Abstract
Setting: Persons experiencing homelessness (PEH) represent a population at high risk for tuberculosis (TB). While quantitative studies have characterized some important features of this key group, less has been captured directly from PEH about how they experience TB illness itself and the prevention and control measures implemented in response to an outbreak. This qualitative study aimed to explore PEH's TB disease experiences in the context of a large TB outbreak involving homeless shelters in Atlanta, Georgia, USA.
Design: This was a qualitative cross-sectional study involving in-depth interviews with 10 PEH with active TB disease. Key themes were identified through coded data analysis.
Results: The central theme to emerge was that stressful social environments of homeless shelters shape illness experiences and health care seeking behaviors, and limit the influence of shelter-based prevention and control measures implemented in response to a TB outbreak. Despite availability, shelter-based latent tuberculous infection (LTBI) testing and education services were minimally engaged. Furthermore, hardships inherent to homelessness were interrelated with disease normalization and symptom minimization.
Conclusions: Homeless shelter-related stress may have important implications for the prevention and control of TB outbreaks in this setting. This stress may hinder case finding; a model of supplemental TB education and testing for LTBI at proximal community venues is necessary.
Keywords: United States, persons experiencing homelessness, homelessness, qualitative research
Abstract
Contexte: Les personnes sans domicile fixe (SDF) représentent une population à haut risque de tuberculose (TB). Si les études quantitatives ont caractérisé certains traits importants de ce groupe clé, moins d'informations ont été obtenues directement des SDF sur la façon dont ces personnes expérimentent la TB maladie elle-même et les mesures de prévention et de lutte mises en œuvre en réponse à l'épidémie. Cette étude qualitative visait à explorer l'expérience des SDF en matière de TB maladie dans le contexte d'une vaste flambée épidémique impliquant des centres d'hébergement de SDF à Atlanta, Georgie.
Schéma : Une étude qualitative transversale impliquant des entretiens approfondis avec dix SDF atteints de TB active. Les thèmes clés ont été identifiés grâce à une analyse des données codées.
Résultats : Le thème central qui a émergé est que l'environnement social stressant des centres d'hébergement façonne les expériences de la maladie et les comportements de recherche de soins et limite l'influence des mesures de prévention et de lutte basées dans ces centres et mises en œuvre en réponse à une flambée de TB. En dépit de leur disponibilité dans les centres d'hébergement, le dépistage de l'infection tuberculeuse latent (ITL) et les services d'éducation ont été très peu engagés. Plus encore, les difficultés inhérentes à l'absence de domicile fixe ont été indissociables de la normalisation de la maladie et de la minimisation des symptômes.
Conclusions: Le stress lié à l'hébergement dans un refuge pour SDF peut avoir des implications majeures dans la prévention et la lutte contre les flambées de TB dans ce contexte. Ce stress peut entraver la découverte des cas et soutenir un modèle d'éducation supplémentaire à la TB et une recherche de l'ITL dans les lieux communautaires proches.
Abstract
Marco de referencia: Las personas que carecen de vivienda constituyen una población con alto riesgo de contraer la tuberculosis (TB). Los estudios cuantitativos han caracterizado algunos aspectos importantes de este grupo poblacional, pero poco se ha captado directamente de su forma de vivenciar la enfermedad tuberculosa y las medidas de prevención y de control que se instauran en respuesta a un brote epidémico. El presente estudio cualitativo tuvo por objeto analizar las vivencias de la enfermedad tuberculosa por parte de las personas que carecen de vivienda, en el contexto de un amplio brote epidémico de TB que ocurrió en los albergues para personas sin techo en Atlanta, Georgia.
Método: Fue este un estudio cualitativo transversal, que comportó entrevistas exhaustivas a 10 personas sin vivienda, con enfermedad tuberculosa activa. Se reconocieron los principales temas mediante un análisis temático con datos codificados.
Resultados: El principal tema que surgió en el análisis fue que los entornos sociales estresantes de los albergues determinan las experiencias de la enfermedad y el comportamiento de búsqueda de atención y limitan la repercusión de las medidas de prevención y control que se aplican en los albergues en respuesta a un brote epidémico de TB. Pese a su disponibilidad, las pruebas diagnósticas de la infección tuberculosa latente y los servicios educativos prestados en los albergues se utilizaban poco. Además, las adversidades inherentes a la falta de vivienda se correlacionaron con una normalización de la enfermedad y la minimización de los síntomas.
Conclusión: El estrés generado en los albergues destinados a las personas sin vivienda puede tener repercusiones importantes en la prevención y el control de los brotes de TB en estos entornos. Este estrés puede obstaculizar la búsqueda de casos y su demostración respalda la aplicación de un modelo de educación complementaria en materia de TB y de pruebas diagnósticas de la infección latente en los centros comunitarios próximos.
Among US-born tuberculosis (TB) cases, homelessness represents a major risk factor.1 Compared with housed individuals, persons experiencing homelessness (PEH) have a 10-fold increased risk of TB disease,2 are more often hospitalized, and experience worse disease outcomes.3 Furthermore, TB outbreaks among PEH are associated with increased TB transmission, resulting in larger outbreak clusters.4 Despite this, an important perspective is underrepresented in both guidelines and research in the field: that of the affected PEH themselves. Understanding this internal, or ‘emic’ perspective of illness can allow for more defensible public health decision making, and is essential to the implementation of appropriate control measures and effective risk communication.5,6
A large outbreak of drug-resistant TB involving overnight homeless shelters began in Atlanta, Georgia, USA, in 2008, resulting in over 100 cases of active TB disease and involving nine additional states.7 The resultant multifaceted response involved public health collaboration with shelters to develop and implement prevention and control measures.8 It remains unclear, however, how these interventions were experienced by PEH with TB. Utilizing the unique opportunity to interview PEH with active TB disease in the setting of an ongoing outbreak and evolving public health response, this study aimed to explore how individuals experience illness and shelter-based interventions. The goals of this research were to inform ongoing TB control efforts and contribute hypothesis-generating data for further research on TB elimination in this setting.
METHODS
Context
This study was conducted in Atlanta, GA, during an ongoing outbreak of drug-resistant TB among PEH that began in 2008.7 Atlanta has a population of about 5.7 million, with a homeless population estimated at 4317 in 2015.9,10 The metropolitan area is primarily located in Fulton County, where there was an average of 55 cases of TB per year from 2008 to 2015, and 36% of TB cases occurred among PEH.7 The county's public health response to the outbreak included shelter-based prevention and control interventions implemented across all homeless facilities, including TB screening requirements for admission to shelters (TB card program), active TB case finding measures (e.g., intake symptom screening, cough logs), increased availability of voluntary latent tuberculous infection (LTBI) screening, TB education activities (e.g., shelter staff/resident teaching, educational posters), and environmental control measures.8,11
Design
In-depth interviews were conducted with a purposive sample of 10 PEH with active TB disease. Study eligibility criteria were age ⩾18 years, clinical diagnosis of active TB disease, homelessness during the year preceding TB diagnosis, and prior contact with Atlanta city shelters. Homelessness was defined as living in an emergency shelter, a transitional housing program, a place not meant for human habitation, or on the streets. The purpose of these criteria was to ensure inclusion of participants with temporally and contextually relevant experiences in the context of the current outbreak.
The interviews took place between May 2016 and January 2017, were conducted one-on-one, and lasted 30–60 minutes. The interview guide consisted of questions related to six domains, including 1) history and experience of homelessness, 2) homeless shelter context, 3) health literacy, 4) health care seeking behaviors and experiences, 5) TB illness experience, and 6) homeless shelter TB outbreak public health response. Questions were grouped chronologically (pre-diagnosis, post-diagnosis and treatment, post-treatment) to explore changes in knowledge, behavior and experiences over the trajectory of TB illness. Interviews were conducted in English in a private room at the TB Control and Prevention Program by a Caucasian male interviewer (WJC) with training in public health and qualitative methods. Following each interview, the interviewer documented his reflections and noted emerging themes. This information was used to revise the interview guide in an iterative manner. Interviews were digitally recorded and transcribed verbatim by a professional service, then reviewed along with the recordings to ensure accuracy.
After each interview, participants answered a questionnaire documenting demographics, TB risk factors, 2-year housing history, and TB illness history. Each participant's TB clinic medical record was subsequently reviewed to document clinical/microbiological TB diagnoses and epidemiologic/genotypic linkage to the ongoing TB outbreak among PEH.
Recruitment and consent
Most PEH with active TB disease in Fulton County receive treatment through the TB Control and Prevention Program of the Fulton County Department of Health and Wellness (FCDHW). FCDHW disease investigation specialists, homeless shelter outreach team members, and TB clinic staff distributed recruitment flyers to eligible participants. Interested participants called the primary investigator (WJC) and were provided with basic information about the study. Informed consent was obtained at the time of the interviews, and participants were provided with written copies of the study information and an incentive of US$15. Recruitment continued until no new themes were found to be emerging from the interviews, indicating thematic saturation.
The Georgia Department of Public Health Institutional Review Board (ORB; Atlanta, GA, USA) determined that the study did not constitute human subjects research and as such was exempt from the requirement for IRB review and approval (Project 160401).
Thematic analysis
The transcripts were analyzed using the qualitative data management software package MaxQDA (Verbi Software, Berlin, Germany). Thematic analysis was conducted to identify patterns across the interviews in the experiences of the participants. Themes were identified inductively through a structured process of data familiarization, preliminary theme identification, thematic mapping, and theme refinement.12 The qualitative codebook was developed and refined through a process of preliminary identification of salient concepts, initial parallel coding of each interview, discussion among authors about code dimensions across the data, refinement of code definitions, and re-coding of all transcripts to ensure consistency with final code definitions.
RESULTS
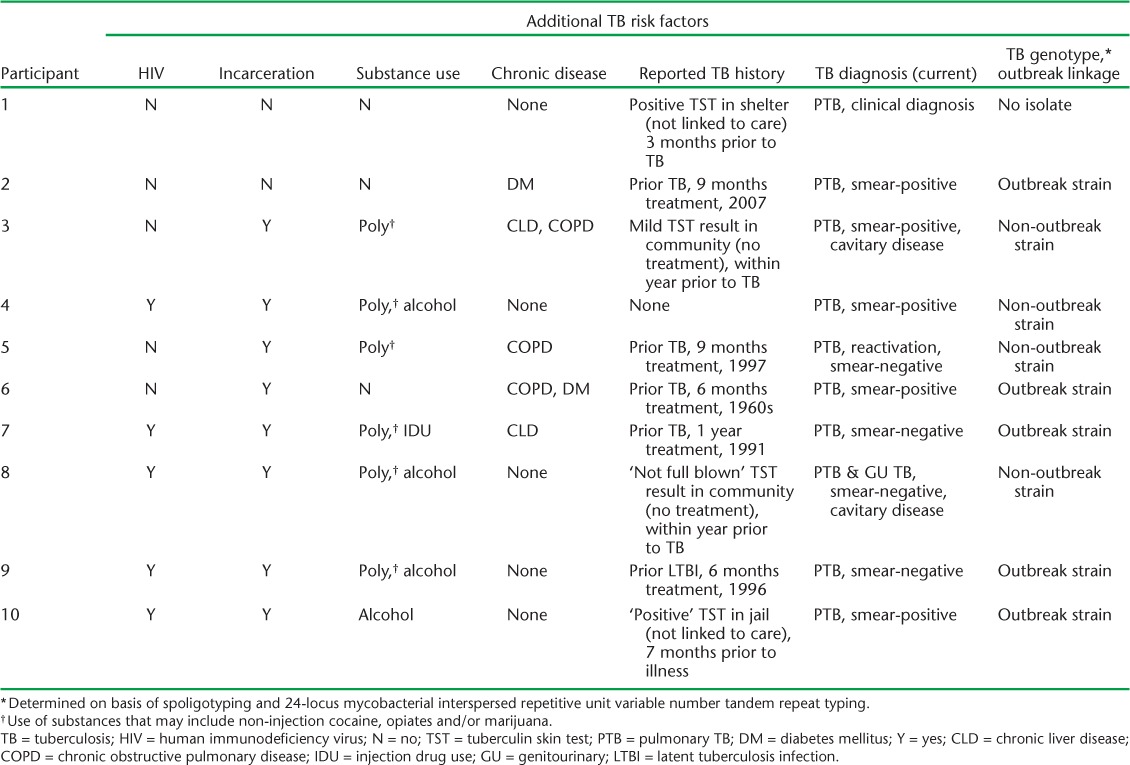
In addition to homelessness, the 10 participants (9 males, 1 female, all African American and born in the USA) had particularly high risk profiles for TB: 50% had previously completed treatment for TB (4 active TB disease cases, 1 LTBI), 50% were infected with the human immunodeficiency virus (HIV), 70% reported substance misuse, and all had a history of incarceration (Table 1). The sex distribution of the participants was representative of that in the outbreak (>90% of cases were male).7 Of the nine cases who had sputum culture-positive disease, genotyping demonstrated that five (56%) had the same TB strain as that associated with the ongoing homeless shelter outbreak (Table 2).
TABLE 1.
Participant demographics and route to TB diagnosis
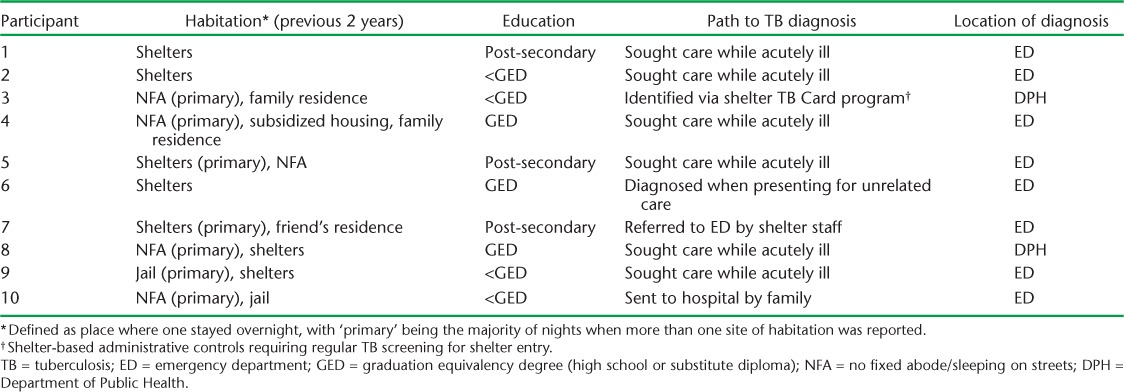
TABLE 2.
Participant TB profile and diagnostics
The interviews identified five pervasive themes regarding the experience of TB among PEH: 1) the health and behavioral impact of the homeless shelter context, 2) the influence of homelessness on disease experience, 3) the role of acute health care services, 4) the experiences with shelter-based interventions implemented in response to the TB outbreak, and 5) sources of TB knowledge and health literacy.
Themes
1. Health and behavioral impact of the homeless shelter context
Participants described shelters as being environments of severe psychological and physical stress, which posed significant health risks. Stress came from the social context of shelters, where violence was described as being common. Half of the participants (n = 5) attributed the violent behavior of shelter residents to mental illness and substance use. The stressful social conditions in the shelters resulted in an antisocial environment in which residents were reticent about disclosing illness or seeking assistance:
Everybody keeps it (health status) quiet. They don't want to (disclose symptoms or seek help)—they feel like they'll be discriminated against and stuff like that. (Participant 7)
The environmental stress of the shelters was viewed as overwhelming:
You won't believe your eyes. I hardly believe my eyes when I see (the shelter). It's like a knife, knife to the heart, trust me. It's not so much the place itself but the type of people you have there. You have to sort of have to mingle with people, that's what I'm trying to say, there are so many people there they be sardines in a can. It's like one of them worse slave boats, out on the ocean. Profound. It is beyond reproach. I'm surprised I dealt with (it) mentally for a while. (Participant 1)
In the shelter, you have to watch your back. You have to watch your step ‘cause you never know who have a gun in there. ‘Cause I done seen a lot of them got killed in there, shot. It's not a place for a suitable human being to be living … I'm telling you, it's not a livable situation. It's unlivable. (Participant 9)
In additional to a pervading sense of risk of physical violence, the poor general health of shelter residents was identified as posing a risk to the participants' own health through communicable disease. Most (n = 7) directly attributed their recent TB to time spent in shelters, specifically noting the physical crowding of ‘coughing’ individuals.
The environmental stress and perceived health risk associated with shelters led most participants (n = 8) to express an aversion to using shelters, with two explicitly stating they would rather sleep on the street. Participants highlighted severe weather conditions as the primary reason for returning to the shelters. Overall, shelters were viewed as repressive environments, as illustrated by poignant references to loss of life and freedom:
I would rather be hung from a tree than to sleep in there … again. (Participant 6)
I don't want to go back to the shelter. It's worse than jail without the bars. (Participant 1)
2. Influence of homelessness on disease experiences
Across all the interviews, reports about the hardships and uncertainties inherent to homelessness were inter-related with disease normalization, symptom minimization and health de-prioritization. Regular exposure to harsh weather conditions and limited access to food were frequently referenced as root causes for recurrent illness and poor general health:
I had noticed that I was kind of losing weight a little bit, but since I wasn't getting no meals, nothing on a regular basis, I chalked it up to that … the cough, I just chalked that up as just, just a minor virus or something. (Participant 5)
In the face of these hardships, participants routinely normalized their symptoms, and it was only on retrospection that most (n = 6) identified the presence of TB symptoms preceding their diagnosis. Rather than limited access to care (discussed further below), participants referenced lack of awareness of being ill as the key reason for not seeking care. The degree of symptom minimization is apparent in that seven participants were severely ill, requiring hospital-based care at the time of first presentation and diagnosis:
I didn't think I had (TB) … I felt that I probably got wet, and when I was drinking and I had this seizure, I thought that I probably just caught a cold and stuff, but I didn't know that I caught TB. (Participant 4)
Three participants also avoided care because of fears about the health and social implications (i.e., isolation or losing shelter) of a medical diagnosis:
Like cancer, people would rather just die of it than to go find out that they have it. (Participant 5)
Substance abuse was also common among participants (n = 7), and may have contributed to a deprioritization of their health among some individuals:
I really didn't take time because of the drug habit. I didn't take time out to go and take care of myself, ‘cause I was too busy trying to chase that crack (cocaine). (Participant 9)
3. Role of acute health care services
A typical case representing patterns of health care engagement and the role of acute health care services is provided in the Figure. Prior to TB illness, hospital emergency rooms (ER) represented the primary access point for all forms of medical care among participants. Less frequently reported sites were community clinics, church health fairs, and a mobile health unit. The ER at Grady Memorial Hospital (GMH, Atlanta, GA, USA) represented the single most common site to access care. GMH is a large public hospital located in proximity to shelters and providing care primarily to low-income, uninsured, and vulnerable populations. All participants reported receiving prior care at GMH, and eight of the 10 participants were diagnosed with TB there. A lack of adequate health insurance was reported by all participants as a barrier to regularly accessing community health services and a determinant for accessing ER services at GMH:
[GMH] is available, so, you know, you can always go to (GMH) emergency without money, without insurance. (Participant 5)
FIGURE.
Typical case representing patterns of health care engagement. HIV = human immunodeficiency virus; LTBI = latent tuberculous infection; ER = emergency room; TB = tuberculosis.
During TB illness the majority of participants (n = 7) reported no health care contacts prior to being diagnosed. Following TB diagnosis, the role of acute health care services was replaced by community-based health services. Nearly all participants (n = 9) remained in ongoing community-based TB care at the time of interview. Participants reported no longer accessing acute health services, and those requiring additional non-TB-related health care services (n = 7) had been linked to community services: HIV care, medical specialists, and primary care.
4. Experiences with shelter-based interventions implemented in response to the TB outbreak
Participants described a wide range of experiences with shelter-based interventions that had been newly implemented in response to the TB outbreak. The TB card program was described as a particularly impactful intervention. This program required homeless individuals to undergo TB screening every 6–12 months, after which they were provided with a dated clearance card, specifying diagnosis and treatment status required for shelter entry. All participants were aware of this program. One participant was diagnosed through the TB card program, illustrating the effectiveness of this intervention.
Participants with recent shelter contact reported that the TB card program had become more uniform across different shelters and stringently enforced over the past 2 years:
You have to have a card. You have to be updated. Cannot be expired. They doing that now. Back a while, back a few years ago, they didn't. You would just go check in. Now you have to … have a card out, before you come in. (Participant 9)
Although voluntary TB screening was available at shelters, participants reported that they did not access this. Instead, the majority of participants (n = 9) reported routine prior testing for LTBI at community-based venues, including churches, health fairs and mobile health units. While prior LTBI testing coverage appeared to be satisfactory, follow-up for interpretation of results was variable. Among participants who did follow up for results, nearly half (n = 4) reported receiving unclear messaging from providers about their results. Two were told their results were positive but ‘mild’ or ‘not full blown’, not requiring treatment or follow-up, and two others were told their results were positive but were not directed to further care. Each of these participants went on to develop active TB within a year.
5. Sources of TB knowledge and health literacy
Most participants (n = 7) reported having no or inaccurate knowledge about the cause, symptoms, or risk factors of TB prior to their current diagnosis. This held true even for those who had previously received treatment for TB. Among this latter group, misconceptions about ongoing risk for TB were common—reported by 4 of 5—and characterized by statements such as:
[…] I had in my mind that since I already had it [TB], that um, I couldn't get it again. (Participant 2)
Interestingly, several participants highlighted disparities in available information between HIV and TB:
They didn't have any pamphlets concerning TB. They have HIV, and stuff like that, but they didn't have awareness of TB at the health fair, the health screenings. (Participant 5)
Participants also commonly reported conflation of HIV and TB risk prior to their current diagnosis, such as perceptions of TB being a disease transmitted through unsafe sexual practices and needle sharing.
The main reported sources of general health information prior to TB diagnosis were church- and community-based health fairs and medical care providers, although TB-specific education from these sources was only reported by a single participant. Only two participants reported receiving or being aware of TB-specific health education in the shelter setting, although this was widely implemented in response to the TB outbreak.11 Following TB diagnosis, the majority of the participants (n = 9) demonstrated accurate knowledge about TB, based on the responses to the interview questions, and identified the Department of Public Health and/or current medical providers as primary sources of health information.
DISCUSSION
Our study explored insiders' perspectives of TB illness among PEH during a large outbreak. The central theme to emerge from our analysis was that the social context of homeless shelters—along with the hardships of homelessness itself—shapes illness experiences and health care-seeking behaviors, and limits the influence of traditional shelter-based prevention and control measures implemented in response to a TB outbreak.
Among our participants, health was de-prioritized in relation to more immediate needs such as safety, shelter, and food. Symptoms of TB were routinely normalized, and health care services were often not sought until disease had progressed to an advanced stage. This delay increases both individual morbidity and public health implications. As an illustration, an earlier investigation of this TB outbreak determined that the average estimated infectious period was greater than 3 months, 85% of cases required hospitalization, and there were 10 TB-related deaths.7 Similar themes of health de-prioritization and symptom normalization relating to delayed presentation for care were identified in two qualitative studies involving homeless persons in the UK.13,14 Our findings add to this work by highlighting the influence of the social environment of the homeless shelter on these suboptimal health care-seeking behaviors.
The stressful shelter environment also appeared to reduce the impact of public health interventions implemented in response to the TB outbreak. The mandatory active TB screening system for shelter admission, the TB card program, was uniformly experienced by participants; however the passive measures of LTBI screening, education, and symptom reporting were either not experienced or under-engaged. While all participants described receiving prior LTBI testing, this occurred exclusively at venues outside the shelter setting. Similarly, shelter-based TB education was minimally experienced by participants.
The majority of participants reported accessing health education from community-based venues; however, TB-specific education was reported to be seldom available. Church- and community-based health fairs represented key points of contact for both LTBI testing and general health education. Our findings suggest that the social context of shelters led to a preference for addressing health concerns outside of the shelters. The concept that health behavior patterns of PEH are often motivated by fears of being labeled as ill, facing discrimination, and being socially isolated is similarly described in previous qualitative studies exploring health care decision prioritization,15 perceived external barriers to accessing health care,16 and attitudes about TB illness.17 This pattern of accessing LTBI testing and health education outside of the shelter setting may also have public health implications in the form of incomplete case finding and delayed care seeking—longer infectious periods—among PEH who develop active TB disease because of limited TB specific health literacy.
Regular access and consistent messaging are necessary to maximize the impact of TB-related risk-communication and LTBI testing procedures.18,19 While general health and HIV-related educational resources were accessible at community venues, TB-specific education was not similarly accessible for our participants. Such reports suggest that outbreak response-related, shelter-based TB education measures might have had greater impact if they had been expanded or relocated to community venues where general health education was more regularly accessed. Regarding LTBI testing, although most participants reported previously being tested at community venues, follow-up and messaging about results appeared to be sub-optimal. As others have found, the need to return for LTBI test results, typically after 48–72 hours, was reported as a barrier to both being tested and obtaining results.15,20 Furthermore, ambiguous messaging about the results and lack of follow-up treatment arrangements suggest a need for more systematic LTBI testing procedures at community venues.
Limitations
Social instability and a lack of fixed habitation were inherent to our study population, and made recruitment particularly challenging. Participants thus predominantly consisted of homeless individuals who were undergoing TB treatment at the time of participation, given that they were more accessible than those who had completed treatment. While this may have minimized recall bias, recent diagnosis and engagement in care at the time of the interviews may mean that the high levels of current TB-specific knowledge among participants are conditional and temporary. The predominance of recently diagnosed participants may also limit the transferability of themes to those no longer in care. Furthermore, the participants' reports of encountering few barriers to accessing care is in stark contrast to the findings of multiple previous studies evaluating the health care-seeking behaviors of homeless persons,13,14,21,22 further limiting the transferability of the findings. We postulate that this largely reflects the unique health care service environment (described above) created by GMH.
CONCLUSIONS
Systematic qualitative assessments in the context of evolving public health responses, such as the work presented here, have the potential to provide novel insights that can strengthen public health decision making and as such represent an important complementary research tool in the fight to end TB.6,23 Our study is among the first to specifically analyze TB disease experiences among PEH, and is unique in that the assessment was made in the context of a large, ongoing outbreak. PEH with active TB disease face many stresses in their lives, most notably the highly stressful social context of shelters. Shelter-related stress may have important implications for the prevention and control of TB outbreaks in this setting, hindering case finding, LTBI testing, and TB education efforts. Furthermore, we found that through the provision of temporary housing during active disease management and by facilitating linkages to community medical care, TB programs can serve as catalysts for longer-term sociomedical stabilization of this population. To break the chronic cycle of homelessness and TB, a concurrent collaborative priority for TB prevention and control efforts is to provide housing for PEH on a more long-term basis.
Acknowledgments
This work was made possible by the generous assistance of the Fulton County Department of Health and Wellness (Atlanta, GA, USA). A Yamin of the Tuberculosis Clinic (Atlanta, GA), disease investigation specialist R Hickson, and the entire Shelter Outreach Teamled by S Alexander were invaluable to the participant recruitment. U Onwubiko of the Georgia Department of Public Health (Atlanta, GA) kindly provided supporting epidemiological data. The authors also acknowledge the support and continued efforts of the Atlanta Tuberculosis Task Force (Atlanta, GA) co-chaired by T Andrews. Finally, this research would not have been possible without the inspirational participants who candidly shared their illness experiences.
Footnotes
Conflicts of interest: none declared.
References
- 1. Salinas J L, Mindra G, Haddad M B, Pratt R, Price S F, Langer A J.. Leveling of tuberculosis incidence—United States, 2013–2015. MMWR Morb Mortal Wkly Rep 2016; 65: 273– 278. [DOI] [PubMed] [Google Scholar]
- 2. Bamrah S, Yelk Woodruff R S, Powell K, Ghosh S, Kammerer J S, Haddad M B.. Tuberculosis among the homeless, United States, 1994–2010. Int J Tuberc Lung Dis 2013; 17: 1414– 1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Marks S M, Taylor Z, Burrows N R, Qayad M G, Miller B.. Hospitalization of homeless persons with tuberculosis in the United States. Am J Public Health 2000; 90: 435– 438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yuen C M, Kammerer J S, Marks K, Navin T R, France A M.. Recent transmission of tuberculosis—United States, 2011–2014. PLOS ONE 2016; 11: e0153728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization. . Rapid risk assessment of acute public health events. WHO/HSE/GAR/ARO/2012.1 Geneva, Switzerland: WHO, 2012. [Google Scholar]
- 6. Beebe J. Rapid assessment process: an introduction. Lanham, MD, USA: AltaMira Press, 2001. [Google Scholar]
- 7. Powell K M, VanderEnde D S, Holland D P, . et al. Outbreak of drug-resistant mycobacterium tuberculosis among homeless people in Atlanta, Georgia, 2008–2015. Public Health Reports 2017; 132: 231– 240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Georgia Department of Public Health. . Guidelines for preventing and controlling tuberculosis in Atlanta homeless housing facilities, 2016. Atlanta, GA, USA: Georgia Department of Public Health, 2016. https://dph.georgia.gov/sites/dph.georgia.gov/files/TBguidelines_5.26.16_EK_FINAL_v2.pdf Accessed July 2017. [Google Scholar]
- 9. Georgia Department of Community Affairs. . 2015 report on homelessness: Georgia's 14 000. Atlanta, GA, USA: Georgia DCA, 2015. [Google Scholar]
- 10. United States Census Bureau. . Annual estimates of the resident population: April 1, 2010 to July 1, 2015—United States—metropolitan statistical area. Washington, DC, USA: United States Census Bureau, 2015. https://fact-finder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk Accessed July 2017 [Google Scholar]
- 11. Preetha N, Worrell M C, Andrews T, . et al. Brief report: engaging homeless service providers in educational efforts during a tuberculosis outbreak in Atlanta. J Ga Public Health Assoc 2016; 6: 4. [Google Scholar]
- 12. Braun V, Clarke V.. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77– 101. [Google Scholar]
- 13. Rae B E, Rees S.. The perceptions of homeless people regarding their health-care needs and experiences of receiving health care. J Adv Nurs 2015; 71: 2096– 2107. [DOI] [PubMed] [Google Scholar]
- 14. Craig G M, Joly L M, Zumla A.. ‘Complex’ but coping: experience of symptoms of tuberculosis and health care seeking behaviours—a qualitative interview study of urban risk groups, London, UK. BMC Public Health 2014; 14: 618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Swigart V, Kolb R.. Homeless persons' decisions to accept or reject public health disease-detection services. Public Health Nurs 2004; 21: 162– 170. [DOI] [PubMed] [Google Scholar]
- 16. Martins D C. Experiences of homeless people in the health care delivery system: a descriptive phenomenological study. Public Health Nurs 2008; 25: 420– 430. [DOI] [PubMed] [Google Scholar]
- 17. West E L, Gadkowski L B, Ostbye T, Piedrahita C, Stout J E.. Tuberculosis knowledge, attitudes, and beliefs among North Carolinians at increased risk of infection. N C Med J 2008; 69: 14– 20. [PubMed] [Google Scholar]
- 18. Infanti J, Sixsmith J, Barry M M, Núñez-Córdoba J, Oroviogoicoechea-Ortega C, Guillén-Grima F A.. A literature review on effective risk communication for the prevention and control of communicable diseases in Europe. Stockholm, Sweden: European Centre for Disease Prevention and Control, 2013. [Google Scholar]
- 19. Targeted tuberculin testing and treatment of latent tuberculosis infection. Am J Respir Crit Care Med 2000; 161 Suppl 3: S221– S247. [DOI] [PubMed] [Google Scholar]
- 20. Kong P M, Tapy J, Calixto P, . et al. Skin-test screening and tuberculosis transmission among the homeless. Emerg Infect Dis 2002; 8: 1280– 1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nickasch B, Marnocha S K.. Healthcare experiences of the homeless. J Am Acad Nurse Pract 2009; 21: 39– 46. [DOI] [PubMed] [Google Scholar]
- 22. Wen C K, Hudak P L, Hwang S W.. Homeless people's perceptions of welcomeness and unwelcomeness in healthcare encounters. J Gen Intern Med 2007; 22: 1011– 1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ngamvithayapong-Yanai J. The role of qualitative research in ending TB. Public Health Action 2016; 6: 209. [DOI] [PMC free article] [PubMed] [Google Scholar]


