Abstract
Chart reviews have been used to assess the incidence and impact of adverse events, but most of them are not a nationally representative sample. In addition, the definition of adverse events is generally broad and covers unintended events; the relationship to outcome is often unclear, and official estimates have not matched those of medical practitioner's recognition. The number of patient deaths from adverse events remains unknown.
This study aimed to investigate the number of adverse event related patient deaths and mortality rate as recognized by medical practitioners in Japan, and to reveal the applicability of our method for estimating the number of adverse event related patient death as an alternative to a chart review.
In 2015, a mail survey of 3270 hospitals asked how many patient deaths had been caused by adverse events at the hospital in the last 3 years. The hospitals were selected by stratified random sampling according to the number of beds. The number of patient deaths caused by adverse events and the mortality rate were estimated, with adjustments for the hospital type and the number of beds.
The mail survey response rate was 22.4% (731/3270). The number of patient deaths caused by adverse events in a year was estimated to be between 1326 and 1433. The mortality rate was estimated at 8.81 to 9.52 cases per 100,000 discharged patients, and 2.65 to 2.87 cases per 1,000,000 person-days. The mortality rate was high at acute care hospitals with ≥500 beds and at psychiatric hospitals.
The nationwide number of patient deaths recognized by medical practitioners as caused by adverse events and its mortality rate were estimated. In comparison with a chart review, a mail survey was a faster and a cheaper way, and was able to cover a wide range of hospitals for estimating mortality rate of adverse events.
Keywords: adverse event, mortality rate, patient safety
1. Introduction
A report by the Institute of Medicine, “To Err Is Human,” estimated the number of patient deaths associated with adverse events in the United States to be 44,000 to 98,000 per year.[1,2] This estimate was based on chart reviews done in dozens of acute care hospitals. In Japan, a study based on a chart review reported that the mortality rate associated with adverse events was 0.2% and that adverse events contributed to 34,000 deaths per year, but this number may not be representative because only acute care hospitals were considered and the sample size was relatively small (4389 patients in 18 hospitals with ≥200 beds).[3] In developed countries, chart review studies have estimated adverse event related mortality rates to be at 0.5% to 1.6%.[4–7] Chart reviews have been used to detect adverse events, but they might be difficult to use widely because they require time and effort. Most of the chart review studies were based on patient records in fewer than 50 hospitals and excluded specialty hospitals such as psychiatric or pediatric hospitals. [2,4–7] Samples from those studies might not be representative of the population. In addition, the definition of adverse events used in chart review studies might be different from that recognized by medical practitioners. In chart reviews, a broad range of events, including unintended events such as side effects of certain medications and pseudomembranous colitis with broad-band antibiotics administration, were classified as adverse events. [3,8] Some of them are regarded by medical practitioners as unavoidable events that occur with certain probability. Thus, the number of deaths and mortality rate due to adverse events remain unclear. In this study, we conducted a nationwide questionnaire survey to investigate the number of adverse event related patient deaths and mortality rate as recognized by medical practitioners, and to reveal the applicability of our method for estimating the number of adverse event related patient death as an alternative to a chart review.
2. Methods
A cross-sectional study using a mail survey of hospitals in Japan was conducted in 2015. The hospitals were selected by stratified random sampling according to number of beds; 25% of hospitals with <100 beds, 50% of hospitals with 100 to 299 beds, and 100% hospitals with ≥300 beds were selected. As a result, the mail survey was sent to 3270 hospitals, representing 38% (3270/8595) of all hospitals in Japan. It was hoped that a nationwide survey would be able to correct the sampling bias that naturally occurs in chart review, resulting in more accurate data. Respondents were patient safety managers, directors of nursing, or chief executive officers at the hospitals. Questionnaires were completed and recovered anonymously. The questionnaire included questions about the number of beds, the number of health care workers, the number of discharged patients, the patient safety management system at each hospital, and the number of patient deaths caused by adverse events in the past 3 years preceding receipt of the survey. The questionnaire asked how many patient deaths had been caused by adverse events at the hospital in the last 3 years.
In Japan, there are 5 types of beds, as defined by the Medical Care Act. Acute care beds account for 57%, psychiatric beds account for 22%, long-term care beds account for 21%, and other types of beds account for less than 1% of all hospital beds. A hospital can have more than one type of hospital bed. In this study, hospitals were classified by the bed type that was most commonly used; they were classified as acute care hospitals, psychiatric hospitals, and long-term care hospitals. Most of the specialty hospitals, such as pediatric hospitals or cardiovascular hospitals, were classified as acute care hospitals because most of the beds at these hospitals were acute care beds. Depending on their proportion of acute care beds or long-term care beds, rehabilitative hospitals were classified as acute care hospitals or long-term care hospitals.
The number of patient deaths caused by adverse events in Japan was estimated in 3 ways:
1) By number of beds
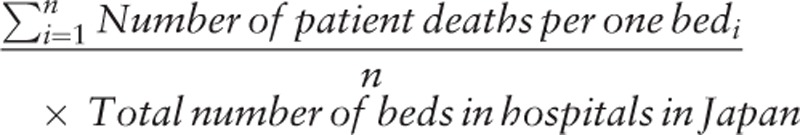 |
2) By number of health care workers
 |
3) By number of discharged patients
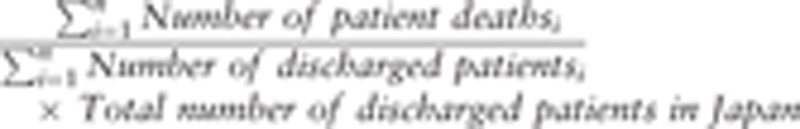 |
n = number of respondents
According to government statistics, in 2014, the average length of stay in an acute care bed was 16.8 days, but the average stay in psychiatric beds and long-term care beds were generally long (281.2 and 164.6 days, respectively), and thus, the number of discharged patients at those hospitals was relatively small. As a result, many outliers of the number of patient deaths per one discharged patient were observed among psychiatric hospitals and long-term care hospitals. Therefore, the estimation method based on the number of discharged patients was modified to absorb the outliers.
The estimate was adjusted by hospital type and number of beds. In this study, the mortality rate was defined as the number of patient deaths per 100,000 discharged patients. The nationwide mortality rate was calculated by dividing the number of patient deaths due to adverse events by 15,055,200 persons, which was the number of discharged patients in 2014. The average length of stay at hospitals in Japan was 33.2 days, which includes not only acute care hospitals but also long-term care and psychiatric hospitals. Inpatients spent 499,832,640 person-days in hospitals in 2014, and the number of patient deaths per 1 million person-days was also calculated.
Missing data were excluded from the analysis. An analysis of variance and the Tukey test was performed to compare the average number of patient deaths. Statistical analyses were performed using SPSS 22.0 (IBM, Armonk, NY). The ethics committee of the Toho University School of Medicine approved the study (27045).
3. Results
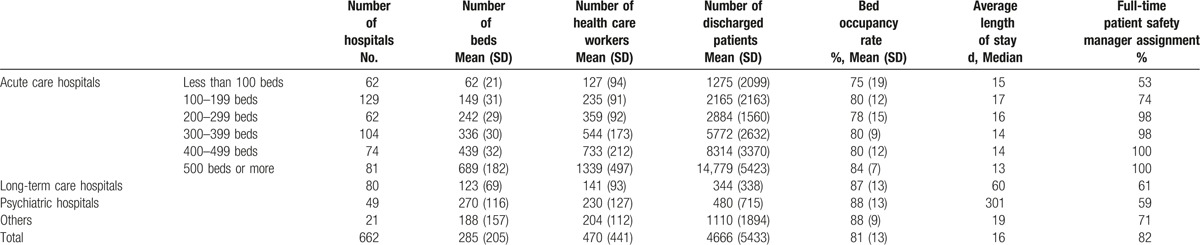
The mail survey response rate was 22.4% (731/3270). Among the respondents, 69 hospitals did not answer the number of patient deaths caused by adverse events, and those data were excluded from the analysis. The valid response represented 8% (662/8595) of all hospitals in Japan. The characteristics of respondent hospitals are summarized in Table 1.
Table 1.
Characteristics of respondent hospitals.
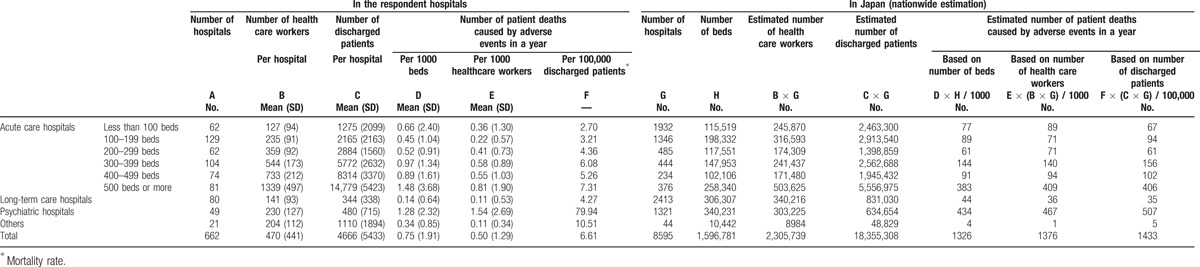
The number of patient deaths caused by adverse events was estimated to be 1326 to 1433 per year (Table 2). According to the estimate based on the number of beds, 64% of patient deaths occurred in acute care hospitals, 3% in long-term care hospitals, and 33% in psychiatric hospitals. The estimated mortality rate was 8.81 to 9.52 cases per 100,000 discharged patients, and 2.65 to 2.87 cases per 1,000,000 person-days. The mortality rate was high in acute care hospitals with ≥500 beds and in psychiatric hospitals.
Table 2.
Estimated number of patient deaths.
The number of patient deaths at acute care hospitals with ≥500 beds was higher than that at acute care hospitals with 100 to 199 beds and at long-term care hospitals (Fig. 1A, B). The number of patient deaths per 1000 health care workers at psychiatric hospitals was significantly higher than those at other types of hospitals (Fig. 1B).
Figure 1.
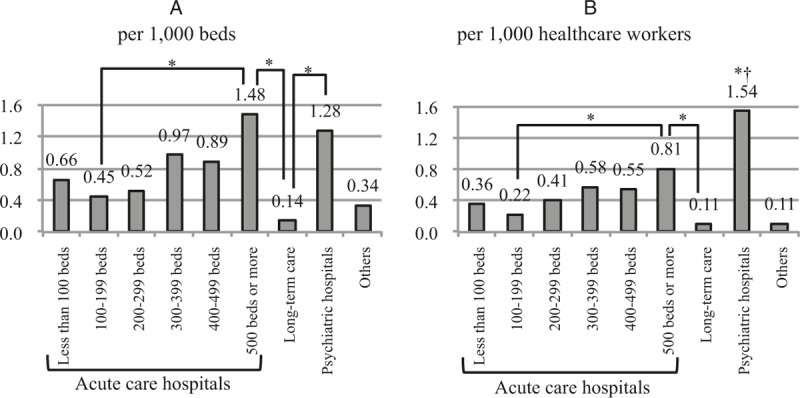
Number of patient deaths. ∗P < .05. †The number of patient deaths at psychiatric hospitals was significantly higher than those at other types of hospitals.
4. Discussion
The number of patient deaths recognized by practitioners to have been caused by adverse events in a year was estimated to be between 1326 and 1433. The mortality rate was estimated to be 8.81 to 9.52 cases per 100,000 discharged patients and 2.65 to 2.87 cases per 1,000,000 person-days.
The difference between the estimate based on chart review and the estimate in this study might reflect a difference in types of hospitals or in the power to detect adverse events. This study cannot exclude the possibility of underestimation because our study was based on data recognized by practitioners. In addition, the number of patient deaths caused by adverse events could vary with the definition of “adverse event” and with the strength of causation between adverse events and outcome. The chart review study in Japan reported that the number of patient deaths was estimated at 34,000 per year. If a more strict criteria for causation used in other studies were applied, the number of deaths decreased from 34,000 to 27,000. [3,4] In the same way, if only cases associated with definitively inappropriate medical care or patient management, which occupied 10% of patient deaths due to adverse events, were selected, the number of deaths decreased from 34,000 to 3400, and the mortality rate decreased from 227.84 to 22.78 cases per 100,000 discharged patients. [3] These numbers are similar to the results of our study, and the respondent hospitals in our study might only report the number of patient deaths caused by definitively inappropriate medical care or patient management.
The number of patient deaths caused by adverse events may vary with the target population, the inclusion or exclusion criteria of adverse events, screening method, or adjustment method.[8] In Japan, Horiguchi[9] conducted a mail survey of 4111 hospitals asking how many patient deaths were caused by inappropriate medical care or management, or patient deaths that might be caused by them, and estimated the number of patient deaths to be between 1460 and 1993 per year, but it was not adjusted by hospital type and number of beds. In Japan, national hospitals and university teaching hospitals (273 hospitals in all) are required by law to report patient deaths caused by inappropriate medical care or management. According to the reported data, the number of patient deaths was estimated at 1288 to 2071 per year, but it was also not adjusted by hospital type and number of beds.[10] In 2014, the Japan Hospital Association conducted a mail survey of 2399 member hospitals to ask the number of patient deaths identified by each hospital, and estimated the number of patient deaths as 1225 per year.[11] The estimate was adjusted by the number of beds but not by the hospital type.
The high mortality rate in acute care hospitals with ≥500 beds might reflect something inherent in large acute care hospitals because such hospitals cover high-risk patients. Other studies also identified that the incidence of adverse events at large hospitals was higher than that at small hospitals.[4,7]
The reason for the high mortality rate at psychiatric hospitals is unclear, but it might be associated with suicide in hospitals.[12,13] Past studies also identified excess mortality according to cardiovascular diseases in patients with schizophrenia, bipolar disorder, and depression.[14] Psychiatric patients might be less likely to be monitored and treated for cardiovascular diseases in psychiatric hospitals, or side effects of psychiatric drugs might be associated with mortality rates at these hospitals.[15–17] Further study is needed to identify the reason for the high mortality rate at psychiatric hospitals.
In this study, the relationship between patient deaths and adverse events was judged by each respondent hospital, and consequently, the number of patient deaths caused by adverse events may be influenced by the patient safety management system of hospitals.[18] For example, big acute care hospitals with more resources could detect unexpected patient deaths and clarify the cause of death, and there would be an underestimation in smaller hospitals with fewer resources. There could be some limitations regarding the representativeness of respondents in this study because the valid response represented only 8% (662/8595) of all hospitals in Japan.
To clarify the mortality rate of adverse events in hospitals by hospital type and size, other methods, such as chart reviews, global trigger tools, and prospective surveys, should be considered in addition to the present study.
5. Conclusion
According to a nation-wide mail survey, the annual number of patient deaths recognized by medical practitioners as caused by adverse events was estimated at 1326 to 1433 in Japan. The mortality rate was estimated at 8.81 to 9.52 cases per 100,000 discharged patients, and at 2.65 to 2.87 cases per 1,000,000 person-days. It was high at large acute care hospitals (with ≥500 beds) and at psychiatric hospitals. In comparison with a chart review, a mail survey was a faster and a cheaper way, and was able to cover a wide range of hospitals for estimating mortality rate of adverse events.
Footnotes
Authorship: All authors contributed to the study design. SF drafted the paper. All authors contributed to the interpretation of the results and approved the final version of the manuscript.
Funding/support: SF, SI, YN, YS, and TH have received a Health Labour Sciences Research Grant from the Ministry of Health Labour and Welfare in Japan. For the remaining authors, none were declared.
The authors report no conflicts of interest.
References
- [1].Institute of Medicine. To Err is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. pp. 26–27. [Google Scholar]
- [2].Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med 1991;324:370–6. [DOI] [PubMed] [Google Scholar]
- [3].Sakai H. A Study for Nationwide Incidence of Adverse Events [Ministry of Health, Labour and Welfare web site]. December 22, 2011. Available at: http://www.mhlw.go.jp/stf/shingi/2r9852000001z7ad-att/2r9852000001z7gi.pdf [Japanese]. Accessed July 17, 2017. [Google Scholar]
- [4].Baker GR, Norton PG, Flintoft V, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. CMAJ 2004;170:1678–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Soop M, Fryksmark U, Koster M, et al. The incidence of adverse events in Swedish hospitals: a retrospective medical record review study. Int J Qual Health Care 2009;21:285–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: preliminary retrospective record review. BMJ 2001;322:517–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Rafter N, Hickey A, Conroy RM, et al. The Irish National Adverse Events Study (INAES): the frequency and nature of adverse events in Irish hospitals: a retrospective record review study. BMJ Qual Saf 2017;26:111–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Vassar M, Holzmann M. The retrospective chart review: important methodological considerations. J Educ Eval Health Prof 2013;10:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Horiguchi H. A Study for Nationwide Incidence of Adverse Events [Ministry of Health, Labour and Welfare web site]. December 22, 2011. Available at: http://www.mhlw.go.jp/stf/shingi/2r9852000001z7ad-att/2r9852000001z7jc.pdf [Japanese]. Accessed July 17, 2017. [Google Scholar]
- [10].Ministry of Health, Labour and Welfare. Tentative Calculation for Incidence Rate of Patient Deaths Associated With Medical Services, [Ministry of Health, Labour and Welfare web site]. May 2, 2013. Available at: http://www.mhlw.go.jp/stf/shingi/2r985200000333dq-att/2r985200000333m8.pdf [Japanese]. Accessed July 17, 2017. [Google Scholar]
- [11].Japan Hospital Association. Investigation into the Actual Condition of Patient Safety in 2014 [Japan Hospital Association web site]. March 3, 2015. Available at: https://www.hospital.or.jp/pdf/06_20150306_01.pdf [Japanese]. Accessed July 17, 2017. [Google Scholar]
- [12].Hunt IM, Kapur N, Webb R, et al. Suicide in current psychiatric in-patients: a case-control study The National Confidential Inquiry into Suicide and Homicide. Psychol Med 2007;37:831–7. [DOI] [PubMed] [Google Scholar]
- [13].Bose S, Khanra S, Umesh S, et al. Inpatient suicide in a psychiatric hospital: fourteen years’ observation. Asian J Psychiatr 2016;19:56–8. [DOI] [PubMed] [Google Scholar]
- [14].De Hert M, Dekker JM, Wood D, et al. Cardiovascular disease and diabetes in people with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC). Eur Psychiatry 2009;24:412–24. [DOI] [PubMed] [Google Scholar]
- [15].Kilbourne AM, Post EP, Bauer MS, et al. Therapeutic drug and cardiovascular disease risk monitoring in patients with bipolar disorder. J Affect Disord 2007;102:145–51. [DOI] [PubMed] [Google Scholar]
- [16].Kreyenbuhl J, Dickerson FB, Medoff DR, et al. Extent and management of cardiovascular risk factors in patients with type 2 diabetes and serious mental illness. J Nerv Ment Dis 2006;194:404–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lally J, MacCabe JH. Antipsychotic medication in schizophrenia: a review. Br Med Bull 2015;114:169–79. [DOI] [PubMed] [Google Scholar]
- [18].Fujita S, Iida S, Hasegawa T. An Estimation of the Number of Patient Deaths Caused by Adverse Events in Hospitals in Japan. 33rd ISQUA International Scientific Meeting. Available at: http://www.epostersonline.com/isqua2016/node/321. Accessed August 23, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]


