Abstract
Medication errors threaten patient safety by requiring admission, readmission, and/or a longer hospital stay, and can even be fatal. Near-misses indicate the potential for medication errors to have occurred. Therefore, reporting near-misses is a first step in preventing medication errors. The aim of this study was to estimate the reporting rate of near-misses among pharmacists in Korean hospitals, and to identify the factors that contributed to reporting medication errors.
We surveyed 245 pharmacists from 32 hospital pharmacies for medication errors, including near-misses. We asked them to describe their experiences of near-misses in dispensing, administration, and prescribing, and to indicate the percentage of near-misses that they reported. Additionally, we asked questions related to the perception of medication errors and barriers to reporting medication errors. These questions were grouped into 4 categories: protocol and methods of reporting, incentives and protections for reporters, attitude related to reporting, and fear. Descriptive statistics and logistic regression were conducted to analyze the data.
Five or more near-misses per month were experienced by 14.8%, 4.3%, and 43.9% of respondents for dispensing, administration, and prescribing errors, respectively. The percentages of respondents who stated that they reported all near-misses involving dispensing errors, administration errors, and prescribing errors were 43.7%, 57.4%, and 37.1%, respectively. Unclear reporting protocols and the absence of harm done to patients were significant factors contributing to the failure to report medication errors (P < .05).
Advances can still be made in the frequency of reporting near-misses. Clear and standardized policies and procedures are likely to increase the reporting rates.
Keywords: hospital pharmacists, medication errors, near-misses, patient safety
1. Introduction
Medications are generally beneficial but can sometimes cause harm, which can occasionally be attributed to errors. Medication errors affect patient safety by requiring admission, readmission, and/or a longer hospital stay, and can even be fatal. They may also incur additional medical costs. Reducing medication errors is an issue that should be addressed.
The Institute of Medicine (IOM) report “To Err Is Human: Building a Safer Health System” raised awareness of medical errors and identified medication errors in health care.[1] The potential for a medication error is present in each step of the medication use process: procuring, prescribing, dispensing, administering the drug, and monitoring the patient's response.[2] The European Medicines Agency has estimated the rate of medication error in European hospital settings to be 0.3% to 9.1% during the prescription stage, 1.6% to 2.1% during the dispensing stage, and 10.5% during the administration stage.[3] A review of medication errors in Middle Eastern countries found that prescribing error rates varied from 7.1% to 90.5%, while administration error rates varied from 9.4% to 80%, although variations were present in definition, setting, and methodology.[4] In South Korea, a survey of administration errors for nurses showed that 63.6% of the participants had been involved in medication errors once or more in the past month.[5] Nurses and doctors in a hospital experienced administration errors an average of 2.3 times per year.[6]
Medication errors can also be categorized according to the severity of the consequences. The National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) classifies its medication error index into 9 categories: no error (category A), error and no harm (categories B–D), error and harm (categories E–H), and error and death (categories I).[7] The American nonprofit Institute for Safe Medication Practices (ISMP) defines a “near-miss” as an event, situation, or error that occurred but did not reach the patient.[8] Near-misses can be classified as belonging to category B of the NCC MERP classification.[7] Near-misses do not reach the patient, but can still potentially cause harm. In 1 emergency department, the rate of an error occurring but not reaching the patient was 11.8%.[9] In a prospective study of 35 community pharmacies in the UK, 84.8% of recorded medication errors were near-misses, while 15.2% were dispensing errors.[10] In the Spanish community, 36% of medication errors were dispensing near-misses, and 10% were dispensing errors.[11]
To reduce the incidence of medication errors, quantifying and reporting medication errors are the first steps in the process of ensuring patient safety and learning from incidents.[3] The National Reporting and Learning Service and the National Health Service Confederation in the UK have recommended that organizations improve patient safety by strengthening reporting and learning, and have stated that they consider high reporting to be a mark of a highly reliable organization.[12] One study estimated that approximately 60% of medication administration errors (MAEs) were actually reported.[13] In a survey about MAEs, 47% of the participating nurses had failed to report MAEs committed by themselves or their colleagues.[14] One study found that the majority of pharmacy staff (pharmacists and technicians) who participated in a survey reported having experienced a near-miss, but only 10% reported the occurrence.[15] The reporting rates were diverse but not high. A low reporting rate of medication errors precludes identifying and preventing the causes. Not reporting medication errors limits opportunities to improve patient safety. Barriers to reporting medication errors and near-misses have been reported to include culture, the reporting system, management behavior, fear, accountability, and the harm to patients.[16,17] Understanding the barriers to reporting errors is a crucial step in improving patient safety.
In this study, we focused on near-misses in hospital pharmacies, since they can easily be ignored but are important for building a framework of patient safety. We also surveyed pharmacists because they play a role in dispensing, administration, and prescription review. Therefore, our aim was to estimate the reporting rates among pharmacists in Korean hospitals. We also analyzed factors contributing to reporting medication errors.
2. Methods
2.1. Participants and survey methods
We surveyed all members of the Korean Society of Health-System Pharmacists (KHSP) from June 2014 to September 2014. First, we emailed their managers requesting that they allow hospital pharmacists to participate in the study. We explained the objectives and contents of this study. We sent questionnaires and informed consent forms to all pharmacists in hospital pharmacies that had agreed to participate. The pharmacists were asked to return the completed questionnaires by email, mail, or fax. They could also complete the questionnaire online. We sent reminders twice to improve response rate. Further, managers were called 1 time to encourage pharmacists to join the survey. Questionnaires were collected by a third party at KHSP for anonymity.
2.2. Definitions
We used the NCC MERP definition of medication errors, since it is widely used,[3] and the ISMP definition of near-misses.
“A medication error is any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer. Such events may be related to professional practice, health care products, procedures, and systems, including prescribing, order communication, product labeling, packaging, and nomenclature, compounding, dispensing, distribution, administration, education, monitoring, and use.[18]”
“Near-miss (close call): An event, situation, or error that took place but was captured before reaching the patient.[8]”
2.3. Instruments
The questionnaire surveyed participants’ experiences of near-misses, their reporting rate, the pharmacy system, perceptions of medication errors, reasons for underreporting, and demographic factors.
We surveyed experiences of near-misses according to the medication use process, which is divided into stages of prescribing, dispensing, and administration. In this study, we considered dispensing and administration errors to be within the scope of pharmacists’ active duties; in contrast, prescribing errors included dosage errors, incorrect directions, illegible prescriptions, and so on, which pharmacists could identify during the process of prescription review. Before pharmacists answered the questions, we asked whether near-misses are considered medication errors, and then explained the definitions of medication errors and near-misses. We also asked how many participants found prescribing errors or made dispensing errors and administration errors during the last 3 months, and whether they had reported near-misses.
Previous studies have identified the following factors as barriers to the reporting of medication errors: fear, disagreement over the error, the administrative response, the effects of reporting, and the reporting process.[14,19,20] We referred to studies of Korean health professionals’ perceptions of medication errors and reporting to understand the most common barriers to reporting.[6,21] We selected 15 common barriers to reporting medication errors, and grouped them into 4 categories: protocol and methods of reporting, incentives and protections for reporters, attitude related to reporting, and fear. The protocol and methods of reporting group included unclear reporting protocol for medication errors, no time to report (heavy workload), no obligation to report, complicated and lengthy procedure and no system to report medication errors. The incentives and protections for reporters group included no legal protection, no incentive to report, and blame culture in the hospital. The attitude related to reporting group included the belief that there is no need to report, no harm done to the patients, and no changes instituted after reporting to prevent future errors. The fear group included fear of blame by patients, fear of blame by colleagues, fear of punishment, and fear of indemnity. Survey participants selected “agree” or “disagree” for each barrier. Before finalizing the questionnaire, we obtained opinions on the questionnaire from 3 experts with experience in hospital pharmacies and conducted a pretest. The reliability of the questionnaire was acceptable (Cronbach alpha, 0.79). The subscale Cronbach alpha was 0.71 for the reporting system, and 0.82 for fear.
2.4. Statistical analysis
We used descriptive statistics to analyze demographic factors and experiences of near-misses, and logistic regression analysis to determine the barriers to reporting medication errors. In the logistic regression, we dichotomized the dependent variable into a high reporting rate group and a low reporting rate group. Participants who reported all near-misses for all 3 stages (prescribing, dispensing, and administration) were defined as the high reporting rate group (n = 42), while participants who did not report all near-misses were defined as the low reporting rate group (n = 52). In the logistic regression, the low reporting rate group was considered to correspond to the event occurrence. We used age, gender, and the 15 underreporting reasons as independent variables to test the barriers. We used backward elimination with a stay level of 0.20. To test the model's goodness of fit, the Hosmer–Lemeshow test was performed. P values < .05 were considered statistically significant. Statistical analyses were performed in STATA version 12 (StataCorp LP, College Station, TX).
3. Ethical approval
Ethical approval for this study was obtained from the Institutional Review Board designated by the Ministry of Health and Welfare. The approval number was P01-201406-SB-04-01.
4. Results
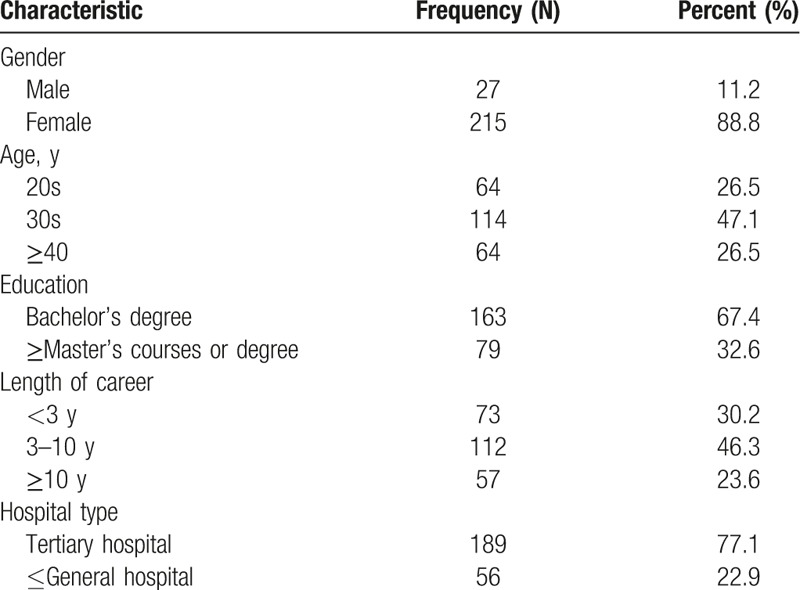
Of the 742 pharmacists surveyed in 32 hospital pharmacies, 245 participated in the survey for a response rate of 33%. In particular, 77.1% of respondents were pharmacists working in tertiary hospitals. Approximately 47% of the respondents were in their 30s and had been pharmacists for 3 to 10 years (Table 1).
Table 1.
Characteristics of survey respondents.
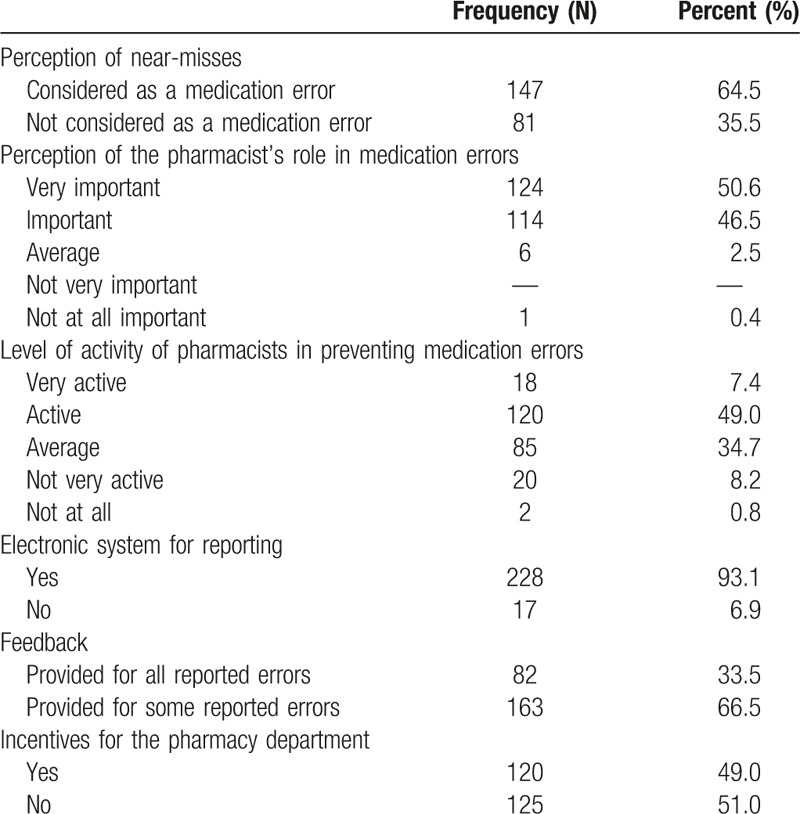
Of the pharmacists, 35.5% stated that near-misses were not medication errors. Approximately 51% of pharmacists thought that the role of pharmacists in medication errors was very important, but only 7.4% answered that pharmacists actively worked to prevent medication errors. Ninety-three percent of the pharmacists worked at hospitals that had an electronic system for reporting medication errors. Only 33.5% of respondents were provided with feedback about medication errors they reported. Forty-nine percent of respondents reported that they had incentive programs for reporting medication errors to the pharmacy department (Table 2).
Table 2.
Pharmacists’ perceptions of medication errors and the pharmacy system.
Most near-misses in dispensing and administration occurred no more than once per month, while near-misses in prescribing occurred 2 to 4 times per month. Five or more near-misses per month were experienced by 14.8%, 4.3%, and 43.9% of respondents for dispensing, administration, and prescribing errors, respectively. All near-misses were reported by 43.7%, 57.4%, and 37.1% of respondents for dispensing, administration, and prescribing errors, respectively. The reporting rate of prescribing errors was lower than that of dispensing and administration errors (Table 3).
Table 3.
Experience of near-misses and reporting rate.
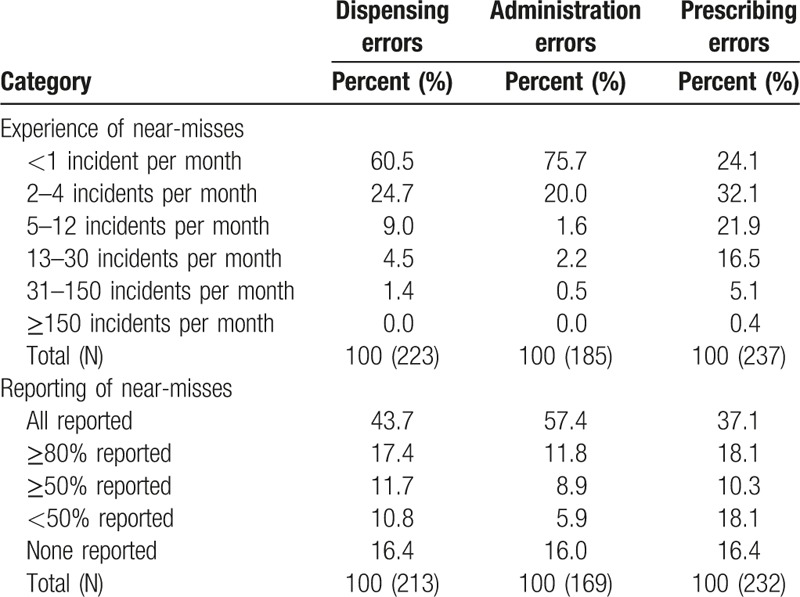
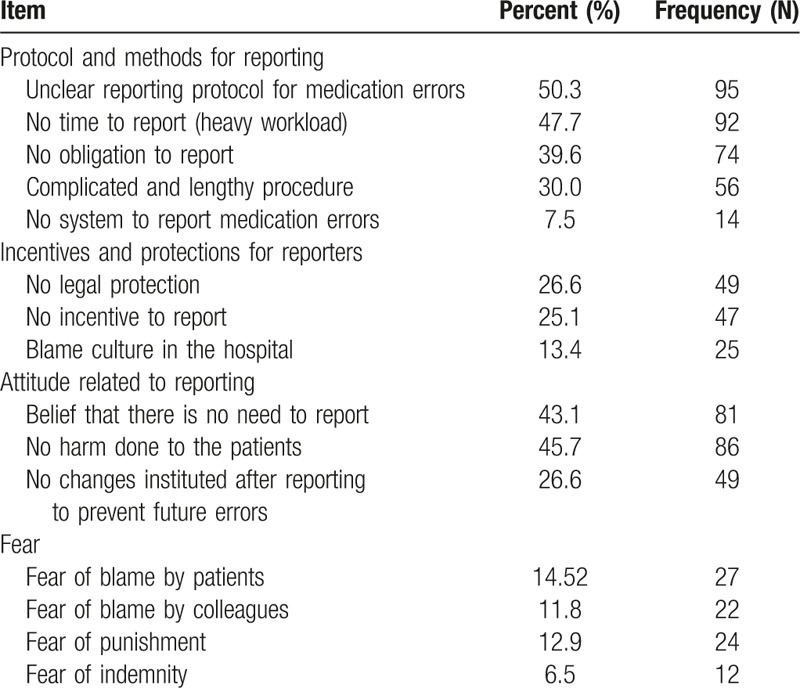
Table 4 presents the extent to which respondents agreed with 15 reasons for underreporting medication errors. The reasons cited most often were an unclear reporting protocol (50.3%), not having time to report (heavy workload) (47.7%), and the absence of harm done to the patients (45.7%). Other commonly cited reasons were the pharmacists’ belief that they did not need to report the error (43.1%), the absence of an obligation to report (39.6%), and a complicated, lengthy reporting procedure (30%).
Table 4.
Reasons for underreporting medication errors.
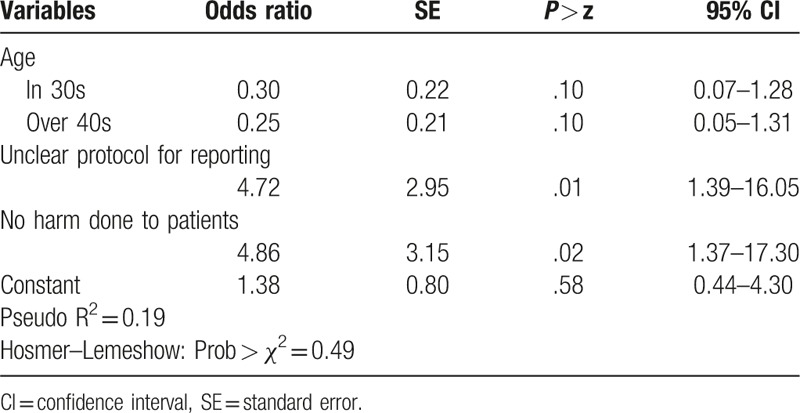
Logistic regression revealed 3 variables (Table 5), including an unclear protocol for reporting medication errors, no harm being done to the patients, and age. The Hosmer–Lemeshow test showed that the logistic regression model had a good fit (P = .49). An unclear protocol for reporting medication errors and the belief that no harm was done to the patients were significant factors contributing to the underreporting of medication errors by pharmacists (P < .05).
Table 5.
Logistic regression model of factors contributing to the underreporting of medication errors, including near-misses.
5. Discussion
Pharmacists experienced near-misses in prescribing more often than in dispensing or administration, but the reporting rate was lower. Approximately 35% of the respondents stated that they reported fewer than 50% of near-misses in prescribing. Lefrak[22] argued that the nonreporting of near-misses deprives health professionals of a learning opportunity, and leads to future harm. Therefore, the reporting rate still needs to be improved.
The 4 top-ranked reasons we found for the failure to report medication errors were an unclear reporting protocol, not having time to report, the absence of harm done to the patients, and the belief that there was no need to report. Logistic regression revealed that an unclear reporting protocol and the effects on patients were key factors in whether medication errors were reported. A standardized, unambiguous protocol for reporting medication errors would simplify the process and increase reporting rates. This is consistent with other studies. In a pediatric hospital, the most common reason for underreporting medication errors was uncertainty about what constituted a medical error.[23] Jung et al[6] also showed the top-ranked barrier to reporting administration errors was absence of harm done to the patients, and the main factor to increase reporting rate was a systematic reporting protocol. Intensive care unit (ICU) nurses in Canada justified not reporting medication errors if no harm came to the patient,[24] and another study found that reporting rates increased with the severity of patient harm.[25]
The commonly cited reasons, such as an unclear reporting protocol, the absence of harm done to patients, and not having time to report are similar to those that have been reported in other studies. A high burden of effort to report (specifically a lack of time to report), a lack of clarity about what to report, as well as uncertainty about who should report errors have all been cited as barriers. Moreover, the severity of the error influenced whether it was reported.[26]
Interestingly, we found a gap between pharmacists’ perceptions of medication errors and their activities to prevent them. Pharmacists thought that medication errors were a critical issue and that they should play a role in preventing medication errors. However, they reported a lack of active participation in this process. The most frequently stated barrier to reporting among doctors and nurses was found to be a lack of feedback. Doctors also argued that some incidents were too trivial, while half of the nurses surveyed stated that there was no point in reporting near-misses.[27] In the present study of hospital pharmacists, only 33.5% of pharmacists reported receiving feedback about errors they had reported, despite the fact that most participating hospitals had an electronic reporting system for tracking medication errors. This reveals a disinclination among hospitals to take steps to reduce medication errors. A qualitative study in a UK ICU found that all interviewees felt that more feedback on medication errors would be helpful.[28] This sentiment was shared by Lefrak[22] and by the physicians and nurses surveyed by Taylor et al.[23] The goal of feedback is not to point out who was at fault, but to provide a chance to share experiences to prevent medication errors from reoccurring.
In this study, 14.5% of pharmacists cited a fear of being blamed by patients as a reason not to report medication errors, 13.4% blamed the culture in the hospital, and 6.5% feared adverse consequences related to the potential indemnity. Multiple studies have shown fear and a culture of blame to be important barriers to reporting medication errors. Fear of blame was the second-ranked barrier among nurses.[6] In a study of the attitudes of physicians toward adverse incident reporting, a culture of blame was found to be a major factor in reluctance to report adverse incidents.[29] In 2 separate studies of nurses’ perception of medication errors, fear and a fear of blame were reported as major barriers for reporting medication administration errors.[30,31] In support of this, a culture of safety was stated as important for increasing reporting rates.[32] In our study, fear of blame ranked much lower than procedural considerations in barriers to reporting medication errors. These findings could assist hospitals in refining their policies and procedures regarding the handling of medication errors.
The strength of this study is that it is the first trial for all members of the KHSP, and showed perceptions of hospital pharmacists for medication errors in South Korea. Unclear reporting protocols and the absence of harm done to patients were perceived as the major factors to underreport medication errors for hospital pharmacists. Hospitals should clarify which incidents staff should report, and work to ensure compliance with these policies. Through systematic approaches, we can improve the reporting process and follow-up actions taken to ensure patient safety.
6. Limitations
A few limitations of this study should be noted. The response rate varied by hospitals. The majority of the participants in this survey were pharmacists working in tertiary hospitals. Therefore, this study could be interpreted as presenting the perception of pharmacists working in large hospitals. It is difficult to generalize for all hospitals. In addition, pharmacists could only report medication errors if they were aware of them. Another limitation was recall bias, since we asked participants to estimate the frequency of medication errors over a period of 3 months. Recall bias could attenuate the frequency of medication errors since 36% of respondents thought near-misses were not included as medication errors based on the survey results. Pharmacists could also be reluctant to remember medication errors because they could be blamed for the errors. Therefore, they might have a tendency to ignore near-misses. However, since we reported the frequencies of medication errors as a wide interval range, its impact might not be large enough to affect the results.
7. Conclusion
In each step of the medication use process (dispensing, administration, and prescribing), near-misses occurred and were reported to various extents. This shows that efforts to increase the reporting rate are still needed. Pharmacists are likely to need systemic support, such as a clear protocol, adequate time for reporting, and education to improve their understanding of near-misses. Reporting near-misses is a way to learn to prevent medication errors. Therefore, hospitals should clarify to their staff what should be reported, and prepare a standard reporting process to increase reporting rates. Doing so would facilitate the development of safety culture in hospitals.
Acknowledgments
The authors thank the KHSP for their efforts in administering and collecting the survey.
Footnotes
Abbreviations: ICU = intensive care unit, IOM = Institute of Medicine, ISMP = Institute for Safe Medication Practices, KHSP = Korean Society of Health-System Pharmacists, MAE = medication administration error, NCC MERP = National Coordinating Council for Medication Error Reporting and Prevention.
This study was funded by the Ministry of Health and Welfare (Korea, Project Name: A study on the improvement of drug safety for pharmaceutical care disparities in Korea). The study funder had no role in the study design or in the collection, analysis, and interpretation of data.
The authors have no conflicts of interest to disclose.
References
- [1].Kohn LT, Corrigan JM, Donaldson MS, Editors; Committee on Quality of Health Care in America, Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington (D.C.): National Academy of Press; 2000.Available at: http://www.nap.edu/catalog/9728.html (accessed February 7, 2016). [Google Scholar]
- [2].Committee on Identifying and Preventing Medication Errors, Aspden P, Wolcott J, Lyle Bootman J, et al, Editors Institute of Medicine. Preventing medication errors: Quality Chasm Series National Academies Press; 2006 Available at: http://www.nap.edu/catalog/11623.html (accessed February 7, 2016). [Google Scholar]
- [3].Council of Europe. Expert Group on Safe Medication Practices. Creation of a better medication safety culture in Europe: Building up safe medication practices. 2006. [Google Scholar]
- [4].Alsulami Z, Conroy S, Choonara I. Medication errors in the Middle East countries: a systematic review of the literature. Eur J Clin Pharmacol 2013;69:995–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kim KS, Kwon SH, Kim JA, et al. Nurses’ perceptions of medication errors and their contributing factors in South Korea. J Nurs Manag 2011;19:346–53. [DOI] [PubMed] [Google Scholar]
- [6].Jung SY, Kim YH, Kang IS, et al. The perception of nurses and physicians regarding medication errors and reporting. Global Health Nursing 2013;3:54–63. [Google Scholar]
- [7].National Coordinating Council for Medication Error Reporting and Prevention. Medication Error Index Available at: http://www.nccmerp.org/sites/default/files/indexBW2001-06-12.pdf (accessed February 10, 2016). [Google Scholar]
- [8].Institute for Safe Medication Practices. Definition of a close call (near miss). Available at: https://www.ismp.org/newsletters/acutecare/articles/20090924.asp (accessed January 3, 2016). [Google Scholar]
- [9].Patanwala AE, Warholak TL, Sanders AB, et al. A prospective observational study of medication errors in a tertiary care emergency department. Ann Emerg Med 2010;55:522–6. [DOI] [PubMed] [Google Scholar]
- [10].Ashcroft DM, Quinlan P, Blenkinsopp A. Prospective study of the incidence, nature and causes of dispensing errors in community pharmacies. Pharmacoepidemiol Drug Saf 2005;14:327–32. [DOI] [PubMed] [Google Scholar]
- [11].de Las Mercedes Martinez Sanchez A. Medication errors in a Spanish community pharmacy: nature, frequency and potential causes. Int J Clin Pharm 2013;35:185–9. [DOI] [PubMed] [Google Scholar]
- [12].NHS Confed|NPSA briefing: Five actions to improve patient safety reporting. Available at: http://www.nrls.npsa.nhs.uk/resources/?entryid45=59903 (accessed January 3, 2016). [Google Scholar]
- [13].Wakefield DS, Wakefield BJ, Borders T, et al. Understanding and comparing differences in reported medication administration error rates. Am J Med Qual 1999;14:73–80. [DOI] [PubMed] [Google Scholar]
- [14].Chiang HY, Lin SY, Hsu SC, et al. Factors determining hospital nurses’ failures in reporting medication errors in Taiwan. Nurs Outlook 2010;58:17–25. [DOI] [PubMed] [Google Scholar]
- [15].Raymond CB, Miller SH, Wheaton HR, et al. Reliability and validity of a survey to evaluate attitudes and behaviours of pharmacy staff toward near misses. Healthc Manage Forum 2010;23:32–7. [DOI] [PubMed] [Google Scholar]
- [16].Vrbnjaka D, Denieffeb S, O’Gormanb C, et al. Barriers to reporting medication errors and near misses among nurses: a systematic review. Int J Nurs Stud 2016;63:162–78. [DOI] [PubMed] [Google Scholar]
- [17].Williams SD, Phipps DL, Ashcroft DM. Understanding the attitudes of hospital pharmacists to reporting medication incidents: a qualitative study. Res Social Adm Pharm 2013;9:80–9. [DOI] [PubMed] [Google Scholar]
- [18].National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP). Definition. Available at: http://www.nccmerp.org/about-medication-errors (accessed January 3, 2016). [Google Scholar]
- [19].Wakefield DS, Wakefield BJ, Uden-Holman T, et al. Perceived barriers in reporting medication administration errors. Best Pract Benchmarking Healthc 1996;1:191–7. [PubMed] [Google Scholar]
- [20].Stratton KM, Blegen MA, Pepper G, et al. Reporting of medication errors by pediatric nurses. J Pediatr Nurs 2004;19:385–92. [DOI] [PubMed] [Google Scholar]
- [21].Kim EG, Hwang JH, Kim CY, et al. A study on nurses’ perception and experience of medication error. Seoul J Nursing 1998;12:133–50. [Google Scholar]
- [22].Lefrak L. Moving toward safer practice: reducing medication errors in neonatal care. J Perinat Neonatal Nurs 2002;16:73–84. [DOI] [PubMed] [Google Scholar]
- [23].Taylor JA, Brownstein D, Christakis DA, et al. Use of incident reports by physicians and nurses to document medical errors in pediatric patients. Pediatrics 2004;114:729–35. [DOI] [PubMed] [Google Scholar]
- [24].Espin S, Wickson-Griffiths A, Wilson M, et al. To report or not to report: a descriptive study exploring ICU nurses’ perceptions of error and error reporting. Intensive Crit Care Nurs 2010;26:1–9. [DOI] [PubMed] [Google Scholar]
- [25].Potylycki MJ, Kimmel SR, Ritter M, et al. Nonpunitive medication error reporting: 3-year findings from one hospital's Primum Non Nocere initiative. J Nurs Adm 2006;36:370–6. [DOI] [PubMed] [Google Scholar]
- [26].Elder NC, Graham D, Brandt E, et al. Barriers and motivators for making error reports from family medicine offices: a report from the American Academy of Family Physicians National Research Network (AAFP NRN). J Am Board Fam Med 2007;20:115–23. [DOI] [PubMed] [Google Scholar]
- [27].Evans SM, Berry JG, Smith BJ, et al. Attitudes and barriers to incident reporting: a collaborative hospital study. Qual Saf Health Care 2006;15:39–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Sanghera IS, Franklin BD, Dhillon S. The attitudes and beliefs of healthcare professionals on the causes and reporting of medication errors in a UK Intensive care unit. Anaesthesia 2007;62:53–61. [DOI] [PubMed] [Google Scholar]
- [29].Waring JJ. Beyond blame: cultural barriers to medical incident reporting. Soc Sci Med 2005;60:1927–35. [DOI] [PubMed] [Google Scholar]
- [30].Petrova E. Nurses’ perceptions of medication errors in Malta. Nurs Stand 2010;24:41–8. [DOI] [PubMed] [Google Scholar]
- [31].Yung HP, Yu S, Chu C, et al. Nurse's attitudes and perceived barriers to the reporting of medication administration errors. J Nurs Manag 2016;24:580–8. [DOI] [PubMed] [Google Scholar]
- [32].Hutchinson A, Young TA, Cooper KL, et al. Trends in healthcare incident reporting and relationship to safety and quality data in acute hospitals: results from the National Reporting and Learning System. Qual Saf Health Care 2009;18:5–10. [DOI] [PubMed] [Google Scholar]


