Abstract
Background:
Intraoperative nerve stimulation is done routinely in brachial plexus and peripheral nerve surgery as well as in selective neurectomy in spastic patients.
Objective:
The current study compares the use of 2 different devices for nerve stimulation: a totally disposable nerve stimulator and a nerve stimulator used for nerve blocks by anesthetists.
Methods:
A retrospective study of 60 patients who underwent brachial plexus surgery: In 30 patients, we used the totally disposable nerve stimulator (group 1) and in another 30 patients, we used the anesthesia device (group 2). The cost of disposable materials used for nerve stimulation was calculated in each group. The same surgeon performed all operations, and he was asked to give his subjective opinion regarding the convenience and ease of use of the device in each group.
Results:
The main advantages of the totally disposable device are its placement totally within the sterile field, and it is operated by the surgeon without the need to communicate with the anesthetist. However, the totally disposable device had several major disadvantages when compared to the anesthesia device. Firstly, the disposable stimulator can only deliver 0.5, 1.0, and 2.0 mA stimuli, while the anesthesia device can deliver stimuli of 0.1 to 5 mA (in 0.1 mA increments). Secondly, the disposable stimulator frequently fails to operate during surgery, and this is not experienced with the anesthesia device. Finally, the cost of disposables is less using the anesthesia device.
Conclusion:
Our center has stopped using the disposable nerve stimulator in favour for the anesthesia device.
Keywords: brachial plexus, surgery, nerve stimulation
Abstract
Historique :
La stimulation nerveuse intraopératoire est utilisée régulièrement lors d’opérations du plexus brachial et des nerfs périphériques, de même que lors de neurectomies sélectives chez les patients spastiques.
Objectif :
La présente étude visait à comparer deux dispositifs différents pour la stimulation nerveuse, soit un stimulateur nerveux entièrement jetable et un stimulateur nerveux qu’utilisent les anesthésistes pour les blocages nerveux.
Méthodologie :
Les chercheurs ont effectué une étude rétrospective auprès de 60 patients qui avaient subi une opération du plexus brachial. Chez 30 patients, ils ont utilisé le stimulateur nerveux entièrement jetable (groupe I) et chez 30 autres, le dispositif d’anesthésie (groupe II). Les chercheurs ont calculé le coût des fournitures jetables utilisées pour la stimulation nerveuse dans chaque groupe. Le même chirurgien a effectué toutes les opérations et a été invité à donner son avis subjectif sur le caractère pratique et la facilité d’utilisation du dispositif dans chaque groupe.
Résultats :
Les dispositifs complètement jetables ont comme principaux avantages de se situer entièrement dans le champ stérile et d’être utilisés par le chirurgien sans qu’il communique avec l’anesthésiste. Cependant, ils comportent plusieurs désavantages par rapport au dispositif d’anesthésie. D’abord, ils peuvent seulement délivrer un stimulus de 0,5 mA, 1,0 mA et 2,0 mA, alors que les dispositifs d’anesthésie en délivrent de 0,1 mA à 5 mA (par incréments de 0,1 mA). Ensuite, le stimulateur jetable est souvent défaillant pendant la chirurgie, ce qui ne se produit pas avec le dispositif d’anesthésie. Enfin, le dispositif d’anesthésie réduit le coût des fournitures jetables.
Conclusion :
Le centre des chercheurs a cessé d’utiliser le stimulateur nerveux jetable au profit du dispositif d’anesthésie.
Introduction
Intraoperative nerve stimulation is done routinely in brachial plexus surgery. Totally disposable nerve stimulators are widely used during brachial plexus surgery mainly because the entire device is sterile and is placed within the sterile field.1
Brachial plexus blocks and other nerve blocks are performed by anesthetists using a device that has 2 components: a non-sterile, battery-operated nerve stimulator which is connected to a sterile wire/needle.2,3
For many years, our center has been using a totally disposable nerve stimulator during brachial plexus surgery. We have noted that the stimulator may fail to operate or operate intermittently during surgery, necessitating the use of more than 1 device in almost all cases. Failure was apparently from faulty probe tip–battery connections rather from battery failure because the battery light indicator was always present despite the failure of nerve stimulation. Two years ago, we started using the anesthesia nerve block device during brachial plexus surgery. A review of the literature did not reveal any study comparing these 2 techniques of nerve stimulation in brachial plexus surgery, and the current study compares the 2 techniques with regard to cost, convenience, and ease of use.
Materials and Methods
This study was approved by the research committee of the Department of Surgery at our hospital.
The Devices
The totally disposable nerve stimulator used in our brachial plexus surgery is the VARI-STIM III nerve stimulator (Medtronic Inc, Jacksonville, Florida) and is shown in Figure 1. It is a sterile, single-use, hand-held device which is placed within the sterile field. When the probe tip is in direct contact with the nerve, the device can deliver 0.5, 1, or 2 mA stimuli (by adjusting the probe knob). The base of the probe has a grounding needle which is inserted subcutaneously in the wound during stimulation. Each device costs our hospital $60.
Figure 1.
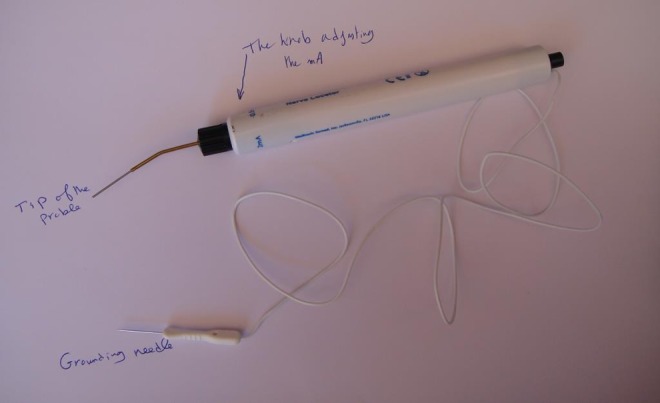
The total disposable nerve stimulator.
The anesthesia nerve block device available at our anesthesia department is Stimuplex HNS11 (Braun Medical Inc, Bethlehem, Pennsylvania; Figure 2). The stimulator device is non-sterile and battery operated. It can deliver stimuli of 0.1 to 5 mA (in 0.1 mA increments). The cost of the Stimuplex device is $1500. However, this is a one-time cost and the device has no limit in the number of times it can be reliably used as long as the battery is functional. This cost will not be included in the cost analysis because the device is routinely purchased by the Department of Anesthesia for nerve blocks, and hence, it is already available for use free of charge for the Department of Surgery. The anode is placed on the skin of the patient (outside the sterile field) via an ECG electrode. The cathode is connected to a sterile wire and needle marketed as Sonoplex Stim cannula (Pajunk, Geisingen, Germany). The sterile wire/needle is disposable and costs our hospital $9. After draping the patient, the sterile wire/needle is placed near the operative site to ensure that it will reach the brachial plexus easily (Figure 3). A small hole is made in the drape to connect the wire to the cathode of the nerve stimulator, and the hole in the drape is covered with Tegaderm (3M, St Paul, Minnesota), as shown in Figure 4. The Tegaderm sheet has an adhesive; hence, it seals the sterile field and minimizes movements of sterile wire at the hole made in the sterile drape (Figure 4). Each Tegaderm sheet costs our hospital $1. During nerve stimulation, the surgeon instructs the anesthetist to adjust the mA knob of the nerve stimulator.
Figure 2.
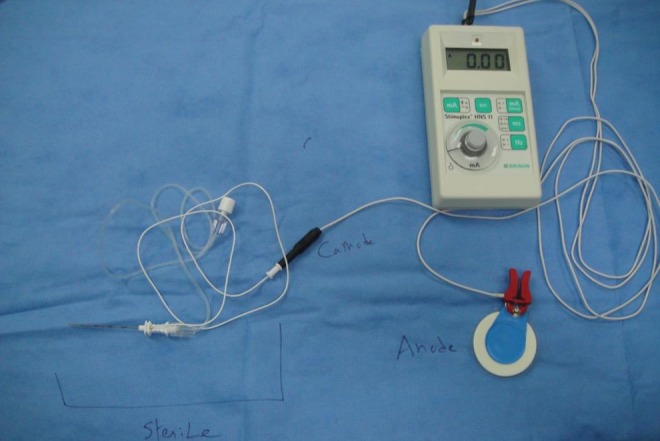
The anesthesia nerve block device (non-sterile) connected to the sterile wire/needle at the cathode.
Figure 3.

The anesthesia device in use in a case of obstetric paralysis.
Figure 4.

A close-up of hole made in the sterile drapes covered by the Tegaderm sheet.
Patients
A retrospective study of 60 patients who underwent brachial plexus surgery: In 30 patients, we used the totally disposable nerve stimulator (group 1), and in another 30 patients, we used the non-sterile stimulator with the sterile wire/needle (group 2). The cost of disposable materials used for nerve stimulation was calculated in each group. The same surgeon performed all the operations, and he was asked to give his subjective opinion regarding the convenience and ease of use of the device in each group.
Results
In group 1, the totally disposable nerve stimulator failed to operate at least once during surgery. In the 30 operated patients, 70 stimulators were used (a total cost of $4200). In group 2, there were no instances of failures of stimulation and the combined cost of the disposable wire/needle and the Tegaderm sheet was $300. The totally disposable nerve stimulator (group 1) was easier to use because the entire device can be placed within the sterile field and the device was totally operated by the surgeon without communicating with the anesthetist. However, the anesthesia device was preferred mainly because of the convenience of raising the mA from 0.1 to 5 mA at 0.1 mA increments. The surgeon has stopped using the disposable nerve stimulator in favour for the anesthesia device.
Discussion
Nerve stimulation in upper limb operations is used for axillary and brachial plexus blocks,2,3 selective neurectomy in spastic patients,4,5 and intraoperative nerve stimulation during brachial plexus surgery.1,6-8
In brachial plexus surgery, nerve stimulation is used for specific nerve identification such as the phrenic1 and the accessory spinal8 nerves. In certain situations, the degrees of nerve stimulation and motor response are critical for intraoperative decisions. Two examples are distal nerve transfers6 and management of conducting neuromas-in-continuity.7 For example, Oberlin distal nerve transfer from the ulnar nerve to the biceps nerve requires selecting the fascicle that mainly supplies the flexor carpi ulnaris.6 The lowest mA of the totally disposable nerve stimulator is 0.5 mA and this may cause overstimulation to adjacent fascicles (particularly before inter-fascicular dissection of the ulnar nerve). Selection is usually easier using lower mA, which can be provided by the anesthesia device. Another example is the intraoperative decision either to excise the conducting neuroma-in-continuity or to do neurolysis.7 That decision is mainly based on the distal muscle response upon stimulation, which is best done using a graded mA stimuli. This explains why our surgeon preferred the anesthesia device. The anesthesia nerve stimulator can also give the surgeon more options regarding pulse duration (which may be adjusted from 0.1 to 0.3 milliseconds). A stretched nerve may need longer pulse duration to show a response. Another option is the ability to adjust the frequency of stimulation (from 1 to 2 Hz), which is helpful while searching for a specific nerve such as the spinal accessory nerve.
Brachial plexus surgeons do not normally consider cost as a major issue in brachial plexus surgery. For example, most surgeons have switched from micro-sutures to fibrin glue (the latter is much more expensive) in nerve repair mainly because coaptation is easier, quicker, and more accurate using the glue. However, cost remains an important issue for hospital administration. The results of our study were welcomed by our hospital because the surgeon favoured the less costly device. Furthermore, the anesthesia device is of better quality than the disposable nerve stimulation because the former provides a wider range of mA stimuli with the extra options of adjusting the pulse duration and stimulation frequency at each selected stimulus strength.
Footnotes
Level of Evidence: Level 4, Therapeutic
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Al-Qattan MM. Identification of the phrenic nerve in surgical explanations of the brachial plexus on obstetrical palsy. J Hand Surg Am. 2004;29(3):391–392. [DOI] [PubMed] [Google Scholar]
- 2. Singh S, Goyal R, Upadhyang KK, et al. An evaluation of brachial plexus block using a nerve stimulator versus ultrasound guidance: a randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2015;31(3)370–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Killicaslan A, Topal A, Taylan A, Erol A, Otelcioglu S. Differences in tip visibility and nerve block parameters between two echogenic needles during a stimulation study with experienced anesthesia trainees. J Anesth. 2014;28(3):460–462. [DOI] [PubMed] [Google Scholar]
- 4. Leclercq C. General assessment of the upper limb. Hand Clin. 2003;19(4):557–564. [DOI] [PubMed] [Google Scholar]
- 5. Cambon-Binder A, Leclercq C. Anatomical study of the musculocutaneous nerve branching pattern: application for selective neurectomy in the treatment of elbow flexors spasticity. Surg Radiol Anat. 2015;37(4):341–348. [DOI] [PubMed] [Google Scholar]
- 6. Teboul F, Kakkar R, Ameur N, Beaulieu JY, Oberlin C. Transfer of fascicles from the ulnar nerve to the nerve to the biceps in the treatment of upper brachial plexus palsy. J Bone Joint Surg Am. 2004;86(7):1485–1490. [DOI] [PubMed] [Google Scholar]
- 7. Clarke HM, Al-Qattan MM, Curtis CG, Zuker RM. Obstetrical brachial plexus palsy: results following neurolysis of conducting neuromas-in-continuity. Plast Reconstr Surg. 1996;97(5):974–982. [DOI] [PubMed] [Google Scholar]
- 8. Dailiana ZH, Mehdian H, Gilbert A. Surgical anatomy of spinal accessory nerve: is trapezius functional deficit inevitable after division of the nerve. J Hand Surg Br. 2001;26(2):137–141. [DOI] [PubMed] [Google Scholar]


