Abstract
Background:
This meta-analysis compared clinical and radiographic outcomes and complications of kinematic alignment (KA) and mechanical alignment (MA) techniques in primary total knee arthroplasty (TKA).
Methods:
All studies comparing the operation time, change in hemoglobin, length of hospital stay, postoperative complications, and clinical and radiographic outcomes as assessed with various measurement tools, from direct interview to imaging methods, in patients who underwent primary TKA through the KA or MA technique were included.
Results:
Six studies were included in the meta-analysis. The proportion of patients who developed postoperative complications (OR: 1.10, 95% CI: 0.49–2.46; P = .69) did not differ significantly between the KA and MA techniques. The 2 groups were also similar in terms of change in hemoglobin (95% CI: −0.38 to 0.34; P = .91), length of hospital stay (95% CI: −0.04 to 0.55; P = .10), hip-knee-ankle angle (95% CI: −1.76 to 0.75; P = .43), joint line orientation angle (95% CI: −4.27 to 4.23; P = .99), tibial component slope (95% CI: −0.53 to 3.56; P = .15), and femoral component flexion (95% CI: −2.61 to 7.57; P = .34). In contrast, operation time (95% CI: −27.16 to −3.71; P = .01), overall functional outcome (95% CI: 6.59–11.51; P < .0001), knee anatomical axis (95% CI: −1.38 to −0.01; P = .05), femoral component relative to the mechanical axis (95% CI: −2.47 to −1.40; P < .0001), and tibial component relative to the mechanical axis (95% CI: 1.56–2.95; P < .0001) were significantly different between the 2 groups.
Conclusions:
There were no significant differences in postoperative complications, change in hemoglobin, length of hospital stay, hip-knee-ankle angle, joint line orientation angle, tibial component slope, or femoral component flexion between the KA and MA techniques for primary TKA. However, the KA technique resulted in a significantly shorter operation time and better overall functional outcome than the MA technique, even though the femoral component was placed in a slightly more valgus position relative to the mechanical axis and the tibial component in a slightly more varus position with the KA technique.
Keywords: kinematic alignment, mechanical alignment, meta-analysis, total knee arthroplasty
1. Introduction
Proper alignment of the knee is one of the most important factors in determining long-term implant survival after total knee arthroplasty (TKA).[1,2] The standard surgical techniques for TKA use 2 different alignment methods for prosthesis implantation: mechanical alignment (MA) and kinematic alignment (KA). The MA technique aims to create a neutral lower limb axis by cutting the distal femur and proximal tibia perpendicular to the femoral and tibial mechanical axes and provides reliable long-term fixation and functional improvement.[3] In addition, navigation-assisted TKA has been shown to better replicate the neutral MA of the knee, leading to fewer alignment outliers.[4,5] However, the MA technique with or without navigation can lead to unfavorable results, including abnormal tightening or slackening of the collateral, posterior cruciate, and retinacular ligaments and abnormal contact kinematics caused by changing the angle and level of the natural joint line, leading to unsatisfactory outcomes in up to 25% of patients.[6–8] Thus, the KA technique has increased in popularity. This technique aims to restore the 3 functional axes that determine normal knee kinematics based on an understanding of predictable patterns of cartilage wear and lack of bone wear in arthritic knees. The KA technique is associated with improved postoperative satisfaction and function.[6,9,10] However, there are also potential concerns with the KA technique: restoring natural varus can increase the risk of early implant failure and poor function because the tibial component is aligned with the natural, pre-arthritic joint lines of the knee and not perpendicular to the mechanical axis of the tibia.[9] Although many studies have reported the clinical and radiographic outcomes of patients who underwent primary TKA with 1 of the 2 techniques, few comparative studies exist, and no systematic reviews or meta-analyses have been published. Therefore, this meta-analysis compared the clinical and radiographic outcomes and complications between the KA and MA techniques in primary TKA. It was hypothesized that there would be no difference in clinical or radiographic outcomes and complications between the 2 surgical techniques for primary TKA.
2. Materials and methods
2.1. Data and literature sources
This study followed the Cochrane Review Methods and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses reporting guidelines for the meta-analysis of intervention trials. Although the present study involved human participants, ethical approval or informed consent from the participants was not required because all the data were based on previously published studies and analyzed anonymously without any potential harm to the participants. Multiple comprehensive databases, including MEDLINE (January 1, 1966 to June 30, 2016), Embase (January 1, 1947 to June 30, 2016), Web of Science (January 1, 1960 to June 30, 2016), SCOPUS (January 1, 1960 to June 30, 2016), and the Cochrane Library (January 1, 1966 to June 30, 2016) were searched for studies that compared the operation time, change in hemoglobin, length of hospital stay, postoperative complications, and overall functional and radiographic outcomes after surgery in primary TKA through the KA and MA techniques. There were no restrictions on language. Search terms used in the title, abstract, MeSH, and keywords fields included (“arthroplasty, replacement, knee” [MeSH] AND “arthroplasty” [tiab] OR “replacements” [tiab] OR “knee” [tiab] OR “kinematics” [tiab] OR “kinematical” [tiab] OR “kinematically” [tiab] OR “mechanical” [tiab] OR “mechanically” [tiab] OR “aligned” [tiab] OR “alignment” [tiab]). After the initial electronic search, relevant articles and their bibliographies were searched manually.
2.2. Study selection
From the title and abstract, 2 reviewers independently selected the relevant studies for full review. The full text copy of the article was reviewed if the abstract did not provide enough data to make a decision. Studies were included in the meta-analysis if they assessed operation time, change in hemoglobin, length of hospital stay, postoperative complications, overall functional and radiographic outcomes after surgery in primary TKA; reported direct comparisons of surgical outcomes in primary TKA through the KA and MA techniques; included at least 1 of the following 6 parameters: operation time, change in hemoglobin, length of hospital stay, functional outcomes, including distance walked prior to discharge, Oxford Knee Score (OKS), Western Ontario McMaster Universities Arthritis Index (WOMAC), Knee Society Score (KSS), Knee Society Function Score (KSFS), Combined Knee Society Score (CKSS), and flexion range of motion (ROM), radiographic outcomes, including hip-knee-ankle (HKA) angle, knee anatomical axis (KAA), joint line orientation angle (JLOA), femoral component relative to mechanical axis (FCRTMA), tibial component relative to mechanical axis (TCRTMA), tibial component slope (TCS), and femoral component flexion (FCF), and major or minor complications; fully reported the parameters of operation time, change in hemoglobin, length of hospital stay, overall functional and radiographic outcomes, or postoperative complications, including means, standard deviations, and sample sizes; and used adequate statistical methods to compare these parameters between 2 groups of patients. For the coronal plane, the HKA angle was defined as the angle subtended by a line drawn from the center of the femoral head to the center of the knee and a line drawn from the center of the knee to the center of the talus on a standing AP lower limb radiograph. The KAA was defined as the angle between the anatomic axis of the femur and tibia. The JLOA was defined as the angle formed between the joint line and a line parallel to the floor. The FCRTMA was defined as the angle between the MA of the femur and the transcondylar line of the femoral component. The TCRTMA was defined as the angle between the MA of the tibia and the transcondylar line of the tibial component. For all coronal radiographic parameters, a negative value denotes valgus angulation, whereas a positive value denotes varus angulation. For the sagittal plane, the TCS was defined as the angle between the tibial component and anatomic axis of the tibia. A negative value denotes tibial component flexion, whereas a positive value denotes tibial component extension. The FCF was defined as the angle between the femoral component and the anatomic axis of the femur. A negative value denotes femoral component extension, whereas a positive value denotes FCF. Postoperative complications were classified as major and minor. Major complications included any complication resulting in the need for additional surgical intervention such as removal or revision of the components. Minor complications included any complication that required surgical intervention in which the components were retained.
2.3. Data extraction
Two reviewers independently recorded data from each study using a predefined data extraction form. Disagreement between the reviewers was resolved by consensus or by discussion with a third investigator when consensus could not be reached. Variables recorded included those associated with surgical outcomes, such as operation time, change in hemoglobin, length of hospital stay, postoperative complications, and overall functional and radiographic outcomes. Sample sizes and the means and standard deviations of surgical outcomes in each group were also recorded. If these variables were not mentioned in the articles, the study authors were contacted by email to retrieve further information.
2.4. Assessment of methodological quality
Two reviewers independently assessed the methodological quality of the prospective RCTs using the modified Jadad scale, including randomization, blinding, withdrawals and dropouts, inclusion and exclusion criteria, adverse reactions, and statistical analysis. High-quality studies are reflected by scores of 4 to 8, whereas low-quality studies are indicated by scores of 0 to 3.[11] For the Newcastle-Ottawa Scale,[12] as recommended by the Cochrane Non-Randomized Studies Methods Working Group, we assessed the studies based on 3 criteria: selection of the study groups, comparability of the groups, and ascertainment of either the exposure or the outcome of interest for case-control and cohort studies. Any unresolved disagreements between reviewers were resolved by consensus or by consultation with a third investigator. Publication bias could not be assessed in these trials. Tests for funnel plot asymmetry are typically performed only when at least 10 studies are included in the meta-analysis.[13] As our analysis included only 6 studies, tests for asymmetry were not performed because these tests would not be able to differentiate asymmetry from chance.
2.5. Statistical analysis
The main outcomes of the meta-analysis were the proportion of cases that developed postoperative complications, and the weighted mean difference (WMD) in operation time, change in hemoglobin, length of hospital stay, and overall functional and radiographic outcomes in the 2 groups. For all comparisons, odds ratios (ORs) and 95% confidence intervals (CI) were calculated for binary outcomes, while the WMD and 95% CI were calculated for continuous outcomes. For the OKS measure, we combined comparable scores of postoperative pain as presented on a 48-point scale, where 48 indicated the absence of pain and 0 indicated the worst pain imaginable. For the WOMAC measure, we combined comparable scores of postoperative pain as presented on a 96-point scale, where 96 indicated absence of pain and 0 indicated the worst pain imaginable. For the KSS measures, we combined comparable scores of postoperative pain as presented on a 100-point scale, where 100 indicated absence of pain and 0 indicated the worst pain imaginable. For the KSFS measures, we combined comparable scores from functional outcome tools when these tools scored disability on a 100-point scale; the lower the score, the greater the disability. For the CKSS measure, we combined KSS and KSFS scores as presented on a 200-point scale. Heterogeneity was determined by estimating the proportion of between-study inconsistencies due to actual differences between studies rather than differences due to random error or chance using the I2 statistic, with values of 25%, 50%, and 75% considered low, moderate, and high heterogeneity, respectively. All statistical analyses were performed with RevMan version 5.3 statistical software. Subgroup analysis was performed for postoperative complications only to explore a potential source of heterogeneity. As a result, 2 subgroups were created: major and minor complications.
3. Results
3.1. Identification of studies
The details of study identification, inclusion, and exclusion are summarized in Figure 1. An electronic search yielded 2412 studies in PubMed (MEDLINE), 2333 in Embase, 604 in Web of Science, 3217 in SCOPUS, and 378 in the Cochrane Library. After removing 3568 duplicates, 5380 studies remained; of these, 5366 were excluded based on reading the abstracts and full-text articles, and an additional 8 studies were excluded because they had unusable information or made inappropriate group comparisons. Four additional publications were identified through manual searching. This eventually resulted in 6 studies that were included in the meta-analysis.[14–19]
Figure 1.

PRISMA flow diagram of literature selection. PRISMA = preferred reporting items for systemic reviews and meta-analyses.
3.2. Study characteristics, patient populations, and quality assessment of the included studies
The 6 studies we examined included 371 patients who underwent primary TKA through the KA technique and 372 patients who underwent primary TKA through the MA technique. Five studies (5 RCTs) compared prospectively measured parameters, whereas 1 study compared measured parameters by retrospective chart review. Four studies compared groups according to WOMAC, KSFS, HKA, FCRTMA, and postoperative complications; 3 compared length of hospital stay, OKS, CKSS, flexion ROM, JLOA, TCRTMA, and TCS; and 2 compared operation time, change in hemoglobin, distance walked prior to discharge, KAA, and FCF (Table 1). The quality of the 6 studies included in the meta-analysis is summarized in Table 1. There were 4 RCTs of high quality (modified Jadad scale > 4) and 1 RCT of low quality (modified Jadad scale < 3). The non-RCT (1 RCS) was of low quality (Newcastle-Ottawa Scale > 6).
Table 1.
Characteristics of the studies included in the meta-analysis.

3.3. Operation time, change in hemoglobin, and length of hospital stay
Of the 6 studies, 2 compared the operation time between the KA and MA techniques, which were performed in 90 and 91 patients, respectively. The pooled mean difference in operation time was −15.44 minutes (95% CI: −27.16 to −3.71 minutes; P = .01; I2 = 60%, Fig. 2), indicating that the operation time was significantly shorter with the KA technique than the MA technique. Of the 6 studies, 2 compared the change in hemoglobin between the 2 techniques, involving 85 and 85 patients, respectively. The pooled data showed that the mean change in hemoglobin was −0.02 g/dL (95% CI: −0.38 to 0.34 g/dL; P = .91; I2 = 17%, Fig. 3). Of the 6 studies, 2 compared the length of hospital stay between the 2 techniques, involving 134 and 135 patients, respectively. The pooled data showed that the mean length of hospital stay was 0.25 days (95% CI: −0.04 to 0.55 days; P = .10; I2 = 0%, Fig. 4).
Figure 2.

Results of aggregate analysis for comparison of OT according to different alignment techniques. OT = operation time.
Figure 3.

Results of aggregate analysis for comparison of CHB according to different alignment techniques. CHB = change in hemoglobin.
Figure 4.
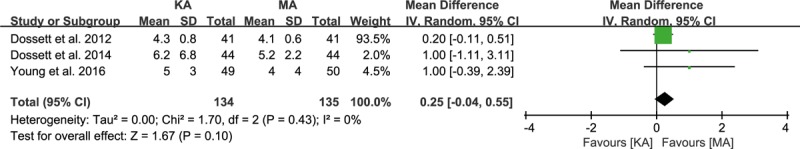
Results of aggregate analysis for comparison of LHS according to different alignment techniques. LHS = length of hospital stay.
3.4. Overall functional outcome
Of the 6 studies, 2 compared the distance walked prior to discharge between the KA and MA techniques, which were performed in 90 and 91 patients, respectively. The pooled mean difference in distance walked prior to discharge was 48.11 ft (95% CI: 11.63–84.58 ft; P = .01; I2 = 0%, Fig. 5). Three studies, including 134 patients who underwent the KA technique and 135 who underwent the MA technique, reported the OKS. The pooled mean difference in OKS score was 4.72 points (95% CI: 0.24–9.21 points; P = .04; I2 = 79%, Fig. 5). Four studies compared WOMAC scores between the 2 techniques, involving 234 patients who underwent the KA technique and 235 who underwent the MA technique. The pooled mean difference in WOMAC score was 10.56 points (95% CI: 4.75–16.38 points; P = .0004; I2 = 71%, Fig. 5). Four studies compared KSS and KSFS scores between the 2 approaches, involving 206 patients who underwent the KA technique and 207 who underwent the MA technique. The pooled mean difference was 9.33 points for the KSS score (95% CI: 3.84–14.82 points; P = .0009; I2 = 65%, Fig. 5) and 9.79 points for the KSFS score (95% CI: 5.68–13.90 points; P < .0001; I2 = 10%, Fig. 5). Three studies compared CKSS scores between the 2 approaches, involving 185 patients who underwent the KA technique and 185 who underwent the MA technique. The pooled mean difference in CKSS score was 17.81 points (95% CI: 8.56–27.07 points; P = .0004; I2 = 54%, Fig. 5). Three studies compared flexion ROM between the 2 approaches, involving 134 patients who underwent the KA technique and 135 who underwent the MA technique. The pooled mean difference in flexion ROM was 5.19° (95% CI: 2.34–8.04 points; P = .0004; I2 = 13%, Fig. 5). All functional outcomes included in current meta-analysis were significantly greater with the KA technique than the MA technique.
Figure 5.
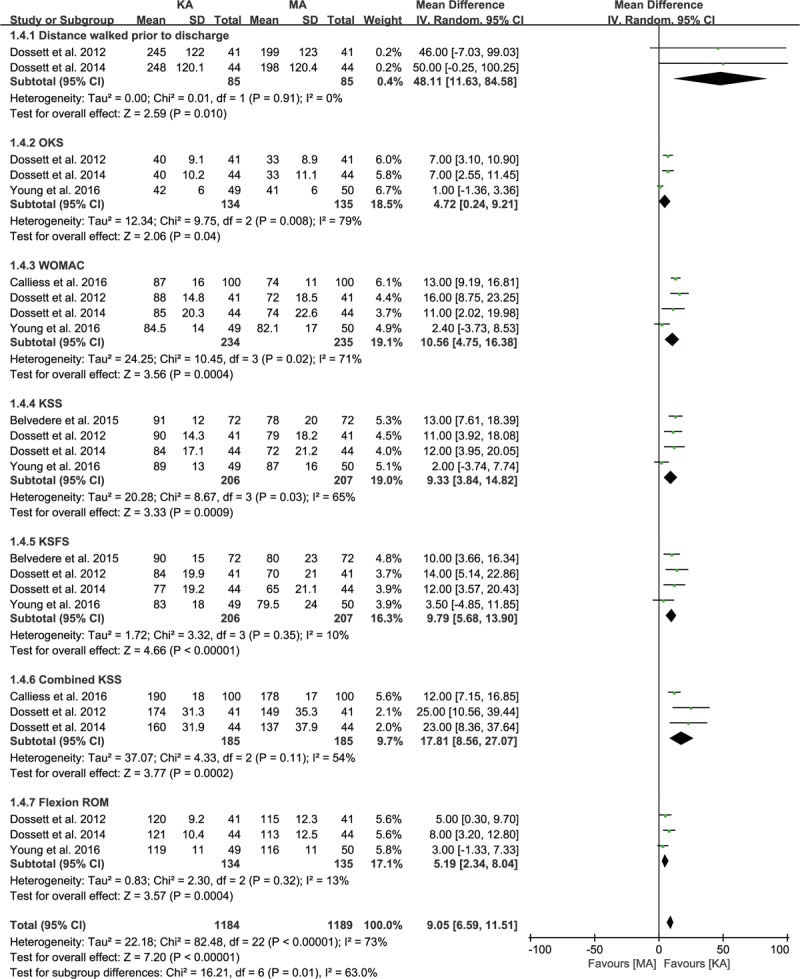
Results of aggregate analysis for comparison of postoperative functional outcomes, including DWPTD, OKS, WOMAC, KSS, KSFS, CKSS, and flexion ROM according to different alignment techniques. CKSS = Combined Knee Society Score, DWPTD = distance walked prior to discharge, KSFS = Knee Society Function Score, KSS = Knee Society Score, flexion ROM = flexion range of motion, OKS = Oxford Knee Score, WOMAC = Western Ontario McMaster Universities Arthritis index.
3.5. Overall radiographic outcome
Of the 6 studies, 4 compared the HKA angle between the KA and MA techniques, which were performed in 234 and 235 patients, respectively. The pooled mean difference in HKA angle was −0.50° (95% CI: −1.76 to 0.75°; P = .43; I2 = 86%, Fig. 6). Two studies compared the KAA between the KA and MA techniques, which were performed in 85 and 85 patients, respectively. The pooled mean difference in KAA was −0.70° (95% CI: −1.38 to −0.01°; P = .05; I2 = 0%, Fig. 6), indicating that the KAA was significantly more valgus with the KA technique than the MA technique. Three studies compared the JLOA between the KA and MA techniques, which were performed in 150 and 150 patients, respectively. The pooled mean difference in JLOA was −0.02° (95% CI: −4.27 to 4.23°; P = .99; I2 = 99%, Fig. 6). Four studies compared the FCRTMA between the KA and MA techniques, performed in 234 and 235 patients, respectively. The pooled mean difference in FCRTMA was −1.93° (95% CI: −2.47 to −1.40°; P < .0001; I2 = 0%, Fig. 6), indicating that the FCRTMA was significantly more valgus with the KA technique than the MA technique. Three studies compared the TCRTMA between the KA and MA techniques, performed in 193 and 194 patients, respectively. The pooled mean difference in TCRTMA was 2.25° (95% CI: 1.56–2.95°; P < .0001; I2 = 0%, Fig. 6), indicating that the TCRTMA was significantly more varus with the KA technique than the MA technique. Three studies compared the TCS between the KA and MA techniques, performed in 190 and 191 patients, respectively. The pooled mean difference in TCS was 1.52° (95% CI: −0.53 to 3.56°; P = .15; I2 = 90%, Fig. 6). Two studies compared the FCF between the KA and MA techniques, performed in 141 and 141 patients, respectively. The pooled mean difference in FCF was 2.48° (95% CI: −2.61 to 7.57°; P = .34; I2 = 94%, Fig. 6).
Figure 6.
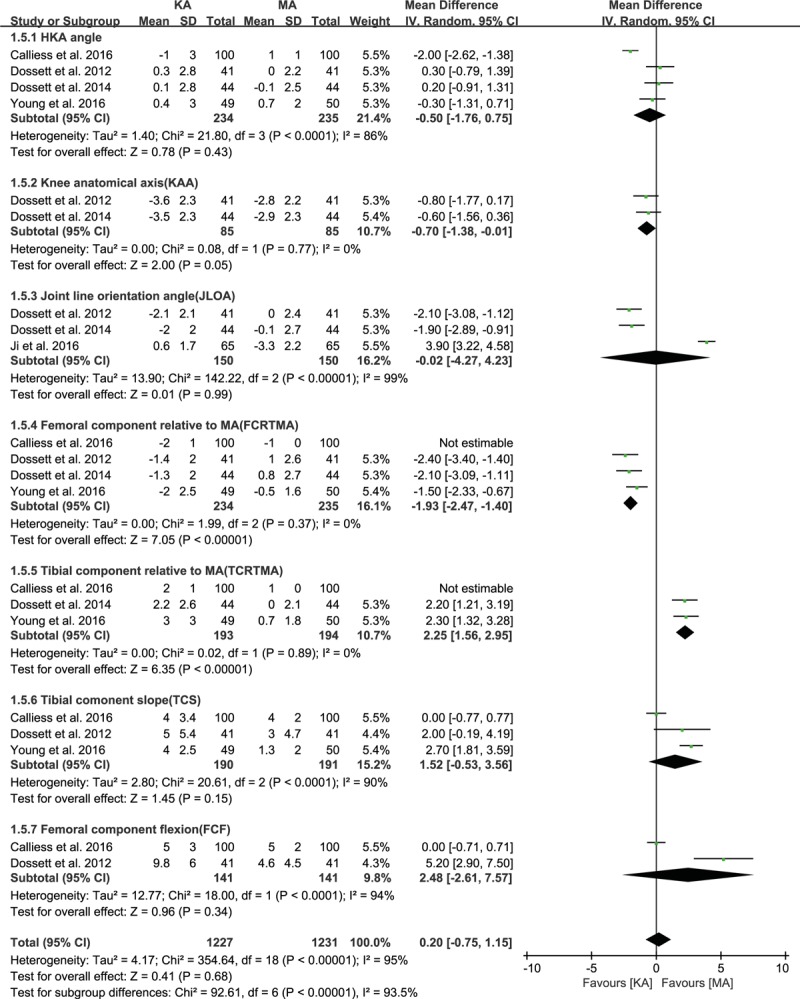
Results of aggregate analysis for comparison of postoperative radiographic outcomes, including HKA angle, KAA, JLOA, FCRTMA, TCRTMA, TCS, and FCF according to different alignment techniques. FCF = femoral component flexion, FCRTMA = femoral component relative to mechanical axis, HKA = hip-knee-ankle, JLOA = joint line orientation angle, KAA = knee anatomical axis, TCRTMA = tibial component relative to mechanical axis, TCS = tibial component slope.
3.6. Postoperative complications
Of the 6 studies, 4 presented data on the proportion of patients who developed postoperative complications. There were no significant differences between groups (KA, 13/368; MA, 12/370; OR, 1.10, 95% CI: 0.49–2.46; P = .82; I2 = 0%, Fig. 7). Four studies were assigned to the major complications subgroup, and 3 were assigned to the minor complications subgroup. The proportion of patients who developed major complications was similar between groups (KA, 3/234; MA, 2/235; OR, 1.51, 95% CI: 0.25–9.19; P = .65; I2 = 0%, Fig. 7), as was the proportion of patients who developed minor complications (KA, 10/134; MA, 10/135; OR, 1.01, 95% CI: 0.41–2.51; P = .99; I2 = 0%, Fig. 7).
Figure 7.
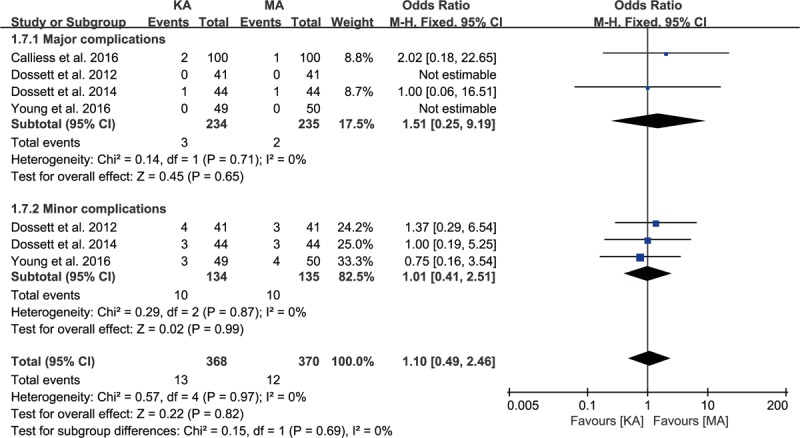
Results of aggregate analysis for comparison of POC according to different alignment techniques, including subgroup analysis by major and minor complications. POC = postoperative complications.
4. Discussion
This meta-analysis found that the KA and MA techniques for primary TKA did not differ significantly in terms of postoperative complications, change in hemoglobin, length of hospital stay, HKA, JLOA, TCS, or FCF. However, the KA technique resulted in a significantly shorter operation time and better functional outcomes than the MA technique, even though the femoral component was placed slightly more valgus and the tibial component, slightly more varus relative to the mechanical axis with the KA technique.
The MA technique for primary TKA leads to improved implant durability and patient function because it has good radiographic alignment and few axis outliers.[20,21] However, a study of clinical and radiographic outcomes in 280 patients who underwent primary TKA reported that placement of the prosthesis within 3° of varus or valgus did not improve the Kaplan-Meier 15-year survivorship estimates compared with placement of the prosthesis outside of this range.[22] Theoretically, the KA technique should provide better clinical results than the MA technique in primary TKA because the KA technique reproduces the obliquity and location of the pre-arthritic joint line, which may lead to improvements in clinical outcomes, greater flexion ROM, and increased patient satisfaction.[9] In the current meta-analysis, we found that overall knee function scores after primary TKA were higher with the KA technique than the MA technique. In addition, the KA technique was associated with a greater distance walked prior to discharge and greater flexion ROM than the MA technique. These results can be explained by the fact that the MA technique requires significant alteration of femoral and tibial joint line obliquity and overall knee alignment from the pre-arthritic state to achieve adequate coronal alignment with a balanced implantation, resulting in the need for considerable soft tissue release.[23,24] In contrast, the KA technique reestablishes more normal knee kinematics by restoring the patient's natural alignment, not neutral alignment, thus preserving the soft tissue envelope and minimizing the frequency of ligament release.[25,26] Another factor that can explain these results is that the orientation of the joint line is parallel to the floor on a long-leg weight-bearing radiograph after the KA technique, despite the range of obliquity to the mechanical axis. This possibility is supported by the results of a study showing that tibial component orientation with the KA technique using navigation is in slight varus relative to the mechanical axis of the tibia. In that study, 62% of patients were outliers to the orientation of 3° varus or valgus to this axis, but only 11% were in excessive varus relative to the floor when weight-bearing. This may help to explain why the KA technique has resulted in no catastrophic failures and has high patient satisfaction and function regardless of whether or not the alignment is in range.[10,27]
Despite the clinical advantages of the KA technique, it also has limitations that may favor the MA technique. Many studies have reported that restoring natural varus with the KA technique creates the risk that the intended or inconsistent position of the components may cause higher stresses on the tibial insert.[28–30] With the KA technique, it is necessary to avoid excessive varus tilt of the tibial component, as this is associated with increased medial compartment wear, even when ideal limb alignment is achieved.[31] In addition, 1 study comparing the kinematics and contact stresses between the KA and MA techniques through computer simulation and finite element analysis found that the peak contact stresses with 5° varus tilt of the tibial component were associated with greater tibiofemoral contact stress than 3° varus tilt or neutral alignment of the tibial component at all flexion angles.[32] Our meta-analysis revealed a significant difference between the KA and MA techniques in radiographic parameters, including the TCRTMA, one of the most important parameters for assessing the clinical failure of polyethylene, suggesting that the tibial component was placed in a slightly more varus (2.25°) position with the KA technique than the MA technique. The discrepancy between the results of this meta-analysis and earlier studies may have arisen because the TCRTMA with the KA technique was less varus than expected, and because the KA technique now has patient-specific instruments and improvements in fixation and surgical techniques that diminish the risk of excessive varus tilt of the tibial components and restore the 3 functional kinematic axes. These axes are parallel or perpendicular to the natural joint line between the femur and tibia throughout the motion arc.[33] Together, these findings suggest that the KA technique may lead to postoperative alignment of >3° varus due to restoration of pre-arthritic joint alignment. Therefore, the results of weight-bearing radiographs that show natural limb alignment of >3° varus without maintaining the orientation of the joint line parallel to the floor should be interpreted with caution. These cases may result in polyethylene wear and component loosening after the KA technique.
This study had several limitations. Of the 6 studies, 1 was observational, leading to reducing the accuracy and reliability of the results due to uncontrolled bias. In addition, the heterogeneity of the included studies could be explained by slight differences in other factors affecting clinical outcomes, including the use of a wide variety of implants and patient-specific instruments. Finally, long-term results of implant survival and patient function were not compared between the 2 techniques. Therefore, long-term, high-quality RCTs are needed to confirm the clinical benefits of the KA and MA techniques in primary TKA.
5. Conclusions
In summary, this meta-analysis found no significant differences between the KA and MA techniques for primary TKA in terms of postoperative complications, change in hemoglobin, length of hospital stay, HKA, JLOA, TCS, or FCF. However, the KA technique resulted in a significantly shorter operation time and better overall functional outcomes than the MA technique, even though the femoral component was placed slightly more valgus and the tibial component slightly more varus relative to the mechanical axis with the KA technique.
Footnotes
Abbreviations: CI = confidence interval, KA = kinematic alignment, MA = mechanical alignment, OR = odds ratio, TKA = total knee arthroplasty.
J-RY and S-BH contributed equally to this work.
The research of this study was conducted at Veterans Health Service Medical Center.
The authors report no conflicts of interest.
References
- [1].Song MH, Yoo SH, Kang SW, et al. Coronal alignment of the lower limb and the incidence of constitutional varus knee in Korean females. Knee Surg Relat Res 2015;27:49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Barrett WP, Mason JB, Moskal JT, et al. Comparison of radiographic alignment of imageless computer-assisted surgery vs conventional instrumentation in primary total knee arthroplasty. J Arthroplasty 2011;26:1273–84. [DOI] [PubMed] [Google Scholar]
- [3].Kim DK, Seo MC, Song SJ, et al. Are Korean patients different from other ethnic groups in total knee arthroplasty? Knee Surg Relat Res 2015;27:199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Shetty GM, Mullaji A, Khalifa AA, et al. The effect of sagittal knee deformity on preoperative measurement of coronal mechanical alignment during total knee arthroplasty. Knee Surg Relat Res 2017;29:110–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Shin YS, Kim HJ, Ko YR, et al. Minimally invasive navigation-assisted versus conventional total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 2016;24:3425–32. [DOI] [PubMed] [Google Scholar]
- [6].Baker P, Van der Meulen J, Lewsey J, et al. The role of pain and function in determining patient satisfaction after total knee replacement: data from the National Joint Registry for England and Wales. J Bone Joint Surg Br 2007;89:893–900. [DOI] [PubMed] [Google Scholar]
- [7].Bourne RB, Chesworth BM, Davis AM, et al. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 2010;468:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Rothwell A, Hooper G, Hobbs A, et al. An analysis of the Oxford hip and knee scores and their relationship to early joint revision in the New Zealand Joint Registry. J Bone Joint Surg Br 2010;92:413–8. [DOI] [PubMed] [Google Scholar]
- [9].Howell SM, Hull ML. Kinematic alignment in total knee arthroplasty. Insall and Scott Surgery of the Knee. Philadelphia, PA: Elsevier; 2012. 1255–68. [Google Scholar]
- [10].Victor JM, Bassens D, Bellemans J, et al. Constitutional varus does not affect joint line orientation in the coronal plane. Clin Orthop Relat Res 2014;472:98–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Griffin D, Parsons N, Shaw E, et al. Operative versus non-operative treatment for closed, displaced, intra-articular fractures of the calcaneus: randomised controlled trial. BMJ 2014;349:g4483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wells G, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2013. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed on May 1, 2016. [Google Scholar]
- [13].Deeks J, Higgins J, Altman D, et al. Cochrane Handbook for Systematic Reviews of Interventions, version 5.1. 0 (updated March 2011). The Cochrane Collaboration; 2011. [Google Scholar]
- [14].Belvedere C, Tamarri S, Ensini A, et al. Better joint motion and muscle activity are achieved using kinematic alignment than neutral mechanical alignment in total knee replacement. Gait Posture 2015;42:S19–20. [Google Scholar]
- [15].Calliess T, Bauer K, Stukenborg-Colsman C, et al. PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 2017;25:1743–8. [DOI] [PubMed] [Google Scholar]
- [16].Dossett H, Estrada N, Swartz G, et al. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J 2014;96:907–13. [DOI] [PubMed] [Google Scholar]
- [17].Dossett HG, Swartz GJ, Estrada NA, et al. Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics 2012;35:e160–9. [DOI] [PubMed] [Google Scholar]
- [18].Ji HM, Han J, San Jin D, et al. Kinematically aligned TKA can align knee joint line to horizontal. Knee Surg Sports Traumatol Arthrosc 2016;24:2436–41. [DOI] [PubMed] [Google Scholar]
- [19].Young SW, Walker ML, Bayan A, et al. The Chitranjan S. Ranawat Award: no difference in 2-year functional outcomes using kinematic versus mechanical alignment in TKA: a randomized controlled clinical trial. Clin Orthop Relat Res 2017;475:9–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Harvie P, Sloan K, Beaver RJ. Computer navigation vs conventional total knee arthroplasty: five-year functional results of a prospective randomized trial. J Arthroplasty 2012;27:667–72. [DOI] [PubMed] [Google Scholar]
- [21].Saibaba B, Dhillon MS, Chouhan DK, et al. Significant incidence of extra-articular tibia vara affects radiological outcome of total knee arthroplasty. Knee Surg Relat Res 2015;27:173–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Parratte S, Pagnano MW, Trousdale RT, et al. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 2010;92:2143–9. [DOI] [PubMed] [Google Scholar]
- [23].Bellemans J, Colyn W, Vandenneucker H, et al. The Chitranjan Ranawat Award: Is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 2012;470:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Gu Y, Roth JD, Howell SM, et al. How frequently do four methods for mechanically aligning a total knee arthroplasty cause collateral ligament imbalance and change alignment from normal in white patients? J Bone Joint Surg Am 2014;96:e101. [DOI] [PubMed] [Google Scholar]
- [25].Howell SM, Papadopoulos S, Kuznik K, et al. Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop 2015;39:2117–24. [DOI] [PubMed] [Google Scholar]
- [26].Hutt J, LeBlanc MA, Massé V, et al. Kinematic TKA using navigation: surgical technique and initial results. Orthop Traumatol Surg Res 2016;102:99–104. [DOI] [PubMed] [Google Scholar]
- [27].Howell SM, Papadopoulos S, Kuznik KT, et al. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 2013;21:2271–80. [DOI] [PubMed] [Google Scholar]
- [28].Howell SM, Chen J, Hull ML. Variability of the location of the tibial tubercle affects the rotational alignment of the tibial component in kinematically aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2013;21:2288–95. [DOI] [PubMed] [Google Scholar]
- [29].Nedopil AJ, Howell SM, Rudert M, et al. How frequent is rotational mismatch within 0(±10) in kinematically aligned total knee arthroplasty? Orthopedics 2013;36:e1515–20. [DOI] [PubMed] [Google Scholar]
- [30].Park A, Duncan ST, Nunley RM, et al. Relationship of the posterior femoral axis of the “kinematically aligned” total knee arthroplasty to the posterior condylar, transepicondylar, and anteroposterior femoral axes. Knee 2014;21:1120–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Srivastava A, Lee GY, Steklov N, et al. Effect of tibial component varus on wear in total knee arthroplasty. Knee 2012;19:560–3. [DOI] [PubMed] [Google Scholar]
- [32].Ishikawa M, Kuriyama S, Ito H, et al. Kinematic alignment produces near-normal knee motion but increases contact stress after total knee arthroplasty: a case study on a single implant design. Knee 2015;22:206–12. [DOI] [PubMed] [Google Scholar]
- [33].Eckhoff DG, Bach JM, Spitzer VM, et al. Three-dimensional morphology and kinematics of the distal part of the femur viewed in virtual reality. J Bone Joint Surg Am 2003;85:97–104. [DOI] [PubMed] [Google Scholar]


