold of $50 000/QALY or less was used to indicate cost-effectiveness.19 Analyses were performed using SPSS, version 18.0 (SPSS, Chicago, Illinois).
Results
Twenty-nine patients participated in this study, 21 from Canada and 8 from the United States. No patients were lost to follow up. Patient demographics are summarized in Table 1. There were no significant differences between Canadian and US study participants. Patients’ insurance at the US site was Medicare (25%), private insurance (63%), and self-pay (12%).
Table 1.
Patient Demographics.
| Canada (n = 21) | United States (n = 8) | P Value | |
|---|---|---|---|
| Age, years, mean (SD) | 59 (14) | 57 (15) | NS |
| Female, n (%) | 13 (62) | 4 (57) | NS |
| Duration of symptoms, months | 59 (64) | 45 (67) | NS |
| Married, n (%) | 16 (80) | 7 (88) | NS |
| Insurance type, n (%) | |||
| Provincial insurance | 21 (100) | ||
| Medicare | 2 (25) | ||
| Private insurance | 5 (63) | ||
| Self-pay | 1 (12) | ||
| Employment, n (%) | NS | ||
| Full-time | 7 (35) | 3 (37) | |
| Part-time | 2 (10) | 1 (12) | |
| Homemaker | 2 (10) | 3 (37) | |
| Retired | 9 (45) | 1 (12) | |
| Repetitive tasks, n (%) | 9 (45) | 2 (40) | NS |
| Gross household income, n (%) | NS | ||
| <$25 000 | 5 (25) | 3 (37) | |
| $25-$49 999 | 3 (15) | 4 (50) | |
| $50-$74 999 | 2 (10) | 0 | |
| ≥$75 000 | 9 (45) | 1 (12) | |
| College or university degree, n (%) | 6 (30) | 2 (25) | NS |
| Smoker, n (%) | 4 (20) | 0 | NS |
Abbreviations: NS, not significant; SD, standard deviation.
Comparison of the routine practices for open carpal tunnel release between the 2 primary surgeons (A.T. and N.N.) identified some distinct differences. Although both surgeons performed a variation of a short scar or classic open carpal tunnel release, carpal tunnel release (CTR) in Canada was performed under local anaesthesia in a minor procedure room setting with only 1 registered nurse or registered practical nurse and no anesthesiologist present . A medical trainee (resident or medical student) was present to assist. Mean operative time was 15 ± 5 minutes, and total time in the procedure room was 23 ± 8 minutes (measured by total nursing time).
CTR at the US site was performed in a main operating room under regional anesthesia (Bier block) with an anesthesiologist and 3 registered nurses or licensed practical nurses present. Mean operative time was 8 ± 3 minutes. Each case was booked for 30 minutes. One patient sustained an adverse event unrelated to the surgery (fall from standing) 4 weeks postoperatively. No other complications were identified.
Mean total costs were less in Canada compared to the United States ($1581 ± $1965 vs $2179, range: $1421-$2741) resulting in a cost difference of $598. Direct costs of CTR in Canada and the United States were $541 ± $102 and $1176 (range: 426-1738), respectively. Breakdown of costs is summarized in Table 2. Direct costs from the US institution were provided as a mean and range. Patient charges were $2185 for patients with private insurance and $1638.75 for self-pay.
Table 2.
Direct and Indirect Costs of Open Carpal Tunnel Surgery in Canada and the United States.
| Canada (US$) | US (US$) | |
|---|---|---|
| Direct costs, mean (SD) | 541 (102) | 1176 (426-1738)a |
| Consultation | 100 | |
| Facility, mean $ (SD) | 186 (77) | |
| Supplies | 46 | 51 |
| Nursing | 32 | |
| Anesthesia | NA | |
| Surgeon | 189 | |
| Follow-up | 65 | |
| Indirect costs, mean (SD) | 1039 (1963) | 1002 (1499) |
| Physiotherapy, mean $ (SD) | 17 (74) | 210 (165) |
| Mileage, mean $ (SD) | 7 (19) | 36 (40) |
| Parking, mean $ (SD) | 15 (8) | NA |
| Other (splints, bandages, and medications) | 10 (9) | 6 (5) |
| Productivity loss (societal) | ||
| Personal, $ (SD) | 816 (1932) | 675 (1483) |
| Caregiver, $ (SD) | 170 (337) | 75 (139) |
| Total direct + indirect | 1581 (1965) | 2179 (1421-2741)a |
Abbreviations: NA, not applicable; SD, standard deviation.
arange
Total mean indirect costs were similar in Canada compared to the United States ($1039 ± $1963 vs $1002 ± $1499). All 8 patients in the United States attended physiotherapy compared to only 1 of 21 in Canada. Personal expenditures (parking, gas, and medications) only comprised a small proportion of the indirect costs. Employed patients and caregivers required similar time off work (United States: 5.8 ± 10.2 days and 0.4 ± 0.8 days, respectively; Canada: 7.6 ± 12.2 days and 0.8 ± 1.7 days, respectively). Costs due to productivity loss between US and Canadian patients averaged $675 ± $1483 and $816 ± $1932 when considering all patients in the study sample, respectively.
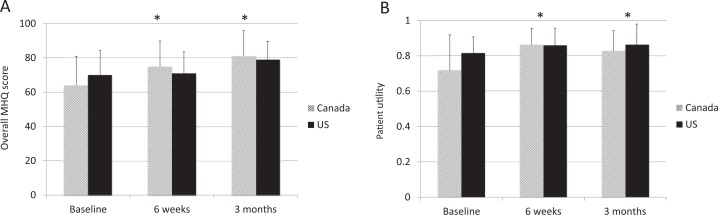
Quality of life improved significantly at both 6-week and 3-month time points following carpal tunnel release. There were no significant differences in quality-of-life scores at each time point between patients in Canada and the United States (Figure 1). At 3 months postoperatively, overall MHQ scores for Canadian and US patients improved from baseline scores of 64 ± 17 and 70 ± 14 to 81 ± 15 and 79 ± 11, respectively (P < .001). EQ-5D utility values also improved significantly from baseline. At 3 months postoperatively, EQ-5D utility scores for Canadian and US patients improved from baseline scores of 0.72 ± 0.20 and 0.81 ± 0.09 to 0.83 ± 0.12 and 0.86 ± 0.12, respectively (P = .008).
Figure 1.
Health-related quality of life outcomes preoperatively and 6 weeks and 3 months postoperatively. (A) Michigan Hand Questionnaire and (B) EuroQOL 5D. *P < .05 compared to baseline.
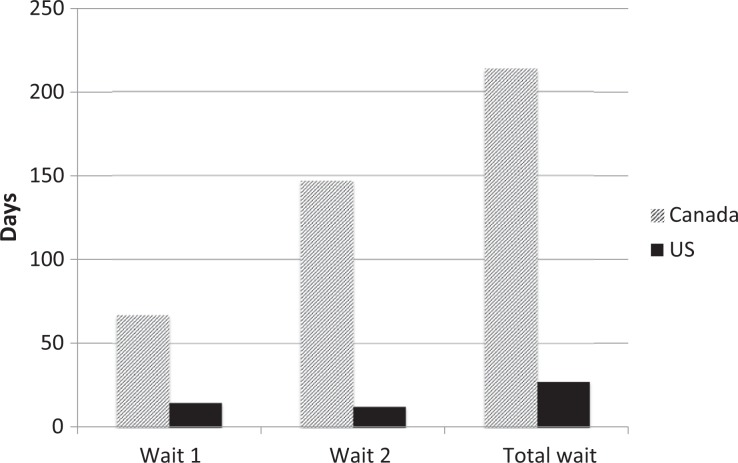
Wait times for carpal tunnel surgery in Canada were significantly longer than in the United States. Wait times from referral to initial consultation with a hand surgeon (wait 1) were 66 ± 103 days and 15 ± 9 days in Canada and the United States, respectively (P = .180). Wait times from decision to operate to surgery (wait 2) were 147 ± 60.5 days and 12 ± 4 days (P < .001), respectively. Total wait times from initial referral to surgery in Canada and the United States were 214 ± 119 days and 27 ± 10 days, respectively (P < .001; Figure 2).
Figure 2.
Wait times for carpal tunnel surgery. Wait 1: time from initial referral to initial consultation; wait 2: time from decision to operate to surgery; total wait: wait 1 + wait 2.
Although carpal tunnel release resulted in similar improvements in quality of life, significantly shorter wait times for US patients resulted in a gain of 0.077 QALYs compared to their Canadian counterparts. An ICUR was then calculated to be $7758/QALY.
One-way sensitivity analyses demonstrated that the results were robust. Variations in the costs of carpal tunnel surgery had little impact on the overall ICUR. As illustrated in Figure 3, carpal tunnel surgery in the United States would remain cost-effective (ICUR < $50 000/QALY) unless total costs exceed $5500 per surgery (cost difference >$4000). Since patients in the United States may be charged more than the actual cost of services, sensitivity analyses were performed to consider patient charges instead of cost; the US system remains favored (ICUR $20 828/QALY). Similarly, wait times for surgery in Canada would have to be reduced to less than 60 days before the US system would become less favorable.
Figure 3.
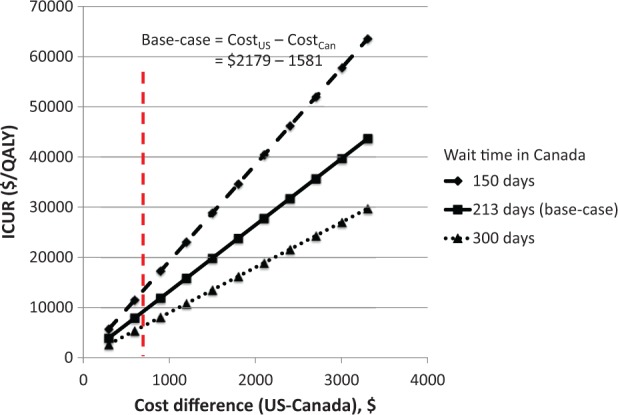
Sensitivity analysis of the incremental cost-utility ratio (ICUR) varying the difference in total costs and wait times for carpal tunnel surgery in the United States versus Canada. Dashed vertical line indicates base-case scenario.
Discussion
Patients with carpal tunnel syndrome experienced significant improvements in quality of life following carpal tunnel surgery. This improvement was similar between patients treated in Canada and the United States. Significant differences in cost and wait times for surgery between these patients, however, demonstrate inefficiencies in both health-care systems. From this prospective pilot study, an ICUR of $7758/QALY was calculated; this is below the conventional willingness-to-pay threshold of $50 000/QALY thus favoring the US system.19
Although no prior study has compared both the costs and effectiveness of health care in Canada and the United States, previous studies have independently demonstrated lower costs in Canada, with similar outcomes but longer wait times. Antoniou et al demonstrated lower in-hospital costs for Canadian patients undergoing total hip arthroplasty, while wait times for knee replacement surgery were longer in Canada compared to American counterparts.1,3 A systematic review suggested similar, possibly superior, health outcomes across multiple health conditions including cancer, coronary artery disease, chronic medical illnesses, and surgical procedures for patients treated in Canada versus the United States.8 Our study supports these findings—costs were less, wait times were longer, and improvements in HRQOL directly associated with surgery were similar for carpal tunnel surgery in Canada compared to the United States.
Previous cost-effectiveness studies of carpal tunnel surgery offer the opportunity for comparison; however, most are limited by a lack of prospective data or failure to account for indirect costs. Multiple authors have independently performed cost-effectiveness analyses comparing endoscopic to open carpal tunnel release.20–22 Reported costs of open carpal tunnel surgery were similar to our results. Chung et al performed a decision analytic model based on a hypothetical group of patients in the United States.20 Only direct costs were considered based on Medicare relative value units with sensitivity analyses performed for costs associated with private practice in Southeastern Michigan. For open carpal tunnel release, costs (in US$1997) were $842 and $2202 for Medicare and private practice, respectively.
Vasen et al found similar costs—the reimbursement of open carpal tunnel surgery by the Massachusetts Department of Industrial Accidents was $1672.21 The total cost, however, was $6315 after accounting for lost wages due to absence from work. Time to return to work was estimated to be 54 days, but this was estimated from previous randomized controlled trials that included a mix of patients with and without worker’s compensation. In contrast, employed patients in our study missed 7.6 ± 12.2 and 5.8 ± 10.2) days of work in Canada and the United States, respectively. Five patients in Canada and 2 patients in the United States required caregiver assistance postoperatively resulting in caregiver time off work of a mean of 0.8 ± 1.7 and 0.4 ± 0.8 days, respectively.
Time off work varied in the literature. Saw et al. performed a prospective randomized controlled trial comparing endoscopic to open carpal tunnel release in the United Kingdom.22 Time off work for employed patients undergoing open carpal tunnel surgery was 26 (±14) days. No patients in their study required additional support from a community support or caregiver. Korthals-de Bos et al performed an economic evaluation alongside a randomized controlled trial comparing splinting to open carpal tunnel release in the Netherlands.23 Mean cost for patients undergoing surgery was €2126 including both direct and indirect costs. Indirect costs included lost wages for a mean of 9.2 days off work after excluding outliers.
Effectiveness of carpal tunnel surgery was similar to previously reported studies. Chung et al surveyed nurses, hand therapists, and surgical residents using the rating method to determine the utility for several of hypothetical situations.20 Baseline utility for patients with carpal tunnel syndrome was 6.98 (of 10) compared to 0.72 (of 1) and 0.81 for our patients in Canada and the United States, respectively. Chung et al assumed that patients returned to perfect health following successful surgery (utility = 10). In our study, patient utility at 3 months postoperatively reached 0.83 and 0.86 in Canada and the United States, respectively. Korthals-de Bos et al similarly used the EQ-5D and found patient utility to be 0.85 (0.12) following carpal tunnel release.23 Imperfect health-related quality of life (HRQOL) following successful surgery was similar to the self-reported health status of the age-matched general adult US population.24
Limitations of this study include the small sample size and consideration of only 1 institution in each health-care system. Even with modest recruitment goals, we were only able to recruit 8 patients from the US centre. At interim review, we identified that a large number of patients presented with bilateral carpal tunnel syndrome were excluded because of their desire for contralateral surgery before the study end point at 3-month follow-up.
Due to the single payer public health-care system, cost data from the single Canadian centre are likely generalizable to nonworker’s compensation patients across Ontario. Variations exist across Canada, as health care is administered at a provincial level. It is more difficult, however, to generalize cost data across the United States based on a single center due to the multipayer public/private health-care system. Sensitivity analyses, however, offer the opportunity to account for these unpredictable variations. Even with cost differences between the United States and Canada approaching $4000 (base-case: $598), the US system remained cost-effective.
Mean total wait times of 213 days likely underestimated the wait times for open carpal tunnel surgery in Canada. Because of knowledge of study enrolment, office administrators would prioritize patients with carpal tunnel syndrome to be seen sooner in initial consultation. Instead of the 67-day wait time from referral to initial consultation in the current study; the typical wait time is approximately 8 to 9 months (240-270 days). Total wait times in Canada would thus be closer to 390 days, further favoring the US system.
Although cost-effectiveness analysis favored the US system due to significantly shorter wait times, detailed prospective analysis offers the opportunity to identify areas to improve efficiency in both health-care systems. Good evidence demonstrates that open carpal tunnel release can be performed under local anesthetic in a minor procedure room without anesthesia presence at lower cost and similar outcomes including patient satisfaction.25–27 Similarly, there is a paucity of evidence supporting routine prescription of physiotherapy following carpal tunnel release.28
Reducing wait times in Canada remains a challenge. Simply increasing the physician workforce may not be the solution.29 Barriers exist not only to timely access to hand/plastic surgeons for carpal tunnel syndrome, as evident from wait times from referral to initial consultation, but also to availability of operating room resources, illustrated by wait times from decision to operate to the time of surgery.
Conclusion
Our pilot study demonstrates the feasibility of prospectively measuring the costs and effectiveness of open carpal tunnel release at institutions in Canada and the United States in a larger trial. Preliminary results suggest that, despite higher costs, carpal tunnel surgery in the United States is more cost-effective due to HRQOL implications of extended wait times in Canada. Further investigation may improve generalizability of results and elucidate specific areas for improved efficiency.
Footnotes
Level of Evidence: Risk, Level 2
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Antoniou J, Martineau PA, Filion KB, et al. In-hospital cost of total hip arthroplasty in Canada and the United States. J Bone Joint Surg. 2004;86-A(11):2435–2439. [DOI] [PubMed] [Google Scholar]
- 2. Roos LL, Fisher ES, Brazauskas R, Sharp SM, Shapiro E. Health and surgical outcomes in Canada and the United States. Health Aff (Millwood). 1992;11(2):56–72. [DOI] [PubMed] [Google Scholar]
- 3. Coyte PC, Wright JG, Hawker GA, et al. Waiting times for knee-replacement surgery in the United States and Ontario. New Engl J Med. 1994;331(16):1068–1071. [DOI] [PubMed] [Google Scholar]
- 4. Tu JV, Pashos CL, Naylor CD, et al. Use of cardiac procedures and outcomes in elderly patients with myocardial infarction in the United States and Canada. N Engl J Med. 1997;336(21):1500–1505. [DOI] [PubMed] [Google Scholar]
- 5. Ho V, Hamilton BH, Roos LL. Multiple approaches to assessing the effects of delays for hip fracture patients in the United States and Canada. Health Serv Res. 2000;34(7):1499–1518. [PMC free article] [PubMed] [Google Scholar]
- 6. Gorey KM, Kliewer E, Holowaty EJ, Laukkanen E, Ng EY. An international comparison of breast cancer survival. Ann Epidemiol. 2003;13(1):32–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bell CM, Crystal M, Detsky AS, Redelmeier DA. Shopping around for hospital services: a comparison of the United States and Canada. JAMA. 1998;279(13):1015–1017. [DOI] [PubMed] [Google Scholar]
- 8. Guyatt GH, Devereaux PJ, Lexchin J, Stone SB, et al. A systematic review of studies comparing health outcomes in Canada and the United States. Open Med. 2007;1(1):E27–E36. [PMC free article] [PubMed] [Google Scholar]
- 9. Redelmeier DA, Fuchs VR. Hospital expenditures in the United States and Canada. N Engl J Med. 1993;328(11):772–778. [DOI] [PubMed] [Google Scholar]
- 10. Woolhandler S, Campbell T. Costs of health care administration in the United States and Canada. New Engl J Med. 2003;349(8):768–775. [DOI] [PubMed] [Google Scholar]
- 11. Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the panel on cost-effectiveness in health and medicine. JAMA. 1996;276(15):1253–1258. [PubMed] [Google Scholar]
- 12. Goossens M, Rutten-van Mölken MP, Vlaeyen JW, van der Linden SM. The cost diary: a method to measure direct and indirect costs in cost-effectiveness research. J Clin Epidemiol. 2000;53(7):688–695. [DOI] [PubMed] [Google Scholar]
- 13. Goeree R, O’Brien BJ, Blackhouse G, Agro K, Goering P. The valuation of productivity costs due to premature mortality: a comparison of the human-capital and friction-cost methods for schizophrenia. Can J Psychiatry. 1999;44(5):455–463. [DOI] [PubMed] [Google Scholar]
- 14. Statistics Canada. Table 380-0037—Purchasing Power Parities for Gross Domestic Product (GDP), Organisation for Economic Co-operation and Development (OECD) Countries, Annual (National Currency per Canadian Dollar). http://www5.statcan.gc.ca/cansim/a26. Accessed September, 2013.
- 15. Marra CA, Woolcott JC, Kopec JA, et al. A comparison of generic, indirect utility measures (the HUI2, HUI3, SF-6D, and the EQ-5D) and disease-specific instruments (the RAQoL and the HAQ) in rheumatoid arthritis. Soc Sci Med. 2005;60(7):1571–1582. [DOI] [PubMed] [Google Scholar]
- 16. Kotsis SV, Chung KC. Responsiveness of the Michigan hand outcomes questionnaire and the disabilities of the arm, shoulder and hand questionnaire in carpal tunnel surgery. J Hand Surg. 2005;30(1):81–86. [DOI] [PubMed] [Google Scholar]
- 17. Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care. 2005;43(3):203–220. [DOI] [PubMed] [Google Scholar]
- 18. Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ. 2005;14(5):487–496. [DOI] [PubMed] [Google Scholar]
- 19. Laupacis A, Feeny D, Detsky AS, Tugwell PX. How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. Can Med Assoc J. 1992;146(4):473–481. [PMC free article] [PubMed] [Google Scholar]
- 20. Chung KC, Walters MR, Greenfield M, Chernew ME. Endoscopic versus open carpal tunnel release: a cost-effectiveness analysis. Plast Reconstr Surg. 1998;102(4):1089–1099. [DOI] [PubMed] [Google Scholar]
- 21. Vasen AP, Kuntz KM, Simmons BP, Katz JN. Open versus endoscopic carpal tunnel release: a decision analysis. J Hand Surg. 1999;24(5):1109–1117. [DOI] [PubMed] [Google Scholar]
- 22. Saw N. Early outcome and cost-effectiveness of endoscopic versus open carpal tunnel release: a randomized prospective trial. J Hand Surg Brit Eur. 2003;28(5):444–449. [DOI] [PubMed] [Google Scholar]
- 23. Korthals-de Bos I, Gerritsen A, van Tulder MW, et al. Surgery is more cost-effective than splinting for carpal tunnel syndrome in the Netherlands: results of an economic evaluation alongside a randomized controlled trial. BMC Musculoskelet Disord. 2006;7:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Luo N, Johnson JA, Shaw JW, Feeny D, Coons SJ. Self-reported health status of the general adult U.S. population as assessed by the EQ-5D and Health Utilities Index. Med Care. 2005;43(11):1078. [DOI] [PubMed] [Google Scholar]
- 25. Chatterjee A, McCarthy JE, Montagne SA, Leong K, Kerrigan CL. A cost, profit, and efficiency analysis of performing carpal tunnel surgery in the operating room versus the clinic setting in the United States. Ann Plast Surg. 2011;66(3):245–248. [DOI] [PubMed] [Google Scholar]
- 26. LeBlanc MR, Lalonde J, Lalonde DH. A detailed cost and efficiency analysis of performing carpal tunnel surgery in the main operating room versus the ambulatory setting in Canada. Hand (N Y). 2007;2(4):173–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. LeBlanc MR, Lalonde DH, Thoma A, et al. Is main operating room sterility really necessary in carpal tunnel surgery? A multicenter prospective study of minor procedure room field sterility surgery. Hand (N Y). 2010;6(1):60–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Peters S, Page MJ, Coppieters MW, Ross M, Johnston V. Rehabilitation following carpal tunnel release. Cochrane Database Syst Rev. 2013;(6):CD004158. [DOI] [PubMed] [Google Scholar]
- 29. Cheung K, Sweetman A, Thoma A. Plastic surgery wait times in Ontario: a potential surrogate for workforce demand. Can J Plast Surg. 2012;20(4):229–232. [DOI] [PMC free article] [PubMed] [Google Scholar]