Abstract
The aim of this study was to explore the clinical value of ultrasonic monitoring in the assessment of pulmonary recruitment and the best positive end-expiratory pressure (PEEP).
Between January 2015 and June 2017, 40 patients with acute respiratory distress syndrome in our hospital were randomly divided into 2 groups: ultrasound group (ULS group; n = 20) and oxygenation group (OXY group; n = 20). The PEEP incremental method was used to perform recruitment maneuvers. Ultrasound scoring and the oxygenation method were used to evaluate the pulmonary recruitment endpoint. The best PEEP was chosen by ultrasound scoring and the oxygenation method after achieving the pulmonary recruitment endpoint and sustaining it for 15 minutes.
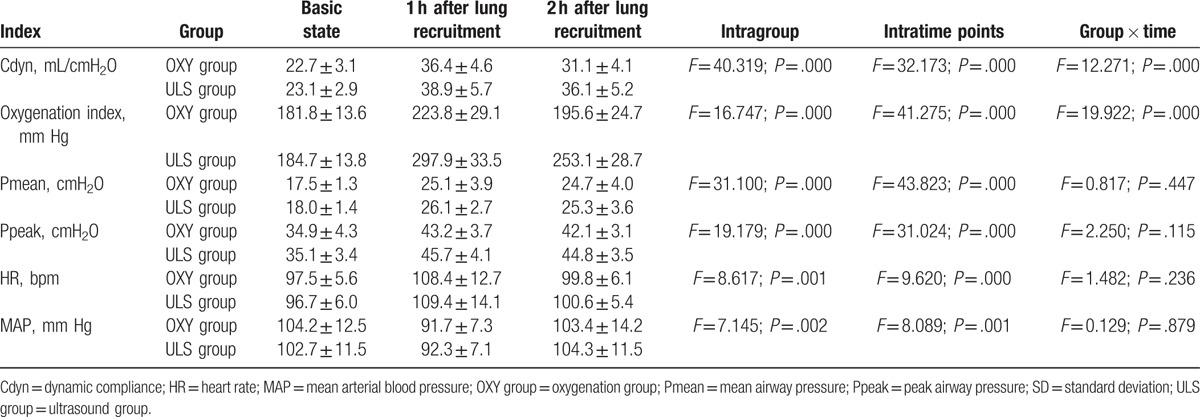
The oxygenation index, PEEP, peak airway pressure (Ppeak), mean airway pressure (Pmean), and dynamic compliance (Cdyn) in the OXY group were significantly lower than those in the ULS group (P < .05) at the pulmonary recruitment endpoint; however, there was no statistical significance in the mean arterial blood pressure (MAP) or heart rate (HR) (P > .05). The best PEEPs in the OXY and ULS groups were 13.1 ± 3.1 and 15.7 ± 4.2 cmH2O, respectively, with a significant difference between the 2 groups (t = 2.227, P = .016). Compared with the basal state, the Cdyn, oxygenation index, Pmean, and Ppeak in both groups significantly increased after pulmonary recruitment (P < .05). Furthermore, the Cdyn and oxygenation index in the ULS group were significantly higher than those in the OXY group after pulmonary recruitment (P < .05). The HR in both groups significantly increased, and the MAP significantly decreased. Two hours after recruitment, the HR and MAP returned to near basal levels without a significant difference between the 2 groups (P > .05).
Lung ultrasound can be used to detect the endpoint of lung recruitment and the best PEEP, with good effects on lung compliance and oxygenation improvement.
Keywords: lung recruitment maneuver, oxygenation, positive end-expiratory pressure, ultrasound scoring
1. Introduction
Knowing the positive end-expiratory pressure (PEEP) helps in the treatment of acute respiratory distress syndrome (ARDS),[1] which is associated with a significant risk of mortality.[2] Methods used to evaluate the effect of PEEP-induced pulmonary recruitment include computed tomography (CT), the static pressure–volume (P–V) curve, and the oxygenation method.[3–5] However, the uses of these methods are limited due to objective factors. For example, for lung CT examination, critically ill patients must be transported out of the intensive care unit, which carries risk of transfer, high cost, and radiation exposure.[6–8] Static P–V curve tracing requires deep sedation and muscle relaxation. The oxygenation method is the most commonly used in clinics, but it is necessary to repeat arterial blood collection many times, which is cumbersome and expensive.
An ultrasonic examination is noninvasive, convenient, and reproducible. Due to the low water content, normal lung tissue cannot be detected by an ultrasonic examination; however, abnormal lung tissue has obvious changes in the gas/water ratio, which can be observed by the ultrasonic method.[9–11] Studies have confirmed the value of ultrasound in the evaluation of lung recruitment.[12–17] However, most of these compared ultrasound scoring with CT and the static P–V curve method. Comparisons between ultrasound scoring and the oxygenation method, which is commonly used in clinics, are rarely reported.
In the present study, the PEEP incremental method was used for pulmonary recruitment, and the best PEEP was evaluated using ultrasound scoring and the oxygenation method, which could provide a new way for monitoring the pulmonary recruitment endpoints of ARDS and the best PEEP.
2. Methods
2.1. Patients
A total of 40 patients with ARDS who were admitted to our hospital from January 2015 to June 2017 were enrolled. Among them, there were 27 males and 13 females, aged 19 to 84 years (53.8 ± 9.3 years).
Inclusion criteria were as follows: patients diagnosed according to the 2012 Berlin definition of ARDS[18]; patients hospitalized within 3 days after onset; oxygenation index [(arterial carbon dioxide partial pressure (PaCO2)/fraction of inspiration oxygen (FiO2)] ≤200 mm Hg; chest X-ray showing a patchy shadow on the lungs; respiratory failure could not be completely explained by heart failure or excessive fluid input; and patients providing informed consent and the inclusion was approved by the ethics committee of Shanghai Songjiang District Central Hospital.
Exclusion criteria were as follows: patients with intracranial hypertension, pleural fistula, or pneumothorax; patients with an oxygenation index of <100 mm Hg; patients with chronic obstructive pulmonary disease and hemodynamic instability during lung recruitment; and patients with a history of extrapulmonary organ dysfunction, pregnancy, or chest wall surgery.
The patients were randomly divided into 2 groups: ultrasound group (ULS group; n = 20) and oxygenation group (OXY group; n = 20). Baseline characteristics were collected, including gender, age, acute physiology, and chronic health evaluation [Acute Physiology and Chronic Health Evaluation (APACHE) II system].[19]
2.2. Lung recruitment method
All patients accepted tracheotomy or tracheal intubation for mechanical ventilation with the initial model of volume-controlled ventilation [tidal volume (VT), 6 mL/kg according to the actual body weight of patients; PEEP, 0 cmH2O; inspiratory time, 25%; inspiratory pause time, 0.2 seconds; respiratory rate adjusted to keep the PaCO2 at 35–45 mm Hg; and inhaled FiO2 adjusted to ensure SPO2 > 90%). Arterial intubation was then performed to monitor blood pressure. Arterial blood gas analysis and ultrasound regasification scoring [zero–added PEEP (ZEEP)] were conducted. During the observation period, patients were treated with propofol or midazolam for full sedation.
After placing the patients in the supine position, the PEEP incremental method was used for lung recruitment using the ventilator mode of pressure control (PC): After mechanical ventilation was resumed with pressure assist/control at a peak pressure of 35 cmH2O (PC setting 15 cmH2O and PEEP setting at 20 cmH2O) with 100% FiO2 for 15 minutes, blood gas analysis and lung ultrasonography were performed; PC was kept constant (20 cmH2O), the PEEP was increased at intervals of 5 cmH2O, maintaining the incremented PEEP for ventilation of 60 seconds, adjusted to 15 cmH2O and maintained for another 15 minutes; blood gas analysis and lung ultrasonography were then performed. The PEEP was increased until achieving the pulmonary recruitment endpoint that was evaluated by ultrasound scoring and oxygenation method.
After full pulmonary recruitment was obtained, the PEEP was adjusted to 20 cmH2O to prevent the collapse of alveoli and PC was adjusted to 6 mL/kg of VT for lung protective ventilation.
2.3. Recruitment endpoint
2.3.1 ULS group
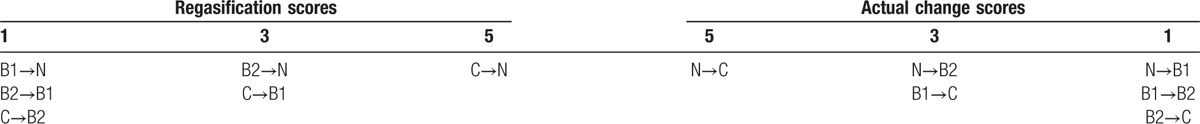
After adjustment of the PEEP and stable ventilation for 15 minutes, ultrasound of the whole lung was performed and the ZEEP was recorded. According to the method as previously described[20] (Table 1), regasification scores were calculated and then ultrasound findings were divided into 4 classes: normal ventilation (N): A line can be found but B line is rare; slightly reduced ventilation (B1): multiple boundaries clear, regularly distributed (spacing > 7 mm) A line or irregularly distributed B line; severely reduced ventilation (B2): diffuse distributed, continuous fused B line (spacing <3 mm); and signs of pulmonary consolidation (C): liver echo with dynamic air-filled bronchogram. If the score displayed no further increase, pulmonary recruitment was considered sufficient and the corresponding PC + PEEP was defined as the opening pressure.
Table 1.
Semi-quantitative calculation method for ultrasonic regasification.
2.3.2 OXY group
After adjustment of the PEEP and stable ventilation for 15 minutes each time, arterial blood gas analysis was conducted immediately and the oxygenation index was calculated. If the oxygenation index was higher than 400 mm Hg, pulmonary recruitment was considered sufficient and the corresponding PC + PEEP was defined as the opening pressure.
2.4. Best PEEP for pulmonary recruitment
To select the best PEEP, the PEEP incremental method was used to reduce the PEEP for 2 cmH2O every 5 minutes and PC was adjusted to maintain the VT at 6 mL/kg. In the ULS group, if 2 consecutive scores suddenly increased by more than 30%, then the last level was the best PEEP. In the OXY group, if arterial oxygen partial pressure (PaO2)/FiO2 reduced by more than 10%, then the last level was the best PEEP.
2.5. Observation index
2.5.1 Hemodynamics
A PHILIPS MP60 monitor (Philips Electronics NV, Eindhoven, Netherlands) was used for continuous monitoring of the electrocardiogram and for recording the heart rate (HR), systolic blood pressure, diastolic blood pressure, and mean arterial blood pressure (MAP).
2.5.2 Respiratory mechanics
The PEEP, VT, peak airway pressure (Ppeak), plateau airway pressure (Pplat), mean airway pressure (Pmean), and dynamic compliance (Cdyn) were monitored through a ventilator monitoring panel.
2.5.3 Pulmonary gas exchange indicators
Arterial blood was drawn to determine pulmonary gas exchange indexes. Blood gas analysis (GEM Premier 3000 equipped with GEM CarTIDGE blood gas analyzer, Instrumentation Laboratory, Lexington, MA) was used to determine the pH, PaO2, PaCO2, and arterial oxygen saturation for calculating the oxygenation index.
2.6. Statistical analysis
SPSS19.0 (SPSS Inc., Chicago, IL) was used for statistical analyses. Count data were expressed as n (%) and compared using the χ2 test. Measurement data are presented as mean ± standard derivation. The comparison between the 2 groups was done by using a t test, and the comparison among different time points was conducted using analysis of variance for repeated measurement data. Differences with P values less than .05 were considered statistically significant.
3. Results
3.1. Baseline characteristics
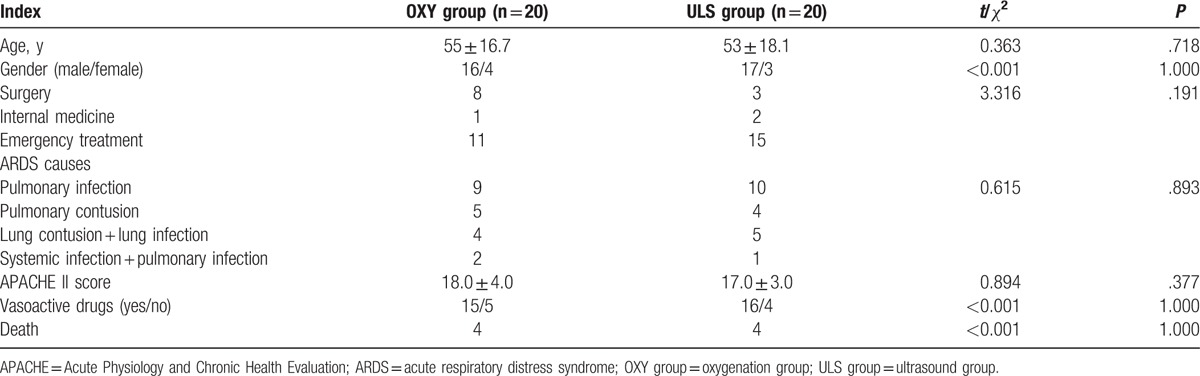
As summarized in Table 2, baseline characteristics, such as gender, age, acute physiology, and chronic health evaluation (APACHE II system), were not significantly different between the OXY group and the ULS group (all P > .05).
Table 2.
Characteristics of patients with ARDS.
3.2. Comparison of the indexes of lung recruitment between the 2 groups
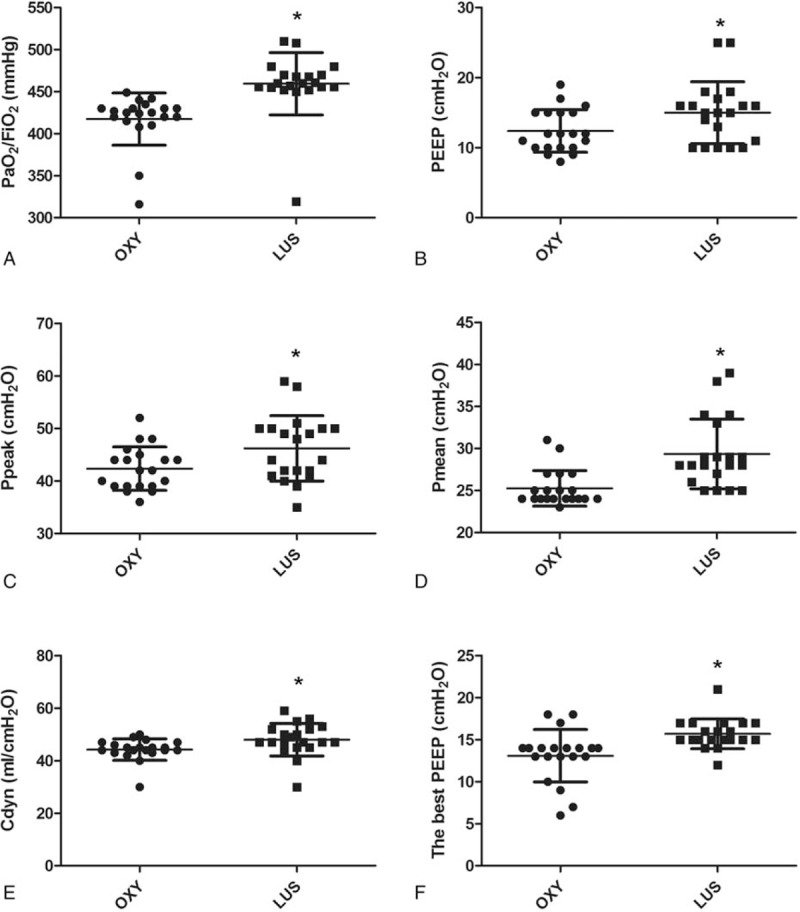
At the end of lung recruitment, the oxygenation index, PEEP, Ppeak, Pmean, and Cdyn in the OXY group were significantly lower than those in the ULS group (P < .05, Table 3 and Fig. 1 A–E). Notably, patients in the above 2 groups were treated with propofol or midazolam for full sedation, and the highest Pmean values in the OXY and ULS groups were 27 and 33 cmH2O, respectively. Considering that the highest Pmean in the 2 groups was not higher than 35 cmH2O and PC could be adjusted to reach 6 mL/kg VT, the VT and PEEP were not compromised. There were no significant differences between the 2 groups in terms of the MAP and HR (P > .05; Table 3). Until the endpoint of the oxygenation method, there were still some B lines. Under different PEEP conditions during the process of lung recruitment, ultrasound showed that the B line decreased and consolidation changed to air bronchogram (Fig. 2). Most of these changes occurred in the anterior and lateral chest walls. There were few changes in the posterior chest wall.
Table 3.
Comparison of lung recruitment endpoints in the 2 groups (n = 20, mean ± SD).
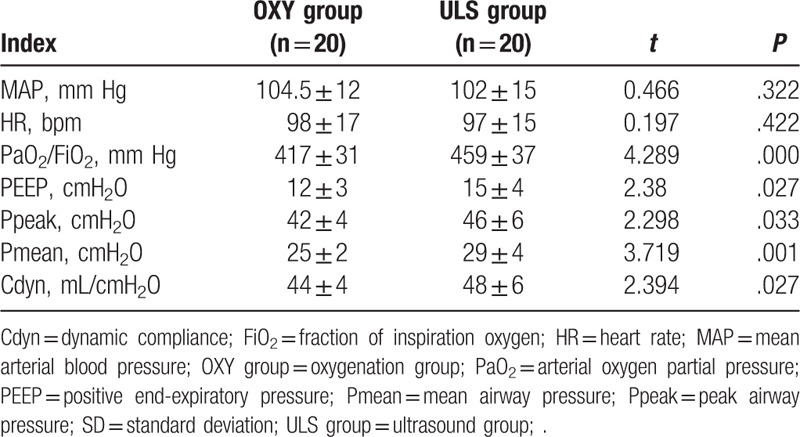
Figure 1.
PaO2/FiO2 (A), PEEP (B), Ppeak (C), Pmean (D), and Cdyn (E) at the end of recruitment maneuvers and the best PEEP (G) in the OXY group and the ULS group. Cdyn = dynamic compliance; FiO2 = fraction of inspiration oxygen; OXY group = oxygenation group; PaO2 = arterial oxygen partial pressure; PEEP = positive end-expiratory pressure; Pmean = mean airway pressure; Ppeak = peak airway pressure; ULS group = ultrasound group. ∗P < .05 compared with the OXY group.
Figure 2.
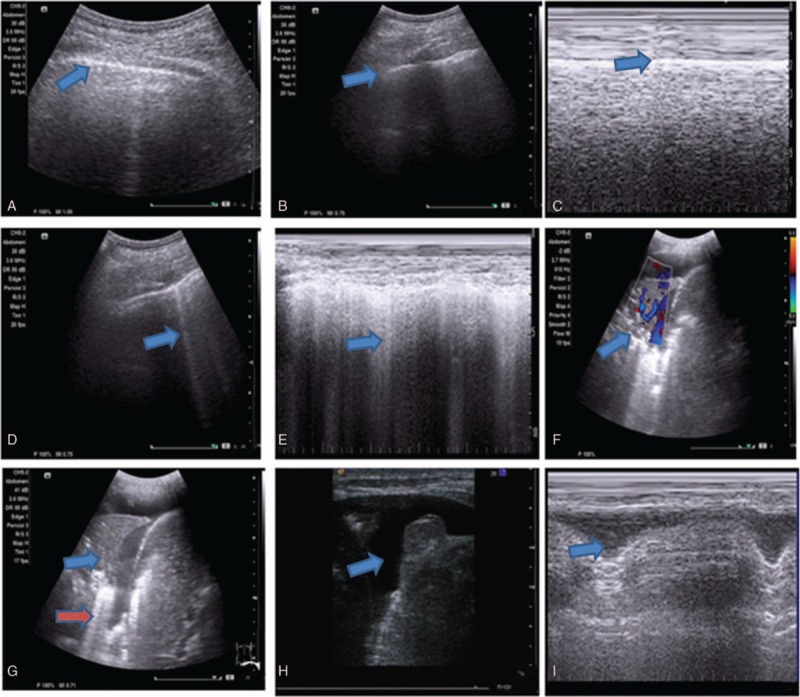
Ultrasound findings. (A) Normal lung ultrasound showing the pleural line (blue arrow); (B) Normal lung ultrasound showing pleural ribs between artifacts (blue arrow); (C) M-type ultrasound normal pleural line; (D) sparse line B1 (blue arrow); (E) M-type fusion line B2 (blue arrow); (F) blood flow signals inside lung consolidation (blue arrow); (G) dynamic air bronchogram inside lung consolidation, in with lung consolidation (blue arrow) and sparse line B1 (red arrow) were observed; (H) pleural effusion (blue arrow); (I) M-type ultrasound line showing the pleural effusion lung line (blue arrow).
3.3. Comparison of the best PEEP titration of the 2 groups
The best PEEPs in the OXY group and the ULS group were 13.1 ± 3.1 and 15.7 ± 1.8 cmH2O, respectively, with a significant difference between the 2 groups (t = 3.41, P = .003, Fig. 1F).
3.4. Comparison of the oxygenation index and hemodynamic indexes before and after lung recruitment
Compared with the basal state, the Cdyn, oxygenation index, Pmean, and Ppeak significantly increased after lung recruitment, and the differences were statistically significant (P < .05) in both groups. After lung recruitment, the Cdyn and oxygenation index in the ULS group were significantly higher than those in the OXY group (P < .05). The HR was significantly increased and the MAP decreased 1 hour after pulmonary recruitment and returned to close to the basal level 2 hours after pulmonary recruitment, without a statistical significance between the 2 groups (P > .05, Table 4).
Table 4.
Comparison of the oxygenation index and hemodynamic indexes between the 2 groups before and after lung recruitment (n = 20, mean ± SD).
4. Discussion
This study used ultrasound scoring and the oxygenation method to monitor the endpoint of lung recruitment. After lung recruitment, with decreasing PEEP levels, recruited alveoli collapsed and the oxygenation level decreased. Until the endpoint, more alveoli collapsed and pulmonary parenchyma changes were aggravated, which led to dramatic changes in the air/water ratio that could be detected by ultrasound; these changes were manifested as replacing of the A line by the B line or air bronchogram consolidation inside the original B line. Our results showed that until the endpoint of the oxygenation method, there was still a part of the B line by the oxygenation method, while at the endpoint of the ultrasound score, oxygenation was closer to normal levels. Moreover, at the endpoint of the ultrasound score method, no difference was observed in the MAP, HR, or other indicators between the 2 groups, indicating that high airway pressure does not significantly affect circulation perfusion. The Cdyn between the 2 groups was not statistically different, which confirmed that at the pulmonary recruitment endpoint assessed by ultrasound scoring, there was no lung injury caused by alveolar overdistension.
During lung recruitment, intermittent high airway pressure was first given to open the collapsed alveoli fully; this was followed by applying appropriate pressure to maintain the opening of the alveoli.[21] Choosing an appropriate PEEP is key to maintain the alveoli open after lung recruitment.[22,23] However, one feature of segment lesions in ARDS is that the lesions of the lower and dorsal lungs are severe, while those of the upper and anterior lungs are slight.[24] The best PEEP was considered when the trapped alveoli was just expanded and the alveolar gas quantity increased by more than 20%; in addition, part of the shunt was removed, oxygenation was improved, lung injury induced by shear stress by repeated alveolar opening and closing was reduced, and pulmonary circulation was improved.[22,23] This research used the PEEP incremental method for lung recruitment and the ultrasound score and oxygenation method for evaluating the best PEEP. The results showed that at the PEEP in the ULS group was significantly higher than that in the OXY group, indicating that although at the oxygenation method endpoint, the oxygenation levels did not decrease and alveoli appeared collapsed. In the ULS group, the Cdyn and oxygenation index were significantly higher than those in the OXY group at the same period, suggesting that at the ultrasound endpoint, most of the alveoli were open after pulmonary recruitment, thereby avoiding an arteriovenous shunt and improving oxygenation and lung compliance.
The advantages of lung ultrasound in the guidance for the PEEP include the following: it can be used for real-time operation; there is no need for deep sedation and muscle relaxants; and it can be used to assess the effect of lung recruitment in gravity-dependent and gravity-independent zones. However, in our study, ultrasound could not accurately identify excessive or normal ventilation. In addition, whether lung ultrasound can translate to shorter time of ventilator use and/or shorter time of ICU stay is largely unknown. Besides, VT was calculated with actual body weight, but not ideal body weight. Therefore, it is necessary to further confirm the ultrasound score as the end of lung recruitment.
In summary, lung ultrasound can be used to detect the lung recruitment endpoint, guide the best PEEP, and improve lung compliance of ARDS patients and oxygenation effect.
Footnotes
Abbreviations: APACHE = Acute Physiology and Chronic Health Evaluation, ARDS = acute respiratory distress syndrome, Cdyn = dynamic compliance, CT = computed tomography, FiO2 = fraction of inspiration oxygen, HR = heart rate, MAP = mean arterial blood pressure, OXY group = oxygenation group, PaCO2 = arterial carbon dioxide partial pressure, PaO2 = arterial oxygen partial pressure, PC = pressure control, PEEP = positive endexpiratory pressure, Pmean = mean airway pressure, Ppeak = peak airway pressure, Pplat = plateau airway pressure, P–V = pressure–volume, SD = standard derivation, ULS group = ultrasound group, VT = tidal volume, ZEEP = zero-added PEEP.
Both KQT and SLY are co-first authors.
Funding/support: This work was supported by the Scientific Research Fund of Shanghai Municipal Commission of Health and Family Planning (Project number: 201440451).
The authors report no conflicts of interest.
References
- [1].Heinrichs W. Positive end-expiratory pressure (PEEP). Der Anaesth 1992;41:653–69. [PubMed] [Google Scholar]
- [2].Mortelliti MP, Manning HL. Acute respiratory distress syndrome. Indian Pediatr 2010;47:861–8. [DOI] [PubMed] [Google Scholar]
- [3].Tehrani FT. A closed-loop system for control of the fraction of inspired oxygen and the positive end-expiratory pressure in mechanical ventilation. Comput Biol Med 2012;42:1150–6. [DOI] [PubMed] [Google Scholar]
- [4].Ingaramo OA, Ngo T, Khemani RG, et al. Impact of positive end-expiratory pressure on cardiac index measured by ultrasound cardiac output monitor∗. Pediatr Crit Care Med 2014;15:15–20. [DOI] [PubMed] [Google Scholar]
- [5].Regli A, Chakera J, De Keulenaer BL, et al. Matching positive end-expiratory pressure to intra-abdominal pressure prevents end-expiratory lung volume decline in a pig model of intra-abdominal hypertension. Crit Care Med 2012;40:1879–86. [DOI] [PubMed] [Google Scholar]
- [6].Oks M, Cohen R, Koenig S, et al. The use of point of care ultrasound in the medical intensive care unit reduces healthcare cost and patient radiation exposure. Chest 2013;144:542A.23429940 [Google Scholar]
- [7].Parker MS, Hui FK, Camacho MA, et al. Female breast radiation exposure during CT pulmonary angiography. AJR Am J Roentgenol 2005;185:1228–33. [DOI] [PubMed] [Google Scholar]
- [8].Xie Z, Liao X, Kang Y, et al. Radiation exposure to staff in intensive care unit with portable CT scanner. Biomed Res Int 2016;2016:1–4. (2, article 183). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Mohanty K, Blackwell J, Egan T, et al. Characterization of the lung parenchyma using ultrasound multiple scattering. Ultrasound Med Biol 2016;140:3186–7. [DOI] [PubMed] [Google Scholar]
- [10].Skouras C, Davis ZA, Sharkey J, et al. Lung ultrasonography as a direct measure of evolving respiratory dysfunction and disease severity in patients with acute pancreatitis. HPB (Oxford) 2015;18:159–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Soldati G, Smargiassi A, Inchingolo R, et al. Lung ultrasonography and vertical artifacts: the shape of air. Respiration 2015;90:86. [DOI] [PubMed] [Google Scholar]
- [12].Du J, Tan J, Yu K, et al. Lung recruitment maneuvers using direct ultrasound guidance: a case study. Respir Care 2015;60:e93–6. [DOI] [PubMed] [Google Scholar]
- [13].Li DK, Liu DW, Long Y, et al. Use of lung ultrasound to assess the efficacy of an alveolar recruitment maneuver in rabbits with acute respiratory distress syndrome. J Ultrasound Med 2015;34:2209–15. [DOI] [PubMed] [Google Scholar]
- [14].Rode B, Vučić M, Siranović M, et al. Positive end-expiratory pressure lung recruitment: comparison between lower inflection point and ultrasound assessment. Wien Klin Wochenschr 2012;124:842–7. [DOI] [PubMed] [Google Scholar]
- [15].Sameshima YT, de Almeida JF, Silva MM, et al. Ultrasound-guided lung recruitment in a 3-month-old infant with acute respiratory distress syndrome. Ultrasound Q 2014;30:301–5. [DOI] [PubMed] [Google Scholar]
- [16].Tusman G, Acosta CM, Costantini M. Ultrasonography for the assessment of lung recruitment maneuvers. Crit Ultrasound J 2016;8:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Sharma JP, Salhotra R, Kumar S, et al. Noninvasive lung recruitment maneuver prevents reintubation and reduces ICU stay. Lung India 2016;33:99–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA 2012;307:2526–33. [DOI] [PubMed] [Google Scholar]
- [19].Knaus WA, Zimmerman JE, Wagner DP, et al. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med 1981;9:591. [DOI] [PubMed] [Google Scholar]
- [20].Bouhemad B, Brisson H, Le-Guen M, et al. Bedside ultrasound assessment of positive end-expiratory pressure–induced lung recruitment. Am J Respir Crit Care Med 2011;183:341–7. [DOI] [PubMed] [Google Scholar]
- [21].Nunn JF. Positive end-expiratory pressure. Surg Gynecol Obstet 1980;58:349. [Google Scholar]
- [22].Jin WH, Jung H, Choi HS, et al. Efficacy of positive end-expiratory pressure titration after the alveolar recruitment manoeuvre in patients with acute respiratory distress syndrome. Crit Care 2009;13:R22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Scohy TV, Bikker IG, Hofland J, et al. Alveolar recruitment strategy and PEEP improve oxygenation, dynamic compliance of respiratory system and end-expiratory lung volume in pediatric patients undergoing cardiac surgery for congenital heart disease. Pediatr Anesth 2009;19:1207–12. [DOI] [PubMed] [Google Scholar]
- [24].Tomashefski JF, Jr, Davies P, Boggis C, et al. The pulmonary vascular lesions of the adult respiratory distress syndrome. Am J Pathol 1983;112:112–26. [PMC free article] [PubMed] [Google Scholar]


